Abstract
Purpose of Review
In this article, the current use and limitations of existing retinal tamponades are discussed. Potential novel developments that address those limitations are subsequently highlighted, along with areas of future improvements.
Recent Findings
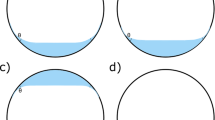
While retinal tamponades have existed for decades and improved the treatment of retinal detachments, many problems still exist with their use, including inadequate tamponade of the inferior retina, toxicity from retained heavy liquids, glaucoma, and keratopathy, among others. New advancements in the components of heavy liquids and vitreous substitutes aim to mitigate those issues.
Summary
Existing retinal tamponades, including perfluorocarbon heavy liquids, fluorinated gases, and silicone oil, have specific limitations that cause potentially avoidable morbidity. New developments, such as heavy silicone oil, novel vitreous gels, and future avenues of approach, such as potentially reabsorbing heavy liquids may help increase our ability to treat retinal detachments with fewer complications.


Similar content being viewed by others
References
Mitry D, Charteris DG, Fleck BW, Campbell H, Singh J. The epidemiology of rhegmatogenous retinal detachment: geographical variation and clinical associations. Br J Ophthalmol. 2010;94(6):678–84.
Ohm J. On the treatment of retinal detachment by surgical evacuation of subretinal fluid and injection of air into the vitreous. Albrecht Von Graefes Arch Für Ophthalmol. 1911;79(3):442–50.
Gonin J. The treatment of detached retina by searing the retinal tears. Arch Ophthalmol. 1930;4(5):621–5.
Murtagh PJ, Stephenson KA, Rhatigan M, McElnea EM, Connell PP, Keegan DJ. Rhegmatogenous retinal detachments: primary reattachment rates and visual outcomes over a 4-year period. Ir J Med Sci. 2020;189(1):355–63.
Li Y, Cheung N, Jia L, Zhang H, Liu N. Surgical outcomes of 25-gauge pars plana vitrectomy using air as an internal tamponade for primary rhegmatogenous retinal detachment. Retina. 2020.
Wang JC, Ryan EH, Ryan C, Kakulavarapu S, Mardis PJ, Rodriguez M, Stefater JA, Forbes NJ, Gupta O, Capone A Jr, Emerson GG, Joseph DP, Eliott D, Yonekawa Y; Primary Retinal Detachment Outcomes (PRO) Study Group. Factors associated with the use of 360-degree laser retinopexy during primary vitrectomy with or without scleral buckle for rhegmatogenous retinal detachment and impact on surgical outcomes (pro study report number 4). Retina. 2019.
Goldman DR, Shah CP, Heier JS. Expanded criteria for pneumatic retinopexy and potential cost savings. Ophthalmology. 2014;121(1):318–26.
Mohamed S, Lai TY. Intraocular gas in vitreoretinal surgery. HK J Ophthalmol. 2010;14(1):8–13.
Petersen J. The physical and surgical aspects of silicone oil in the vitreous cavity. Graefes Arch Clin Exp Ophthalmol. 1987;225(6):452–6.
Regillo CD, Tornambe PE. Primary retinal detachment repair. In: Regillo CD, Brown GC, Flynn Jr HW, editors. Vitreoretinal disease: the essentials. 1st ed. New York: Thieme; 1998. p. 631–46.
Zauberman H. Tensile strength of chorioretinal lesions produced by photocoagulation, diathermy, and cryopexy. Br J Ophthalmol. 1969;53:749–52.
Yoon YH, Marmor MF. Rapid enhancement of retinal adhesion by laser photocoagulation. Ophthalmology. 1988;95:1385–138.
Chang S. Low viscosity liquid fluorochemicals in vitreous surgery. Am J Ophthalmol. 1987 Jan 15;103(1):38–43.
Kreiger AE, Lewis H, Management of Giant Retinal Tears without Scleral Buckling. Use of radical dissection of the vitreous base and perfluoro-octane and intraocular tamponade. Ophthalmology. 1992;99(4):491–7.
Scott IU, Murray TG, Flynn HW Jr, Feuer WJ, Schiffman JC. Outcomes and complications associated with giant retinal tear management using perfluoro-n-octane. Ophthalmology. 2002;109(10):1828–33.
Shunmugam M, Ang GS, Lois N. Giant retinal tears. Surv Ophthalmol. 2014 Mar-Apr;59(2):192–216.
Kreissig I. The perfluorocarbon gases. In: Practical guide to minimal surgery for retinal detachment, vol. 2. 1st ed. Stuttgart: Thieme; 2000. p. 129–32.
Russo A, Morescalchi F, Donati S, Gambicorti E, Azzolini C, Costagliola C, et al. Heavy and standard silicone oil: intraocular inflammation. Int Ophthalmol. 2018 Apr;38(2):855–67.
Sullivan PM, Luff AJ, Aylward GW. Results of primary retinal reattachment surgery: a prospective audit. Eye Lond Engl. 1997;11(Pt 6):869–71.
Scott IU, Flynn HW Jr, Murray TG, Smiddy WE, Davis JL, Feuer WJ. Outcomes of complex retinal detachment repair using 1000- vs 5000-centistoke silicone oil. Arch Ophthalmol. 2005;123(4):473–8.
Douglas JF, et al. Viscosity. In: Fluid mechanics. 5th ed. Harlow: England; 2005. p. 11–4.
Stilma JS, Koster R, Zivojnović R. Radical vitrectomy and silicone-oil injection in the treatment of proliferative vitreoretinopathy following retinal detachment. Doc Ophthalmol Adv Ophthalmol. 1986;64:109–16.
Azen SP, Scott IU, Flynn HW, et al. Silicone oil in the repair of complex retinal detachments. A prospective observational multicenter study. Ophthalmology. 1998;105:1587–97.
Lai WW, Yusof W, Lo A, Wong IY, Wong D. Long-term intraocular tamponade with silicone oil. In: Narendran V, Kothar AR, editors. Principles and practice of Vitreoretinal surgery. 1st ed. New Delhi: JP Medical Ltd; 2014. p. 145–50.
Shunmugam M, Shah AN, Hysi PG, Williamson TH. The pattern and distribution of retinal breaks in eyes with rhegmatogenous retinal detachment. Am J Ophthalmol. 2014;157(1):221–6 e1.
Pastor JC, de la Rúa ER, Martín F. Proliferative vitreoretinopathy: risk factors and pathobiology. Prog Retin Eye Res. 2002;21(1):127–44.
Idrees S, Sridhar J, Kuriyan AE. Proliferative vitreoretinopathy: a review. Int Ophthalmol Clin. 2019 Winter;59(1):221–40.
Shiraki N, Sakimoto S, Sakaguchi H, Nishida K, Nishida K, Kamei M. Vitrectomy without prone positioning for rhegmatogenous retinal detachments in eyes with inferior retinal breaks. PLoS One. 2018;13(1):e0191531.
Abu El-Asrar AM, Al-Kwikbi HF, Kangave D. Prognostic factors after primary vitrectomy and perfluorocarbon liquids for bullous rhegmatogenous retinal detachment. Eur J Ophthalmol. 2009;19(1):107–17.
Ghoraba HH, Ghoraba HH, Heikal MA, Elgouhary SM, Mansour HO, Abdelhafez MA, Zaky AG. Submacular perfluorocarbon liquid: long-term follow-up. Int Ophthalmol 2020.
Winter M, Winter C, Wiechens B. Quantification of intraocular retained perfluorodecalin after macroscopic complete removal. Graefes Arch Clin Exp Ophthalmol. 1999;237:153–6.
Shulman M, Sepah YJ, Chang S, Abrams GW, Do DV, Nguyen QD. Management of retained subretinal perfluorocarbon liquid. Ophthalmic Surg Lasers Imaging Retina. 2013;44(6):577–83.
Chang S, Sparrow JR, Iwamoto T, Gershbein A, Ross R, Ortiz R. Experimental studies of tolerance to intravitreal perfluoro-n-octane liquid. Retina. 1991;11(4):367–74.
Eckardt C, Nicolai U, Winter M, Knop E. Experimental intraocular tolerance to liquid perfluorooctane and perfluoropolyether. Retina. 1991;11(4):375–84.
Elsing SH, Fekrat S, Green WR, Chang S, Wajer SD, Haller JA. Clinicopathologic findings in eyes with retained perfluoro-n-octane liquid. Ophthalmology. 2001;108:45–8.
Singh J, Ramaesh K, Wharton SB, Cormack G, Chawla HB. Perfluorodecalin-induced intravitreal inflammation. Retina (Philadelphia, Pa). 2001;21:247–51.
Wilbanks GA, Apel AJ, Jolly SS, Devenyi RG, Rootman DS. Perfluorodecalin corneal toxicity: five case reports. Cornea. 1996;15:329–34.
Foster RE, Smiddy WS, Alfonso EC, Parrish RK. Secondary glaucoma associated with perfluorophenanthrene. Am J Ophthalmol. 1994;118:253–5.
Kanclerz P, Grzybowski A. Complications associated with the use of expandable gases in vitrectomy. J Ophthalmol. 2018;2018:8606494.
Van Horn DL, Edelhauser HF, Aaberg TM, Pederson HJ. In vivo effects of air and sulfur hexafluoride gas on rabbit corneal endothelium. Investig Ophthalmol. 1972;11(12):1028–36.
Tan CSH, Wee K, Zaw M-D, Lim TH. Anterior chamber gas bubble following pneumatic retinopexy in a young, phakic patient. Clin Exp Ophthalmol. 2011;39(3):276–7.
Taher RM, Haimovici R. Anterior chamber gas entrapment after phakic pneumatic retinopexy. Retina. 2001;21(6):681–2.
Han DP, Lewis H, Lambrou FH Jr, Mieler WF, Hartz A. Mechanisms of Intraocuular Pressure Elevation after Pars Plana Vitrectomy. Ophthalmology. 1989;96(9):1357–62.
Chang S, Lincoff HA, Coleman DJ, Fuchs W, Farber ME. Perfluorocarbon gases in vitreous surgery. Ophthalmology. 1985;92(5):651–6.
Chen CJ. Glaucoma after macular hole surgery. Ophthalmology. 1998;105(1):94–9 discussion 99-100.
Modi A, Giridhar A, Gopalakrishnan M. Sulfur hexafluoride (SF6) versus perfluoropropane (C3F8) gas as tamponade in macular hole surgery. Retina. 2017;37(2):283–90.
Yee KMP, Tan S, Lesnik Oberstein SY, Filas B, Nguyen JH, Nguyen-Cuu J, et al. Incidence of cataract surgery after vitrectomy for vitreous opacities. Ophthalmology Retina. 2017;1(2):154–7.
Ichhpujani P, Jindal A, Jay Katz L. Silicone oil induced glaucoma: a review. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Für Klin Exp Ophthalmol. 2009;247:1585–93.
Cour AM, Lux A, Heegaard S. Visual loss under silicone oil. Klin Monatsblätter Für Augenheilkd. 2010;227:181–4.
Tyagi M, Basu S. Glue-assisted retinopexy for rhegmatogenous retinal detachments (GuARD): a novel surgical technique for closing retinal breaks. Indian J Ophthalmol. 2019;67(5):677–80.
Haruta M, Arai M, Sueda J, Hirose T, Yamakawa R. Patching retinal breaks with Seprafilm for treating retinal detachments in humans: 9 years of follow-up. Eye. 2017;31:776–80.
Georgalas I, Petrou P, Koutsandrea C, Papaconstadinou D, Ladas I, Gotzaridis E, et al. Eur J Ophthalmol. 2009;19(2):324–6.
Doi M, Refojo MF. Histopathology of rabbit eyes with silicone-fluorosilicone copolymer oil as six months internal retinal tamponade. Exp Eye Res. 1995;61:469–78.
Schatz B, El-Shabrawi Y, Haas A, Langmann G. Adverse side effects with perfluorohexyloctane as a long-term tamponade agent in complicated vitreoretinal surgery. Retina Phila Pa. 2004;24:567–73.
Georgalas I, Ladas I, Tservakis I, Taliantzis S, Gotzaridis E, Papaconstantinou D, et al. Perfluorocarbon liquids in vitreoretinal surgery: a review of applications and toxicity. Cutan Ocul Toxicol. 2011;30(4):251–62.
Levasseur SD, Schendel S, Machuck RW, Dhanda D. High-density silicone oil Densiron-68 as an intraocular tamponade for primary inferior retinal detachments. Retina. 2013;33(3):627–33.
Caporossi T, Franco F, Finocchio L, Barca F, Giansanti F, Tartaro R, et al. Densiron 68 heavy silicone oil in the management of inferior retinal detachment recurrence: analysis on functional and anatomical outcomes and complications. Int J Ophthalmol. 2019;12(4):615–20.
Peyman GA, Conway MD, Karacorlu M, et al. Evaluation of silicone gel as a long-term vitreous substitute in non-human primates. Ophthalmic Surg. 1992;23:811–7.
Liang CP, Peyman GA, Serracarbassa P, Calixto N, Chow AA, Rao P. An evaluation of methylated collagen as a substitute for vitreous and aqueous humor. Int Ophthalmol. 1998;22:13–8.
Nakagawa M, Tanaka M, Miyata T. Evaluation of collagen gel and hyaluronic acid as vitreous substitutes. Ophthalmic Res. 1997;29:409–20.
Chirila TV, Sharp C, Moore SR, et al. Synthetic hydrogel as an artificial vitreous body. A one-year animal study of its effects on the retina. Cell Mater. 1995;5:83–96.
Fernandez-Vigo J, Refojo MF, Verstraeten T. Evaluation of a viscoelastic solution of hydroxypropyl methylcellulose as a potential vitreous substitute. Retina. 1990;10:148–52.
Crafoord S, Andreasson S, Ghosh F. Experimental vitreous tamponade using polyalkylimide hydrogel. Graefes Arch Clin Exp Ophthalmol. 2011;249:1167–74.
De Jong C, Bali E, Libert J, et al. ADCON-L hydrogel as a vitreous substitute: preliminary results. Bull Soc Belge Ophtalmol. 2000:71–5.
Maruoka S, Matsuura T, Kawasaki K, Okamoto M, Yoshiaki H, Kodama M, et al. Biocompatibility of polyvinylalcohol gel as a vitreous substitute. Curr Eye Res. 2006;31(7–8):599–606.
Katagiri Y, Iwasaki T, Ishikawa T, Yamakawa N, Suzuki H, Usui M. Application of thermo-setting gel as artificial vitreous. Jpn J Ophthalmol. 2005;49(6):491–6.
Hayashi K, Okamoto F, Hoshi S, Katashima T, Zujur DC, Li X, et al. Fast-forming hydrogel with ultralow polymeric content as an artificial vitreous body. Nat Biomed Eng. 2017;1:0044.
Liu Z, Liow SS, Lai SL, Alli-Shaik A, Holder GE, Parikh BH, et al. Retinal-detachment repair and vitreous-like-body reformation via a thermogelling polymer endotamponade. Nat Biomed Eng. 2019;3:598–610.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Retina
Rights and permissions
About this article
Cite this article
Deobhakta, A., Rosen, R. Retinal Tamponades: Current Uses and Future Technologies. Curr Ophthalmol Rep 8, 144–151 (2020). https://doi.org/10.1007/s40135-020-00247-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40135-020-00247-9