Abstract
Purpose of Review
We reviewed recently published literature around the care of transgender and gender-nonconforming youth. In this nascent area of medicine, there are few randomized controlled trials, but there are treatment guidelines that include expert opinion and best practices for a more standardized approach to care.
Recent Findings
The most significant article published the past year is the updated standards of care—“Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline”—which establishes a care framework with special emphasis on the importance of interdisciplinary care. However, there are several other important articles that review health-care utilization and outcomes after treatment in the transgender population.
Summary
As gender dysphoria and nonconformity become more visible and prevalent, health-care providers will deliver care for these patients and will need to understand common health concerns and treatment options. The ability to provide culturally competent and appropriate care can improve psychosocial outcomes for these patients.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •Of importance, ••Of major importance
• Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender and gender-nonconforming people, version 7. Int J Transgend. 2012;13(4):165–232. Treatment guidelines from WPATH (World Professional Association for Transgender Health).
•• Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2017;102(11):3869–903. Most current guidelines for treatment of transgender persons
Flores AR, Herman JL, Gates GJ, Brown TNT. How many adults identify as transgender in the United States? The Williams Institute. 2016. Available at: https://williamsinstitute.law.ucla.edu/wp-content/uploads/How-Many-Adults-Identify-as-Transgender-in-the-United-States.pdf. Accessed May 8, 2018.
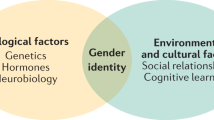
van Beijsterveldt CE, Hudziak JJ, Boomsma DI. Genetic and environmental influences on cross-gender behavior and relation to behavior problems: a study of Dutch twins at ages 7 and 10 years. Arch Sex Behav. 2006;35(6):647–58.
Human Rights Campaign. Growing up LGBT in America. In: May; 2012.
Kosciw JG, Greytak EA, Giga NM, Villenas C, Danischewski DJ. The 2015 National School Climate Survey: the experiences of lesbian, gay, bisexual, transgender, and queer youth in our nation’s schools. New York: GLSEN; 2016.
American Psychiatric Association. (2013). Gender dysphoria. In Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing, 2013; https://doi.org/10.1176/appi.books.9780890425596.dsm14.
Steensma TD, Biemond R, de Boer F, Cohen-Kettenis PT. Desisting and persisting gender dysphoria after childhood: a qualitative follow-up study. Clin Child Psychol Psychiatr. 2011;16(4):499–516.
Hoekzema E, Schagen SE, Kreukels BP, et al. Regional volumes and spatial volumetric distribution of gray matter in the gender dysphoric brain. Psychoneuroendocrinology. 2015 May;55:59–71.
Green R. Family co-occurrence of gender dysphoria: ten sibling or parent-child pairs. Arch Sex Behav. 2000;29:499–507.
Bao A-M, Swaab DF. Sexual differentiation of the human brain: relation to gender identity, sexual orientation and neuropsychiatric disorders. Front Neuroendocrinol. 2011;32:214–26.
Russell ST, Pollitt AM, Li G, et al. Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicide behavior among transgender youth. J Adolesc Health. 2018; https://doi.org/10.1016/j.jadohealth.2018.02.003.
• Rider GN, BJ MM, Gower AL, et al. Health and care utilization of transgender and gender nonconforming youth: a population-based study. Pediatrics. 2018;141(3):e20171683. This article reviews variability in health care use based on gender identity.
Grant J, Mottet L, Tanis J, et al. Injustice at every turn: a report of the national transgender discrimination survery. Washington DC: National Center for Transgender Equality and National Gay and Lesbian Task Force; 2011.
Connolly MD, Zervos MK, Barone CJ, et al. The mental health of transgender youth: advances in understanding. J Adolesc Health. 2016 Nov;59(5):489–95.
Reisner SL, Vetters R, Leclerc M, Zaslow S, Wolfrum S, Shumer D, et al. Mental health of transgender youth in care at an adolescent urban community health center; a matched retrospective cohort study. J Adolesc Health. 2015 Mar;56(3):274–9.
Haas A, Rodgers P, Herman J. Suicide attempts among transgender and gender non-conforming adults: findings of the National Transgender Discrimination Survey. Los Angeles: UCLA, Williams Institute and American Foundation for Suicide Prevention; 2014.
Olson J, Schrager SM, Belzer M, Simons LK, Clark LF. Baseline physiologic and psychosocial characteristics of transgender youth seeing care for gender dysphoria. J Adolesc Health. 2015 Oct;57(4):374–80.
Singh AA. Transgender youth of color and resilience: negotiating oppression and finding support. Sex Roles. 2013 Jun;68(11):690–702.
Janssen A, Huang H, Duncan C. Gender variance among youth with autism spectrum disorders: a retrospective chart review. Transgend Health. 2016;1:63–8.
Carswell J, Roberts S. Induction and maintenance of amenorrhea in transmasculine and nonbinary adolescents. Transgend Health. 2017;2(1):195–201.
Committee on Adolescent Health Care. Care for transgender adolescents. Committee Opinion No 685. Obstet Gynecol. 2017;129:e11–6.
Committee on Adolescent Health Care. Committee Opinion No. 668: menstrual manipulation for adolescents with physical and developmental disabilities. Obstet Gynecol. 2016;128:e20–5.
Ahmad S, Leinung M. The response of the menstrual cycle to initiation of hormonal therapy in transgender men. Transgend Health. 2017;2:176–9.
ACOG Committee Opinion No. 701 Summary: Choosing the route of hysterectomy for benign disease. Obstet Gynecol. 129(6):1149–1150.
Kailas M, Lu HMS, Rothman EF, Safer JD. Prevalence and types of gender-affirming surgery among a sample of transgender endocrinology patients prior to state expansion of insurance coverage. Endocr Pract. 2017;23(7):780–6.
Buncamper ME, van der Sluis WB, de Vries M, Witte BI, Bouman MB, Mullender MG. Penile inversion vaginoplasty with or without additional full-thickness skin graft: to graft or not to graft? Plast Reconstr Surg. 2017;139(3):649e–56e.
Cizek S, Nguyen N, Lyon L, Zaritsky E, Weiss E. Combined hysterectomy and mastectomy surgery for transgender patients in an integrated health care setting. Int J Transgend. 2017;18:382–8.
Obedin-Maliver J, Light A, de Haan G, Jackson RA. Feasibility of vaginal hysterectomy for female to male transgender men. Obstet Gynecol. 2017;129:457–63.
Capitan L, Simon D, Meyer T, et al. Facial feminization surgery: simultaneous hair transplant during forehead reconstruction. Plast Reconsty Surg. 2017;139(3):573–84.
Papadopulos NA, Zavlin D, Lelle JD, et al. Male to female sex reassignment surgery using the combined technique leads to increased quality of life in a prospective study. Plast Reconstr Surg. 2017;140(2):286–94.
Wiepejes CM, Nota NM, de Blok CJM, et al. The Amsterdam cohort of gender dysphoria study (1972-2015): trends in prevalence, treatment and regrets. J Sex Med. 2018;15(4):582–90.
Milrod C. How young is too young: ethical concerns in genital surgery of the transgender MTF adolescent. J Sex Med. 2014;11(2):338–46.
Olson-Kennedy J, Warus J, Okonta V, et al. Chest reconstruction and chest dysphoria in transmasculine minors and young adults—comparisons of nonsurgical and postsurgical cohorts. JAMA Pediatr. 2018; https://doi.org/10.1001/jamapediatrics.2017.5440.
Finlayson C, Johnson E, Chen D, et al. Proceedings of the working group session on fertility preservation for individuals with gender and sex diversity. Transgend Health. 2016;1:99–107.
Wierckx K, Caenegem E, Pennings G. Reproductive wish in transsexual men. Hum Reprod. 2012;27:483–7.
De Roo C, Tilleman K, T’Sjoen G, et al. Fertility options in transgender people. Int Rev Psychiatry. 2016;28:112–9.
Nahata L, Tishelman AC, Caltabellotta NM, Quinn GP. Low fertility preservation utilization among transgender youth. J Adolsc Health. 2017 Jul;61(1):40–4.
Chen D, Simons L, Johnson E, et al. Fertility preservation for transgender adolescents. J Adolesc Health. 2017;6:120–3.
Strang J, Jarin J, Call D, et al. Transgender youth fertility attitudes questionnaire: measure development in nonautistic and autistic transgender youth and their parents. J Adolesc Health. 2018 Feb;62(2):128–35.
Chen D, Matson M, Macapagal K, et al. Attitudes toward fertility and reproductive health among transgender and gender-nonconforming adolescents. J Adolesc Health. 2018; https://doi.org/10.1016/j.jadohealth.2017.11.306.
•• Owen-Smith AA, Gerth J, Sineath RC, et al. Association between gender confirmation treatments and perceived gender congruence, body image satisfaction, and mental health in a cohort of transgender individuals. J Sex Med. 2018;15(4):591–600. Larger study of the correlation between medical intervention and outcomes for transgender adults.
• de Vries AL, McGuire JK, Steensma TD, et al. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics. 2014;134(4):696–704. First description of transition outcomes for transgender youth
• Ryan C, Russell ST, Huebner D, et al. Family acceptance in adolescence and the health of LGBT young adults. J Child Adolesc Psychiatr Nurs. 2010;23(4):205–13. Description of best practices for suicide prevention in sexual minority youth.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Adolescent Medicine
Rights and permissions
About this article
Cite this article
Conard, L.A.E., Corathers, S.D. & Trotman, G. Caring for Transgender and Gender-Nonconforming Youth. Curr Pediatr Rep 6, 139–146 (2018). https://doi.org/10.1007/s40124-018-0173-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-018-0173-8