Abstract
Purpose of Review
This review article will discuss recent developments in high-resolution pharyngeal manometry, including diagnostic applications, and proposed standard metrics and protocol, as well as its use as a therapeutic biofeedback tool.
Recent Findings
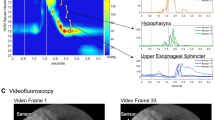
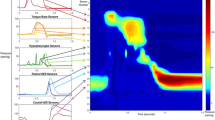
An International High-Resolution Pharyngeal Manometry (HRPM) Working Group has proposed use of three classes of HRPM metric standardization of HRPM data collection: pharyngeal lumen occlusive pressures (including pressures at the velopharynx, mesopharynx, and hypopharynx), upper esophageal sphincter (UES) function parameters (UES relaxation time and integrated relaxation pressure), and hypopharyngeal intrabolus pressure. The pharyngeal contractile integral (PhCI), in particular, has been shown to have promise as an indicator of the presence of swallowing impairment. Complex biomechanical relationships between pharyngeal drive and UES contractility have been identified, necessitating that clinicians take the entire system into account when assessing pharyngeal swallowing deficits. HRPM biofeedback therapy is an emerging form of dysphagia therapy which provides visual feedback of swallowing performance to patients in real time.
Summary
HRPM is a non-radiologic clinical tool that provides objective measures of pharyngeal swallowing pressures and timing. Development of normative values remains an ongoing effort, with only a few studies available that provide normal values for the standard metrics recently proposed by the HRPM International Working Group. HRPM biofeedback dysphagia therapy is safe and well-tolerated, and has anecdotal evidence supporting its use.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gyawali CP, Kahrilas PJ. A short history of high-resolution esophageal manometry. Dysphagia. 2021 Nov 5.
Clouse RE, Staiano A, Alrakawi A, Haroian L. Application of topographical methods to clinical esophageal manometry. Am J Gastroenterol. 2000;95(10):2720–30.
Clouse RE, Staiano A. Topography of the esophageal peristaltic pressure wave. Am J Physiol. 1991;261(4 Pt 1):G677-684.
Kahrilas PJ, Ghosh SK, Pandolfino JE. Esophageal motility disorders in terms of pressure topography: the Chicago Classification. J Clin Gastroenterol. 2008;42(5):627–35.
Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJPM, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24 Suppl 1(Suppl 1):57–65.
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJPM, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160–74.
•• Yadlapati R, Kahrilas PJ, Fox MR, Bredenoord AJ, Prakash Gyawali C, Roman S, et al. Esophageal motility disorders on high-resolution manometry: Chicago Classification version 4.0©. Neurogastroenterol Motil. 2021;33(1):e14058. Defines the most recent iteration of the Chicago Classification, the classification scheme used to identify esophageal motility disorders using HRM metrics.
Brandy S, Donzelli J. The modified barium swallow and the functional endoscopic evaluation of swallowing. Otolarnygol Clin North Am. 2013;46(6):1009–22.
Omari T, Schar M. High-resolution manometry: what about the pharynx? CurrOpinOtolaryngol Head Neck Surg. 2018;26:382–91.
Huckabee ML, Flynn R, Mills M. Expanding rehabilitation options for dysphagia: skill-based swallowing training. Dysphagia. 2022.
• Cock C, Omari T. Diagnosis of swallowing disorders: how we interpret pharyngeal manometry. Curr Gastroenterol Rep. 2017;19(3):11. Clinical review which defines various HRPM metrics and explains their clinical relevance.
•• Omari TI, Ciucci M, Gozdzikowska K, Hernández E, Hutcheson K, O’Rourke A, et al. High-resolution pharyngeal manometry and impedance: protocols and metrics-recommendations of a high-resolution pharyngeal manometry international working group. Dysphagia. 2020;35(2):281–95.
Ferris L, Schar M, McCall L, Doeltgen S, Scholten I, Rommel N, et al. Characterization of swallow modulation in response to bolus volume in healthy subjects accounting for catheter diameter. Laryngoscope. 2018;128(6):1328–34.
Winiker K, Gillman A, Guiu Hernandez E, Huckabee ML, Gozdzikowska K. A systematic review of current methodology of high resolution pharyngeal manometry with and without impedance. Eur Arch Otorhinolaryngol. 2019;276(3):631–45.
Doeltgen SH, Ong E, Scholten I, Cock C, Omari T. Biomechanical quantification of Mendelsohn maneuver and effortful swallowing on pharyngoesophageal function. Otolaryngol Head Neck Surg. 2017;157(5):816–23.
• O’Rourke A, Humphries K, Lazar A, Martin-Harris B. The pharyngeal contractile integral is a useful indicator of pharyngeal swallowing impairment. NeurogastroenterolMotil. 2017;29(12). Prospective observational study examining the relationship between PhCI and videofluoroscopic abnormalities as assessed by the MBSImp.
Martin-Harris B, Brodsky MB, Michel Y, Castell DO, Schleicher M, Sandidge J, et al. MBS measurement tool for swallow impairment–MBSImp: establishing a standard. Dysphagia. 2008;23(4):392–405.
• Nativ-Zeltzer N, Logemann JA, Zecker SG, Kahrilas PJ. Pressure topography metrics for high-resolution pharyngeal-esophageal manofluorography-a normative study of younger and older adults. Neurogastroenterol Motil. 2016;28(5):721–31. Prospective observational study that collected normative data from different age groups using HRPM concurrently with videoflouroscopy.
• Jadcherla SR, Prabhakar V, Hasenstab KA, Nawaz S, Das J, Kern M, et al. Defining pharyngeal contractile integral during high-resolution manometry in neonates: a neuromotor marker of pharyngeal vigor. Pediatr Res. 2018;84(3):341–7. Observational study that characterized PhCI in a cohort of 19 neonates and assessed the effect of different modes of stimulation on PhCI.
Jones CA, Colletti CM. Age-related functional reserve decline is not seen in pharyngeal swallowing pressures. J Speech Lang Hear Res. 2021;64(10):3734–41.
Regan J. Impact of sensory stimulation on pharyngo-esophageal swallowing biomechanics in adults with dysphagia: a high-resolution manometry study. Dysphagia. 2020;35(5):825–33.
Schaen-Heacock NE, Jones CA, McCulloch TM. Pharyngeal swallowing pressures in patients with radiation-associated dysphagia. Dysphagia. 2021;36(2):242–9.
Kern MK, Balasubramanian G, Sanvanson P, Agrawal D, Wuerl A, Shaker R. Pharyngeal peristaltic pressure variability, operational range, and functional reserve. Am J PhysiolGastrointest Liver Physiol. 2017;312(5):G516–25.
Omari TI, Dejaeger E, Tack J, Van Beckevoort D, Rommel N. Effect of bolus volume and viscosity on pharyngeal automated impedance manometry variables derived for broad dysphagia patients. Dysphagia. 2013;28(2):146–52.
• Walczak CC, Jones CA, McCulloch TM. Pharyngeal pressure and timing during bolus transit. Dysphagia. 2017;32(1):104–14. Observational study of a cohort of 10 healthy subjects which used concurrent HRPM and videofluoroscopy to characterize patterns of bolus pressure during normal swallowing.
Omari T, Cock C, Wu P, Szczesniak MM, Schar M, Tack J, et al. Using high resolution manometry impedance to diagnose upper esophageal sphincter and pharyngeal motor disorders. NeurogastroenterolMotil. 2023;35(1): e14461.
Lee T, Park JH, Sohn C, Yoon KJ, Lee YT, Park JH, et al. Failed deglutitive upper esophageal sphincter relaxation is a risk factor for aspiration in stroke patients with oropharyngeal dysphagia. J NeurogastroenterolMotil. 2017;23(1):34–40.
Jiao H, Mei L, Sharma T, Kern M, Sanvanson P, Shaker R. A human model of restricted upper esophageal sphincter opening and its pharyngeal and UES deglutitive pressure phenomena. Am J PhysiolGastrointest Liver Physiol. 2016;311(1):G84-90.
Omari TI, Kritas S, Cock C, Besanko L, Burgstad C, Thompson A, et al. Swallowing dysfunction in healthy older people using pharyngeal pressure-flow analysis. NeurogastroenterolMotil. 2014;26(1):59–68.
Schar M, Woods C, Ooi EH, Athanasiadis T, Ferris L, Szczesniak MM, et al. Pathophysiology of swallowing following oropharyngeal surgery for obstructive sleep apnea syndrome. NeurogastroenterolMotil. 2018;30(5): e13277.
Cock C, Besanko L, Kritas S, Burgstad CM, Thompson A, Heddle R, et al. Maximum upper esophageal sphincter (UES) admittance: a non-specific marker of UES dysfunction. NeurogastroenterolMotil. 2016;28(2):225–33.
Park CH, Lee YT, Yi Y, Lee JS, Park JH, Yoon KJ. Ability of high-resolution manometry to determine feeding method and to predict aspiration pneumonia in patients with dysphagia. Am J Gastroenterol. 2017;112(7):1074–83.
Park D, Oh Y, Ryu JS. Findings of abnormal videofluoroscopic swallowing study identified by high-resolution manometry parameters. Arch Phys Med Rehabil. 2016;97(3):421–8.
Walters RK, Gudipudi R, Davidson S, Nguyen SA, O’Rourke AK. A systematic review of pharyngeal high resolution manometry normative data. [Pending publication].
Jones CA, Meisner EL, Broadfoot CK, Rosen SP, Samuelsen CR, McCulloch TM. Methods for measuring swallowing pressure variability using high-resolution manometry. Front Appl Math Stat. 2018;4:23.
Athukorala RP, Jones RD, Sella O, Huckabee ML. Skill training for swallowing rehabilitation in patients with Parkinson’s disease. Arch Phys Med Rehabil. 2014;95(7):1374–82.
Denk DM, Kaider A. Videoendoscopic biofeedback: a simple method to improve the efficacy of swallowing rehabilitation of patients after head and neck surgery. ORL J OtorhinolaryngolRelat Spec. 1997;59(2):100–5.
Krishnan G, Prasad T. Compensatory strategies and feedback of hyolaryngeal excursion for swallow in treatment of swallowing difficulties in Parkinson’s disease: a case report. J All India Inst Speech Hear. 2013;32.
Winiker K, et al. Potential for behavioural pressure modulation at the upper oesophageal sphincter in healthy swallowing. Dysphagia. 2021;37:763.
Lamvik K, et al. The capacity for volitional control of pharyngeal swallowing in healthy adults. PhysiolBehav. 2015;152:257–63.
Huckabee M-L, Lamvik K, Jones R. Pharyngeal mis-sequencing in dysphagia: characteristics, rehabilitative response, and etiological speculation. J Neurol Sci. 2014;343(1–2):153–8.
Davidson K (Humphries), O’Rourke AK. The utility of high-resolution pharyngeal manometry in dysphagia treatment. Perspectives of the ASHA special interest groups. 2019;4(3):507–16.
Omari TI, Dejaeger E, van Beckevoort D, Goeleven A, Davidson GP, Dent J, et al. A method to objectively assess swallow function in adults with suspected aspiration. Gastroenterology. 2011;140(5):1454–63.
Ghosh SK, Pandolfino JE, Rice J, Clarke JO, Kwiatek M, Kahrilas PJ. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. Am J PhysiolGastrointest Liver Physiol. 2007;293(4):G878-885.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Haley Sibley has nothing to disclose. Kasey Miller reports being a guest lecturer for MUSC’s Speech-Language Pathology program. Kate Davidson reports the following: salary from Medical University of South Carolina; royalties and consulting fees from Northern Speech Services for MBSImP; honorarium from Cincinnati Children’s Hospital for lecture on HRPM. Ashli O’Rourke reports personal fees from Medtronic Inc. and Laborie Medical Inc.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have previously been published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sibley, H., Miller, K., Davidson, K. et al. High-Resolution Pharyngeal Manometry: Recent Developments and Future Directions. Curr Otorhinolaryngol Rep 11, 374–380 (2023). https://doi.org/10.1007/s40136-023-00461-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-023-00461-6