Abstract
Purpose of Review
A racially and ethnically diverse healthcare workforce leads to increased access to care and better health outcomes. Radiology and specifically the patient-centered subspecialty of breast imaging have a growing mismatch between the demographics of the physician workforce and the patient population served. Identifying and addressing the barriers for diversity is imperative in order to decrease disparities in breast cancer morbidity and mortality and achieve excellence in patient care.
Recent Findings
Three major barriers to promoting diversity and inclusion in the field of breast imaging and in the specialty of radiology more generally are unconscious bias, lack of mentorship for underrepresented minority (URM) students, and career development challenges facing women in radiology. We focus on these three issues and provide suggestions for addressing each of them.
Summary
Tackling unconscious bias through encouraging individual accountability and establishing implicit bias programs at the institutional level, supporting both formal and informal mentorship opportunities for URMs, and creating an environment to support women in leadership will bring us one step closer to fostering a diverse and inclusive breast imaging workforce and meeting the healthcare needs of the diverse US population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The USA has been described as a mosaic or salad bowl due to its rich mixture of people of different cultural backgrounds and the resultant wide range of diversity, which include all aspects of one’s identity including race, ethnicity, religion, gender, sexual orientation, and age. Such a diverse population demands a culturally competent healthcare workforce to provide patient-centered care [1••]. Diversity is an important aspect of every organization, as a diverse workforce can help to foster innovation, creativity, productivity, and cultural competence. Many institutions have done work aimed at improving awareness of the importance of diversity and inclusion and the potential benefits of incorporating both into the workplace culture. For example, IBM developed a 3-tiered system that can be adopted by academic medicine to achieve an equitable healthcare system capable of providing culturally and ethnically responsive care to all patients. The end goal is a shared understanding by all stakeholders that diversity and inclusion are essential for achieving excellence in patient care and central to attaining positive health outcomes [2]. A contributing factor that plays an important role when considering health disparities in the USA is the lack of a racially and ethnically diverse physician workforce. African American and Hispanic physicians are more likely to establish practices in minority communities and care for a higher percentage of Medicaid patients [3]. Similarly, women physicians are more likely to pursue a career in women’s health [4]. A shared race or ethnicity has been shown to enhance communication between physicians and their patients which leads to increased patient satisfaction and compliance [5]. When underrepresented minorities (URMs) and women are excluded from the workforce, the communities they represent and largely care for suffer. Thus, a diverse healthcare system should be a top public health initiative as it leads to increased access to care and better health outcomes.
The topic of diversity and inclusion is particularly relevant in the field of breast imaging, which is one of the few radiologic subspecialties where radiologists have significant in-person interaction with patients. Breast cancer affects one in eight women in the USA [6]. Additionally, it has become the most common cancer globally [7]. Breast imaging is a patient-centered subspeciality within radiology tasked with the early detection of breast cancer. As such, breast imaging radiologists serve a multiethnic, multicultural, and multilingual patient population. Thus, a diverse breast imaging workforce is essential. In spite of a roughly equal incidence of breast cancer, Black women are diagnosed at more advanced stages of disease and experience a lower 5-year survival rate compared to White women [8]. This discrepancy is believed to be, in part, due to confounding socioeconomic factors related to poverty, educational background, and limited access to care [9]. It is highly reasonable that a more diverse breast imaging healthcare community can help to increase screening efforts within the disadvantaged and marginalized populations for earlier breast cancer detection and improved survival outcomes. Appropriate breast cancer screening may not be sufficient to eliminate racial disparities in breast cancer survival. For example, Black women have been shown to experience higher breast cancer mortality at every stage compared to their White counterparts, which is multifactorial in nature [10]. Increased diversity in the medical profession may further promote inclusion of minority populations in research studies and treatment trials to decrease this racial disparity in breast cancer outcomes.
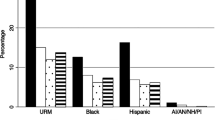
The US population is becoming more diverse every year; however, the healthcare workforce does not mirror the diversity of the general population. Underrepresented minorities in Medicine (URMs), including African Americans, Native Americans, and Hispanics, account for approximately 30% of the general population, yet they represent only 15.3% of medical school graduates and 6.5% of diagnostic radiologists [5]. Radiology, unfortunately, has proven to be the least diverse nonsurgical medical specialty [1]. Compared to the 20 largest medical training fields, radiology ranks at 18th for diversity with only 8.3% of residents identifying as URMs [5]. Although interest in radiology does not differ between male and female medical students [11], women are also underrepresented in the field of radiology. Compared to other medical subspecialties, women make up approximately 50% of graduating medical students, yet less than 33% of radiology residents and less than 10% of radiology department chairs are women [12]. Although women comprise the majority within the subspeciality of women’s Imaging, they are underrepresented among senior faculty and leadership [4]. It is imperative to address the growing mismatch between the demographics of the radiology physician workforce and the patient population being served. We have identified three major barriers to promoting diversity and inclusion in breast imaging and in the specialty of radiology more generally: unconscious bias, lack of mentorship for URM students, and career development challenges facing women in radiology. In this manuscript, we will focus on these three issues and provide suggestions for addressing them.
Barriers Hindering Diversity and Inclusion
Unconscious Bias
To promote diversity and inclusion in radiology, the American College of Radiology (ACR) created the Commission for Women and General Diversity to identify barriers to diversity and suggest solutions. One of the major barriers toward diversity is unconscious bias. Unconscious bias, also known as implicit bias [13], is an involuntary, automatic process based on deeply ingrained stereotypes and prejudices unconsciously absorbed from surrounding influences. It can cloud a person’s thought process, influence their decision-making process, and increase prejudiced and discriminatory behavior. It can affect all aspects of the medical field from how we recruit physicians to how we treat our patients. For example, when analyzing recommendation letters for radiology residency applicants, White and Asian applicants were notably found to be described with agentic traits as compared to their Black and Hispanic counterparts which may be secondary to implicit bias against URMs [14•].
Tackling Unconscious Bias Through Institutional- and Individual-Level Interventions
Unconscious bias must be tackled at both the institutional and individual level [4]. That is, institutions should supply programming and support to reduce implicit bias and individuals should be encouraged to take lessons learned and continuously apply these principles to their everyday lives. Through this multi-level model, the field of radiology, and breast imaging more specifically, can tackle the problem of unconscious bias. However, the question of how to create effective anti-bias modules is still unsettled. Programming for addressing unconscious bias varies across the nation with no standardized curriculum. Implicit bias training can range from non-interactive PowerPoints to intensive workshops characterized by small group discussions and activities requiring active participation. Given the complexity of effective implicit bias training, we must turn to the evidence-based methods for effective anti-discrimination curricula. Lessons from existing literature emphasize the need for nuance in the creation of such curricula. Duguid et al. found that subjects were more likely to stereotype when they were told that most people held stereotypical preconceptions that biased their interactions with others. On the other hand, those who were told that it was uncommon to hold stereotypical preconceptions and those who were told it was common to challenge preconceived notions were less likely to stereotype [15]. Legault et al. also found that subjects primed to think about non-prejudice as a personally motivated, positive goal had a reduction in bias while those primed to think about non-prejudice as a social expectation or obligation were more likely to perpetuate stereotypes [16]. In total, these findings emphasize that not all anti-bias programs are created equal and that it is imperative to use precise and thoughtful language that emphasizes autonomous motivation versus external pressure. Furthermore, in a time where COVID-19 restrictions have limited in-person sessions, integrating virtual and socially distant alternatives that are equally engaging and effective has become increasingly important.
While institution-level programming is a critical part of reducing bias, the individual must integrate anti-discrimination and anti-bias into their everyday interactions. In line with existing recommendations in the literature, we recommend that individuals actively combat their own unconscious biases by diversifying their life experiences and actively seeking opportunities to get to know people from different racial, ethnic, religious, and cultural backgrounds, explore examples of counter-stereotypes to challenge both their explicit and implicit biases, and purposely remind themselves to question whether implicit bias is affecting their decision-making at any moment [4].
Lack of Mentorship for URM Students
Academic preparation is another barrier to a diverse healthcare workforce. Systemic inequalities in the education system prevent many low-income and minority students from securing standardized testing scores needed to be considered for admission into the health professional programs. These same students have a high dropout rate, lack mentors, and lack knowledge about the variety of careers available to them [17]. Lack of mentorship has been cited as a major contributing factor for the underrepresentation of Black trainees within the field of radiology [18].
Increasing Early Career Guidance and Exposure to Radiology Through Mentorship
Leveraging mentorship at all levels of training can help to increase early exposure to radiology and help trainees with educational advancement and career promotion [17]. Mentorship can take a variety of forms. A more structured mentorship opportunity may involve a set schedule with specific requirements, goals, milestones, and activities [18]. The University of California San Francisco’s Research Initiative to promote Diversity in Radiology (RIDR) is an example of a successful structured mentorship program. Through an intensive 8-week summer program, RIDR connects high school and medical students with faculty mentorship, holds regular seminars aimed at demystifying a career in radiology, addresses unique challenges faced by URMs, and provides financial and structural support for the completion of successful research projects [19]. While measuring the benefit of such programs is never straight forward, the program tripled its applicants over 2 years, suggesting that the program reached URMs in need of mentorship [19]. Mentorship can also be a more informal and personalized arrangement requiring both the mentor and the mentee to establish their own interim goals and milestones. Both types of mentorship have proven to serve a critical role in recruiting and supporting URMs in STEM programs [20]. Mentorship primed to support URMs are characterized by the same core features found in good mentorship more broadly. This includes but is not limited to respect, collaboration, communication, commitment, and shared values [21]. However, mentors with URM mentees must also be equipped to address questions and hardships more commonly faced by URMs. Diversity and Inclusion policies are often a double-edged sword in that they can cause URMs to believe they are “Affirmative action hires”. This fear can snowball into significant imposter syndrome that then leads URMs to act with greater self-doubt, avoid taking credit for their work, and perform more poorly in inter-personal interactions [20, 22]. Thus, mentors of URMs, especially those mentors who identify as URMs themselves, must work against this imposter syndrome by re-affirming the mentee’s capabilities and by inspiring with their own personal experience [23]. While the challenge of navigating informal, unspoken institutional norms and cultures is a maze that all must face, URMs—especially those from lower socioeconomic status and those without generational exposure to graduate level education—often have more difficulty navigating this obstacle [20]. Mentors who acknowledge this difficulty and endow their URM mentees with the skills to navigate this challenge will help their URM mentees to be better equipped to advance through their careers successfully. Relevant to the discussion of mentorship for URMs is a discussion around who these mentors should be. Undoubtedly, mentors and mentees do not have to be racially congruent to have a productive relationship, however the benefits of a mentor who shares the same cultural and social experiences secondary to race cannot be dismissed. Unfortunately, a scarcity of URM faculty often means they take on outsized mentorship responsibilities [18]. While it is our hope that diversity and inclusion efforts will increase URM faculty appointments in the future, recruiting URM physicians from outside of academia e.g., community hospitals and integrating virtual opportunities to allow mentors to reach mentees from around the country will hopefully relieve some of this burden.
While our discussion thus far has focused on URMs, most often defined as those who identify as African American or Black, Mexican–American, Native American, Pacific Islander, or mainland Puerto Rican [24], a discussion of underrepresented demographics in breast imaging must include a discussion of the paucity of men in breast imaging. Although women are underrepresented in radiology as a whole, women are overrepresented in breast imaging, making up approximately 81.5% of breast imagers [25]. Unfortunately, little data exists on the specific barriers that deter men from pursuing breast imaging as a specialty. It is also unclear how much of this difference is secondary to lack of interest in breast imaging. However, it is important that we support and nurture those men who are interested in pursuing breast imaging fellowships. To this effect, we emphasize the importance of encouraging male breast imager mentors to mentor male trainees who are potentially interested in breast imaging, so that they may serve as a model for and encourage other men to consider the field.
Career Development Challenges Facing Women in Radiology
Society places a disproportionate burden related to family responsibilities on women compared to men. As such, women would benefit from programs and policies aimed at supporting and enabling them to achieve optimal balance in their work and family responsibilities. For example, policies ensuring women’s access to adequate maternity leave and work-life flexibility in the USA is an area where there is room for improvement. Pregnancy and the postpartum period are challenges that are unique to women during their training and formative career years. Additionally, childrearing responsibilities disproportionately fall onto women and can disrupt their career advancement. Although women constitute roughly half of all physicians, women often do not advance at the same rate as men and in some cases remain stagnate at the same position for their entire careers [26]. The COVID-19 pandemic has further worsened this gender disparity as women have been forced to take on increased responsibilities at home especially with childcare due to school closures [18, 27••]. Although this is a concern for the field of radiology as a whole, it is particularly relevant for the subspecialty of breast imaging, which is mostly comprised of women physicians.
Moss-Racusin et al. demonstrate the extent of gender bias in the academic science setting [28]. Both male and female faculty members considered a male applicant to be more competent than an identical female counterpart. For the same resume, faculty wished to offer a higher salary and increased mentoring opportunities to the male applicant [28]. This gender discrimination is the basis for gender and pay disparities that exists in all professional settings. In 2018, radiology was the medical specialty with the fourth largest pay gap with men earning 21% more than their female colleagues [29]. Additionally, the female-dominated field of breast imaging is the lowest paid radiology subspeciality [30]. While the pay gap in radiology is complicated by the fact that women radiologists are significantly more likely to work part-time than their male counterparts (30% vs. 7% respectively) [31], it is important to recognize the outsized gender pay gap in radiology. This difference in compensation can further deter women from considering the field of radiology or make them more prone to experiencing job dissatisfaction.
Supporting Career Advancement and Leadership for Women in Radiology
Although the vast majority (81.5%) of breast imaging radiologists are women, women fill less than 60% of breast imaging leadership positions [25]. Further, in radiology at large, women only make up 13% of leaders in radiology practices (defined as “managing partner, chair, vice chair, or executive committee member, etc.”) [32]. To increase female representation in radiology leadership, we must address policies that disrupt work-family balance and disincentivize women from pursuing leadership and career advancement opportunities. Equitable and robust parental leave policies are one way to relieve the stress of work-family balance for women radiologists. Supportive parental leave policies both relieve the temporal and financial cost of early family building for women and may serve to create an environment where motivated women radiologists can more easily advance in their careers. Parental leave has become an increasingly visible aspect of work-life balance conversations, but parental leave policies are far from universal and comprehensive. In fact, while parental leave was frequently mentioned on radiology residency program websites, paid parental leave was mentioned only 37.7% of the time and paid leave time averaged only 27.8 days [33]. This alarmingly short period of paid leave falls short of the minimum 6–8 weeks of paid leave recommended by the American Association of Pediatrics [34]. However, at least one radiology department in a large academic medical center has bucked against this trend and implemented a policy giving faculty 14 weeks of paid family leave and residents 12 weeks of family leave with resounding success [35]. While the challenges of implementing these policies secondary to small program size and limited institutional budget cannot be ignored, this case study emphasizes the feasibility of such policies. We urge radiology practices and radiology departments across the USA to evaluate their current institutional policies related to faculty and trainee wellbeing and work-life balance.
Pay parity or equal pay for equal work must also be discussed in a conversation about increasing women radiologists in leadership. Unfortunately, salary and compensation data are difficult to obtain for the private practice and hospital settings. However, public institution compensation data are available. Interestingly, unadjusted salaries between male and female radiologists in the US. public academic institutions were the same. After adjusting for age, faculty rank, years since residency, clinical trial involvement, publications, total Medicare payments, NIH funding, and graduation from a highly ranked medical school, there was still no difference between salary [36]. This limited data suggest public academic institutions may serve as a good model for pay parity. Thus, we recommend that radiology practices adopt policies that promote salary transparency and salary structures that correlate pay with level of experience and position.
All together, we encourage radiology practices and hospital systems to adopt policies that support both work-life balance and equitable pay structures, policies that prioritize efforts aimed at supporting women radiologists’ career advancement.
Conclusions and Recommendations
In this review, we outline key barriers to achieving optimal diversity and inclusion in radiology and detail critical solutions to these barriers. Increasing the diversity of practicing breast imaging radiologists and radiologists overall will better equip us to serve the USA’ diverse population. While efforts to increase diversity and inclusion in the trainee, private practice, hospital, and academic facets of radiology have already made great strides, our work is not done. Tackling unconscious bias through implicit bias programs at the institutional level, encouraging an environment of individual accountability, supporting both formal and informal mentorship opportunities for URMs, and creating an environment to support women in leadership will bring us one step closer to fostering a diverse and inclusive breast imaging workforce, one step closer to meeting the needs of URM and women radiologists and one step closer to meeting the needs of the USA’ diverse population.
References
Recently published papers of particular interest have been highlighted as: • Of importance •• Of major importance
•• Manik R, Sadigh G. Diversity and inclusion in radiology: a necessity for improving the field. Br J Radiol. 2021;20210407. This paper describes the importance of addressing diversity and inclusion, and the potential impact on all stakeholders in medicine.
Nivet MA. Commentary: diversity 3.0: a necessary systems upgrade. Acad Med. 2011;86(12):1487–9.
Sullivan LW. Improving diversity among health professionals in the United States: a brief history. J Am Acad Orthop Surg. 2007;15(Suppl 1):S1–3.
Allen BJ, Garg K. Diversity matters in academic radiology: acknowledging and addressing unconscious bias. J Am Coll Radiol. 2016;13(12 Pt A):1426–32.
Lightfoote JB, Fielding JR, Deville C, Gunderman RB, Morgan GN, Pandharipande PV, et al. Improving diversity, inclusion, and representation in radiology and radiation oncology part 1: why these matter. J Am Coll Radiol. 2014;11(7):673–80.
Centers for Disease Control and Prevention. Breast cancer in young women. 2019. https://www.cdc.gov/cancer/breast/young_women/bringyourbrave/breast_cancer_young_women/index.htm.
Reuters. Breast cancer overtakes lung as most common cancer-WHO. 2021. https://www.reuters.com/article/us-health-cancer/breast-cancer-overtakes-lung-as-most-common-cancer-who-idUSKBN2A21AK.
American Cancer Society. Cancer facts & figures for African Americans 2016–2018. Atlanta: American Cancer Society; 2016.
Moormeier J. Breast cancer in black women. Ann Intern Med. 1996;124(10):897–905.
Yedjou CG, Sims JN, Miele L, Noubissi F, Lowe L, Fonseca DD, et al. Health and racial disparity in breast cancer. Adv Exp Med Biol. 2019;1152:31–49.
Roubidoux MA, Packer MM, Applegate KE, Aben G. Female medical students’ interest in radiology careers. J Am Coll Radiol. 2009;6(4):246–53.
Chapman CH, Hwang WT, Both S, Thomas CR, Deville C. Current status of diversity by race, Hispanic ethnicity, and sex in diagnostic radiology. Radiology. 2014;270(1):232–40.
Ross, HJ. 3 ways to make less biased decisions. Harvard Business Review. 2015. https://hbr.org/2015/04/3-ways-to-make-less-biased-decisions.
• Grimm LJ, Redmond RA, Campbell JC, Rosette AS. Gender and racial bias in radiology residency letters of recommendation. J Am Coll Radiol. 2020;17(1 Pt A):64–71. This paper described racial/ethnic and gender-based differences in the extent to which agentic and communal language was used in letters of recommendation written for diagnostic radiology residency candidates.
Duguid MM, Thomas-Hunt MC. Condoning stereotyping? How awareness of stereotyping prevalence impacts expression of stereotypes. J Appl Psychol. 2015;100(2):343–59.
Legault L, Gutsell JN, Inzlicht M. Ironic effects of antiprejudice messages: how motivational interventions can reduce (but also increase) prejudice. Psychol Sci. 2011;22(12):1472–7.
Valentine P, Wynn J, McLean D. Improving diversity in the health professions. N C Med J. 2016;77(2):137–40.
Fite BZ, Hinostroza V, States L, Hicks-Nelson A, Baratto L, Kallianos K, et al. Increasing diversity in radiology and molecular imaging: current challenges. Mol Imaging Biol. 2021;23:625–38.
Bucknor MD, Villanueva-Meyer JE, Kumar V, Talbott JF, Wall SD, Glastonbury CM, et al. Diversity and inclusion efforts in university of california, san francisco radiology: reflections on 3 years of pipeline, selection, and education initiatives. J Am Coll Radiol. 2019;16(12):1716–9.
Zambrana RE, Ray R, Espino MM, Castro C, Douthirt Cohen B, Eliason J. “Don’t leave us behind”: the importance of mentoring for underrepresented minority faculty. Am Educ Res J. 2015;52(1):40–72.
Straus SE, Johnson MO, Marquez C, Feldman MD. Characteristics of successful and failed mentoring relationships: a qualitative study across two academic health centers. Acad Med. 2013;88(1):82–9.
Brems C, Baldwin MR, Davis L, Namyniuk L. The imposter syndrome as related to teaching evaluations and advising relationships of university faculty members. J Higher Educ. 1994;65(2):183–93.
Dancy TE, Brown MC. The mentoring and induction of educators of color: addressing the impostor syndrome in academe. J School Leadership. 2011;21(4):607–34.
Underrepresented in Medicine Definition. Association of American Medical Colleges. 2019. https://www.aamc.org/initiatives/urm/.
Khurshid K, Shah S, Ahmadi M, Jalal S, Carlos R, Nicolaou S, et al. Gender differences in the publication rate among breast imaging radiologists in the United States and Canada. Am J Roentgenol. 2017;210(1):2–7.
Lightfoote JB, Fielding JR, Deville C, Gunderman RB, Morgan GN, Pandharipande PV, et al. Improving diversity, inclusion, and representation in radiology and radiation oncology part 2: challenges and recommendations. J Am Coll Radiol. 2014;11(8):764–70.
•• Plaunova A, Heller SL, Babb JS, Heffernan CC. Impact of COVID-19 on radiology faculty: an exacerbation of gender differences in unpaid home duties and professional productivity. Acad Radiol. 2021;28(9):1185–90. This study evaluated the impact of the COVID-19 pandemuc on the home duties and workplace productivity of academic radiologists with respect to gender.
Moss-Racusin CA, Dovidio JF, Brescoll VL, Graham MJ, Handelsman J. Science faculty’s subtle gender biases favor male students. Proc Natl Acad Sci. 2012;109(41):16474–9.
Walter M. Radiology's average salary is $429K, but women make 21% Less than Men. RadiologyBusiness.com. 2019. https://www.radiologybusiness.com/topics/economics/radiology-compensation-average-salary-wage-gap.
Interventional radiologists earn higher salaries than diagnostic radiologists. InterventionalNews.com. 2019. https://interventionalnews.com/interventional-radiologists-high/.
Abduljabbar AH, Alnajjar SF, Alshamrani H, Bashamakh LF, Alshehri HZ, Alqulayti WM, et al. The influence of gender on the choice of radiology as a specialty among medical students in Saudi Arabia: cross-sectional study. Interact J Med Res. 2020;9(2):e14666.
Lewis RS, Sunshine JH, Bhargavan M. A portrait of breast imaging specialists and of the interpretation of mammography in the United States. Am J Roentgenol. 2006;187(5):W456–68.
Wong TY, Huang JJ, Hoffmann JC, Flug JA, Cooke EA, Donnelly EF. Resident wellness in radiology as portrayed by departmental websites. Acad Radiol. 2021. https://doi.org/10.1016/j.acra.2021.07.016.
Section On Medical Students R, Fellowship T, Committee On Early C. Parental leave for residents and pediatric training programs. Pediatrics. 2013;131(2):387.
Dodelzon K, Schweitzer AD. Paid family leave in a large urban center academic radiology department: how we do it. Clin Imaging. 2020;64:67–9.
Kapoor N, Blumenthal DM, Smith SE, Ip IK, Khorasani R. Sex differences in radiologist salary in U.S. public medical schools. Am J Roentgenol. 2017;209(5):953–8.
Funding
E. Oluyemi has received a research grant from GE Healthcare. The remaining authors declare that there are no other disclosures relevant to the subject matter of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
None for this work.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical collection on Breast Imaging.
Rights and permissions
About this article
Cite this article
Haken, O.J., Gong, A.J., Ambinder, E.B. et al. Diversity and Inclusion in Breast Imaging and Radiology at Large: What Can We Do to Improve?. Curr Radiol Rep 9, 13 (2021). https://doi.org/10.1007/s40134-021-00389-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s40134-021-00389-z