Abstract
Purpose of Review
Avoidant/restrictive food intake disorder (ARFID) is a relatively new psychiatric and eating disorder diagnosis that most often emerges in childhood. Due to ARFID’s diagnostic infancy, its medical complications are just starting to be delineated in the literature, and some are extrapolated from the medical manifestations of malnutrition in anorexia nervosa, restricting subtype (AN-R). Pediatric patients with ARFID can have a myriad of physical complaints, most commonly gastrointestinal, that prompt them to seek medical evaluation; thus, familiarity with its medical manifestations is important for all physicians.
Recent Findings
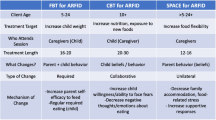
Electrolyte abnormalities may be more common in ARFID compared to patients with AN, while bradycardia has been shown to be comparatively less common. ARFID has been found to be associated with low bone density in both males and females. Addressing nutritional deficits and weight issues are paramount. Cognitive behavioral therapy for ARFID (CBT-ARFID) and several psychotropic medications have been found to be acceptable treatment modalities, but randomized controlled trials are needed.
Summary
ARFID has numerous reported and theoretical medical complications due to the resulting malnutrition that can last until adulthood if left untreated.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Arlington: American Psychiatric Publishing; 2013.
Norris ML, Robinson A, Obeid N, Harrison M, Spettigue W, Henderson K. Exploring avoidant/restrictive food intake disorder in eating disordered patients: a descriptive study. Int J Eat Disord. 2014;47(5):495–9. https://doi.org/10.1002/eat.22217.
Norris ML, Spettigue WJ, Katzman DK. Update on eating disorders: current perspectives on avoidant/restrictive food intake disorder in children and youth. Neuropsychiatr Dis Treat. 2016;12:213–8. https://doi.org/10.2147/NDT.S82538.
•• Bourne L, Bryant-Waugh R, Cook J, Mandy W. Avoidant/restrictive food intake disorder: a systematic scoping review of the current literature. Psychiatry Res. 2020;288:112961. https://doi.org/10.1016/j.psychres.2020.112961A review of 78 publications on ARFID addressing clinical presentations, treatment modalities and outcomes.
Nicely TA, Lane-Loney S, Masciulli E, Hollenbeak CS, Ornstein RM. Prevalence and characteristics of avoidant/restrictive food intake disorder in a cohort of young patients in day treatment for eating disorders. J Eat Disord. 2014;2(1):21. https://doi.org/10.1186/s40337-014-0021-3.
• Lieberman M, Houser ME, Voyer AP, Grady S, Katzman DK. Children with avoidant/restrictive food intake disorder and anorexia nervosa in a tertiary care pediatric eating disorder program: a comparative study. Int J Eat Disord. 2019;52(3):239–45. https://doi.org/10.1002/eat.23027Study comparing clinical presentations of patients with AN and ARFID.
Kennedy GA, Wick MR, Keel PK. Eating disorders in children: is avoidant-restrictive food intake disorder a feeding disorder or an eating disorder and what are the implications for treatment? F1000Res. 2018;7:88. https://doi.org/10.12688/f1000research.13110.1.
Cooney M, Lieberman M, Guimond T, Katzman DK. Clinical and psychological features of children and adolescents diagnosed with avoidant/restrictive food intake disorder in a pediatric tertiary care eating disorder program: a descriptive study. J Eat Disord. 2018;6:7. https://doi.org/10.1186/s40337-018-0193-3.
Zimmerman J, Fisher M. Avoidant/restrictive food intake disorder (ARFID). Curr Probl Pediatr Adolesc Health Care. 2017;47(4):95–103. https://doi.org/10.1016/j.cppeds.2017.02.005.
Duncombe Lowe K, Barnes TL, Martell C, Keery H, Eckhardt S, Peterson CB, et al. Youth with avoidant/restrictive food intake disorder: examining differences by age, weight status, and symptom duration. Nutrients. 2019;11(8). https://doi.org/10.3390/nu11081955.
Menzel JE, Reilly EE, Luo TJ, Kaye WH. Conceptualizing the role of disgust in avoidant/restrictive food intake disorder: implications for the etiology and treatment of selective eating. Int J Eat Disord. 2019;52(4):462–5. https://doi.org/10.1002/eat.23006.
Zickgraf HF. Avoidant/restrictive food intake disorder in adults: descriptive psychopathology and measure development. Publicly Accessible Penn Dissertations: University of Pennsylvania; 2018.
Thomas JJ, editor. Cognitive-behavioral therapy for avoidant/restrictive food intake disorder: current evidence and future directions. Eating Disorder Research Society 2020 Conference; 2020; virtual.
Lock J, Sadeh-Sharvit S, L'Insalata A. Feasibility of conducting a randomized clinical trial using family-based treatment for avoidant/restrictive food intake disorder. Int J Eat Disord. 2019;52(6):746–51. https://doi.org/10.1002/eat.23077.
Sharp WG, Stubbs KH, Adams H, Wells BM, Lesack RS, Criado KK, et al. Intensive, Manual-based intervention for pediatric feeding disorders: results from a randomized pilot trial. J Pediatr Gastroenterol Nutr. 2016;62(4):658–63. https://doi.org/10.1097/MPG.0000000000001043.
Dalle Grave A, Sapuppo W. Treatment of avoidant/restrictive food intake disorder: a systematic review. Ital J Eat Disord Obes. 2020;4:13–23. https://doi.org/10.32044/ijedo.2020.04.
Katzman DK, Norris ML, Zucker N. Avoidant restrictive food intake disorder. Psychiatr Clin N Am. 2019;42(1):45–57. https://doi.org/10.1016/j.psc.2018.10.003.
Brigham KS, Manzo LD, Eddy KT, Thomas JJ. Evaluation and treatment of avoidant/restrictive food intake disorder (ARFID) in adolescents. Curr Pediatr Rep. 2018;6(2):107–13. https://doi.org/10.1007/s40124-018-0162-y.
Thomas JJ, Becker KR, Kuhnle MC, Jo JH, Harshman SG, Wons OB, et al. Cognitive-behavioral therapy for avoidant/restrictive food intake disorder: feasibility, acceptability, and proof-of-concept for children and adolescents. Int J Eat Disord. 2020;53(10):1636–46. https://doi.org/10.1002/eat.23355.
Zucker NL, LaVia MC, Craske MG, Foukal M, Harris AA, Datta N, et al. Feeling and body investigators (FBI): ARFID division-An acceptance-based interoceptive exposure treatment for children with ARFID. Int J Eat Disord. 2019;52(4):466–72. https://doi.org/10.1002/eat.22996.
Sharp WG, Allen AG, Stubbs KH, Criado KK, Sanders R, McCracken CE, et al. Successful pharmacotherapy for the treatment of severe feeding aversion with mechanistic insights from cross-species neuronal remodeling. Transl Psychiatry. 2017;7(6):e1157. https://doi.org/10.1038/tp.2017.126.
Bryant-Waugh R. What is the best treatment for ARFID? ARFID Avoidant Restrictive Food Intake Disorder: A Guide for Parents and Carers: Routledge; 2019. https://doi.org/10.4324/9780429023354-6
Thomas JJ, Lawson EA, Micali N, Misra M, Deckersbach T, Eddy KT. Avoidant/restrictive food intake disorder: a three-dimensional model of neurobiology with implications for etiology and treatment. Curr Psychiatry Rep. 2017;19(8):54. https://doi.org/10.1007/s11920-017-0795-5.
Brewerton TD, D’Agostino M. Adjunctive use of olanzapine in the treatment of avoidant restrictive food intake disorder in children and adolescents in an eating disorders program. J Child Adolesc Psychopharmacol. 2017;27(10):920–2. https://doi.org/10.1089/cap.2017.0133.
Mehler PS, Blalock DV, Walden K, Kaur S, McBride J, Walsh K, et al. Medical findings in 1,026 consecutive adult inpatient-residential eating disordered patients. Int J Eat Disord. 2018;51(4):305–13. https://doi.org/10.1002/eat.22830.
Strandjord SE, Sieke EH, Richmond M, Rome ES. Avoidant/restrictive food intake disorder: illness and hospital course in patients hospitalized for nutritional insufficiency. J Adolesc Health. 2015;57(6):673–8. https://doi.org/10.1016/j.jadohealth.2015.08.003.
da Silva JSV, Seres DS, Sabino K, Adams SC, Berdahl GJ, Citty SW, et al. ASPEN Consensus recommendations for refeeding syndrome. Nutr Clin Pract. 2020;35(2):178–95. https://doi.org/10.1002/ncp.10474.
•• Skipper A. Refeeding syndrome or refeeding hypophosphatemia: a systematic review of cases. Nutr Clin Pract. 2012, 27(1):34–40. https://doi.org/10.1177/0884533611427916Guidelines for defining refeeding syndrome and determining risk for refeeding syndrome in both adult and pediatric populations.
Nutrition Support for Adults: Oral Nutrition Support, Enteral tube feeding and parenteral nutrition. National Institute for Health and Clinical Excellence: Guidance. London;2006.
Gaudiani JL, Sabel AL, Mascolo M, Mehler PS. Severe anorexia nervosa: outcomes from a medical stabilization unit. Int J Eat Disord. 2012;45(1):85–92. https://doi.org/10.1002/eat.20889.
Tsang KK, Hayes LC, Bujoreanu S, Samsel CB, Ibeziako PI. Characterization study of patients presenting to an acute care pediatric hospital identified with avoidant/restrictive food intake disorder. Hosp Pediatr. 2020;10(7):600–7. https://doi.org/10.1542/hpeds.2020-0010.
Dovey TM, Wilken M, Martin CI, Meyer C. Definitions and clinical guidance on the enteral dependence component of the avoidant/restrictive food intake disorder diagnostic criteria in children. JPEN J Parenter Enteral Nutr. 2018;42(3):499–507. https://doi.org/10.1177/0148607117718479.
•• Krantz MJ, Blalock DV, Tanganyika K, Farasat M, McBride J, Mehler PS. Is QTc-interval prolongation an inherent feature of eating disorders? A cohort study. Am J Med. 2020. https://doi.org/10.1016/j.amjmed.2020.02.015Recommendations for approach on weaning children with ARFID from enteral feeding.
Peyser D, Scolnick B, Hildebrandt T, Taylor JA. Heart rate variability as a biomarker for anorexia nervosa: A review. Eur Eat Disord Rev. 2020;29:20–31. https://doi.org/10.1002/erv.2791.
Aulinas A, Marengi DA, Galbiati F, Asanza E, Slattery M, Mancuso CJ, et al. Medical comorbidities and endocrine dysfunction in low-weight females with avoidant/restrictive food intake disorder compared to anorexia nervosa and healthy controls. Int J Eat Disord. 2020;53(4):631–6. https://doi.org/10.1002/eat.23261.
•• Doekel RC Jr, Zwillich CW, Scoggin CH, Kryger M, Weil JV. Clinical semi-starvation: depression of hypoxic ventilatory response. N Engl J Med. 1976;295(7):358–61. https://doi.org/10.1056/NEJM197608122950703A study demonstrating similarities and differences in markers of endocrine function in patients of ARFID and AN patients.
Baier H, Somani P. Ventilatory drive in normal man during semistarvation. Chest. 1984;85(2):222–5. https://doi.org/10.1378/chest.85.2.222.
Murciano D. Diaphragmatic function in severely malnourished patients with anorexia nervosa. Pediatr Pulmonol Suppl. 1997;16:169. https://doi.org/10.1002/ppul.1950230889.
Pieters T, Boland B, Beguin C, Veriter C, Stanescu D, Frans A, et al. Lung function study and diffusion capacity in anorexia nervosa. J Intern Med. 2000;248(2):137–42. https://doi.org/10.1046/j.1365-2796.2000.00712.x.
Gardini Gardenghi G, Boni E, Todisco P, Manara F, Borghesi A, Tantucci C. Respiratory function in patients with stable anorexia nervosa. Chest. 2009;136(5):1356–63. https://doi.org/10.1378/chest.08-3020.
Coxson HO, Chan IH, Mayo JR, Hlynsky J, Nakano Y, Birmingham CL. Early emphysema in patients with anorexia nervosa. Am J Respir Crit Care Med. 2004;170(7):748–52. https://doi.org/10.1164/rccm.200405-651OC.
Sahebjami H, MacGee J. Effects of starvation on lung mechanics and biochemistry in young and old rats. J Appl Physiol (1985). 1985;58(3):778–84. https://doi.org/10.1152/jappl.1985.58.3.778.
Minano Garrido E, Di Lodovico L, Dicembre M, Duquesnoy M, Ohanyan H, Melchior JC, et al. Evaluation of muscle-skeletal strength and peak expiratory flow in severely malnourished inpatients with anorexia nervosa: a pilot study. Nutrition. 2021;85:111133. https://doi.org/10.1016/j.nut.2020.111133.
Adson DE, Crow SJ, Mitchell JE. Spontaneous pneumothorax in anorexia nervosa. Psychosomatics. 1998;39(2):162–4. https://doi.org/10.1016/S0033-3182(98)71363-5.
Biffl WL, Narayanan V, Gaudiani JL, Mehler PS. The management of pneumothorax in patients with anorexia nervosa: a case report and review of the literature. Patient Saf Surg. 2010;4(1):1. https://doi.org/10.1186/1754-9493-4-1.
Loung RP, Cooney M, Fallon EM, Langer JC, Katzman DK. Pneumothorax in a young man with anorexia nervosa. Int J Eat Disord. 2016;49(9):895–8. https://doi.org/10.1002/eat.22558.
Murray HB, Bailey AP, Keshishian AC, Silvernale CJ, Staller K, Eddy KT, et al. Prevalence and characteristics of avoidant/restrictive food intake disorder in adult neurogastroenterology patients. Clin Gastroenterol Hepatol. 2020;18(9):1995–2002.e1. https://doi.org/10.1016/j.cgh.2019.10.030.
• Harer KN. Irritable bowel syndrome, disordered eating, and eating disorders. Gastroenterol Hepatol (N Y). 2019;15(5):280–2 A study demonstrating 6.3% prevalence of ARFID in sub- sub- specialty adult GI practice.
Winstead NS, Willard SG. Gastrointestinal complaints in patients with eating disorders. J Clin Gastroenterol. 2006;40(8):678–82. https://doi.org/10.1097/00004836-200609000-00003.
Rigaud D, Bedig G, Merrouche M, Vulpillat M, Bonfils S, Apfelbaum M. Delayed gastric emptying in anorexia nervosa is improved by completion of a renutrition program. Dig Dis Sci. 1988;33(8):919–25. https://doi.org/10.1007/BF01535985.
Nobis S, Morin A, Achamrah N, Belmonte L, Legrand R, Chan P, et al. Delayed gastric emptying and altered antrum protein metabolism during activity-based anorexia. Neurogastroenterol Motil. 2018;30(7):e13305. https://doi.org/10.1111/nmo.13305.
Chiarioni G, Bassotti G, Monsignori A, Menegotti M, Salandini L, Di Matteo G, et al. Anorectal dysfunction in constipated women with anorexia nervosa. Mayo Clin Proc. 2000;75(10):1015–9. https://doi.org/10.4065/75.10.1015.
Norris ML, Harrison ME, Isserlin L, Robinson A, Feder S, Sampson M. Gastrointestinal complications associated with anorexia nervosa: a systematic review. Int J Eat Disord. 2016;49(3):216–37. https://doi.org/10.1002/eat.22462.
Werlang ME, Senada PA, Robelin K, Ghoz H, Kröner PT, Lebow Jr et al. Avoidant/restrictive food intake disorder in an outpatient academic inflammatory bowel disease practice: prevalence and provider diagnostic accuracy. Digestive Disease Week; May 2-5, 2020; Virtual: American Gastroenterological Association; 2020.
Werlang ME, Sim LA, Lebow JR, Farraye FA, Kröner PT. Anorexia nervosa is associated with worse outcomes in hospitalized patients with inflammatory bowel disease. Digestive Disease Week; May2-5,2020; Virtual. AGA Abstracts: American Gastroenterological Association; 2020.
Dhir S, Tarasenko M, Napoli E, Giulivi C. Neurological, psychiatric, and biochemical aspects of thiamine deficiency in children and adults. Front Psychiatry. 2019;10:207. https://doi.org/10.3389/fpsyt.2019.00207.
Walsh K, Blalock DV, Mehler PS. Hematologic findings in a large sample of patients with anorexia nervosa and bulimia nervosa. Am J Hematol. 2020;95:E98–E101. https://doi.org/10.1002/ajh.25732.
Alberts Z, Fewtrell M, Nicholls DE, Biassoni L, Easty M, Hudson LD. Bone mineral density in anorexia nervosa versus avoidant restrictive food intake disorder. Bone. 2020;134:115307. https://doi.org/10.1016/j.bone.2020.115307.
• Schorr M, Drabkin A, Rothman MS, Meenaghan E, Lashen GT, Mascolo M, et al. Bone mineral density and estimated hip strength in men with anorexia nervosa, atypical anorexia nervosa and avoidant/restrictive food intake disorder. Clin Endocrinol. 2019;90(6):789–97. https://doi.org/10.1111/cen.13960A study showing child and adolescent patients with ARFID are at risk for low bone mineral density.
• Sharp WG, Berry RC, Burrell L, Scahill L, McElhanon BO. Scurvy as a sequela of avoidant-restrictive food intake disorder in autism: a systematic review. J Dev Behav Pediatr. 2020;41(5):397–405. https://doi.org/10.1097/dbp.0000000000000782A study showing men with ARFID are at risk for low bone mineral density.
Harshman SG, Wons O, Rogers MS, Izquierdo AM, Holmes TM, Pulumo RL, et al. A diet high in processed foods, total carbohydrates and added sugars, and low in vegetables and protein is characteristic of youth with avoidant/restrictive food intake disorder. Nutrients. 2019;11(9). https://doi.org/10.3390/nu11092013.
Greenblatt JM, Delane DD. Zinc supplementation in anorexia nervosa. J Orthomol Med. 2018;33(1). https://isom.ca/article/zinc-supplementation-anorexia-nervosa/.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs Allison Nitsch, Jamie Manwaring, Erin Knopf, and Phil Mehler each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Adolescent Medicine
Rights and permissions
About this article
Cite this article
Nitsch, A., Knopf, E., Manwaring, J. et al. Avoidant/Restrictive Food Intake Disorder (ARFID): Its Medical Complications and Their Treatment—an Emerging Area. Curr Pediatr Rep 9, 21–29 (2021). https://doi.org/10.1007/s40124-021-00239-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-021-00239-8