Abstract
Introduction
This study evaluated the cost-effectiveness of anti-vascular endothelial growth factor (VEGF) therapies for subtypes of neovascular age-related macular degeneration (nAMD) from the societal perspective, and for any nAMD from the patient perspective in Japan.
Methods
A Markov model was developed to simulate the lifetime transitions of a cohort of patients with nAMD through various health states based on the involvement of nAMD, the treatment status, and decimal best-corrected visual acuity. Ranibizumab biosimilar was compared with aflibercept from the societal perspective regardless of treatment regimen for the analysis of three subtypes (typical nAMD, polypoidal choroidal vasculopathy (PCV), and retinal angiomatous proliferation (RAP)). Two analyses from the patient perspective focusing on the treat-and-extend regimens were performed, one with a cap on patients’ copayments and one without. Ranibizumab biosimilar was compared with branded ranibizumab, aflibercept, aflibercept as the loading dose switching to ranibizumab biosimilar during maintenance (aflibercept switching to ranibizumab biosimilar), and best supportive care (BSC), for patients with any nAMD.
Results
In the subtype analyses, ranibizumab biosimilar when compared with aflibercept resulted in incremental quality-adjusted life years (QALYs) of − 0.015, 0.026, and 0.009, and the incremental costs of Japanese yen (JPY) − 50,447, JPY − 997,243, and JPY − 1,286,570 for typical nAMD, PCV, and RAP, respectively. From the patient perspective, ranibizumab biosimilar had incremental QALYs of 0.015, 0.009, and 0.307, compared with aflibercept, aflibercept switching to ranibizumab biosimilar, and BSC, respectively. The incremental costs for ranibizumab biosimilar over a patient lifetime excluding the cap on copayment were estimated to be JPY − 138,948, JPY − 391,935, JPY − 209,099, and JPY − 6,377,345, compared with branded ranibizumab, aflibercept, aflibercept switching to ranibizumab biosimilar, and BSC, respectively.
Conclusions
Ranibizumab biosimilar was demonstrated as a cost-saving option compared to aflibercept across all subtypes of nAMD, irrespective of the perspectives considered.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Why carry out this study? |
Our previous study suggested that ranibizumab biosimilar was a dominant alternative over other widely used anti-vascular endothelial growth factor (VEGF) treatments in patients with neovascular age-related macular degeneration (nAMD) from the societal perspective in Japan. |
Cost-effectiveness studies featuring both analysis on the treatment of the subtypes of nAMD with ranibizumab biosimilar and analyses including the patient perspective have not yet been conducted in Japan. |
This study aimed to evaluate the cost-effectiveness of anti-VEGF therapies for treating (a) the subtypes of nAMD from the societal perspective and (b) any nAMD from the patient perspective in Japan. |
What was learned from the study? |
Ranibizumab biosimilar was demonstrated as a cost-saving option compared to aflibercept across all subtypes of nAMD from both the patient and societal perspectives. |
The results from this study can help optimize the cost-effectiveness of the most preferred treatment strategies for elderly patients with nAMD, from the perspective of each stakeholder involved in the Japanese healthcare system. Furthermore, these results may contribute to future policy decisions related to biosimilars. |
Introduction
Anti-vascular endothelial growth factor (VEGF) therapy is the most effective method for the treatment of neovascular age-related macular degeneration (nAMD). In Japan, the two most commonly used anti-VEGF agents are ranibizumab (RBZ) (Lucentis®; Novartis Pharma, Japan) and aflibercept (AFL) (Eylea®; Bayer Yakuhin, Japan) [1]. Additionally, brolucizumab (Beovu®) and faricimab (Vabysmo®) are anti-VEGF agents that were recently approved in Japan. In 2021, a ranibizumab biosimilar (RBZ BS) (Senju Pharmaceuticals, Japan) was approved in Japan for the treatment of nAMD. Biosimilars of ranibizumab have shown similar efficacy, safety, and immunogenicity to Lucentis® in Japan, as well as across other Asian and European countries [2,3,4,5,6,7]. Our previous study showed that RBZ BS could be a cost-effective treatment alternative to other anti-VEGF agents as well as best supportive care (BSC) for patients with any type of nAMD in Japan [8].
However, there are two major gaps in knowledge that must be addressed. First, although the effects of anti-VEGF agents may vary by nAMD subtype [9], cost-effectiveness studies on the subtypes of nAMD are yet to be conducted anywhere globally. There are three major subtypes of nAMD which are classified according to clinical features, that is typical nAMD, polypoidal choroidal vasculopathy (PCV), and retinal angiomatous proliferation (RAP) [10,11,12]. According to the previous retrospective study conducted in Japan [10], 54.7% had PCV, followed by 35.3% with typical nAMD and 4.5% with RAP. As such, it is imperative to perform a cost-effectiveness analysis of anti-VEGF therapies for each nAMD subtype.
Second, with the rapid transformation of healthcare delivery [13], it is crucial to assess cost-effectiveness not only from the societal standpoint but from the patient perspective to ensure the sustained delivery of care to patients. In Japan, all residents must enroll in one of the public health insurance systems and patients bear the copayment costs for treatments where rates vary by age [14]. The two most common systems are (1) the National Health Insurance for retired persons, the self-employed, and their dependents and (2) the Employee Health Insurance for employees and their dependents. When an individual reaches the age of 75 years, they become eligible for the Advanced Elderly Medical Service System which became available in 2008. With this system, patient copayments in households at standard income levels decrease to 10% [14]. More specifically, in the Japanese healthcare system, copayments are age-specific, meaning copayment rates vary across the patient’s lifetime. The copayment rates are 30%, 20%, and 10% of the total medical costs for patients < 70 years, 70–74 years, and ≥ 75 years, respectively [15]. Additionally, a cap on monthly copayment spending (High-Cost Medical Expense Benefit System) is applied in Japan, which is a policy to reduce monthly copayments for patients. For households at standard income levels, the cap is JPY 80,100 and JPY 18,000 for patients aged ≤ 69 years and ≥ 70 years if medical expenses do not exceed 267,000 yen per month, respectively [16]. In previous economic evaluations of treatment strategies for nAMD, most studies reported from a third-party payer perspective and some from a societal perspective, but none included a patient perspective [17].
The societal perspective analysis can help guide policy makers in developing social healthcare policy. On the other hand, the patient perspective can be used to measure the impact on copayments, which are dependent on the age of the patient in the current Japanese health insurance system. Thus, this study aims to address these gaps in knowledge by providing an economic evaluation considering the treatment strategies for the nAMD subtypes from the societal perspective and offering a comparison of anti-VEGF therapies from the patient perspective. More specifically, there are two objectives in this study: (1) to assess the cost-effectiveness of RBZ BS compared with AFL in patients with nAMD by subtype from the Japanese societal perspective and (2) to assess the cost-effectiveness of anti-VEGF therapies in Japan, focusing on RBZ BS, in patients with any type of nAMD from the patient perspective.
Methods
Model Overview
The key parameters of the model structure were developed after face-to-face and online meetings among experts in retinal diseases (YY, KT, TI, FG, and TS) as in the previous study [8].
A Markov state-transition cohort model which simulates the transition of a cohort of patients with nAMD through health states based on the involvement of nAMD (single-eye vs. both-eye involvement), the treatment status of the patients (i.e., on- or off-treatment), and decimal best-corrected visual acuity was used. The details of the model structure including a description of the primary health states, sub-health states, and health transitions within sub-health states are described in our previous study [8]. The three key assumptions from this study (discontinuation of the assigned treatment according to pre-defined rates, a maximum anti-VEGF treatment period of 5 years, and following the same course as BSC after stopping treatment) were the same as in the previous study [8].
General Settings
The model considered a cycle length of 3 months, and a time horizon of 20 years which covered patient lifetimes [18] based on the mean age of the patient population (74 years [19]) in Japan. A discount rate of 2.0% per year was applied to health outcomes and costs based on local guidelines [20].
This study included two objectives and the details of the analysis settings used for each comparison are summarized in Table 1.
Objective 1: Subtype Analysis
Target Population
The target population consisted of patients with each of the nAMD subtypes including (a) typical nAMD (including all types of choroidal neovascularization (CNV) and RAP), (b) PCV, and (c) RAP.
Interventions and Comparators
For objective 1, the cost-effectiveness model compared RBZ BS with AFL (i.e., Eylea®).
Baseline Characteristics
The baseline characteristics including the initial distribution of sub-health states in patients with each nAMD subtype were informed by a previous epidemiological study conducted among Japanese patients [9] (Supplementary Tables S1 and S2).
Clinical Inputs
A targeted literature review was performed to extract the clinical parameters of the nAMD subtypes from the MEDLINE and Embase databases (access via the OVID interface) and the Cochrane Central Register of Controlled Trials for studies published from January 2005 to October 2022 (search strategies in Supplementary Tables S3 and S4). Following this review, no randomized controlled trial was identified which compared RBZ to AFL among each nAMD subtype. Thus, the clinical parameters were inferred on the basis of previous head-to-head observational studies or a retrospective matched cohort study.
In the base case, an observational cohort study in Japan examining patients with each nAMD subtype conducted by the Japanese Clinical Retinal Study (J-CREST) Group [9] was selected for the transition probabilities and treatment frequencies of all subtypes in year 1. For typical nAMD and PCV in years ≥ 2, data from a matched-cohort analysis in Korea (the Bundang AMD cohort study) [21] were adopted as it entails a head-to-head comparison of RBZ versus AFL among each nAMD subtype with up to 4 years of follow-up. It is important to note that the Bundang study [21] defined typical nAMD as nAMD other than PCV (i.e., classic CNV, occult CNV, and RAP). Furthermore, the choice between the pro re nata and treat-and-extend (TAE) regimens was dependent on the preference of the physicians in the Bundang study. Therefore, the analysis for typical nAMD and PCV was conducted regardless of the treatment regimen. For the RAP subtype, data from a study at Gunma University in Japan investigating patients with RAP [22] and the CANTREAT Study conducted in Canada investigating the long-term effectiveness of ranibizumab in patients with nAMD [23] were used for the transition probabilities in year 2 and years 3–5, respectively (Supplementary Table S5). The treatment frequencies were based on data from J-CREST [9] (for year 1) and Gunma University [22] (for years ≥ 2) (Supplementary Table S6). As a result of a lack of subtype-specific data, incidence rates of fellow-eye involvement, monitoring frequencies, incidence rates of adverse events (AEs), annual discontinuation rates, and AE-specific disutilities were assumed to be analogous among subtypes as in the previously published analysis [8]. To explore the uncertainty of the clinical inputs, scenario analyses were conducted in which transition probabilities and treatment frequencies were obtained from the Bundang study [21] for typical nAMD and PCV, and Gunma University [22] for RAP in year 1 (Supplementary Tables S7 and S8).
Objective 2: Patient Perspective
Target Population
The target population for objective 2 was patients with any type of nAMD.
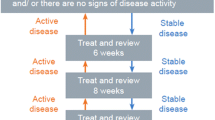
Interventions and Comparators
For objective 2, treatment regimens for anti-VEGF administrations were considered and data on the TAE regimen were adopted for the relevant input parameters, which were consistent with our previous study [8]. Therefore, RBZ BS TAE was compared with Lucentis® (RBZ TAE), AFL TAE, AFL as the loading dose (i.e., induction phase) switched to RBZ BS TAE in the maintenance phase (AFL to RBZ BS TAE), and BSC (regular follow-up with ophthalmological examinations only). The dosing schedule of each treatment strategy was as previously described [8].
Baseline Characteristics
For analysis from the patient perspective in objective 2, two starting ages of the patients were considered: 74 years (base case analysis) and 65 years (scenario analysis) to account for age-dependent differences in patient copayment rates. Other baseline characteristics of the patients were the same as in the previously published analysis [8].
Clinical Inputs
The same clinical parameters including transition probabilities, treatment and monitoring frequencies, annual incidence of fellow-eye involvement, annual discontinuation rates, utilities, and incidence of AEs were assumed as in the previously published study [8]. To explore the uncertainties of the transition probabilities and treatment frequencies in the analysis, two different sets of parameters were considered based on either a head-to-head comparison study (RIVAL study conducted in Australia [24] for the base case analysis) or on an indirect treatment comparison using randomized controlled trials [19] for the scenario analysis between RBZ TAE and AFL TAE and conducted in the same manner as in our previous study [8]. Furthermore, another scenario analysis with the starting age of patients set at 65 years was also conducted.
Cost Inputs
All costs were reported in Japanese yen (JPY) and were obtained from the Japanese medical service fee schedule, revised in June 2024 [25].
Objective 1: Subtype Analysis
The costs were included from the societal perspective as previously described [8] and included direct medical costs (drug administration, monitoring, and AEs), and the societal costs related to accompanying a patient to a physician’s office or related to daily care. Drug administration costs, resource utilization for each AE, and costs of AEs were as described in our previous study [8] (Supplementary Table S9). Costs related to monitoring and disease management and the societal costs related to accompanying a patient to a physician’s office or related to daily care are shown in Supplementary Tables S10 and S11.
Objective 2: Patient Perspective
In the analysis from the patient perspective, copayments were considered instead of the total direct medical costs reimbursed by the public payer, while the other societal costs remained the same as in the previous analysis from the societal perspective [8]. For patients entering the model at 74 years of age, copayments reduce to 10% after 1 year of treatment according to the age-specific copayment. Similarly, for patients starting at 65 years of age, copayment reduces by 10% after the fifth year and then again after the tenth year. Since the model cycle length was 3 months, the cap on copayment was applied if the 3-month averaged copayment amount exceeded the threshold.
Compliance with Ethics Guidelines
This study is based on data from previously conducted studies and does not contain any novel data from human participants. Therefore, this study complies with ethical guidelines and did not require an ethics review.
Analysis
This cost-effectiveness analysis estimated the costs and health outcomes of each intervention and comparator. The estimated cost per patient for each treatment strategy was the sum of the costs associated with each health state multiplied by the probability of a patient being in that health state at each point in time (i.e., each model cycle). A half cycle correction was applied to the cycle length of 3 months. The cost-effectiveness of each treatment strategy was determined by the ratio of the average cost per patient and the health benefits it brings, resulting in a cost per quality-adjusted life year (QALY) gained. The incremental cost-effectiveness ratio (ICER) was determined by calculating the differences in costs per QALY gained between the treatment strategies. A willingness-to-pay (WTP) threshold of JPY 5,000,000 per QALY gained was used for this cost-effectiveness analysis [26].
The probability sensitivity analysis (PSA) was conducted for the subtype analysis in objective 1 through Monte Carlo simulation with 10,000 iterations. Similar parameter distributions were used as in our previous study [8].
Results
Objective 1: Subtype Analysis
Base Case Results
In this analysis, treatment with RBZ BS and AFL accumulated a total of 7.529 and 7.544 QALYs for typical nAMD, 8.142 and 8.115 for PCV, and 4.994 and 4.984 for RAP, respectively (Table 2). RBZ BS resulted in incremental QALYs of − 0.015, 0.026, and 0.009 compared with AFL for typical nAMD, PCV, and RAP, respectively. The total respective costs associated with RBZ BS and AFL over a lifetime were JPY 23,994,476 and JPY 24,044,923 for typical nAMD, JPY 24,303,915 and JPY 25,301,158 for PCV, and JPY 24,413,899 and JPY 25,700,469 for RAP. The incremental costs associated with RBZ BS were JPY − 50,447, JPY − 997,243, and JPY − 1,286,570 compared with AFL for typical nAMD, PCV, and RAP, respectively. In all subtypes, costs were consistently lower with RBZ BS than with AFL while QALYs were similar for both treatments.
Although RBZ BS had lower drug and administration costs than AFL for typical nAMD (JPY − 506,963), the increased societal costs due to daily care were higher for RBZ BS than for AFL (JPY 475,105), which was the main reason for the smaller difference in total costs compared to other subtypes (Table 2). In the base case of typical nAMD, efficacy inputs were derived from the J-CREST study [9] and the Bundang AMD cohort study [21] for year 1 and years ≥ 2, respectively. The decline in visual acuity from baseline was higher for RBZ than AFL, resulting in the increased societal costs due to daily care in RBZ. The reduced total cost of RBZ BS relative to AFL mainly resulted from lower drug and administration costs in PCV (JPY − 545,575) and RAP (JPY − 1,213,957) (Table 2).
Scenario Analysis Results
A scenario analysis using alternative transition probabilities and treatment frequencies in year 1 was conducted and the results are shown in Supplementary Table S12. Similar to the base case results, costs were consistently lower for RBZ BS than AFL across all subtypes (difference in total costs JPY − 537,347, JPY − 1,805,440, and JPY − 1,893,175 for typical nAMD, PCV and RAP, respectively), and only minor differences were observed in QALYs between the treatments (difference in QALYs 0.009, 0.062, and 0.014 for typical nAMD, PCV and RAP, respectively). In contrast to the base case result for typical nAMD, the decreased societal costs due to daily care in RBZ (JPY − 57,792) were due to the clinical inputs from the Bundang study [21], where the visual acuity increase from baseline was greater for RBZ than AFL in year 1, although visual acuity decline was higher in RBZ than AFL in years ≥ 2.
Objective 2: Patient Perspective
Base Case Results
The base case results were analyzed from the patient perspective where the patients’ starting age was 74 years. Compared with the brand drug Lucentis®, RBZ BS TAE incurred comparable QALYs (7.945) (Table 3). The total QALYs gained with AFL TAE, AFL to RBZ BS TAE, and BSC were 7.930, 7.936, and 7.638, respectively. The incremental QALYs associated with RBZ BS TAE were 0.015, 0.009, and 0.307 QALYs, compared with AFL TAE, AFL to RBZ BS TAE, and BSC, respectively.
The incremental costs for RBZ BS TAE over a patient lifetime excluding the cap on copayment were estimated to be JPY − 138,948, JPY − 391,935, JPY − 209,099, and JPY − 6,377,345, compared with RBZ TAE, AFL TAE, AFL to RBZ BS TAE, and BSC, respectively (Table 3). When the cap on copayment was included in the analysis, the total costs associated with all anti-VEGF therapies were reduced and therefore the incremental costs with RBZ BS TAE were also lower. The incremental costs with RBZ BS TAE were JPY − 81,469, JPY − 257,891, JPY − 186,227, and JPY − 6,408,395 compared with RBZ TAE, AFL TAE, AFL to RBZ BS TAE, and BSC, respectively (Table 3). Therefore, RBZ BS TAE was a dominant treatment alternative to all the comparators (except RBZ TAE) with higher QALYs and lower costs, irrespective of the cap on copayment.
Major contributors to total costs amongst all treatment strategies were the societal costs due to daily care followed by direct costs, except for BSC where direct costs were lower than societal costs due to physician visits (Table 3). The main driver of reduced total costs with RBZ BS TAE compared with RBZ TAE, AFL TAE, and AFL to RBZ BS TAE was direct costs, regardless of cap copayment. However, the magnitude of this difference reduced when the cap on copayment was applied (JPY − 138,948 vs. JPY − 81,469, JPY − 391,935 vs. JPY − 257,891, and JPY − 209,099 vs. JPY − 186,227 for RBZ TAE, AFL TAE, and AFL to RBZ BS TAE, respectively) (Table 3). On the other hand, the lower cost with RBZ BS TAE compared with BSC was largely driven by lower societal costs due to daily care (JPY − 6,856,930).
Scenario Analysis Results 1: Modeling with Patients’ Starting Age at 65 Years
A scenario analysis was conducted from the patient perspective where the starting age of the patients was considered as 65 years. The results are presented in Supplementary Table S13. Although the QALYs and costs of each anti-VEGF agent were higher than the base case (QALYs 9.700, 9.685, 9.690, and 9.357 for RBZ BS TAE and RBZ TAE, AFL TAE, AFL to RBZ BS TAE, and BSC; total costs JPY 29,268,724, JPY 29,682,401, JPY 30,044,074, JPY 29,507,113, and JPY 35,909,357 for RBZ BS TAE, RBZ TAE, AFL TAE, AFL to RBZ BS TAE, and BSC), which is due to starting at a younger age (65 years vs. 74 years for base case and scenario 1, respectively), the comparison results with the interventions were the same as in the base case. Thus, the results of the base case were found to be robust, i.e., RBZ BS TAE might be a more effective and less costly treatment alternative, irrespective of patients’ starting age.
Scenario Analysis Results 2: Clinical Inputs Using Data from the Previous Indirect Comparison Study
To explore the uncertainties of the clinical parameters, another scenario analysis was conducted using the data from the indirect treatment comparison in which the average number of injections for RBZ TAE was higher by 6.12 injections for 2 years compared to AFL TAE [19]. RBZ BS TAE was slightly higher in QALYs (0.0104 and 0.0005 for AFL TAE and AFL to RBZ BS TAE, respectively), and was associated with lower total costs compared with AFL TAE regardless of copayment (JPY − 73,761 and JPY − 97,817 with and without cap copayment, respectively) and AFL to RBZ BS TAE (JPY − 12,296 and JPY − 35,599 with and without cap copayment, respectively) (Supplementary Table S14). This analysis showed that the base case results remain unchanged and RBZ BS TAE was still a dominant treatment alternative over other comparators regardless of the clinical inputs parameters. Thus, the scenario analysis showed the robustness of the base case results.
Sensitivity Analysis Results
A cost-effectiveness plane was generated to illustrate the results of the PSA comparing RBZ BS to AFL for objective 1: subtype analysis (Figs. 1, 2 and 3). The results showed that 94.4% and 71.6% of the iterations were estimated in the southeast quadrant for PCV and RAP subtypes, respectively, implying that RBZ BS was likely to be dominant over AFL with the possible ranges of input parameters (± 20% of point estimates). For these nAMD subtypes, 0.1–0.5% of the iterations were estimated to be higher than the WTP threshold of JPY 5,000,000 per QALY gained. For typical nAMD, the majority of the iterations were estimated in the northwest or southwest (39.9% for both) quadrants. Moreover, 51.9% of the iterations were estimated to be higher than the WTP threshold of JPY 5,000,000 per QALY gained.
Discussion
This study conducted an economic analysis of anti-VEGF therapy in Japan and found that (1) ranibizumab biosimilar was less costly than aflibercept in all nAMD subtypes with only minor differences in QALYs from the societal perspective and (2) the ranibizumab biosimilar TAE regimen was a cost-saving treatment alternative to other anti-VEGF therapies (branded ranibizumab TAE, aflibercept TAE, and aflibercept switching to ranibizumab biosimilar TAE) and BSC, from the patient perspective. To the best of our knowledge, this study is the first economic evaluation of anti-VEGF therapy considering the subtypes of nAMD and patient copayments in the Japanese public health insurance systems.
Objective 1: nAMD Subtype Analysis
The subtype analysis conducted in this study found that across all subtypes of nAMD, treatment with ranibizumab biosimilar consistently incurred lower costs compared to treatment with aflibercept. In contrast, only minor differences in QALYs were observed between ranibizumab biosimilar and aflibercept using data from the base case or scenario analyses. This indicates that small changes in the model parameters can have an impact on the QALYs which is a key component for determining whether a treatment is dominant or not. Moreover, findings from the scenario analysis and probabilistic sensitivity analysis were relatively consistent with those from the base case analysis demonstrating that ranibizumab biosimilar can be a cost-saving treatment option for the treatment of all nAMD subtypes, indicating the robustness of the base case results.
Objective 2: Economic Evaluation from the Patient Perspective
From the patient perspective, our study found that the ranibizumab biosimilar TAE regimen was a dominant treatment alternative to other commonly available treatment options in Japan (with the exception of branded ranibizumab TAE). This was found to be true regardless of whether the cap on monthly copayments was applied. The ranibizumab biosimilar TAE regimen maintained dominance over other comparators in the scenario analysis where the patient starting age was 65 years, thus substantiating the base case results.
Anti-VEGF drugs are generally expensive and pose a significant financial burden to patients. According to the results of a survey of patients with rheumatoid arthritis [27], one of the most frequent requests from patients to medical institutions was for information on treatments and medications that would reduce their medical expenses. The results from this present study suggest that the use of ranibizumab biosimilar can lead to a reduction in medical costs for patients with nAMD. As it is known that patients prefer lower medical costs for their treatments, it may be prudent to consider treatment strategies that entail switching to a less expensive biosimilar after a disease is properly observed using branded drugs during the induction phase [28]. Additionally, in order to maintain a sustainable social security system, the Japanese government is promoting the use of biosimilars and formulary formulation [29, 30], and the insights from this study can contribute to decisions related to the policymaking for these drugs.
There are some limitations to this study. Firstly, the modeling approach has inherent limitations due to uncertainties regarding some of the parameters resulting from the lack of data available in the Japanese clinical settings. The first parameter was discontinuation rates, which were assumed to be the same for all treatments. Additionally, the assumption of 0.1 utility reduction for blindness compared to no visual impairment for the visual acuity of the worst-seeing eye in the single-eye involvement was made. Finally, for the productivity loss of caregivers due to daily care which was based on the severity of visual impairment was determined by the experts in the field. These limitations were further detailed in our previous analysis [8]. Second, there was a lack of high-quality data for the clinical input parameters, unbiased data with long-term follow-up of Japanese patients with nAMD, and data from randomized controlled trials with direct comparisons for the nAMD subtype analysis. The parameter values of the number of treatments after year 3 for PCV were taken directly from a multicenter study conducted in Korea [21], which was the most comprehensive study with real-world data focusing on the outcomes of ranibizumab and aflibercept for PCV with a long follow-up period available at the time. Unfortunately, there were no comparative studies conducted in Japan. Third, it is also expected that future results might be affected by changes in the proportion of copayments for medical expenses in Japan as a result of a review of the benefits and burdens in the medical insurance system [31], as well as drug price revisions [32]. Fourth, the decreased direct medical costs applied to the cap on copayment could be underestimated in the analysis from the patient perspective. Lastly, the current analysis focused only on ranibizumab and aflibercept which are the two most commonly used anti-VEGF agents in Japan. Brolucizumab (Beovu®) and faricimab (Vabysmo®) are anti-VEGF agents which have recently received approval in Japan. These drugs were not included in this analysis, however, as a result of the lack of sufficient studies to make assumptions at the same level of reliability as ranibizumab and aflibercept.
Conclusion
Ranibizumab biosimilar was demonstrated as a cost-saving option compared to aflibercept across all subtypes of nAMD from all perspectives considered. The results from this study can aid in optimizing cost–benefit analyses for the most preferred treatment strategies among the available options for elderly patients with nAMD from the perspective of each stakeholder involved in the Japanese healthcare system. Furthermore, these results can contribute to future policymaking decisions related to biosimilars.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
References
National Database of Health Insurance Claims and Specific Health Checkups of Japan (NDB). Quantity by drug class in NDB Open Data, Date of medical treatment: April 2021 to March 2022 injection medicine outpatient (in-hospital) (in Japanese) 2021. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000177221_00012.htmlAccessed 20 Dec 2023.
Chakraborty D, Mondal S, Boral S, et al. Biosimilar versus innovator molecule of ranibizumab in neovascular age-related macular degeneration (The BALANCE Trial): real-world evidence. Clin Ophthalmol. 2023;17:1067–76.
Loewenstein A, Czumbel N, Ernest J, Dusová J, Pearlman J, Nowosielska A. Randomized trial of biosimilar XSB-001 versus reference ranibizumab in patients with neovascular age-related macular degeneration. Ophthalmol Retina. 2023;7(9):753–61.
Bressler NM, Veith M, Hamouz J, et al. Biosimilar SB11 versus reference ranibizumab in neovascular age-related macular degeneration: 1-year phase III randomised clinical trial outcomes. Br J Ophthalmol. 2023;107(3):384–91.
Holz FG, Oleksy P, Ricci F, et al. Efficacy and safety of biosimilar FYB201 compared with ranibizumab in neovascular age-related macular degeneration. Ophthalmology. 2022;129(1):54–63.
Yoon CK, Oh J, Bae K, Park UC, Yu KS, Yu HG. Efficacy and safety of a new ranibizumab biosimilar CKD-701 using a pro re nata treatment regimen in neovascular age-related macular degeneration: a phase 3 randomized clinical trial. PLoS ONE. 2022;17(11):e0275611.
Kondo M, Ogura Y, Takahashi K, et al. Phase III clinical trial to verify the equivalence between ranibizumab (genetic recombination) biosimilar (SJP-0133) and a ranibizumab reference product in patients with wet age-related macular degeneration and evaluate the long-term safety and efficacy of SJP-0133. J Eye. 2022;39(10):1421–34.
Yanagi Y, Takahashi K, Iida T, et al. Cost-effectiveness analysis of ranibizumab biosimilar for neovascular age-related macular degeneration in Japan. Ophthalmol Ther. 2023;12(4):2005–21.
Yoneda K, Takeuchi M, Yasukawa T, et al. Anti-VEGF treatment strategies for 3 subtypes of neovascular age-related macular degeneration in a clinical setting: a multicenter cohort study in Japan. Ophthalmol Retina. 2023;7(10):869–78.
Maruko I, Iida T, Saito M, Nagayama D, Saito K. Clinical characteristics of exudative age-related macular degeneration in Japanese patients. Am J Ophthalmol. 2007;144(1):15–22.
Singerman LJ, Brucker AJ, Jampol LM, et al. Neovascular age-related macular degeneration: roundtable. Retina. 2005;25(7 Suppl):S1–S22.
Yannuzzi LA, Negrão S, Tomohiro I, et al. Retinal angiomatous proliferation in age–related macular degeneration. Retina. 2012;32:416–34.
Ministry of Health, Labor and Welfare (MHLW). [Medical insurance system reform for Japan 2022] (in Japanese). https://www.mhlw.go.jp/content/12401000/001022176.pdf. Accessed 20 Dec 2023.
Ministry of Health, Labor and Welfare (MHLW). [Overview of medical service regime in Japan]. https://www.mhlw.go.jp/bunya/iryouhoken/iryouhoken01/dl/01_eng.pdf. Accessed 20 Dec 2023.
Ministry of Health, Labor and Welfare (MHLW). [Out-of-pocket medical expenses] (in Japanese) [updated 9 December 2022]. https://www.mhlw.go.jp/bunya/shakaihosho/iryouseido01/info02d-37.html. Accessed 20 Dec 2023.
Ministry of Health, Labor and Welfare (MHLW). [High-cost medical expense benefit] (in Japanese) [updated 9 December 2022]. https://www.mhlw.go.jp/content/000333279.pdf. Accessed 20 Dec 2023.
Schmier JK, Hulme-Lowe CK. Cost-effectiveness models in age-related macular degeneration: issues and challenges. Pharmacoeconomics. 2016;34(3):259–72.
Ministry of Health, Labor and Welfare (MHLW). [Abridged life table for Japan 2021] [updated 29-Jul-2022]. https://www.mhlw.go.jp/toukei/saikin/hw/life/life21/index.html. Accessed 20 Dec 2023.
Ohji M, Lanzetta P, Korobelnik JF, et al. Efficacy and treatment burden of intravitreal aflibercept versus intravitreal ranibizumab treat-and-extend regimens at 2 years: network meta-analysis incorporating individual patient data meta-regression and matching-adjusted indirect comparison. Adv Ther. 2020;37(5):2184–98.
Center for Outcomes Research and Economic Evaluation for Health- National Institute of Public Health (C2H Japan). Guideline for Preparing Cost-Effectiveness Evaluation to the Central Social Insurance Medical Council. Version 3 2022 [updated 19-Jan-2022]. http://c2h.niph.go.jp/tools/guideline/guideline_ja.pdf. Accessed 20 Dec 2023.
Jin KW, Kim JH, Park JY, et al. Long-term outcomes of ranibizumab vs. aflibercept for neovascular age-related macular degeneration and polypoidal choroidal vasculopathy. Sci Rep. 2021;11(1):14623.
Hoshino J, Matsumoto H, Morimoto M, Mukai R, Nakamura K, Akiyama H. Comparison of aflibercept and ranibizumab therapies using treat-and-extend regimen for retinal angiomatous proliferation. J Jpn Ophthalmol Soc. 2020;124(8):628–36.
Kertes PJ, Sheidow T, Williams G, Greve M, Galic IJ, Baker J. Long-term efficacy of a treat-and-extend regimen with ranibizumab in patients with neovascular age-related macular disease: an open-label 12-month extension to the CANTREAT study. Ophthalmologica. 2021;245(3):230–8.
Gillies MC, Hunyor AP, Arnold JJ, et al. Macular atrophy in neovascular age-related macular degeneration: a randomized clinical trial comparing ranibizumab and aflibercept (RIVAL study). Ophthalmology. 2020;127(2):198–210.
Ministry of Health, Labor and Welfare (MHLW). [Regarding the revision of physician fee schedule in fiscal year 2024 (Reiwa-6 Nendo)] (in Japanese). https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000188411_00045.html. Accessed 29 Mar 2024.
Hasegawa M, Komoto S, Shiroiwa T, Fukuda T. Formal implementation of cost-effectiveness evaluations in Japan: a unique health technology assessment system. Value Health. 2020;23(1):43–51.
Yamanaka H, Ogawa Y. Survey on the actual situation of rheumatoid arthritis patients using a patient panel, Part 3: current status of employment, medical expenses, and information collection. Pharma Medica. 2011;29(11)
Hutton DW, Glassman AR, Liu D, Sun JK. Cost-effectiveness of aflibercept monotherapy vs bevacizumab first followed by aflibercept if needed for diabetic macular edema. JAMA Ophthalmol. 2023;141(3):268–74.
Ministry of Health, Labor and Welfare (MHLW). [Regarding the basic policy for the fourth stage of medical cost optimization] (in Japanese) 2023. https://www.mhlw.go.jp/content/12401000/001114696.pdf. Accessed 20 Dec 2023.
Ministry of Health, Labor and Welfare (MHLW). [Government policy regarding biosimilars] (in Japanese) 2022. https://www.mhlw.go.jp/content/001095684.pdf. Accessed 20 Dec 2023.
Ministry of Health, Labor and Welfare (MHLW). [Changes in counter burden ratio for elderly people in later stages of life, regarding the 2021 law revision] (in Japanese) 2022. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/iryouhoken/newpage_21060.html. Accessed 20 Dec 2023.
Ministry of Health, Labor and Welfare (MHLW). [Regarding Reiwa 6-nen drug price revision] (in Japanese) 2023. https://www.mhlw.go.jp/content/12404000/001110566.pdf. Accessed 15 Mar 2024.
Medical Writing/Editorial Assistance
The authors would like to acknowledge Anshika Singhal and Saurabh Trikha from IQVIA India for their support with medical writing and editing. We would also like to acknowledge Louis Patrick Watanabe, Karin Matsumoto, and Koki Idehara from IQVIA Solutions Japan G.K. for their support regarding writing the manuscript and data analysis. All medical writing and data analysis activities were funded through Senju Pharmaceutical Co., Ltd.
Funding
This study and the journal’s Rapid Service Fee were funded by Senju Pharmaceutical Co., Ltd.
Author information
Authors and Affiliations
Contributions
Yasuo Yanagi, Kanji Takahashi, Tomohiro Iida, Fumi Gomi, Hiroshi Onishi, and Taiji Sakamoto were involved in the conception and design, interpretation of the data and critical revision for intellectual content, and final approval of the version to be published. Junko Morii was involved in the conception and design, interpretation of the data, drafting of the paper, and final approval for publication. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
Yasuo Yanagi, Kanji Takahashi, Tomohiro Iida, Fumi Gomi and Taiji Sakamoto report honorarium from Senju during the conduct of the study. Yasuo Yanagi reports financial support from—Alcon Japan, Sanbio; consultant—Chugai, Roche, Boehringer Ingelheim, Bayer; lecturer—Chugai, Novartis, Bayer, Santen, Boehringer Ingelheim, Senju. Kanji Takahashi reports consultant for—Novartis, Bayer, Kyowa Kirin, Santen, Allergan; lecture fees—Novartis, Bayer, Santen, Senju. Tomohiro Iida reports consultant for—Bayer, Novartis, Chugai, Boehringer Ingelheim; lecture fees and grant support—AMO, Alcon, Bayer, Canon, HOYA, Nikon, Nidek, Novartis, Otsuka, Pfizer, Santen, Senju, and Topcon outside the submitted work. Fumi Gomi reports honorarium from—Bayer, Chugai, Kyowa Kirin, Novartis, Santen, Senju; support for attending meetings and/or travel—Bayer, Chugai, Novartis, Santen, Senju. Taiji Sakamoto reports appointment as a consultant & advisory board—Bayer, Boehringer Ingelheim, Novartis, Chugai, Senju, Santen. Hiroshi Onishi is an employee of Senju. Junko Morii is an employee of IQVIA, which was contracted by Senju to perform the analyses.
Ethical Approval
This study is based on data from previously conducted studies and does not contain any novel data from human participants. Therefore, this study complies with ethical guidelines and did not require an ethics review.
Additional information
Prior Presentation: The 77th Annual Congress of Japan Clinical Ophthalmology, October 7, 2023, Japan. The 62nd Annual Meeting of Japanese Retina and Vitreous Society, November 24, 2023, Japan.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yanagi, Y., Takahashi, K., Iida, T. et al. Cost-effectiveness Analysis of Ranibizumab Biosimilar for Neovascular Age-Related Macular Degeneration and its Subtypes from the Societal and Patient Perspectives in Japan. Ophthalmol Ther (2024). https://doi.org/10.1007/s40123-024-01011-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40123-024-01011-z