Abstract
Purpose of Review
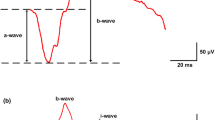
Currently, the clinical evaluation of neuro-ophthalmologic diseases is mainly focused on identifying stages where structural or functional damage occurs. Recognition of retinal ganglion cell (RGC) functional patterns as well as monitoring RGC dysfunction can be performed using steady-state pattern electroretinogram (PERG). The analysis of the amplitude and latency shift aids on providing information on early damage or monitoring of the RGC, allowing for prompt clinical intervention and management modification, potentially changing the natural history of the disease. The purpose of this article is to review the latest findings in PERG, in early manifest glaucoma, non-arteritic ischemic optic neuropathy, multiple sclerosis with unilateral recovered optic neuritis, and its fellow eyes.
Recent Findings
The steady-state PERG responses provide new and early specific information in neuro-ophthalmic diseases affecting the inner retina.
Summary
Steady-state PERG presents specific amplitude and latency outcomes based on the neuro-ophthalmic disease affecting the inner retina, allowing early recognition of changes at the level of RGC and the degree of RGC dysfunction. In addition, PERG alterations may be induced in healthy subjects as well as susceptible eyes using different stress tests such as head-down tilting or water-drinking tests.





Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Porciatti V. Electrophysiological assessment of retinal ganglion cell function. Exp Eye Res. 2015;141:164–70. https://doi.org/10.1016/j.exer.2015.05.008.
Porciatti V, Ventura LM. The PERG as a tool for early detection and monitoring of glaucoma. Current Ophthalmology Reports. 2017;5(1):7–13. https://doi.org/10.1007/s40135-017-0128-1.
Holder GE. Pattern electroretinography (PERG) and an integrated approach to visual pathway diagnosis. Prog Retin Eye Res. 2001;20(4):531–61.
Bach M, Brigell MG, Hawlina M, Holder GE, Johnson MA, McCulloch DL, et al. ISCEV standard for clinical pattern electroretinography (PERG): 2012 update. Doc Ophthalmol. 2013;126(1):1–7. https://doi.org/10.1007/s10633-012-9353-y.
Hood DC, Xu L, Thienprasiddhi P, Greenstein VC, Odel JG, Grippo TM, et al. The pattern electroretinogram in glaucoma patients with confirmed visual field deficits. Invest Ophthalmol Vis Sci. 2005;46(7):2411–8. https://doi.org/10.1167/iovs.05-0238.
•• Monsalve P, Triolo G, Toft-Nielsen J, Bohorquez J, Henderson AD, Delgado R, et al. Next generation PERG method: expanding the response dynamic range and capturing response adaptation. Transl Vis Sci Technol, This study compares the new steady state PERG method to a previously validated PERG method. 2017;6(3):5. https://doi.org/10.1167/tvst.6.3.5.
•• Monsalve P, Ren S, Triolo G, Vazquez L, Henderson AD, Kostic M, et al. Steady-state PERG adaptation: a conspicuous component of response variability with clinical significance. Doc Ophthalmol. 2018;136(3):157–64. https://doi.org/10.1007/s10633-018-9633-2 This study describes the within test variability of the steady state PERG reponse and describes its significant physiological and clinical implications.
Porciatti V, Sartucci F. Retinal and cortical evoked responses to chromatic contrast stimuli. Specific losses in both eyes of patients with multiple sclerosis and unilateral optic neuritis. Brain. 1996;119(Pt 3):723–40.
Jansonius NM, Kooijman AC. The effect of defocus on edge contrast sensitivity. Ophthalmic Physiol Opt. 1997;17(2):128–32.
Digre KB, Evangelou N, Konz D, Esiri MM, et al. Size-selective neuronal changes in the anterior optic pathways suggest a differential susceptibility to injury in multiple sclerosis. J Neuroophthalmol. 2002;22(2):143. https://doi.org/10.1097/00041327-200206000-00040.
Centofanti M, Fogagnolo P, Oddone F, Orzalesi N, Vetrugno M, Manni G, et al. Learning effect of Humphrey matrix frequency doubling technology perimetry in patients with ocular hypertension. J Glaucoma. 2008;17(6):436–41. https://doi.org/10.1097/IJG.0b013e31815f531d.
Porciatti V, Sorokac N, Buchser W. Habituation of retinal ganglion cell activity in response to steady state pattern visual stimuli in normal subjects. Invest Ophthalmol Vis Sci. 2005;46(4):1296–302. https://doi.org/10.1167/iovs.04-1242.
Porciatti V, Ventura LM. Adaptive changes of inner retina function in response to sustained pattern stimulation. Vis Res. 2009;49(5):505–13. https://doi.org/10.1016/j.visres.2008.12.001.
Porciatti V, Bosse B, Parekh PK, Shif OA, Feuer WJ, Ventura LM. Adaptation of the steady-state PERG in early glaucoma. J Glaucoma. 2014;23(8):494–500. https://doi.org/10.1097/IJG.0b013e318285fd95.
Bach M. Electrophysiological approaches for early detection of glaucoma. Eur J Ophthalmol. 2001;11(Suppl 2):S41–9.
Trick GL. Retinal potentials in patients with primary open-angle glaucoma: physiological evidence for temporal frequency tuning deficits. Invest Ophthalmol Vis Sci. 1985;26(12):1750–8.
Hattenhauer MG, Leavitt JA, Hodge DO, Grill R, Gray DT. Incidence of nonarteritic anteripr ischemic optic neuropathy. Am J Ophthalmol. 1997;123(1):103–7. https://doi.org/10.1016/s0002-9394(14)70999-7.
Parisi V, Gallinaro G, Ziccardi L, Coppola G. Electrophysiological assessment of visual function in patients with non-arteritic ischaemic optic neuropathy. Eur J Neurol. 2008;15(8):839–45. https://doi.org/10.1111/j.1468-1331.2008.02200.x.
Kidd DP, Plant GT. Chapter 6 Optic Neuritis. Blue Books of Neurology. 2008. p. 134–52.
Plant GT. Optic neuritis and multiple sclerosis. Curr Opin Neurol. 2008;21(1):16–21. https://doi.org/10.1097/WCO.0b013e3282f419ca.
Petzold A, Wattjes MP, Costello F, Flores-Rivera J, Fraser CL, Fujihara K, et al. The investigation of acute optic neuritis: a review and proposed protocol. Nat Rev Neurol. 2014;10(8):447–58. https://doi.org/10.1038/nrneurol.2014.108.
Szilasiová J, Klímová E, Veselá D. Optic neuritis as the first sign of multiple sclerosis. Cesk Slov Oftalmol. 2002;58(4):259–64.
Lizrova Preiningerova J, Grishko A, Sobisek L, Andelova M, Benova B, Kucerova K, et al. Do eyes with and without optic neuritis in multiple sclerosis age equally? Neuropsychiatr Dis Treat. 2018;14:2281–5. https://doi.org/10.2147/NDT.S169638.
Hokazono K, Raza AS, Oyamada MK, Hood DC, Monteiro MLR. Pattern electroretinogram in neuromyelitis optica and multiple sclerosis with or without optic neuritis and its correlation with FD-OCT and perimetry. Doc Ophthalmol. 2013;127(3):201–15. https://doi.org/10.1007/s10633-013-9401-2.
Klistorner A, Sriram P, Vootakuru N, Wang C, Barnett MH, Garrick R, et al. Axonal loss of retinal neurons in multiple sclerosis associated with optic radiation lesions. Neurology. 2014;82(24):2165–72. https://doi.org/10.1212/WNL.0000000000000522.
Akçam HT, Capraz IY, Aktas Z, Batur Caglayan HZ, Ozhan Oktar S, Hasanreisoglu M, et al. Multiple sclerosis and optic nerve: an analysis of retinal nerve fiber layer thickness and color Doppler imaging parameters. Eye. 2014;28(10):1206–11. https://doi.org/10.1038/eye.2014.178.
Janaky M, Janossy A, Horvath G, Benedek G, Braunitzer G. VEP and PERG in patients with multiple sclerosis, with and without a history of optic neuritis. Documenta ophthalmologica Advances in ophthalmology. 2017;134(3):185–93. https://doi.org/10.1007/s10633-017-9589-7.
Rodriguez-Mena D, Almarcegui C, Dolz I, Herrero R, Bambo MP, Fernandez J, et al. Electropysiologic evaluation of the visual pathway in patients with multiple sclerosis. J Clin Neurophysiol. 2013;30(4):376–81. https://doi.org/10.1097/WNP.0b013e31829d75f7.
Fraser CL, Holder GE. Electroretinogram findings in unilateral optic neuritis. Documenta ophthalmologica Advances in ophthalmology. 2011;123(3):173–8. https://doi.org/10.1007/s10633-011-9294-x.
Parisi V, Manni G, Spadaro M, Colacino G, Restuccia R, Marchi S, et al. Correlation between morphological and functional retinal impairment in multiple sclerosis patients. Invest Ophthalmol Vis Sci. 1999;40(11):2520–7.
Falsini B, Porrello G, Porciatti V, Fadda A, Salgarello T, Piccardi M. The spatial tuning of steady state pattern electroretinogram in multiple sclerosis. Eur J Neurol. 1999;6(2):151–62.
Falsini B, Porciatti V. The temporal frequency response function of pattern ERG and VEP: changes in optic neuritis. Electroencephalogr Clin Neurophysiol. 1996;100(5):428–35.
•• Monsalve P, Ren S, Jiang H, Wang J, Kostic M, Gordon P, et al. Retinal ganglion cell function in recovered optic neuritis: faster is not better. Clin Neurophysiol, This study describes the steady state PERG response in patients with multiple sclerosis and recovered optice neuritis. 2018;129(9):1813–8. https://doi.org/10.1016/j.clinph.2018.06.012.
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–7. https://doi.org/10.1136/bjo.2005.081224.
Porciatti V, Ventura LM. Retinal ganglion cell functional plasticity and optic neuropathy: a comprehensive model. J Neuroophthalmol. 2012;32(4):354–8. https://doi.org/10.1097/WNO.0b013e3182745600.
Banitt MR, Ventura LM, Feuer WJ, Savatovsky E, Luna G, Shif O, et al. Progressive loss of retinal ganglion cell function precedes structural loss by several years in glaucoma suspects. Invest Ophthalmol Vis Sci. 2013;54(3):2346–52. https://doi.org/10.1167/iovs.12-11026.
Karaśkiewicz J, Drobek-Słowik M, Lubiński W. Pattern electroretinogram (PERG) in the early diagnosis of normal-tension preperimetric glaucoma: a case report. Doc Ophthalmol. 2013;128(1):53–8. https://doi.org/10.1007/s10633-013-9414-x.
Bach M, Hoffmann MB. Update on the pattern electroretinogram in glaucoma. Optom Vis Sci. 2008;85(6):386–95. https://doi.org/10.1097/OPX.0b013e318177ebf3.
Ventura LM, Porciatti V, Ishida K, Feuer WJ, Parrish RK 2nd. Pattern electroretinogram abnormality and glaucoma. Ophthalmology. 2005;112(1):10–9. https://doi.org/10.1016/j.ophtha.2004.07.018.
Bode SF, Jehle T, Bach M. Pattern electroretinogram in glaucoma suspects: new findings from a longitudinal study. Invest Ophthalmol Vis Sci. 2011;52(7):4300–6. https://doi.org/10.1167/iovs.10-6381.
Porciatti V, Feuer WJ, Monsalve P, Triolo G, Vazquez L, McSoley J, et al. Head-down posture in glaucoma suspects induces changes in IOP, systemic pressure, and PERG that predict future loss of optic nerve tissue. J Glaucoma. 2017;26(5):459–65. https://doi.org/10.1097/ijg.0000000000000648.
Fadda A, Di Renzo A, Martelli F, Marangoni D, Batocchi AP, Giannini D, et al. Reduced habituation of the retinal ganglion cell response to sustained pattern stimulation in multiple sclerosis patients. Clin Neurophysiol. 2013;124(8):1652–8. https://doi.org/10.1016/j.clinph.2013.03.001.
Yücel YH. Loss of neurons in magnocellular and parvocellular layers of the lateral geniculate nucleus in glaucoma. Arch Ophthalmol. 2000;118(3):378–84. https://doi.org/10.1001/archopht.118.3.378.
La Morgia C, Di Vito L, Carelli V, Carbonelli M. Patterns of retinal ganglion cell damage in neurodegenerative disorders: parvocellular vs magnocellular degeneration in optical coherence tomography studies. Front Neurol. 2017;8. https://doi.org/10.3389/fneur.2017.00710.
Gameiro G, Monsalve P, Golubev I, Ventura L, Porciatti V. Neurovascular changes associated with the water drinking test. J Glaucoma. 2018;27(5):429–32. https://doi.org/10.1097/IJG.0000000000000898.
Trick GL, Nesher R, Cooper DG, Shields SM. The human pattern ERG: alteration of response properties with aging. Optom Vis Sci. 1992;69(2):122–8.
Porciatti V, Burr DC, Morrone MC, Fiorentini A. The effects of aging on the pattern electroretinogram and visual evoked potential in humans. Vis Res. 1992;32(7):1199–209.
Funding
Supported by NIH Center Core Grant R43EY023460 and Research to Prevent Blindness Unrestricted Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Pedro Monsalve declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Topical Collection on Retina
Rights and permissions
About this article
Cite this article
Monsalve, P. Decoding PERG: a Neuro-Ophthalmic Retinal Ganglion Cell Function Review. Curr Ophthalmol Rep 7, 51–58 (2019). https://doi.org/10.1007/s40135-019-00199-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40135-019-00199-9