Abstract
Purpose of Review
The aim of this report was to review the recent literature related to the assessment and management of obstructive sleep apnea (OSA) in children under the age of 2 years.
Recent Findings
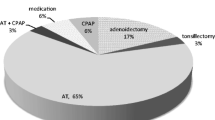
Adenotonsillectomy (AT) indications are changing, with a greater proportion of younger children undergoing AT for OSA. Medical therapies may be an alternative to AT in mild-moderate OSA cases; however, further research is needed. Coblation® intracapsular tonsillectomy may confer benefits in reduced post-operative pain and hemorrhage. Recent concerns regarding the safety of general anesthesia in young children are an important area for further investigation.
Summary
There is a paucity of literature related to OSA in children younger than 2 years. Recent large-scale trials have actively excluded children from this age group and there are no planned studies of this specific population. These children represent a distinct population with differing etiologies, presentations, investigations, and management consideration.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Section on Pediatric Pulmonology SoOSASAAoP. Clinical practice guideline: diagnosis and management of childhood obstructive sleep apnea syndrome.[see comment]. Pediatrics. 2002;109:(4)704–712. https://doi.org/10.1542/peds.109.4.704.
Muzumdar H, Arens R. Physiological effects of obstructive sleep apnea syndrome in childhood. Respir Physiol Neurobiol. 2013;188(3):370–82. https://doi.org/10.1016/j.resp.2013.05.006.
Walter LM, Nixon GM, Davey MJ, O’Driscoll DM, Trinder J, Horne RSC. Sleep disturbance in pre-school children with obstructive sleep apnoea syndrome. Sleep Med. 2011;12(9):880–6. https://doi.org/10.1016/j.sleep.2011.07.007.
Marcus CL. Pathophysiology of childhood obstructive sleep apnea: current concepts. Respir Physiol. 2000;119(2-3):143–54. https://doi.org/10.1016/S0034-5687(99)00109-7.
Shine NP, Coates HL, Lannigan FJ. Obstructive sleep apnea, morbid obesity, and adenotonsillar surgery: a review of the literature. Int J Pediatr Otorhinolaryngol. 2005;69(11):1475–82. https://doi.org/10.1016/j.ijporl.2005.08.008.
Childhood RWPoSPaRCDi. Standards for services for children with disorders of sleep physiology. 2009.
Don DM, Geller KA, Koempel JA, Ward SD. Age specific differences in pediatric obstructive sleep apnea. Int J Pediatr Otorhinolaryngol. 2009;73(7):1025–8. https://doi.org/10.1016/j.ijporl.2009.04.003.
Dickison AE. The normal and abnormal pediatric upper airway. Recognition and management of obstruction. Clin Chest Med. 1987;8(4):583–96.
Swift PG, Emery JL. Clinical observations on response to nasal occlusion in infancy. Arch Dis Child. 1973;48(12):947–51. https://doi.org/10.1136/adc.48.12.947.
Brietzke SE, Katz ES, Roberson DW. Can history and physical examination reliably diagnose pediatric obstructive sleep apnea/hypopnea syndrome? A systematic review of the literature. Otolaryngol Head Neck Surg. 2004;131(6):827–32. https://doi.org/10.1016/j.otohns.2004.07.002.
Moore M, Bonuck K. Comorbid symptoms of sleep-disordered breathing and behavioral sleep problems from 18-57 months of age: a population-based study. Behav Sleep Med. 2013;11(3):222–30. https://doi.org/10.1080/15402002.2012.666219.
Nolan J, Brietzke SE. Systematic review of pediatric tonsil size and polysomnogram-measured obstructive sleep apnea severity. Otolaryngol Head Neck Surg. 2011;144(6):844–50. https://doi.org/10.1177/0194599811400683.
Tang A, Benke JR, Cohen AP, Ishman SL. Influence of tonsillar size on OSA improvement in children undergoing adenotonsillectomy. Otolaryngol Head Neck Surg. 2015;153(2):281–5. https://doi.org/10.1177/0194599815583459.
Qubty WF, Mrelashvili A, Kotagal S, Lloyd RM. Comorbidities in infants with obstructive sleep apnea. J Clin Sleep Med. 2014;10(11):1213–6. https://doi.org/10.5664/jcsm.4204.
Tan HL, Kheirandish-Gozal L, Abel F, Gozal D. Craniofacial syndromes and sleep-related breathing disorders. Sleep Med Rev. 2016;27:74–88. https://doi.org/10.1016/j.smrv.2015.05.010.
Garcia J, Wical B, Wical W, Schaffer L, Wical T, Wendorf H, et al. Obstructive sleep apnea in children with cerebral palsy and epilepsy. Dev Med Child Neurol. 2016;58(10):1057–62. https://doi.org/10.1111/dmcn.13091.
Dinwiddie R. Congenital upper airway obstruction. Paediatr Respir Rev. 2004;5(1):17–24. https://doi.org/10.1016/j.prrv.2003.10.001.
Rastatter JC, Schroeder JW Jr, French A, Holinger L. Synchronous airway lesions in children younger than age 3 years undergoing adenotonsillectomy. Otolaryngol Head Neck Surg. 2011;145(2):309–13. https://doi.org/10.1177/0194599811403071.
Daar G, Sari K, Gencer ZK, et al. The relation between childhood obesity and adenotonsillar hypertrophy. Eur Arch Otorhinolaryngol. 2016;273(2):505–9. https://doi.org/10.1007/s00405-015-3554-4.
Lam YY, Chan EY, Ng DK, et al. The correlation among obesity, apnea-hypopnea index, and tonsil size in children. Chest. 2006;130(6):1751–6. https://doi.org/10.1378/chest.130.6.1751.
Kang KT, Chou CH, Weng WC, Lee PL, Hsu WC. Associations between adenotonsillar hypertrophy, age, and obesity in children with obstructive sleep apnea. PLoS One. 2013;8(10):e78666. https://doi.org/10.1371/journal.pone.0078666.
Xu Z, Jiaqing A, Yuchuan L, Shen K. A case-control study of obstructive sleep apnea-hypopnea syndrome in obese and nonobese chinese children. Chest. 2008;133(3):684–9. https://doi.org/10.1378/chest.07-1611.
Coles N, Birken C, Hamilton J. Emerging treatments for severe obesity in children and adolescents. BMJ. 2016;354:i4116.
Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288(14):1723–7. https://doi.org/10.1001/jama.288.14.1723.
Gittner LS, Ludington-Hoe SM, Haller HS. Infant obesity and severe obesity growth patterns in the first two years of life. Matern Child Health J. 2014;18(3):613–24. https://doi.org/10.1007/s10995-013-1285-y.
• Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–14. Good overview of the impact of childhood obesity. https://doi.org/10.1001/jama.2014.732.
Costa DJ, Mitchell R. Adenotonsillectomy for obstructive sleep apnea in obese children: a meta-analysis. Otolaryngol Head Neck Surg. 2009;140(4):455–60. https://doi.org/10.1016/j.otohns.2008.12.038.
Imanguli M, Ulualp SO. Risk factors for residual obstructive sleep apnea after adenotonsillectomy in children. Laryngoscope. 2016;126(11):2624–9. https://doi.org/10.1002/lary.25979.
Brouillette RT, Morielli A, Leimanis A, Waters KA, Luciano R, Ducharme FM. Nocturnal pulse oximetry as an abbreviated testing modality for pediatric obstructive sleep apnea. Pediatrics. 2000;105(2):405–12. https://doi.org/10.1542/peds.105.2.405.
Walter LM, Nixon GM, Davey MJ, Anderson V, Trinder J, Walker A, et al. Differential effects of sleep disordered breathing on polysomnographic characteristics in preschool and school aged children. Sleep Med. 2012;13(7):810–5. https://doi.org/10.1016/j.sleep.2012.03.014.
DeHaan KL, Seton C, Fitzgerald DA, Waters KA, MacLean JE. Polysomnography for the diagnosis of sleep disordered breathing in children under 2 years of age. Pediatr Pulmonol. 2015;50(12):1346–53. https://doi.org/10.1002/ppul.23169.
Barnes ME, Gozal D, Molfese DL. Attention in children with obstructive sleep apnoea: an event-related potentials study. Sleep Med. 2012;13(4):368–77. https://doi.org/10.1016/j.sleep.2011.06.007.
Persak SC, Sin S, McDonough JM, Arens R, Wootton DM. Noninvasive estimation of pharyngeal airway resistance and compliance in children based on volume-gated dynamic MRI and computational fluid dynamics. J Appl Physiol. 2011;111(6):1819–27. https://doi.org/10.1152/japplphysiol.01230.2010.
Bani MMM, Az-Zaqah R, Aldofash AK, et al. Contactless method for detection of infant sleep apnoea. J Med Eng Technol. 2010;34(5-6):324–8. https://doi.org/10.3109/03091902.2010.481034.
Revenaugh PC, Chmielewski LJ, Edwards T, Krishna J, Krakovitz P, Anne S. Utility of preoperative cardiac evaluation in pediatric patients undergoing surgery for obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 2011;137(12):1269–75. https://doi.org/10.1001/archoto.2011.208.
Section on Pediatric Pulmonology SoOSASAAoP. Clinical practice guideline: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2002;109:704–12.
Goldberg S, Shatz A, Picard E, Wexler I, Schwartz S, Swed E, et al. Endoscopic findings in children with obstructive sleep apnea: effects of age and hypotonia. Pediatr Pulmonol. 2005;40(3):205–10. https://doi.org/10.1002/ppul.20230.
Lin AC, Koltai PJ. Sleep endoscopy in the evaluation of pediatric obstructive sleep apnea. Int J Pediatr. 2012;2012:576719.
Durr ML, Meyer AK, Kezirian EJ, Rosbe KW. Drug-induced sleep endoscopy in persistent pediatric sleep-disordered breathing after adenotonsillectomy. Arch Otolaryngol Head Neck Surg. 2012;138(7):638–43. https://doi.org/10.1001/archoto.2012.1067.
Marcus CL, Radcliffe J, Konstantinopoulou S, Beck SE, Cornaglia MA, Traylor J, et al. Effects of positive airway pressure therapy on neurobehavioral outcomes in children with obstructive sleep apnea. Am J Respir Crit Care Med. 2012;185(9):998–1003. https://doi.org/10.1164/rccm.201112-2167OC.
Simon SL, Duncan CL, Janicke DM, Wagner MH. Barriers to treatment of paediatric obstructive sleep apnoea: development of the adherence barriers to continuous positive airway pressure (CPAP) questionnaire. Sleep Med. 2012;13(2):172–7. https://doi.org/10.1016/j.sleep.2011.10.026.
Marcus CL, Beck SE, Traylor J, et al. Randomized, double-blind clinical trial of two different modes of positive airway pressure therapy on adherence and efficacy in children. J Clin Sleep Med. 2012;8(1):37–42. https://doi.org/10.5664/jcsm.1656.
Downey R 3rd, Perkin RM, MacQuarrie J. Nasal continuous positive airway pressure use in children with obstructive sleep apnea younger than 2 years of age. Chest. 2000;117(6):1608–12. https://doi.org/10.1378/chest.117.6.1608.
Miller MJ, Carlo WA, Martin RJ. Continuous positive airway pressure selectively reduces obstructive apnea in preterm infants. J Pediatr. 1985;106(1):91–4. https://doi.org/10.1016/S0022-3476(85)80475-3.
McNamara F, Sullivan CE. Effects of nasal CPAP therapy on respiratory and spontaneous arousals in infants with OSA. J Appl Physiol (1985). 1999;87(3):889–96. https://doi.org/10.1152/jappl.1999.87.3.889.
Verhulst SL, Franckx H, Van Gaal L, de Backer W, Desager K. The effect of weight loss on sleep-disordered breathing in obese teenagers. Obesity (Silver Spring). 2009;17(6):1178–83. https://doi.org/10.1038/oby.2008.673.
Van K, Franckx H, Debode P, et al. Weight loss and sleep-disordered breathing in childhood obesity: effects on inflammation and uric acid. Obesity. 2012;20:172–7.
Kuhle S, Urschitz MS. Anti-inflammatory medications for obstructive sleep apnea in children. Cochrane Database Syst Rev. 2011; https://doi.org/10.1002/14651858.CD007074.pub2.
Kheirandish-Gozal L, Bandla HP, Gozal D. Montelukast for children with obstructive sleep apnea: results of a double-blind, randomized, placebo-controlled trial. Ann Am Thorac Soc. 2016;13(10):1736–41. https://doi.org/10.1513/AnnalsATS.201606-432OC.
Goldbart AD, Greenberg-Dotan S, Tal A. Montelukast for children with obstructive sleep apnea: a double-blind, placebo-controlled study. Pediatrics. 2012;130(3):e575–80. https://doi.org/10.1542/peds.2012-0310.
Kheirandish-Gozal L, Bhattacharjee R, Bandla HPR, Gozal D. Antiinflammatory therapy outcomes for mild OSA in children. Chest. 2014;146(1):88–95. https://doi.org/10.1378/chest.13-2288.
Czinn SJ, Blanchard S. Gastroesophageal reflux disease in neonates and infants: when and how to treat. Paediatr Drugs. 2013;15(1):19–27. https://doi.org/10.1007/s40272-012-0004-2.
Wasilewska J, Semeniuk J, Cudowska B, Klukowski M, Dębkowska K, Kaczmarski M. Respiratory response to proton pump inhibitor treatment in children with obstructive sleep apnea syndrome and gastroesophageal reflux disease. Sleep Med. 2012;13(7):824–30. https://doi.org/10.1016/j.sleep.2012.04.016.
Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130(3):e714–55. https://doi.org/10.1542/peds.2012-1672.
Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Rep. 2009:1–25.
Hultcrantz E, Ericsson E. Factors influencing the indication for tonsillectomy: a historical overview and current concepts. ORL J Otorhinolaryngol Relat Spec. 2013;75(3):184–91. https://doi.org/10.1159/000342322.
Borgstrom A, Nerfeldt P, Friberg D, et al. Trends and changes in paediatric tonsil surgery in Sweden 1987-2013: a population-based cohort study. BMJ Open. 2017;7:e013346.
Patel HH, Straight CE, Lehman EB, et al. Indications for tonsillectomy: a 10 year retrospective review. Int J Pediatr Otorhinolaryngol. 2014;78(12):2151–5. https://doi.org/10.1016/j.ijporl.2014.09.030.
Parker NP, Walner DL. Trends in the indications for pediatric tonsillectomy or adenotonsillectomy. Int J Pediatr Otorhinolaryngol. 2011;75(2):282–5. https://doi.org/10.1016/j.ijporl.2010.11.019.
Venekamp RP, Hearne BJ, Chandrasekharan D et al. Tonsillectomy or adenotonsillectomy versus non-surgical management for obstructive sleep-disordered breathing in children. Cochrane Database Syst Rev. 2015:CD011165.
Marcus CL, Moore RH, Rosen CL, et al. A randomized trial of adenotonsillectomy for childhood sleep apnea. N Engl J Med. 2013;368(25):2366–76. https://doi.org/10.1056/NEJMoa1215881.
Redline S, Amin R, Beebe D, Chervin RD, Garetz SL, Giordani B, et al. The Childhood Adenotonsillectomy Trial (CHAT): rationale, design, and challenges of a randomized controlled trial evaluating a standard surgical procedure in a pediatric population. Sleep. 2011;34(11):1509–17. https://doi.org/10.5665/sleep.1388.
Sudarsan SS, Paramasivan VK, Arumugam SV, Murali S, Kameswaran M. Comparison of treatment modalities in syndromic children with obstructive sleep apnea—a randomized cohort study. Int J Pediatr Otorhinolaryngol. 2014;78(9):1526–33. https://doi.org/10.1016/j.ijporl.2014.06.027.
Goldstein NA, Pugazhendhi V, Rao SM, Weedon J, Campbell TF, Goldman AC, et al. Clinical assessment of pediatric obstructive sleep apnea. Pediatrics. 2004;114(1):33–43. https://doi.org/10.1542/peds.114.1.33.
Cheng J, Elden L. Outcomes in children under 12 months of age undergoing adenotonsillectomy for sleep-disordered breathing. Laryngoscope. 2013;123(9):2281–4. https://doi.org/10.1002/lary.23796.
Acevedo JL, Shah RK, Brietzke SE. Systematic review of complications of tonsillotomy versus tonsillectomy. Otolaryngol Head Neck Surg. 2012;146(6):871–9. https://doi.org/10.1177/0194599812439017.
•• Hoey AW, Foden NM, Hadjisymeou Andreou S, Noonan F, Chowdhury AK, Greig SR, et al. Coblation(R) intracapsular tonsillectomy (tonsillotomy) in children: a prospective study of 500 consecutive cases with long-term follow-up. Clin Otolaryngol. 2017. Important large study of Coblation intracapsular tonsillectomy in chidren.;42(6):1211–7. https://doi.org/10.1111/coa.12849.
Lowe D, van der Meulen J, Cromwell D, et al. Key messages from the National Prospective Tonsillectomy Audit. Laryngoscope. 2007;117:717–24.
Shah UK, Theroux Z, Shah GB, et al. Resource analysis of tonsillectomy in children. Laryngoscope. 2014;124(5):1223–8. https://doi.org/10.1002/lary.24388.
Marino A, Ranieri R, Chiarotti F, et al. Rapid maxillary expansion in children with obstructive sleep apnoea syndrome (OSAS). Eur J Paediatr Dent. 2012;13:57–63.
Kadouch DJ, Maas SM, Dubois L, van der Horst CM. Surgical treatment of macroglossia in patients with Beckwith-Wiedemann syndrome: a 20-year experience and review of the literature. Int J Oral Maxillofac Surg. 2012;41(3):300–8. https://doi.org/10.1016/j.ijom.2011.10.021.
Sisson TR, Whalen LE, Telek A. The blood volume of infants. II. The premature infant during the first year of life. J Pediatr. 1959;55:430–46.
Windfuhr JP. Serious complications following tonsillectomy: how frequent are they really? ORL J Otorhinolaryngol Relat Spec. 2013;75:166–73.
• Andropoulos DB, Greene MF. Anesthesia and developing brains—implications of the FDA warning. N Engl J Med. 2017;376(10):905–7. Good overview of the current understanding of general anesthesia exposure and neurocognitive outcomes. https://doi.org/10.1056/NEJMp1700196.
Armstrong R, Xu F, Arora A, Rasic N, Syed NI. General anesthetics and cytotoxicity: possible implications for brain health. Drug Chem Toxicol. 2017;40(2):241–9. https://doi.org/10.1080/01480545.2016.1188306.
Fodale V, Tripodi VF, Penna O, Famà F, Squadrito F, Mondello E, et al. An update on anesthetics and impact on the brain. Expert Opin Drug Saf. 2017;16(9):997–1008. https://doi.org/10.1080/14740338.2017.1351539.
Rappaport BA, Suresh S, Hertz S, et al. Anesthetic neurotoxicity—clinical implications of animal models. N Engl J Med. 2015;372:796–7.
•• Sun LS, Li G, Miller TL, et al. Association between a single general anesthesia exposure before age 36 months and neurocognitive outcomes in later childhood. JAMA. 2016;315:2312–20. Important, recent. well-designed study investigating the effect of general anesthesia exposure before 36 months and neurocognitive outcomes.
Mann GE, Kahana M. The uncomfortable reality ... We simply do not know if general anesthesia negatively impacts the neurocognitive development of our small children. Int J Pediatr Otorhinolaryngol. 2015;79(9):1379–81. https://doi.org/10.1016/j.ijporl.2015.05.011.
Sanders RD, Hassell J, Davidson AJ, et al. Impact of anaesthetics and surgery on neurodevelopment: an update. Br J Anaesth. 2013;110(Suppl 1):i53–72.
Youshani AS, Thomas L, Sharma RK. Day case tonsillectomy for the treatment of obstructive sleep apnoea syndrome in children: Alder Hey experience. Int J Pediatr Otorhinolaryngol. 2011;75(2):207–10. https://doi.org/10.1016/j.ijporl.2010.10.036.
ME MC, Sheyn A, Haupert M, et al. Predicting complications after adenotonsillectomy in children 3 years old and younger. Int J Pediatr Otorhinolaryngol. 2011;75:1391–4.
Waters KA, Chawla J, Harris MA, et al. Rationale for and design of the “POSTA” study: evaluation of neurocognitive outcomes after immediate adenotonsillectomy compared to watchful waiting in preschool children. BMC Pediatr. 2017;17:47.
Primhak R, Kingshott R. Sleep physiology and sleep-disordered breathing: the essentials. Arch Dis Child. 2012;97(1):54–8. https://doi.org/10.1136/adc.2010.186676.
Ramgopal S, Kothare SV, Rana M, Singh K, Khatwa U. Obstructive sleep apnea in infancy: a 7-year experience at a pediatric sleep center. Pediatr Pulmonol. 2014;49(6):554–60. https://doi.org/10.1002/ppul.22867.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pediatric Otolaryngology
Rights and permissions
About this article
Cite this article
Powell, J., Powell, S. Obstructive Sleep Apnea in the Very Young. Curr Otorhinolaryngol Rep 6, 48–55 (2018). https://doi.org/10.1007/s40136-018-0184-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-018-0184-6