Abstract
Purpose of Review
In this article, we define the ocular surface microbiome (OSM) and review the literature investigating its putative role in anterior segment diseases.
Recent Findings
The complex networks of microorganisms that compose the OSM play integral roles in many physiologic processes. The three most common bacterial phyla that contribute to the microbiome are Proteobacteria, Firmicutes, and Actinobacteria, although the composition has been found to vary by anatomic site, age, and systemic disease. Multiple ocular conditions have definitive associations with OSM alterations, some with specific signature colonization of atypical genera or species, while others have more broad changes in abundance or alpha diversity of natural microbiota.
Summary
Dysbiosis of the OSM appears to play a role in multiple ocular surface and anterior segment diseases. Future larger, longitudinal, and multicentered studies investigating its composition will lend insight into the pathophysiology of disease and potential methods for therapeutic interventions.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
• Doan T, Akileswaran L, Andersen D, Johnson B, Ko N, Shrestha A, et al. Paucibacterial microbiome and resident DNA virome of the healthy conjunctiva. Invest Ophthalmol Vis Sci. 2016;57(13):5116–26. https://doi.org/10.1167/iovs.16-19803. Conjunctival swabs from over 100 healthy volunteers were analyzed by culture, 16S sequencing and biome representational in silico karyotyping, along with swabs from facial skin, buccal mucosa and controls from the environment. The authors found a paucibacterial, distinct conjunctival bacterial community when compared with the facial skin, buccal mucosa and controls.
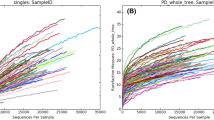
• Ozkan J, Nielsen S, Diez-Vives C, Coroneo M, Thomas T, Willcox M. Temporal stability and composition of the ocular surface microbiome. Sci Rep. 2017;7(1):9880. https://doi.org/10.1038/s41598-017-10494-9. The study identified the composion of the resident ocular surface micrbiome in a healthy population at baseline and then at 1 month and 3 months to asses for change over time. They found that the ocular surface microbiome overall has low diveristy and does not appear to have a core composition, although the microbiome appears specific to an individual.
Kang Y, Lin S, Ma X, Che Y, Chen Y, Wan T, et al. Strain heterogeneity, cooccurrence network, taxonomic composition and functional profile of the healthy ocular surface microbiome. Eye Vis (Lond). 2021;8(1):6. https://doi.org/10.1186/s40662-021-00228-4.
Matysiak A, Kabza M, Karolak JA, Jaworska MM, Rydzanicz M, Ploski R, et al. Characterization of ocular surface microbial profiles revealed discrepancies between conjunctival and corneal microbiota. Pathogens. 2021;10(4):405. https://doi.org/10.3390/pathogens10040405.
Suzuki T, Sutani T, Nakai H, Shirahige K, Kinoshita S. The microbiome of the meibum and ocular surface in healthy subjects. Invest Ophthalmol Vis Sci. 2020;61(2):18. https://doi.org/10.1167/iovs.61.2.18.
Wen X, Miao L, Deng Y, Bible PW, Hu X, Zou Y, et al. The influence of age and sex on ocular surface microbiota in healthy adults. Invest Ophthalmol Vis Sci. 2017;58(14):6030–7. https://doi.org/10.1167/iovs.17-22957.
Katzka W, Dong TS, Luu K, Lagishetty V, Sedighian F, Arias-Jayo N, et al. The ocular microbiome is altered by sampling modality and age. Transl Vis Sci Technol. 2021;10(12):24. https://doi.org/10.1167/tvst.10.12.24.
Cavuoto KM, Mendez R, Miller D, Galor A, Banerjee S. Effect of clinical parameters on the ocular surface microbiome in children and adults. Clin Ophthalmol. 2018;12:1189–97. https://doi.org/10.2147/OPTH.S166547.
Cavuoto KM, Banerjee S, Miller D, Galor A. Composition and comparison of the ocular surface microbiome in infants and older children. Transl Vis Sci Technol. 2018;7(6):16. https://doi.org/10.1167/tvst.7.6.16.
Ozkan J, Coroneo M, Willcox M, Wemheuer B, Thomas T. Identification and visualization of a distinct microbiome in ocular surface conjunctival tissue. Invest Ophthalmol Vis Sci. 2018;59(10):4268–76. https://doi.org/10.1167/iovs.18-24651.
Ozkan J, Willcox M, Wemheuer B, Wilcsek G, Coroneo M, Thomas T. Biogeography of the human ocular microbiota. Ocul Surf. 2019;17(1):111–8. https://doi.org/10.1016/j.jtos.2018.11.005.
Cavuoto KM, Galor A, Banerjee S. Anatomic characterization of the ocular surface microbiome in children. Microorganisms. 2019;7(8):259. https://doi.org/10.3390/microorganisms7080259.
Andersson J, Vogt JK, Dalgaard MD, Pedersen O, Holmgaard K, Heegaard S. Ocular surface microbiota in contact lens users and contact-lens-associated bacterial keratitis. Vision (Basel). 2021;5(2):27. https://doi.org/10.3390/vision5020027.
Zhang H, Zhao F, Hutchinson DS, Sun W, Ajami NJ, Lai S, et al. Conjunctival microbiome changes associated with soft contact lens and orthokeratology lens wearing. Invest Ophthalmol Vis Sci. 2017;58(1):128–36. https://doi.org/10.1167/iovs.16-20231.
Retuerto MA, Szczotka-Flynn L, Mukherjee PK, Debanne S, Iyengar SK, Richardson B, et al. Diversity of ocular surface bacterial microbiome adherent to worn contact lenses and bacterial communities associated with care solution use. Eye Contact Lens. 2019;45(5):331–9. https://doi.org/10.1097/ICL.0000000000000578.
Doan T, Hinterwirth A, Worden L, Arzika AM, Maliki R, Chen C, et al. Post-antibiotic ocular surface microbiome in children: a cluster-randomized trial. Ophthalmology. 2020;127(8):1127–30. https://doi.org/10.1016/j.ophtha.2020.02.014.
Ham B, Hwang HB, Jung SH, Chang S, Kang KD, Kwon MJ. Distribution and diversity of ocular microbial communities in diabetic patients compared with healthy subjects. Curr Eye Res. 2018;43(3):314–24. https://doi.org/10.1080/02713683.2017.1406528.
Li S, Yi G, Peng H, Li Z, Chen S, Zhong H, et al. How ocular surface microbiota debuts in type 2 diabetes mellitus. Front Cell Infect Microbiol. 2019;9:202. https://doi.org/10.3389/fcimb.2019.00202.
Zhu X, Wei L, Rong X, Zhang Y, Zhang Q, Wen X, et al. Conjunctival microbiota in patients with type 2 diabetes mellitus and influences of perioperative use of topical levofloxacin in ocular surgery. Front Med (Lausanne). 2021;8:605639. https://doi.org/10.3389/fmed.2021.605639.
St Leger AJ, Desai JV, Drummond RA, Kugadas A, Almaghrabi F, Silver P, et al. An ocular commensal protects against corneal infection by driving an interleukin-17 response from mucosal gammadelta T cells. Immunity. 2017;47(1):148-58 e5. https://doi.org/10.1016/j.immuni.2017.06.014.
Ueta M, Kinoshita S. Innate immunity of the ocular surface. Brain Res Bull. 2010;81(2–3):219–28. https://doi.org/10.1016/j.brainresbull.2009.10.001.
Cavuoto KM, Banerjee S, Galor A. Relationship between the microbiome and ocular health. Ocul Surf. 2019;17(3):384–92. https://doi.org/10.1016/j.jtos.2019.05.006.
Ozkan J, Willcox MD. The ocular microbiome: molecular characterisation of a unique and low microbial environment. Curr Eye Res. 2019;44(7):685–94. https://doi.org/10.1080/02713683.2019.1570526.
Gomes JAP, Frizon L, Demeda VF. Ocular surface microbiome in health and disease. Asia Pac J Ophthalmol (Phila). 2020;9(6):505–11. https://doi.org/10.1097/APO.0000000000000330.
Watters GA, Turnbull PR, Swift S, Petty A, Craig JP. Ocular surface microbiome in Meibomian gland dysfunction. Clin Exp Ophthalmol. 2017;45(2):105–11. https://doi.org/10.1111/ceo.12810.
Dong X, Wang Y, Wang W, Lin P, Huang Y. Composition and diversity of bacterial community on the ocular surface of patients with Meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2019;60(14):4774–83. https://doi.org/10.1167/iovs.19-27719.
Jiang X, Deng A, Yang J, Bai H, Yang Z, Wu J, et al. Pathogens in the Meibomian gland and conjunctival sac: microbiome of normal subjects and patients with Meibomian gland dysfunction. Infect Drug Resist. 2018;11:1729–40. https://doi.org/10.2147/IDR.S162135.
Zhao F, Zhang D, Ge C, Zhang L, Reinach PS, Tian X, et al. Metagenomic profiling of ocular surface microbiome changes in Meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2020;61(8):22. https://doi.org/10.1167/iovs.61.8.22.
Lee SH, Oh DH, Jung JY, Kim JC, Jeon CO. Comparative ocular microbial communities in humans with and without blepharitis. Invest Ophthalmol Vis Sci. 2012;53(9):5585–93. https://doi.org/10.1167/iovs.12-9922.
Wang C, Dou X, Li J, Wu J, Cheng Y, An N. Composition and diversity of the ocular surface microbiota in patients with blepharitis in northwestern China. Front Med (Lausanne). 2021;8:768849. https://doi.org/10.3389/fmed.2021.768849.
Yan Y, Yao Q, Lu Y, Shao C, Sun H, Li Y, et al. Association between demodex infestation and ocular surface microbiota in patients with demodex blepharitis. Front Med (Lausanne). 2020;7:592759. https://doi.org/10.3389/fmed.2020.592759.
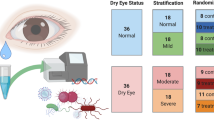
Andersson J, Vogt JK, Dalgaard MD, Pedersen O, Holmgaard K, Heegaard S. Ocular surface microbiota in patients with aqueous tear-deficient dry eye. Ocul Surf. 2021;19:210–7. https://doi.org/10.1016/j.jtos.2020.09.003.
Graham JE, Moore JE, Jiru X, Moore JE, Goodall EA, Dooley JS, et al. Ocular pathogen or commensal: a PCR-based study of surface bacterial flora in normal and dry eyes. Invest Ophthalmol Vis Sci. 2007;48(12):5616–23. https://doi.org/10.1167/iovs.07-0588.
Li Z, Gong Y, Chen S, Li S, Zhang Y, Zhong H, et al. Comparative portrayal of ocular surface microbe with and without dry eye. J Microbiol. 2019;57(11):1025–32. https://doi.org/10.1007/s12275-019-9127-2.
Liang Q, Li J, Zou Y, Hu X, Deng X, Zou B, et al. Metagenomic analysis reveals the heterogeneity of conjunctival microbiota dysbiosis in dry eye disease. Front Cell Dev Biol. 2021;9:731867. https://doi.org/10.3389/fcell.2021.731867.
• Willis KA, Postnikoff CK, Freeman A, Rezonzew G, Nichols K, Gaggar A, et al. The closed eye harbours a unique microbiome in dry eye disease. Sci Rep. 2020;10(1):12035. https://doi.org/10.1038/s41598-020-68952-w. This randomized control trial demonstrated a distinct microbiome signature in closed eyes of chronic dry eye patients compared to healthy controls, and showed these differences remain stable despite daily eye wash over a 1 month period. The authors further applied machine learning over the course of the study to identify specific bacteria genera that could function as biomarkers for chronic dry eye patients.
Qi Y, Wan Y, Li T, Zhang M, Song Y, Hu Y, et al. Comparison of the ocular microbiomes of dry eye patients with and without autoimmune disease. Front Cell Infect Microbiol. 2021;11:716867. https://doi.org/10.3389/fcimb.2021.716867.
Song H, Xiao K, Chen Z, Long Q. Analysis of conjunctival sac microbiome in dry eye patients with and without Sjogren’s syndrome. Front Med (Lausanne). 2022;9:841112. https://doi.org/10.3389/fmed.2022.841112.
Kim YC, Ham B, Kang KD, Yun JM, Kwon MJ, Kim HS, et al. Bacterial distribution on the ocular surface of patients with primary Sjogren’s syndrome. Sci Rep. 2022;12(1):1715. https://doi.org/10.1038/s41598-022-05625-w.
Song HY, Qiu BF, Liu C, Zhu SX, Wang SC, Miao J, et al. Identification of causative pathogens in mouse eyes with bacterial keratitis by sequence analysis of 16S rDNA libraries. Exp Anim. 2015;64(1):49–56. https://doi.org/10.1538/expanim.14-0046.
Shivaji S, Jayasudha R, Chakravarthy SK, SaiAbhilash CR, Sai Prashanthi G, Sharma S, et al. Alterations in the conjunctival surface bacterial microbiome in bacterial keratitis patients. Exp Eye Res. 2021;203:108418. https://doi.org/10.1016/j.exer.2020.108418.
Ren Z, Liu Q, Li W, Wu X, Dong Y, Huang Y. Profiling of diagnostic information of and latent susceptibility to bacterial keratitis from the perspective of ocular bacterial microbiota. Front Cell Infect Microbiol. 2021;11:645907. https://doi.org/10.3389/fcimb.2021.645907.
• Ren Z, Li W, Liu Q, Dong Y, Huang Y. Profiling of the conjunctival bacterial microbiota reveals the feasibility of utilizing a microbiome-based machine learning model to differentially diagnose microbial keratitis and the core components of the conjunctival bacterial interaction network. Front Cell Infect Microbiol. 2022;12:860370. https://doi.org/10.3389/fcimb.2022.860370. This prospective cohort study of a fairly large population of various forms microbial keratitis (MK) is the first to apply machine learning to show the feasibility of distinguishing different MK etiologies based on utilizing unique features of the conjunctival bacterial microbiome as biomarkers.
Kang Y, Zhang H, Hu M, Ma Y, Chen P, Zhao Z, et al. Alterations in the ocular surface microbiome in traumatic corneal ulcer patients. Invest Ophthalmol Vis Sci. 2020;61(6):35. https://doi.org/10.1167/iovs.61.6.35.
Cavuoto KM, Galor A, Banerjee S. Ocular surface microbiome alterations are found in both eyes of individuals with unilateral infectious keratitis. Transl Vis Sci Technol. 2021;10(2):19. https://doi.org/10.1167/tvst.10.2.19.
Ge C, Wei C, Yang BX, Cheng J, Huang YS. Conjunctival microbiome changes associated with fungal keratitis: metagenomic analysis. Int J Ophthalmol. 2019;12(2):194–200. https://doi.org/10.18240/ijo.2019.02.02.
Zhou Y, Holland MJ, Makalo P, Joof H, Roberts CH, Mabey DC, et al. The conjunctival microbiome in health and trachomatous disease: a case control study. Genome Med. 2014;6(11):99. https://doi.org/10.1186/s13073-014-0099-x.
Pickering H, Palmer CD, Houghton J, Makalo P, Joof H, Derrick T, et al. Conjunctival microbiome-host responses are associated with impaired epithelial cell health in both early and late stages of trachoma. Front Cell Infect Microbiol. 2019;9:297. https://doi.org/10.3389/fcimb.2019.00297.
Yau JW, Hou J, Tsui SKW, Leung TF, Cheng NS, Yam JC, et al. Characterization of ocular and nasopharyngeal microbiome in allergic rhinoconjunctivitis. Pediatr Allergy Immunol. 2019;30(6):624–31. https://doi.org/10.1111/pai.13088.
Liang Q, Li J, Zhang S, Liao Y, Guo S, Liang J, et al. Characterization of conjunctival microbiome dysbiosis associated with allergic conjunctivitis. Allergy. 2021;76(2):596–600. https://doi.org/10.1111/all.14635.
Inada N, Shoji J, Harata G, Miyazawa K, He F, Tomioka A, et al. Dysbiosis of ocular surface microbiota in patients with refractive allergic conjunctival diseases. Cornea. 2021. https://doi.org/10.1097/ICO.0000000000002940.
Leonardi A, Modugno RL, Cavarzeran F, Rosani U. Metagenomic analysis of the conjunctival bacterial and fungal microbiome in vernal keratoconjunctivitis. Allergy. 2021;76(10):3215–7. https://doi.org/10.1111/all.14963.
Vishwakarma P, Mitra S, Beuria T, Barik MR, Sahu SK. Comparative profile of ocular surface microbiome in vernal keratoconjunctivitis patients and healthy subjects. Graefes Arch Clin Exp Ophthalmol. 2021;259(7):1925–33. https://doi.org/10.1007/s00417-021-05109-z.
Liborio AM, Nishiwaki-Dantas MC, Mimica LM, Dantas PE, Lima AL. Conjunctival microbiota in patients with ocular allergy. Arq Bras Oftalmol. 2005;68(6):824–7. https://doi.org/10.1590/s0004-27492005000600020.
Kittipibul T, Puangsricharern V, Chatsuwan T. Comparison of the ocular microbiome between chronic Stevens-Johnson syndrome patients and healthy subjects. Sci Rep. 2020;10(1):4353. https://doi.org/10.1038/s41598-020-60794-w.
Kittipibul T, Puangsricharern V. The ocular microbiome in Stevens-Johnson syndrome. Front Med (Lausanne). 2021;8:645053. https://doi.org/10.3389/fmed.2021.645053.
Moon J, Lee Y, Yoon CH, Kim MK. Matrix metalloproteinase 9 is associated with conjunctival microbiota culture positivity in Korean patients with chronic Stevens-Johnson syndrome. BMC Ophthalmol. 2022;22(1):179. https://doi.org/10.1186/s12886-022-02406-x.
Ueta M, Hosomi K, Park J, Mizuguchi K, Sotozono C, Kinoshita S, et al. Categorization of the ocular microbiome in Japanese Stevens-Johnson syndrome patients with severe ocular complications. Front Cell Infect Microbiol. 2021;11:741654. https://doi.org/10.3389/fcimb.2021.741654.
Zilliox MJ, Gange WS, Kuffel G, Mores CR, Joyce C, de Bustros P, et al. Assessing the ocular surface microbiome in severe ocular surface diseases. Ocul Surf. 2020;18(4):706–12. https://doi.org/10.1016/j.jtos.2020.07.007.
Shimizu E, Ogawa Y, Saijo Y, Yamane M, Uchino M, Kamoi M, et al. Commensal microflora in human conjunctiva; characteristics of microflora in the patients with chronic ocular graft-versus-host disease. Ocul Surf. 2019;17(2):265–71. https://doi.org/10.1016/j.jtos.2019.02.001.
Li J, Liang Q, Huang F, Liao Y, Zhao W, Yang J, et al. Metagenomic profiling of the ocular surface microbiome in patients after allogeneic hematopoietic stem cell transplantation: ocular surface microbial dysbiosis and oGVHD. Am J Ophthalmol. 2022. https://doi.org/10.1016/j.ajo.2022.04.026.
Baim AD, Movahedan A, Farooq AV, Skondra D. The microbiome and ophthalmic disease. Exp Biol Med (Maywood). 2019;244(6):419–29. https://doi.org/10.1177/1535370218813616.
Astafurov K, Elhawy E, Ren L, Dong CQ, Igboin C, Hyman L, et al. Oral microbiome link to neurodegeneration in glaucoma. PLoS ONE. 2014;9(9):e104416. https://doi.org/10.1371/journal.pone.0104416.
Lim SH, Shin JH, Lee JW, Lee Y, Seo JH. Differences in the eyelid and buccal microbiome of glaucoma patients receiving long-term administration of prostaglandin analog drops. Graefes Arch Clin Exp Ophthalmol. 2021;259(10):3055–65. https://doi.org/10.1007/s00417-021-05218-9.
Ohtani S, Shimizu K, Nejima R, Kagaya F, Aihara M, Iwasaki T, et al. Conjunctival bacteria flora of glaucoma patients during long-term administration of prostaglandin analog drops. Invest Ophthalmol Vis Sci. 2017;58(10):3991–6. https://doi.org/10.1167/iovs.16-20853.
Shin JH, Lee JW, Lim SH, Yoon BW, Lee Y, Seo JH. The microbiomes of the eyelid and buccal area of patients with uveitic glaucoma. BMC Ophthalmol. 2022;22(1):170. https://doi.org/10.1186/s12886-022-02395-x.
Miller D, Iovieno A. The role of microbial flora on the ocular surface. Curr Opin Allergy Clin Immunol. 2009;9(5):466–70. https://doi.org/10.1097/ACI.0b013e3283303e1b.
Asao K, Hashida N, Ando S, Motooka D, Kurakami H, Nakamura S, et al. Conjunctival dysbiosis in mucosa-associated lymphoid tissue lymphoma. Sci Rep. 2019;9(1):8424. https://doi.org/10.1038/s41598-019-44861-5.
Rodriguez-Fernandez CA, Iglesias MB, de Domingo B, Conde-Perez K, Vallejo JA, Rodriguez-Martinez L, et al. Microbiome in immune-mediated uveitis. Int J Mol Sci. 2022;23(13):7020. https://doi.org/10.3390/ijms23137020.
Gunduz A, Gunduz A, Cumurcu T, Seyrek A. Conjunctival flora in Behcet patients. Can J Ophthalmol. 2008;43(4):476–9. https://doi.org/10.3129/i08-089.
Li JJ, Yi S, Wei L. Ocular microbiota and intraocular inflammation. Front Immunol. 2020;11:609765. https://doi.org/10.3389/fimmu.2020.609765.
Iovieno A, Lambiase A, Sacchetti M, Stampachiacchiere B, Micera A, Bonini S. Preliminary evidence of the efficacy of probiotic eye-drop treatment in patients with vernal keratoconjunctivitis. Graefes Arch Clin Exp Ophthalmol. 2008;246(3):435–41. https://doi.org/10.1007/s00417-007-0682-6.
Abengozar-Vela A, Schaumburg CS, Stern ME, Calonge M, Enriquez-de-Salamanca A, Gonzalez-Garcia MJ. Topical quercetin and resveratrol protect the ocular surface in experimental dry eye disease. Ocul Immunol Inflamm. 2019;27(6):1023–32. https://doi.org/10.1080/09273948.2018.1497664.
Chisari G, Chisari EM, Borzi AM, Chisari CG. Aging eye microbiota in dry eye syndrome in patients treated with Enterococcus faecium and Saccharomyces boulardii. Curr Clin Pharmacol. 2017;12(2):99–105. https://doi.org/10.2174/1574884712666170704145046.
Kawashima M, Nakamura S, Izuta Y, Inoue S, Tsubota K. Dietary supplementation with a combination of lactoferrin, fish oil, and Enterococcus faecium WB2000 for treating dry eye: a rat model and human clinical study. Ocul Surf. 2016;14(2):255–63. https://doi.org/10.1016/j.jtos.2015.12.005.
Kim J, Choi SH, Kim YJ, Jeong HJ, Ryu JS, Lee HJ, et al. Clinical effect of IRT-5 probiotics on immune modulation of autoimmunity or alloimmunity in the eye. Nutrients. 2017;9(11):1166. https://doi.org/10.3390/nu9111166.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Ocular Surface
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cavuoto, K.M., Zhu, A.Y. The Role of the Ocular Surface Microbiome (OSM) in Diseases of the Anterior Segment and Ocular Surface. Curr Ophthalmol Rep 10, 179–187 (2022). https://doi.org/10.1007/s40135-022-00294-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40135-022-00294-4