Abstract
Purpose of Review
Although empty nose syndrome (ENS) is axiomatically defined post nasal surgery, these patients present to otolaryngologists with complaints of nasal airflow dysfunction preoperatively. The critical question of how to resolve ENS should be in the preoperative assessment rather than focusing on interventions post nasal surgery. There are no proven factors from surgery that predict ENS post turbinate surgery. We review the latest literature on ENS and evaluate developing trends in the understanding of its pathophysiology and associations. This review seeks to develop a modern approach to the management of this recalcitrant condition.
Recent Findings
Recent literature on ENS suggests possible psychogenic etiologies and associations, providing an avenue for treatment strategies. Previous theories of ENS pathogenesis regarding extent of turbinate surgery are not supported by airflow and radiologic assessments. Premorbid neurosensory alterations may explain why some patients, often with mental health comorbidities, present for nasal surgery without significant clinical findings and is a patient population predisposed to ENS.
Summary
The concept of “functional nasal obstruction” or FNO, needs to become a diagnostic option for the clinician when assessing patients for nasal surgery. Patients identifying with ENS may be a population of patients with functional nasal obstruction, unrecognized and now after surgical efforts to relieve symptoms. The disorder underlying ENS should be considered an unrecognized risk factor in patient selection “prior” to nasal surgery rather than a postoperative complication “from” nasal surgery. Identifying this risk factor preoperatively is critical in avoiding subsequent morbidity. Further research into identifying “functional nasal obstruction” prior to nasal surgery should be undertaken as a priority over interventions after the ENS condition occurs.
Similar content being viewed by others
Introduction
Empty nose syndrome (ENS) remains a controversial topic in contemporary rhinology notwithstanding an initial description almost 30 years ago [1]. It is a phenomenon whereby patients present, after nasal surgery performed to relieve reported nasal obstruction, with postoperative continued or worsening paradoxical nasal obstruction despite a capacious nasal cavity. Debate remains not only around the optimal methods to manage ENS but also with regard to its etiology. Although the degree of nasal surgery is often implicated, studies do not show any difference in nasal airflow or resistance between patients who identify with ENS versus those with uneventful turbinate surgery [2]. Only studies using computational fluid dynamics models, largely from a single research center, have suggested differences [3,4,5,6]. The rarity of the condition has led to the lack of understanding of its pathophysiology and a multitude of reported treatments, issues embedded in this controversy.
In recent years, studies have identified potential pathophysiologic mechanisms inherent in ENS. These include a loss of trigeminal neural sensitivity, underlying anxiety/hyperventilation comorbidities or a possible mix of these producing symptoms. The definition of ENS is problematic as the presence of surgical attempts to improve the airway is part of the description. Therefore, it is has become axiomatic that ENS patients present as a result of their surgery. However, the constellation of presenting symptoms of a patient later identifying as ENS may predict persistent symptomatology after nasal surgery. In this article, we review the latest literature and discuss the various proposed mechanisms and management philosophies of ENS as well as our own approach to this recalcitrant condition.
Historical Perspective
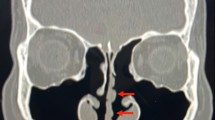
Described by Kern and Stenkvist at the Mayo Clinic in 1994, the term “empty nose syndrome” was originally used to depict the findings of tissue loss on sinus computed tomography (CT) associated with the hallmark symptom of paradoxical nasal obstruction [1]. This is classically attributed to aggressive inferior turbinate resection though symptoms have been described to occur after middle turbinate resection as well. ENS is not the same condition as atrophic rhinitis but the two are sometimes confused due to a similar presentation of symptoms such as nasal obstruction, dryness, and pain. In particular, patients with atrophic rhinitis typically present with complaints of cacosmia and true crusting, with nasal cultures showing presence of the pathogenic organism Klebsiella ozaenae. ENS and atrophic rhinitis are now acknowledged as separate clinical entities (Fig. 1A–B) [7,8,9].
Contrast of endoscopic findings between atrophic rhinitis and ENS. A Patient with atrophic rhinitis, presenting with nasal crusting, obstruction, and cacosmia. Endoscopic examination of the nasal cavity shows true crusting with nasal cultures confirming growth of Klebsiella. B Case example of ENS patient who initially presented with a sensation of nasal obstruction. Post inferior turbinoplasty, patient reported being distressed by persistent symptoms despite a normalized postoperative cavity with patent nasal airway
Nevertheless, the pathophysiology of ENS is still poorly understood. Many theories have been put forward but none sufficiently explain the phenomenon. Proposed etiologies include disruption of airflow dynamics and loss of airflow sensing neuroreceptors due to the alteration of nasal cavity anatomy from nasal surgery, resulting in the persistent sensation of nasal obstruction [3, 4, 9, 10]. Consequently, many of the treatments proposed for ENS have focused on restoration of tissue loss. However, assessments of inferior turbinate volume post turbinate reduction have shown no differences between ENS patients and patients with uneventful postoperative recovery [11]. Researchers have attempted to validate various diagnostic tests to confirm the diagnosis of ENS. These include a disease-specific questionnaire, the Empty Nose Syndrome 6-Item Questionnaire (ENS6Q), and the “cotton wool test” whereby the physician places a cotton wool ball into the patient’s nasal cavity to simulate the deficient nasal turbinate, [12] with an improvement in symptoms said to clinch the diagnosis. Common criticisms include the fact that the cotton wool test itself is inherently unblinded, while the ENS6Q includes questions that overlap with mental health symptoms.
Objective tests and measures have been proposed to define ENS. The presence of CT features of selective hypertrophy and mounding of nasal septal mucosa has been proposed as potentially diagnostic of ENS [11]. However, compensatory mucosal hypertrophy changes are expected post surgery and the ENS group assessed in those studies was more than twice as far out from their surgery compared to the control group, which in itself may have resulted in more septal remodeling.
Significant questions remain about the proposed origins of ENS and there are many fundamental discrepancies with its original description. The proposal of ENS as a "complication of surgery” assumes a casual association of turbinate tissue loss and symptoms of nasal obstruction. It is often overlooked that this group of patients clearly presented to an otolaryngologist initially with symptoms of nasal obstruction but had persistent or worsening symptoms from simple septal and turbinate surgery performed in efforts to relieve the presenting nasal obstruction. Like the feelings of breathlessness in hyperventilation or the “air hunger” of anxiety, it is plausible that a “functional” nasal obstruction may be occurring in some patients with ENS. Surgical attempts to intervene not only fail to resolve symptoms but also lead to worsening symptoms and deterioration in mental health from unrealized expectations of benefit. Other inconsistencies exist in the theories of ENS (Box 1).
Traditional Treatments
The traditional management of ENS consists of an array of medical and surgical therapies including the usage of topical therapies, filler injections, submucosal graft implantation, and stem cell injection therapy [13, 14]. Surgical interventions generally aim to restore inferior meatal volume, based on the concept of inferior meatal volume loss and the resultant alteration of airflow sensation as the potential etiology of symptoms in ENS patients. Unfortunately, none of the surgical intervention studies are controlled studies.
Topical Treatment
Medical therapy revolves around moisturization of the nasal lining, involving regular application of nasal saline irrigation and emollients [9]. Many of these ointments contain menthol, pine oil, and other trigeminal/transient receptor potential melastatin 8 (TRPM8) receptor agonists. These focus on relieving ENS symptoms via lubrication and recreating the cooling effect on the nasal cavity. High-volume irrigation is typically recommended due to improved distribution to the mucosal surfaces within the nasal cavity.
Submucosal Graft Implantation
Popularized surgical techniques primarily involve recreation of the inferior turbinate volume via submucosal implantation of the region of the inferior meatus with grafting materials [15, 16]. The array of grafts described includes acellular dermis, xenografts, cartilage, and synthetic implants such as silicone sheets and porous polyethylene (MedPor) [14]. The main disadvantages of this approach include risks specific to graft implantation such as graft extrusion and resorption.
Filler Injections
A less invasive surgical intervention for ENS is performed by injecting areas of the nasal cavity with a variety of fillers such as hyaluronic acid and carboxymethylcellulose [17, 18]. Similar to grafting techniques, filler injections attempt to restore nasal volume and bring the nose closer to a “physiological” state. This procedure is generally less preferred due to its inconsistent results, temporary effects, and possible tachyphylaxis.
Stem Cell Therapy
In an attempt to find a satisfactory treatment for ENS, Kim et al. evaluated the efficacy and safety of stem cell therapy as a novel method, using the injection of autologous stromal vascular fraction to both inferior turbinates [19]. Inflammatory markers were measured at baseline, with ENS patients showing an increase in markers such as interleukin (IL)-1β, IL-8, and calcitonin gene-related peptide. Initial results show a decrease in inflammatory cytokine expression in treated patients, in particular that of IL-1β and IL-8, though the mean Sinonasal Outcome Test (SNOT)-25 scores of patients at 6 months after injection did not differ significantly from baseline.
The Potential for “Functional Nasal Obstruction” Exists in Otolaryngology
Despite the aforementioned methods previously used to manage ENS, the inconsistency of outcomes together with the lack of control groups and long-term follow-up in studies highlights the need to better understand the pathophysiology of ENS [20]. The potential for an ENS patient’s receptiveness to care, attention, and placebo effect is high in single-arm studies. Additionally, the strategies here are very disparate as they are aimed at a wide range of methods from moisturization, to occlusion of airflow and stem cell therapies.
Earlier literature reviews on ENS pathogenesis attributed the condition primarily to post-surgical impairment of the neurosensory system and trigeminal nerve function in the nasal cavity [10, 13]. However, close scrutiny of the evidence surrounding the pathophysiology of ENS has challenged this original assertion by Kern et al. [21]. It has been shown that patients who have undergone sinonasal tumor resection, involving extensive resection of nasal cavity structures, do not develop ENS [22, 23•]. Other studies looking at turbinate resection during radical sinus surgery for inflammatory diseases also echo this observation [24, 25]. The near absence of ENS in these patient groups with significantly greater alteration of their nasal cavities, as compared to simple turbinate procedures, questions the veracity of the “post-surgical” theory of ENS (Fig. 2A–E). A systematic review of studies examining the pathophysiology of ENS, comparing ENS patients to those with uneventful recovery post turbinate surgery, noted similar anatomical changes between groups and highlighted the presence of significant comorbid mental health disorders in patients with ENS [26••]. This relationship supports the proposal of a “functional” nasal obstruction condition that must be present in some patients with nasal breathing symptoms that seek otolaryngologic assessment, in the same vein as functional hearing loss, functional dystonia, and functional epilepsy. There are examples of functional disorders, such as functional dyspepsia, that might have some subtle underlying pathophysiology beyond mental health interactions, but ultimately the mental health burden dominates symptomatology [27]. In ENS, there may be patients with subtle trigeminal nerve dysfunction but the symptom presentation is disproportionally dominated by deterioration in mental health. The diagnostic entity of “functional nasal obstruction” (FNO) must therefore surely exist within otolaryngology patients but the absence of its discussion in contemporary otolaryngology is remarkable.
Endoscopic examination of various nasal cavities, comparing the ENS patient to other patients with increasing extents of nasal surgery. A Inferior turbinoplasty (ENS patient), B inferior turbinoplasty (patient without ENS), C total inferior turbinectomy, D medial maxillectomy, and E wide resection of skull base tumor. Despite the increasingly extensive loss of nasal cavity structures in patients B–E, none of these patients developed ENS as in patient A
There has been an increasing trend related to published ENS topics over the past 5 years, with a gradual shift from developing novel, further surgical interventions in ENS to identifying associations with psychological factors in attempts to direct therapy to the mental health comorbidities that burden these patients.
Mental Health and Psychogenic Associations
Recent studies acknowledge the association between ENS and mental health comorbidities such as depression and anxiety, highlighting a potential treatment pathway to explore [28, 29, 30•]. However, the causal relationship between the two is difficult to prove, as to whether it is ENS causing subsequent mental health issues or instead patients suffering from underlying FNO developing ENS after surgery. Determining whether these comorbidities predispose a patient to ENS, or vice versa, can be challenging. Patients with seemingly no psychiatric history preoperatively could potentially have an underlying personality disorder or undiagnosed depression and anxiety. These can manifest and exacerbate after the psychological stress of the initial sinonasal surgery, acting as a predisposing factor in ENS rather than as a result of.
An earlier study by Manji et al. looked at the functional and psychological burden of patients with ENS [29]. Patients completed questionnaires assessing their psychological status which included the ENS6Q, the 9-item Patient Health Questionnaire for depression, and the 7-item Generalised Anxiety Disorder questionnaire [31]. ENS symptom severity was noted to have a strong positive correlation with depression, anxiety, and overall impairment in activities of daily living, and it was concluded that a multi-modal approach including cognitive behavioral therapy (CBT) may provide the most optimal treatment outcome.
It is interesting to note that patients with ENS often also fulfill the criteria for somatic symptom disorder [32, 33••]. As per the fifth edition of The Diagnostic and Statistical Manual of Mental Disorders, the diagnostic criteria for somatic symptom disorder include (A) one or more somatic symptoms that are distressing, (B) excessive thoughts, feelings, or behavior related to the somatic symptoms, (C) the state of being persistently symptomatic (typically more than 6 months) [34]. These symptoms are reminiscent of those typically seen in ENS patients and as such, it is not unreasonable to apply similar treatment modalities to those with ENS. Hyperventilation syndrome, characterized by excessive ventilation due to anxiety, has also shown to be comorbid in up to 77% of ENS patients [35] and should considered a potential etiologic factor. This is sometimes described as occurring due to the lack of sensation of the nasal airway in ENS, though laryngectomized patients have not been noted to have hyperventilation despite having a lack of nasal airflow [36]. Feelings of dyspnea, shortness of breath, air hunger, and inability to breathe are common to anxiety disorders [37].
Other studies have also noted the association between ENS and an increase in psychological burden [28, 30•, 38,39,40], with various questionnaires being used to diagnose and assess the distressing effects of ENS, such as the ENS6Q and the SNOT-25 [1]. Validated instruments including the Beck Anxiety Inventory (BAI) and the Beck Depression Inventory-II (BDI-II) have also been used to evaluate mental health comorbidities such as depression and anxiety [41, 42]. In particular, two separate research groups had similar findings of an increased prevalence of depression and mental health burden in ENS patients as compared to patients with chronic rhinosinusitis and chronic rhinitis [28, 30•]. The use of antidepressants and psychosomatic interventions such as CBT has shown potential benefit in ENS patients fulfilling the diagnostic criteria for somatic symptom disorder [33••].
Despite the mental health associations, it should be acknowledged that there is some evidence which suggests physical changes in the nasal anatomy of patients with ENS. Wu et al. showed that the nasal mucosa of ENS patients had a lower expression of TRPM8 receptors when compared to that of the control group [43]. These trigeminal receptors have been implicated in the sensation of nasal patency, though it is uncertain if a reduced number of these receptors were already present premorbid and the actual reason for the patient’s sense of nasal obstruction rather than as a result of surgery.
The Diagnostic Utility of Functional Nasal Obstruction (FNO) in Contemporary Otolaryngology
As we mature in our understanding of ENS, the literature acknowledges an underlying mental health theme which should be incorporated into clinical practice. Given the evidence presented, it would be prudent to manage ENS as a predisposing risk factor in surgery rather than a postoperative complication. Patients at risk for the condition that we currently refer to as ENS should be considered suffering from “functional nasal obstruction” or FNO. This would be in line with other functional conditions in medicine. In keeping the term ENS, it implies a sense of pervasive injustice to the patient and vilifies the surgeon. The idea that “too much tissue was taken” or “the wrong turbinate procedure was performed” is not supported by studies on ENS patients compared to those with uneventful outcomes after turbinate surgery [26••]. Such a non-evidence-based assessment delivers a fatalistic outlook for the patient, condemns the prior surgeon’s efforts to help, and reinforces the externalized locus of control that exists in many patients that blame a procedure for their ongoing symptoms. For many patients with FNO, the motivation for surgery includes unrealistic expectations of improved fitness, sleep, energy, and productivity after nasal surgery rather than simply relieving a blocked nose. FNO patients are at risk of having very high expectations from their turbinate surgery, and with the subsequent unrealized outcomes, the surgery becomes a trigger for mental health decline [44].
This shift in terminology might be more tactful to the patient with regard to future CBT and psychological support, avoids the fatalistic nature of the term “empty nose”, and be more evidence-based with regard to the condition’s etiology. Another practical rationale for this change in mindset is that screening for FNO as a risk factor for ENS would involve a simple but robust process which allows the avoidance of surgery in at-risk patients, potentially obviating the devastating outcome of a patient identifying as ENS. While it would be ideal to identify patients with FNO preoperatively, we are aware that this is not always possible and patients may present postoperatively with ENS despite best efforts. Hence, our current approach to FNO can be dichotomized into preoperative and postoperative strategies.
Preoperative Approach
Care should be taken during history taking to screen for mental health comorbidities such as depression and anxiety, and the SNOT-22 questionnaire can be a useful screening tool. From our experience, at-risk patients tend to have a relatively higher score in the emotional subdomains. This produces a “right shift” of responses in the bottom of the SNOT-22, which reflects the disproportionate severity of psychosocial domains over nasal symptoms. To evaluate patients suitable for turbinate reduction, we commonly use “Ray’s Rules,” [26••] which refers to patients having the triad of (1) fluctuating or “cycling” nasal congestion, (2) postural congestion, and (3) subjective response to topical nasal decongestant. The above represents typical responses in patients with turbinate pathophysiology whereas patients who present without these are more likely to have FNO and be poor surgical candidates. The clinician should also be wary of a disproportional symptom burden compared to objective endoscopic findings. Other useful adjunctive investigations include rhinomanometry to obtain objective measurements of nasal obstruction, as well as CT of the paranasal sinuses to rule out occult sinus disease.
For example, in a patient with nasal obstruction having comorbid depression, equivocal endoscopy, and a “right shift” in the SNOT-22 as well as normal rhinomanometry and CT of the paranasal sinuses, one needs to weigh the risk-benefit ratio of surgery in a potential FNO patient. Opting for conservative measures over surgical management may avoid an at-risk FNO patient developing ENS from surgery. Caution should be taken with the patient harboring unrealistic expectations of improved fitness, sleep, energy, and productivity after nasal surgery as such patients are at risk of having high expectations with unrealized outcomes triggering a mental health decline. When preoperative patients ask about “the risk of ENS” from their procedure, an evidence-based answer should be given (Box 2).
Postoperative Approach
Postoperatively, our approach to patients with FNO is similar to the preoperative approach with detailed history taking and examination undertaken to rule out other obvious causes for persistent symptoms. Rhinomanometry would be particularly useful to confirm normal airway resistance and ensure that no objective nasal obstruction is present, so that patients can be appropriately counseled and reassured. The ENS6Q and SNOT-25 can also be used as a diagnostic aid in these circumstances, with the BAI and BDI-II used to screen for anxiety and depression.
Additionally, referral to a mental health professional should be recommended depending on the impact on the patient’s daily functioning. Such patients are often severely distressed by their symptoms and it would be circumspect to proceed with an early referral for potential CBT and to ensure that appropriate treatments are undertaken for any other comorbid depression and anxiety. Clinicians should try to refocus the patient away from the pervasive sense of injustice that they feel from their journey, which started with a presentation to an otolaryngologist prior to any surgery. We take caution in condemning any prior surgery and provide phrasing that the original nasal obstructive symptoms simply did not have a turbinate etiology (i.e., FNO), and expectation of benefit from surgery was misplaced.
Conclusion
Functional nasal obstruction (FNO) is a diagnostic entity that all surgeons should be aware of as a likely predisposing factor for ENS. Further research is required to ensure the otolaryngology community can identify these patients early and avoid ENS as a sequela after nasal surgery. The literature on ENS supports a strong association with mental health comorbidities compared to other pathologic causes of nasal blockage. A change in the approach from looking at this entity as a postoperative syndrome to that of a preoperative “functional” nasal obstruction should be considered, with potentially converging etiologies of impaired trigeminal sensation, mental health comorbidities, and the unsuccessful nasal surgery as a stress event precipitating mental health decline.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Chhabra N, Houser SM. The diagnosis and management of empty nose syndrome. Otolaryngol Clin North Am. 2009;42(2):311–30, ix. https://doi.org/10.1016/j.otc.2009.02.001.
Konstantinidis I, Tsakiropoulou E, Chatziavramidis A, Ikonomidis C, Markou K. Intranasal trigeminal function in patients with empty nose syndrome. Laryngoscope. 2017;127(6):1263–7. https://doi.org/10.1002/lary.26491.
Li C, Farag AA, Leach J, Deshpande B, Jacobowitz A, Kim K, et al. Computational fluid dynamics and trigeminal sensory examinations of empty nose syndrome patients. Laryngoscope. 2017;127(6):E176–84. https://doi.org/10.1002/lary.26530.
Li C, Farag AA, Maza G, McGhee S, Ciccone MA, Deshpande B, et al. Investigation of the abnormal nasal aerodynamics and trigeminal functions among empty nose syndrome patients. Int Forum Allergy Rhinol. 2018;8(3):444–52. https://doi.org/10.1002/alr.22045.
Maza G, Li C, Krebs JP, Otto BA, Farag AA, Carrau RL, et al. Computational fluid dynamics after endoscopic endonasal skull base surgery-possible empty nose syndrome in the context of middle turbinate resection. Int Forum Allergy Rhinol. 2019;9(2):204–11. https://doi.org/10.1002/alr.22236.
Malik J, Li C, Maza G, Farag AA, Krebs JP, McGhee S, et al. Computational fluid dynamic analysis of aggressive turbinate reductions: is it a culprit of empty nose syndrome? Int Forum Allergy Rhinol. 2019;9(8):891–9. https://doi.org/10.1002/alr.22350.
Payne SC. Empty nose syndrome: what are we really talking about? Otolaryngol Clin North Am. 2009;42(2):331–7, ix-x. https://doi.org/10.1016/j.otc.2009.02.002.
Coste A, Dessi P, Serrano E. Empty nose syndrome. Eur Ann Otorhinolaryngol Head Neck Dis. 2012;129(2):93–7. https://doi.org/10.1016/j.anorl.2012.02.001.
Kuan EC, Suh JD, Wang MB. Empty nose syndrome. Curr Allergy Asthma Rep. 2015;15(1):493. https://doi.org/10.1007/s11882-014-0493-x.
Sozansky J, Houser SM. Pathophysiology of empty nose syndrome. Laryngoscope. 2015;125(1):70–4. https://doi.org/10.1002/lary.24813.
Thamboo A, Velasquez N, Ayoub N, Nayak JV. Distinguishing computed tomography findings in patients with empty nose syndrome. Int Forum Allergy Rhinol. 2016;6(10):1075–82. https://doi.org/10.1002/alr.21774.
Thamboo A, Velasquez N, Habib AR, Zarabanda D, Paknezhad H, Nayak JV. Defining surgical criteria for empty nose syndrome: validation of the office-based cotton test and clinical interpretability of the validated empty nose syndrome 6-item questionnaire. Laryngoscope. 2017;127(8):1746–52. https://doi.org/10.1002/lary.26549.
Gill AS, Said M, Tollefson TT, Steele TO. Update on empty nose syndrome: disease mechanisms, diagnostic tools, and treatment strategies. Curr Opin Otolaryngol Head Neck Surg. 2019;27(4):237–42. https://doi.org/10.1097/MOO.0000000000000544.
Talmadge J, Nayak JV, Yao W, Citardi MJ. Management of postsurgical empty nose syndrome. Facial Plast Surg Clin North Am. 2019;27(4):465–75. https://doi.org/10.1016/j.fsc.2019.07.005.
Lee TJ, Fu CH, Wu CL, Tam YY, Huang CC, Chang PH, et al. Evaluation of depression and anxiety in empty nose syndrome after surgical treatment. Laryngoscope. 2016;126(6):1284–9. https://doi.org/10.1002/lary.25814.
Houser SM. Surgical treatment for empty nose syndrome. Arch Otolaryngol Head Neck Surg. 2007;133(9):858–63. https://doi.org/10.1001/archotol.133.9.858.
Modrzynski M. Hyaluronic acid gel in the treatment of empty nose syndrome. Am J Rhinol Allergy. 2011;25(2):103–6. https://doi.org/10.2500/ajra.2011.25.3577.
Borchard NA, Dholakia SS, Yan CH, Zarabanda D, Thamboo A, Nayak JV. Use of intranasal submucosal fillers as a transient implant to alter upper airway aerodynamics: implications for the assessment of empty nose syndrome. Int Forum Allergy Rhinol. 2019;9(6):681–7. https://doi.org/10.1002/alr.22299.
Kim DY, Hong HR, Choi EW, Yoon SW, Jang YJ. Efficacy and safety of autologous stromal vascular fraction in the treatment of empty nose syndrome. Clin Exp Otorhinolaryngol. 2018;11(4):281–7. https://doi.org/10.21053/ceo.2017.01634.
Leong SC. The clinical efficacy of surgical interventions for empty nose syndrome: a systematic review. Laryngoscope. 2015;125(7):1557–62. https://doi.org/10.1002/lary.25170.
Moore EJ, Kern EB. Atrophic rhinitis: a review of 242 Cases. Am J Rhinol. 2001;15(6):355–61. https://doi.org/10.1177/194589240101500601.
Hardman J, Ahn J, Nirmalananda A. Assessing symptoms of empty nose syndrome in patients following sinonasal and anterior skull base resection. Aust J Otolaryngol. 2018;1.
• Wong EH, Orgain CA, Sansoni ER, Alvarado R, Grayson J, Kalish L, et al. Turbinate loss from non-inflammatory sinonasal surgery does not correlate with poor sinonasal function. Am J Otolaryngol. 2020;41(1):102316. https://doi.org/10.1016/j.amjoto.2019.102316. Study evaluating the effect of turbinate loss on sinonasal function in non-inflammatory sinonasal surgery.
Tan NC, Goggin R, Psaltis AJ, Wormald PJ. Partial resection of the middle turbinate during endoscopic sinus surgery for chronic rhinosinusitis does not lead to an increased risk of empty nose syndrome: a cohort study of a tertiary practice. Int Forum Allergy Rhinol. 2018. https://doi.org/10.1002/alr.22127.
Videler WJ, van Drunen CM, van der Meulen FW, Fokkens WJ. Radical surgery: effect on quality of life and pain in chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2007;136(2):261–7. https://doi.org/10.1016/j.otohns.2006.08.010.
•• Kanjanawasee D, Campbell RG, Rimmer J, Alvarado R, Kanjanaumporn J, Snidvongs K, et al. Empty nose syndrome pathophysiology: a systematic review. Otolaryngol Head Neck Surg. 2022;167(3):434–51. https://doi.org/10.1177/01945998211052919. A systematic review of the literature on the pathophysiology of empty nose syndrome.
Van Oudenhove L, Aziz Q. The role of psychosocial factors and psychiatric disorders in functional dyspepsia. Nat Rev Gastroenterol Hepatol. 2013;10(3):158–67. https://doi.org/10.1038/nrgastro.2013.10.
Kim CH, Kim J, Song JA, Choi GS, Kwon JH. The degree of stress in patients with empty nose syndrome, compared with chronic rhinosinusitis and allergic rhinitis. Ear Nose Throat J. 2021;100(2):NP87-NP92. https://doi.org/10.1177/0145561319858912.
Manji J, Nayak JV, Thamboo A. The functional and psychological burden of empty nose syndrome. Int Forum Allergy Rhinol. 2018;8(6):707–12. https://doi.org/10.1002/alr.22097.
• Lamb M, Bacon DR, Zeatoun A, Onourah P, Thorp BD, Abramowitz J, et al. Mental health burden of empty nose syndrome compared to chronic rhinosinusitis and chronic rhinitis. Int Forum Allergy Rhinol. 2022;12(11):1340–9. https://doi.org/10.1002/alr.22997. Cross-sectional survey of the mental health burden of patients with empty nose syndrome.
Velasquez N, Thamboo A, Habib AR, Huang Z, Nayak JV. The empty nose syndrome 6-item questionnaire (ENS6Q): a validated 6-item questionnaire as a diagnostic aid for empty nose syndrome patients. Int Forum Allergy Rhinol. 2017;7(1):64–71. https://doi.org/10.1002/alr.21842.
Lemogne C, Consoli SM, Limosin F, Bonfils P. Treating empty nose syndrome as a somatic symptom disorder. Gen Hosp Psychiatry. 2015;37(3):273.e9-10. https://doi.org/10.1016/j.genhosppsych.2015.02.005.
•• Tian P, Hu J, Ma Y, Zhou C, Liu X, Dang H, et al. The clinical effect of psychosomatic interventions on empty nose syndrome secondary to turbinate-sparing techniques: a prospective self-controlled study. Int Forum Allergy Rhinol. 2021;11(6):984–92. https://doi.org/10.1002/alr.22726. A prospective study looking at the utility of psychosomatic interventions in patients with empty nose syndrome.
American Psychiatric Association D, Association AP. Diagnostic and statistical manual of mental disorders: DSM-5. vol 5. American psychiatric association Washington, DC; 2013.
Mangin D, Bequignon E, Zerah-Lancner F, Isabey D, Louis B, Adnot S, et al. Investigating hyperventilation syndrome in patients suffering from empty nose syndrome. Laryngoscope. 2017;127(9):1983–8. https://doi.org/10.1002/lary.26599.
Baraniuk JN. Subjective nasal fullness and objective congestion. Proc Am Thorac Soc. 2011;8(1):62–9. https://doi.org/10.1513/pats.201006-042RN.
De Peuter S, Van Diest I, Lemaigre V, Verleden G, Demedts M, Van den Bergh O. Dyspnea: The role of psychological processes. Clin Psychol Rev. 2004;24(5):557–81. https://doi.org/10.1016/j.cpr.2004.05.001.
Huang CC, Wu PW, Fu CH, Huang CC, Chang PH, Wu CL, et al. What drives depression in empty nose syndrome? a sinonasal outcome test-25 subdomain analysis. Rhinology. 2019;57(6):469–76. https://doi.org/10.4193/Rhin19.085.
Huang CC, Wu PW, Fu CH, Huang CC, Chang PH, Lee TJ. Impact of psychologic burden on surgical outcome in empty nose syndrome. Laryngoscope. 2021;131(3):E694–701. https://doi.org/10.1002/lary.28845.
Huang CC, Wu PW, Lee CC, Chang PH, Huang CC, Lee TJ. Suicidal thoughts in patients with empty nose syndrome. Laryngoscope Investig Otolaryngol. 2022;7(1):22–8. https://doi.org/10.1002/lio2.730.
Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–7. https://doi.org/10.1037//0022-006x.56.6.893.
Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck depression inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67(3):588–97. https://doi.org/10.1207/s15327752jpa6703_13.
Wu CL, Fu CH, Lee TJ. Distinct histopathology characteristics in empty nose syndrome. Laryngoscope. 2021;131(1):E14–8. https://doi.org/10.1002/lary.28586.
Ludwig L, Pasman JA, Nicholson T, Aybek S, David AS, Tuck S, et al. Stressful life events and maltreatment in conversion (functional neurological) disorder: systematic review and meta-analysis of case-control studies. Lancet Psychiatry. 2018;5(4):307–20. https://doi.org/10.1016/s2215-0366(18)30051-8.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Larry Kalish is on the speakers’ bureau for Care Pharmaceuticals, Sequiris, and Meda Pharmaceuticals. Raymond Sacks is a consultant for Medtronic. Lu Hui Png has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Png, L.H., Kalish, L. & Sacks, R. Empty Nose Syndrome: The Case for “Functional Nasal Obstruction” as a Predisposing Risk Prior to Nasal Surgery. Curr Otorhinolaryngol Rep 11, 422–429 (2023). https://doi.org/10.1007/s40136-023-00487-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-023-00487-w