Abstract
Purpose of Review
The aim of this analysis is to provide a synopsis of the surgical methods utilized to treat nasal valve collapse resulting in airway obstruction, and to evaluate and contrast lateral crural strut grafts (LCSG) and lateral crural tensioning (LCT).
Recent Findings
Lateral crural strut grafting is a major technique used to treat external nasal valve collapse. However, in recent years, lateral crural tensioning combined with articulated alar rim grafts (AARG) has become popular. A study comparing LCT-AARG to LCSG demonstrated a greater reduction in total nasal airway resistance, as measured by rhinomanometry.
Summary
While LCSG creates a rigid structure, it may require a fair amount of cartilage and has the potential to crowd the airway. In contrast, LCT-AARG can achieve the same improvement in airway however consumes less cartilage, is less likely to crowd the airway, is preferential in narrow noses, and has the additional aesthetic benefits associated with rim grafting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical techniques to address nasal valve collapse continue to evolve, but all share the common objectives of either expanding cross-sectional area or stabilizing deformable structures. Centrally, structural rhinoplasty relies upon the use of cartilage grafts to provide axial stability to the nasal vault in terms of L-strut support. Laterally, grafts are used to prevent sidewall motion due to excessive transmural pressure drops. Numerous techniques have evolved over decades to create stability across the nasal vault, though most are extensions of classical “beam and post” construction techniques [1]. Along the nasal sidewall, lateral crural strut grafts are a classic example of this concept where a central septal extension graft (post) is combined with a long cartilage graft beneath the lateral crus (beam) to provide stability across the entire sidewall. In contrast, newer structural rhinoplasty methods have evolved that rely upon balancing tensile and compressive forces to resist deformation and is akin to the use of ties and struts in civil engineering [2]. This concept is best illustrated by lateral crural tensioning, which relies upon a septal extension graft (strut) and taught lateral crurae (tie).
This chapter will review the physiology of nasal obstruction and valve collapse, and summarize treatment options with an emphasis on lateral crural strut grafts (LCSG) and lateral crural tensioning (LCT).
Anatomic Basis of Nasal Airway Obstruction
Nasal valve compromise is a distinct cause of nasal airway obstruction [3]. It is generally accepted that the term “nasal valve” refers to region in the nasal cavity where airway is most narrow, and thus where airflow is most restricted [3]. In reality, nasal airflow is complex, the structure is deformable, active elements like the muscle alter shape, and turbulence dominates under most non-resting physiologic conditions.
Clinicians divide the nasal valve into external and internal components. The external nasal valve is defined as the area in the nasal vestibule under the nasal ala, formed by the caudal septum, medial crura of the alar cartilage, alar rim, and nasal sill [3]. The internal valve is defined as the region under the upper lateral cartilage, bound medially by the dorsal septum, inferiorly by the head of the inferior turbinate, and laterally by the upper lateral cartilage [3]. Contact between the upper lateral cartilages and septum can unfavorably affect breathing. It is generally accepted the internal nasal valve should maintain an angle of 10–15°, below which patients will experience nasal obstruction [3]. Measuring the angle of the internal nasal valve can be a challenge. Physical examination and endoscopy both fail to provide accurate quantitative estimates of valve angle. CT imaging has demonstrated the challenge of measuring the internal nasal valve geometry, let alone identifying its locus. Optical coherence tomography found a reduction of the valve angle from 18.3 to 14.1° led to subjective nasal obstruction [4].
Nasal valve insufficiency can occur due to various factors such as the collapse of the alar lobule or the nasal sidewall incorporating the upper lateral cartilage. Additionally, a high septal deviation, hypertrophied inferior turbinate, severely ptotic nasal tip, wide nasal columella, or a caudal septal deviation can also contribute to nasal valve collapse [3].
Nasal valve collapse is a common finding prior to nasal surgery. Many rhinoplasty techniques such as separation of the upper lateral cartilages (ULC) from the septum, hump removal, and septal cartilage resection alter the relationship between the ULC and the caudal septum either directly or through scarring, fibrosis, and subsequent collapse [5]. It is therefore important to use techniques to mitigate additional iatrogenic obstruction.
Collapsible soft tissues and/or lower lateral cartilage deformities in the alar lobule can contribute to obstruction [3]. Lateral crura shape and stiffness impact airway function and are an increasingly recognized contributor to nasal obstruction [6]. The ideal lateral crus shape is convex adjacent to the dome and flattens as one moves laterally [6]. Flaccid, malformed, malpositioned, or short lateral crurae can lead to a dynamic collapse of the lobule and present a challenge for treatment [7].
Physiology of Nasal Valve Collapse
Classically, valve collapse is described using Bernoulli’s principle. Air enters the nose; it passes through the narrowed valve regions and accelerates, leading to a drop in intraluminal pressure and collapse of sidewall [3]. The mechanism of airway obstruction in the nasal valve is a consequence of reduced cross-sectional area and deformable lateral walls [5]. The stability of the sidewall depends on its intrinsic mechanical properties and transmural pressure gradient.
Inasmuch as no actual anatomic “valve” exits, but rather a flow limiting region better named the “nasal gateway” is the key location where flow becomes complex [8]. This area begins approximately 2 cm from the nares according to 3D modeling, and extends at least 1 cm beyond the pyriform [9]. When narrowing or expansion occurs, turbulence may occur which leads to collapse and obstruction [8].
To enhance airflow through the airway, it is necessary to increase its cross-sectional area and/or minimize flexural deformation along the lateral walls. There are two methods to achieve this second objective: stiffening the lateral wall with materials like LCSG or battens, or increasing tension across the surface with LCT. The former is similar to the beam and post-conceptual framework, while the latter is comparable to the use of ties and struts. The tie-and-strut model is a versatile design method that balances tension (tie) and compression (strut) and does not place a premium on material (e.g., cartilage) [10].
Overview of Approaches to Support the Nasal Valve
By definition, correcting the compromised nasal valve means addressing the septum, the inferior turbinate, and nasal sidewall. Techniques such as alar batten grafts, spreader grafts, butterfly grafts, flare sutures, suspension sutures, LCGS, lateral crural transposition, and LCT with AARG are aimed at correcting the problem of inadequate lateral wall support [3, 11]. Septal deformations are often addressed through numerous maneuvers such as septoplasty, septal repositioning, or in extreme cases extracorporeal septal reconstruction [11]. Enlarged inferior turbinates are addressed through variations of turbinoplasty. Other adjuncts like columellar base narrowing are also utilized.
The remainder of this chapter will be dedicated to the comparison between LCSG and LCT in conjunction with AARG for the purpose of providing support to the nasal valve.
Lateral Crural Strut Grafts
Technique
First described by Gunter and Friedman in 1997, LCSG involves using cartilage grafts secured to the undersurface of the crura to reshape, reposition, or reconstruct the lateral crura. LCSG can correct curvature and deformities of the lateral crus [7].
This is generally performed via open rhinoplasty. The vestibular skin is undermined off the lateral crus starting at the cephalic border and progressing caudally along the entire cartilage. A cephalic trim may be performed at the same time [7]. Notably, the vestibular skin is left attached to the caudal border along the anterior two-thirds of the lateral crus [7]. Next, cartilage grafts are fashioned and placed into the pocket created on the deep surface of the lateral crus. Once placed, the graft is sutured to the body of crus. The grafts are typically 15–25 mm largely extending along the length of the crus from just lateral to the dome, and 3–5 mm in width. The lateral end of the graft is often placed over pyriform aperture rim, so that there is support both centrally and laterally. Longer grafts (25–30 mm) are required to correct malpositioned lateral crura, alar retraction, and severe alar collapse [7].
The LCSG was popularized by Toriumi who outlined key concepts relating lateral crus position and geometry [12]. In this technique, the entire lateral cartilage is freed from the vestibular skin for the purposes of repositioning. Repositioning or transposition of the crus with a LCSG is a powerful manuever to correct excessive convexity and alar malposition [13]. LCSG can be used to flatten concavity as well [13].
Indications
LCSG is indicated in lateral crural recurvature, external nasal valve collapse, alar rim collapse, correction of the boxy nasal tip, lateral crura malposition, alar rim retraction, and excessive lateral crura convexity [7].
Pros of Lateral Crural Strut Grating
The use of LCSG for external nasal valve support is a well-established technique. The graft forms a rigid structure that is very stable, supported medially by the septal extension graft/domal unit and laterally by the pyriform. If perched on the pyriform aperture, it facilitates the lateral position of the alar wall and widens the nasal aperture internally. Given the amount of stability provided by LCSG alone, the use of a caudal septal extension graft is not always necessary for tip support, provided the medial crural/tip complex is strong.
Cons of Lateral Crural Strut Grafting
This technique consumes significant reservoirs of cartilage. These grafts must be very straight and often must overlap the pyriform aperture to prevent collapse or medialization of the graft edge on inspiration. As noted previously, each LCSG length is on average at least 15–25 mm (30 mm if combined with repositioning) and 3–5 mm in width [7]. Septal cartilage is optimal, followed by rib [13]. Auricular cartilage may be too curved and may lack adequate rigidity. This robust graft may widen the nose or be visible in patients with thin skin. It may lead to an overly flat appearance along the alar lobule with loss of native aesthetic curvature along the supra-alar crease. With transposition, a void is created between the upper and lower alar cartilages, which may require additional cartilage grafts as battens. Rim grafts may be required with this approach as well. Finally, a LCSG graft occupies space. This composite structure thickens the sidewall, and hence, stability and stiffness may come at the cost of a reduction in airway cross-sectional area. This can be catastrophic in patients with a very thick and narrow nasal vault, or those who have little distance between the lateral wall and the septum. Overall, this is a large cartilage-consuming technique.
Lateral Crural Tensioning
Technique
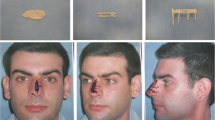
Davis’s lateral crural tensioning maneuver involves performing an aggressive lateral crural steal maneuver in tandem with a caudal septal extension graft (CSEG) [14•, 15, 16]. The lateral crural steal creates a new domal angle along the lateral crus cartilage by recruiting and advancing a portion of the lateral crura medially [14•, 17]. This modified structure is most commonly stabilized by securing it to a CSEG. This advancement shortens the crus and when the new dome is secured to the CSEG and tension increases across the entire length. The steal and tensioning collectively eliminate convexity. The increased tension in turn stabilizes the sidewall and reduces the propensity for dynamic collapse [14•, 18••]. Please see Fig. 1 for intra-operative photos of the technique.
Lateral crural tensioning with CSEG and articulated alar rim grafts. Row 1 from left to right: A with CSEG in place, mark the natural domes of the lower lateral cartilages. B Recruit and advance portion of lateral crura medially to perform lateral crural steal. C Mark the location of the new dome along the lateral crus. Row 2 from left to right: D perform a horizontal mattress suture to create the new dome and establish tensioning. E Secure new structure to CSEG, repeat on opposite side. F Add AARGs bilaterally. Abbreviations: CSEG, caudal septal extension graft; AARGs, articulated alar rim grafts
A CSEG is valuable because it enables comprehensive control of tip projection, rotation, supratip break, infratip break point, and columellar show [2]. The CSEG offers a notable difference from a lateral crural steal alone, as it decouples rotation at the expense of projection that are inherent to a classic lateral crural steal when used alone. In cases of extreme projection, a medial crural division and overlay can be performed following the lateral crural steal, and this medial crural overlay complex is then secured to the CSEG. In select cases with excess caudal septum, a direct tongue-in-groove technique can be used [2].
The recruitment process that occurs with the steal maneuver tends to weaken support through the soft triangle as the caudal border of the crus is medially advanced. Support is required to stabilize this region and correct a potential secondary cosmetic deformity. AARG is used in this setting; their use and placement may be nuanced. While the LCT provides sidewall support, the AARG provides support along the alar margin [11, 19•]. The AARGs are sutured just lateral to the new dome, and then are inserted into a precise soft tissue pocket parallel to the alar margin [11, 18••]. Unlike LCSG, rim grafts tend to be shorter (15–22 mm) and triangular in shape with a base of 4–6 mm [11]. Less cartilage is required for an AARG.
Indications
Lateral crural tensioning corrects dynamic collapse of the external nasal valve and eliminates lateral crural convexity as it refines the tip [2]. LCT is indicated for correction of lateral crural recurvature, external nasal valve collapse, alar rim collapse, correction of bossae, lateral crura malposition, alar rim retraction, and excessive lateral crura convexity [7]. This is essentially identical to LCSG use. Rim grafts are frequently required as LCT can weaken support across the soft triangle facet [19•]. Indications for rim grafts include a weak soft tissue triangle, presence of an alar margin furrow, lack of an alar ridge, and may also be used to correct cephalically oriented lower lateral cartilages [11, 19•].
Pros of Lateral Crural Tensioning
A major advantage of LCT is that it increases stability of the lateral wall through suturing technique without using a large beam made of cartilage [2]. Stability is supplied by tension, and the right and left force vectors across the crurae balance one another while vertical forces are countered by the CSEG [11]. The flexural stability of the alar sidewall is achieved through tensioning and thus dynamic collapse of the nasal alae is reduced. This is a large cartilage-sparing technique.
In contrast to a LCSG, LCT does not require any additional cartilage; therefore, there is overall less consumption of cartilage in comparison. Given that a composite structure is not created, there is no additional bulk, and the inner cross-sectional area of the external nasal valve is not reduced. There is less potential for crowding of the airway [2, 18••]. If rim grafts (in particular AARGs) are used, then a modest amount of additional graft material is required [11]. In addition, suturing techniques preserve the structure, and are adjustable and reversible which is important given rhinoplasty has a historically high revision rate [2].
Performing LCT requires less dissection as compared to LCSG and avoids the morbidity of degloving much of the vestibular surface of the crus. Aesthetically, the curvature of the crura can also be addressed without resection of cartilage or lateral crural division and overlap [2].
The addition of a CSEG to this technique allows the surgeon to maintain both projection and rotation, in comparison to a lateral crural steal alone where projection and rotation are linked [2, 20, 21].
The addition of AARG to this technique allows for additional soft triangle support, alar lobule stability, creation of the alar ridge, and effacement of the alar margin furrow [11]. The AARG contributes to airway patency through a cantilevering effect of the native lower lateral crua [18••]. AARGs require less cartilage than LCSG, are positioned at the alar margin, and do not crowd the valve [19•]. They can be positioned to flare the nostrils which can be of exceptional value in the narrow nasal tip [22].
Kondo et al. published a study in 2020 comparing the effects of LCT with AARG to LCSG [18••]. This study demonstrated benefit in change in total nasal airway resistance (NAR) measured on rhinomanometry in patients who underwent LCT with AARG compared to LCSG. There was no significant difference in other outcome measures including nasal peak inspiratory flow (NPIF), Nasal Obstruction Symptom Evaluation (NOSE), and nasal obstruction score [18••].
Cons of Lateral Crural Tensioning
Lateral crural tensioning is a nuanced and challenging suture technique. It is typically combined with a CSEG and AARG, therefore requires these additional skills to maximize outcomes. It is possible to create a columellar or tip deviation; therefore, the surgeon must give attention to adequately balancing forces between the right and left steal. Aggressive suture fixation of both medial crura to the CSEG can help to redistribute forces that might otherwise act upon the nasal tip alone.
Conclusion
In summary, both grafting and tensioning techniques can be used to address nasal valve collapse. When the two techniques are compared, LCT with AARG can achieve the same improvement in airway as LCSG; however, tensioning consumes less cartilage, is less likely to crowd the airway, is especially preferential in narrow noses, and has the additional benefits associated with rim grafting. LCT with AARG is a nuanced technique associated with a steep learning curve.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kutz M. Eshbach’s handbook of engineering fundamentals, fifth edition; 2009. https://doi.org/10.1002/9780470432754.
Foulad A, Volgger V, Wong B. Lateral crural tensioning for refinement of the nasal tip and increasing alar stability: a case series. Facial Plast Surg. 2017;33(3):316–23. https://doi.org/10.1055/s-0037-1602143FromNLMMedline.
Rhee JS, Weaver EM, Park SS, Baker SR, Hilger PA, Kriet JD, Murakami C, Senior BA, Rosenfeld RM, DiVittorio D. Clinical consensus statement: diagnosis and management of nasal valve compromise. Otolaryngol Head Neck Surg. 2010;143(1):48–59. https://doi.org/10.1016/j.otohns.2010.04.019FromNLMMedline.
Englhard AS, Wiedmann M, Ledderose GJ, Lemieux B, Badran A, Jing JC, Chen Z, Volgger V, Wong BJF. In vivo imaging of the internal nasal valve during different conditions using optical coherence tomography. Laryngoscope. 2018;128(3):E105–10. https://doi.org/10.1002/lary.26962FromNLMMedline.
Spielmann PM, White PS, Hussain SS. Surgical techniques for the treatment of nasal valve collapse: a systematic review. Laryngoscope. 2009;119(7):1281–90. https://doi.org/10.1002/lary.20495FromNLMMedline.
Neves JCTD. Lateral crura control in nasal tip plasty: cephalic oblique domal suture, 7X suture and ANSA banner. Annals of Plastic and Reconstructive Surgery 2020;4(3).
Gunter JP, Friedman RM. Lateral crural strut graft: technique and clinical applications in rhinoplasty. Plast Reconstr Surg 1997;99(4):943–952; discussion 953–945. https://doi.org/10.1097/00006534-199704000-00001. From NLM Medline.
Tripathi PB, Elghobashi S, Wong BJF. The myth of the internal nasal valve. JAMA Facial Plast Surg. 2017;19(4):253–4. https://doi.org/10.1001/jamafacial.2017.0039FromNLMMedline.
Shaida A M, Kenyon GS. The nasal valves: changes in anatomy and physiology in normal subjects. Rhinology. 2000;38(1):7–12. From NLM Medline.
Williams C, Deschenes D, Bayrak O. Strut-and-tie model design example for bridges 5–5253–01–1. 2012.
Goodrich JL, Wong BJ. Optimizing the soft tissue triangle, alar margin furrow, and alar ridge aesthetics: analysis and use of the articulate alar rim graft. Facial Plast Surg. 2016;32(6):646–55. https://doi.org/10.1055/s-0036-1596049FromNLMMedline.
Toriumi DM. New concepts in nasal tip contouring. Arch Facial Plast Surg. 2006;8(3):156–85. https://doi.org/10.1001/archfaci.8.3.156FromNLMMedline.
Toriumi DM, Asher SA. Lateral crural repositioning for treatment of cephalic malposition. Facial Plast Surg Clin North Am. 2015;23(1):55–71. https://doi.org/10.1016/j.fsc.2014.09.004FromNLMMedline.
• Davis RE. Lateral crural tensioning for refinement of the wide and underprojected nasal tip: rethinking the lateral crural steal. Facial Plast Surg Clin North Am. 2015;23(1):23–53. https://doi.org/10.1016/j.fsc.2014.09.003FromNLMMedline. This article introduces the techqniue of lateral crural tensioning.
Davis RE. Nasal tip complications. Facial Plast Surg. 2012;28(3):294–302. https://doi.org/10.1055/s-0032-1312700FromNLMMedline.
Davis RE. Revision of the overresected nasal tip complex. Facial Plast Surg. 2012;28(4):427–39. https://doi.org/10.1055/s-0032-1319844FromNLMMedline.
Kridel RW, Konior RJ, Shumrick KA, Wright WK. Advances in nasal tip surgery. The lateral crural steal. Arch Otolaryngol Head Neck Surg. 1989;115(10):1206–1212. https://doi.org/10.1001/archotol.1989.01860340060018. From NLM Medline.
•• Kondo M, Orgain C, Alvarado R, Marcells GN, Harvey RJ. The effects of lateral crural tensioning with an articulated alar rim graft versus lateral crural strut graft on nasal function. Facial Plast Surg Aesthet Med. 2020;22(4):281–285. https://doi.org/10.1089/fpsam.2020.0056. From NLM Medline. This article is the first to compare the functional outcomes of these two technqiues.
• Calloway HE, Heilbronn CM, Gu JT, Pham TT, Barnes CH, Wong BJ. Functional outcomes, quantitative morphometry, and aesthetic analysis of articulated alar rim grafts in septorhinoplasty. JAMA Facial Plast Surg. 2019;21(6):558–65. https://doi.org/10.1001/jamafacial.2019.1130FromNLMMedline. This article publishes on outcomes of the articulated alar rim graft.
Moubayed SP, Abou Chacra Z, Kridel RW, Ahmarani C, Rahal A. Precise anatomical study of rhinoplasty: description of a novel method and application to the lateral crural steal. JAMA Facial Plast Surg. 2014;16(1):25–30. https://doi.org/10.1001/jamafacial.2013.1416FromNLMMedline.
Patrocinio LG, Patrocinio TG, Barreto DM, Subhan YS, Patrocinio JA. Evaluation of lateral crural steal in nasal tip surgery. JAMA Facial Plast Surg. 2014;16(6):400–4. https://doi.org/10.1001/jamafacial.2014.486FromNLMMedline.
Kim SA, Jang YJ. Mono-unit alar rim graft technique for tip-alar margin support. Aesthet Surg J. 2020;40(10):NP588–NP596. https://doi.org/10.1093/asj/sjaa148. From NLM Medline.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Best, C.A.E., Wong, B.JF. Nasal Valve Management: The Case to Move Away from Grafts to Tensioning. Curr Otorhinolaryngol Rep 11, 260–265 (2023). https://doi.org/10.1007/s40136-023-00478-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-023-00478-x