Abstract
Introduction
This retrospective study explores the connection between preoperative patient risk factors, the experience of ophthalmology residents, and the outcomes of cataract surgeries performed at Hadassah Medical Center. It is hypothesized that with increased experience, residents may demonstrate greater proficiency in handling surgeries on higher-risk patients, potentially leading to improved surgical outcomes overall.
Methods
Data were examined from 691 consecutive cataract surgeries in 590 patients, conducted by ophthalmology residents at Hadassah Medical Center (January 2018 to February 2022). Demographics, surgeon experience, preoperative cataract risk assessment score, and pre- and postoperative corrected distance visual acuity (CDVA) were analyzed. The risk score was based on cataract density, previous vitrectomy, presence of phacodonesis, small pupil, extreme axial length (> 30 mm or < 21.5 mm) or abnormal axial length (26–30 mm), shallow anterior chamber (< 2.5 mm), poor patient cooperation, oral alpha-1 blocker use, diabetic retinopathy (DR), Fuchs endothelial dystrophy, and having one functioning eye. This study focused on the correlation of risk scores with residents’ surgical experience and surgical outcomes.
Results
As residents gained experience, surgeries on patients with at least one risk factor increased from 54% (first year) to 75% (second year; p < 0.001) and fluctuated between 75%, 82%, and 77% (third, fourth, and fifth years, respectively), with initial preoperative CDVA declining progressively. Despite handling more complex cases over time, the percentage of intraoperative complications per patient decreased with each year of residents’ experience (17%, 13%, 11%, 17%, 6%; respectively). Patients without any risk factor had higher postoperative CDVA than those with one or more risk factors (mean ± standard deviation [SD] in logMAR, 0.16 ± 0.26 vs. 0.27 ± 0.35; p < 0.001) and a higher percentage of CDVA improvement (63% vs. 57%, p = 0.016).
Conclusions
The use of a preoperative risk assessment scoring system to allocate surgeries to residents at varying experience levels may reduce the risk for surgical complications, thereby ensuring patient safety and providing residents with a gradual learning experience.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The study investigates the impact of ophthalmology residents’ experience on cataract surgery outcomes, addressing the need for improved patient safety and surgical efficiency in the face of increasing cataract prevalence and economic burden. |
The hypothesis was that greater experience levels among residents would enhance surgical outcomes and that systematic preoperative risk assessments could optimize surgeon–patient pairings. |
Increased experience in residents was associated with better outcomes in high-risk cataract surgeries, with fewer intraoperative complications. |
Strategic assignments based on preoperative risk evaluations can improve patient outcomes, suggesting that the integration of these assessments into surgical training may be beneficial. Sensitivity analyses confirmed the study’s findings, supporting the reliability of the conclusions drawn. |
The study’s outcomes highlight the potential for experience-based task assignments to serve as a model for improving the educational curriculum of ophthalmology residents, potentially influencing policy decisions in clinical training programs. |
Introduction
More than 20 million cataract surgeries are performed annually worldwide [1,2,3]. While generally safe, serious complications can arise, prompting ongoing efforts to increase the safety of this procedure and enhance surgical outcomes [4]. The experience level of ophthalmology residents has been a topic of interest in relation to the occurrence of complications during cataract surgeries [5,6,7,8,9,10,11]. Evidence from the United States highlights a link between resident participation and procedural success, showing that cases involving residents might have less improvement in visual acuity post-surgery and a higher likelihood of postoperative visual acuity falling below 20/40, associated with residents’ relative inexperience [5]. Additionally, research conducted in Finland involving the analysis of 14,520 cases suggests that complications decrease with increasing resident experience [6]. Notably, patients with established risk factors, such as pseudoexfoliation syndrome or small pupils, face a higher risk of complications. Early introduction of cataract surgery training for residents has been observed to reduce significant intraoperative complications in cataract surgeries performed by residents [7].
As part of ongoing efforts to enhance surgical outcomes, the utilization of risk stratification systems has gained prominence. For example, the New Zealand Cataract Risk Stratification (NZCRS) system shows promise in reducing complications when its scoring recommendations are followed [12].
Complication rates in cataract surgeries by residents vary widely, from 1.8 to 14.7% in different reports [5, 7, 10, 13,14,15,16,17,18,19,20,21,22]. The incidence of anterior capsule tears, for instance, ranges from 0.9 to 5.8%, while posterior capsule tears range from 0.4 to 6.4%. Additional complications include iris prolapse/trauma (0.3–2.7%), wound retraction/burn (up to 2.4%), dropped lens fragment (from 0.1 to 2.1%), vitreous loss/vitreous in the anterior chamber (from 0.3 to 7.6%), and other complications (from 0.6 to 3.7%). Reports of resident-performed cataract surgery often exclude cases with challenging preoperative conditions or those at high risk for surgical complications. Additionally, subcategorization of published data to minor and major complications may not consistently align with the overall assessment [15, 19, 20, 22].
In an attempt to improve patient safety and visual outcomes for cataract surgeries performed by residents, we are allocating cases to residents based on their level of surgical experience and a preoperative risk assessment.
This study is designed to assess how case allocation based on preoperative risk assessments and residents’ surgical experience levels affects the frequency of complications and the overall quality of surgical outcomes in cataract operations. It further investigates how preoperative risk factors, including existing medical conditions and ocular characteristics, influence surgical success when surgeries are performed by ophthalmology residents. By analyzing these elements in conjunction with the surgeons’ level of experience, we aim to determine whether and how exposure to varying risk scenarios shapes surgical proficiency. Ultimately, our research strives to uncover strategies that reduce risks and enhance the quality of outcomes in cataract surgery, thereby advancing patient safety and the educational framework for ophthalmology residents.
Methods
Setting: Tertiary referral center.
Participants
Retrospective data from January 2018 to February 2022 were gathered from Hadassah Medical Center’s ophthalmology department. The study included 691 sequential cataract surgery patients operated on by residents, excluding those without a pre-cataract score and missing data.
In Israel, ophthalmology residency spans 5 years. Residents in our program start performing surgeries in their sixth month of residency, and their operating experience is quantified in months from this point. High-risk patients were operated on by more experienced residents or senior surgeons. The study was approved and performed in accordance with the institutional Helsinki committee of Hadassah Medical Center (study # HMO-0459-18). The committee exempts retrospective research from informed consent by the participants. Data were collected from the Ophthalmology Department database and anonymized before analysis. This study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments.
Risk Factors of Study Participants
The pre-cataract risk assessment, adapted from the Buckinghamshire Healthcare NHS Trust model [23], evaluated 12 factors including age (< 80 years: 0; 80–90 years: 1; > 90 years: 2), axial length (< 21.5 mm: 2; 21.5–26 mm: 0; 26–30 mm: 1; > 30 mm: 2), dense cataract (0 or 3), diabetic retinopathy (0 or 1), and Fuchs endothelial dystrophy (0 or 1). Other factors are oral alpha-1 antagonist use (0–2), phacodonesis (0 or 3), prior vitrectomy/trauma (0 or 1), shallow anterior chamber (< 2.5 mm: 0 or 1), small pupil (0 or 2), poor cooperation (0 or 2), and “only eye” presence (0 or 2). Scores ranged between 0 (no risk) and 22 (maximal risk), with higher scores indicating increased risk for complications during surgery. In order to enhance resident training and patient care, the score was integrated into the electronic medical record (EMR) system based on existing literature. This aimed to improve educational programs, align resident performance with patient needs, and ensure optimal surgical outcomes.
Description of the Surgical Procedure
Phacoemulsification surgery follows a structured protocol, beginning with corneal incisions for access. Viscoelastic agents are introduced into the anterior chamber to stabilize the space, safeguard the corneal endothelium, and enhance instrument maneuverability. A continuous curvilinear capsulorhexis is performed on the anterior lens capsule for precise entry into the lens nucleus. Hydrodissection, involving the injection of balanced salt solution (BSS) beneath the lens capsule, facilitates nucleus mobilization for removal. The cataractous nucleus is then fragmented using ultrasound energy in phacoemulsification and aspirated. Subsequent steps include irrigation and aspiration to eliminate leftover cortical matter. The procedure concludes with the implantation of a foldable intraocular lens (IOL) in the capsular bag and the sealing or suturing of corneal incisions.
Surgical Complications
Operation reports were examined for intraoperative complications utilizing predefined search tags. Thirteen complications were evaluated, including anterior capsule (AC) or posterior capsule (PC) tear, vitreous loss, dropped lens, iris prolapse, zonular dehiscence, wound burn, hyphema, central Descemet’s membrane damage, dislocated intraocular lens (IOL), wound leakage requiring sutures, extracapsular cataract extraction (ECCE), and “other” complications. Each complication occurrence during surgery was documented.
Surgical Outcomes
Surgical outcomes were assessed by comparing pre- and post-surgery corrected distance visual acuity (CDVA in logMAR). The percentage of CDVA improvement from the initial CDVA was calculated by the following formula: (preCDVA − postCDVA)/preCDVA. Patients achieving functional CDVA, defined as post-surgery CDVA of less than 0.3 logMAR (according to Israeli law for driving license) [24], were noted. Furthermore, we recorded the number of patients whose CDVA did not demonstrate any improvement or who experienced a decrease after surgery.
Statistical Analysis
Data normality was evaluated using the D’Agostino–Pearson test. For continuous variables, the Mann–Whitney test was applied to non-normally distributed data, while the Student t-test was utilized for normally distributed data. Categorical variables were analyzed using the Z-proportion test. To account for multiple comparisons, Bonferroni’s correction was employed. The adjusted significance level was set at p < 0.05/number of comparisons in each group of risk factors, complications, and outcomes for a two-tailed test.
A sensitivity analysis was performed to compare the results achieved when including only one eye per patient (randomly selected) (n = 590). This was to ensure the robustness of our findings against potential violations of the assumption of independence between eyes from the same patient.
All analyses were conducted using SciPy for Python [25].
Results
Patient Characteristics
The study analyzed 691 eyes from 590 patients undergoing phacoemulsification cataract surgery by 30 residents. Of these, 49% (339) were female patients. Age ranged from 24 to 97 years, averaging 71.33 with a standard deviation (SD) of ± 10.96 years.
Risk Factors
The analysis included 12 risk factors, present in 71% of patients, averaging 1.43 ± 1.32 risk factors per patient. The mean pre-surgical score calculated was 2.9 ± 2.7, ranging between 0 and 13.
Risk Factors and Residency Experience
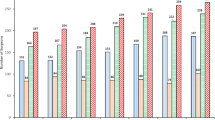
The analysis revealed significant differences in the prevalence of surgeries with risk factors across varying residence experience levels. Table 1 details the distribution of each risk factor across the residency years, followed by a visual representation of the results in Fig. 1A and B. First-year residents, with less than a year of experience, performed surgeries on patients with fewer risk factors than their fellow residents with over a year of practice (mean risk factors per patient 1.64 ± 1.35 vs. 0.84 ± 1.00, respectively, p < 0.001). This distinction was particularly evident in cases involving specific complications such as dense cataract, small pupil size, and patient non-cooperation (p < 0.001). Additionally, these less experienced residents were less likely to operate on patients using oral alpha-1 antagonists (p = 0.003). Accordingly, patients operated on by these less experienced residents demonstrated lower mean pre-scores (1.61 ± 2.0 vs. 3.2 ± 2.7, p < 0.001) and fewer risk factors per patient (mean 0.84 ± 1.00 vs. 1.64 ± 1.34, p < 0.001) than those treated by more seasoned residents. Second-year residents operated on patients with lower pre-scores (2.8 ± 2.5 vs. 3.5 ± 2.8, p = 0.005) and fewer risk factors per patient (mean 1.4 ± 1.19 vs. 1.8 ± 1.4, p = 0.005) than more experienced residents. Similarly, third-year resident-treated patients had a lower mean pre-score than their senior counterparts (3.2 vs. 3.9 p = 0.03).
A, B Comparative analysis of risk factors over residency years. This figure provides a bifurcated visual analysis of risk factors based on their prevalence over the years of residency training. The upper subplot A delineates risk factors with higher percentages, emphasizing those with greater incidence. Conversely, the lower subplot B presents risk factors with lower percentages, offering insights into less frequent occurrences
Sensitivity analysis performed for only one eye for each patient (n = 590) supported our primary findings, with two exceptions. The use of oral alpha-1 antagonists in patients operated on by first-year versus more experienced residents, significant before Bonferroni adjustment (p = 0.003), lost significance post-adjustment (p = 0.03). Additionally, the difference in pre-scores between third-year residents and senior surgeons (initially p = 0.03) was not significant in the sensitivity analysis (p = 0.19).
Risk Factors Associated with CDVA
Risk factors significantly impact post-surgery CDVA outcomes. Patients without risk factors experienced a greater percentage of CDVA improvement (mean 63% ± 36%) than those with risk factors (mean 57% ± 36%; p = 0.01). Post-surgery CDVA was also better in patients without risk factors (0.16 ± 0.26) than those with risk factors (0.27 ± 0.3; p < 0.001). Furthermore, a significant difference was observed in the proportion of patients with functional CDVA pre- and post-surgery: 30–78% in patients without risk factors and 45–92% in those with risk factors (p < 0.001 for both). These findings remained consistent in the sensitivity analysis, which included only one eye per patient.
Surgical Complications
The dataset included 13 predefined types of surgical complications, with a mean number of complications per patient of 0.20 ± 0.6. Some complications were treated as separate incidents in our analysis, despite possible dependence on a preceding complication, such as PC tear, vitreous loss, and dropped lens.
Surgical Complications in Relation to Residency Experience
Analysis of surgical complications in relation to residency experience indicated a decreasing trend in the number of complications over the first 3 years of residency. However, fourth-year residents showed an increased complication rate per patient (mean 0.25 ± 0.62) compared with surgeons with more experience (mean 0.04 ± 0.23, p = 0.01). Furthermore, a higher proportion of fourth-year residents experienced at least one complication (16.6%) relative to their more experienced counterparts (5.8%, p = 0.03). This pattern suggests a nuanced relationship between residency experience and complication rates, with a notable increase in the fourth year. Table 2 provides a comprehensive breakdown of surgical complications by surgeon experience, including comparisons with more experienced surgeons, followed by a visual representation of the results in Fig. 2. These findings largely remained consistent in the sensitivity analysis; except for the difference in complication rates between fourth-year residents and more experienced surgeons, which no longer reached statistical significance (p = 0.07).
Prevalence of specific complications throughout residency training years. This figure illustrates the percentage of residents experiencing particular complications each year, with a focus on those exceeding a 1% incidence rate. Data are segregated by type of complication and year of residency, providing insights into patterns and potential risks associated with each stage of training
Surgical Complications in Different Risk Factor Populations
The prevalence of complications varied between patients with specific risk factors and those without risk factors. IOL complications were higher in the DR group (2% vs. 0%; p < 0.001). Table S1 in the Supplementary Material provides detailed comparative rates of each complication, focusing on patient groups with sample sizes of greater than 30 patients. These findings remained consistent in the sensitivity analysis, which included only one eye per patient.
Surgical Outcomes
The mean improvement in CDVA post-surgery was 0.47 ± 0.62 (logMAR), with a mean post-surgery CDVA of 0.24 ± 0.33. CDVA improvement percentage mean 0.59 ± 0.36. Of the patients, 32 (5%) showed no CDVA change, and 22 (3%) experienced a decrease from the pre-surgery CDVA. Notably, eyes with functional CDVA (< 0.3) increased from 224 patients (34%) pre-surgery to 538 (82%) post-surgery.
Impact of Residency Experience on Surgical Outcomes
CDVA improvement generally increased until the third year, then decreased in the fourth year, stabilizing thereafter.
Figure 3 illustrates the association between residents’ experience and three factors: surgeries of patients with risk factors, surgical complications, and mean CDVA improvement proportion. As residents gain experience, surgeries involving risk factors increase, while the first 3 years demonstrate a decrease in complications and an increase in CDVA improvement. This trend slightly reverses in the fourth year, but complication rates decrease in the fifth year, with a stable CDVA improvement percentage.
Trends in risk factors, cataract surgery complications, and outcomes across residency years: proportion of operations with risk factors (blue), complications (orange), and surgical outcomes (measured by mean improvement in corrected distance visual acuity (CDVA)) (green) among patients operated on by ophthalmology residents with varying levels of operating experience
A smaller proportion of patients operated on by third-year residents experienced no change in CDVA (1% vs. 7% for more experienced surgeons, p = 0.02) or a decrease in CDVA (1% vs. 6%, p = 0.01). The number of patients with either a decline or no change in CDVA decreased annually until the third year of residency, then increased in the fourth year and remained constant thereafter. Figure 4 illustrates these trends, showing the rate of CDVA improvement, the proportion of patients with a decline in CDVA, and those with no CDVA improvement.
Sensitivity analysis, accounting for one eye per patient, supported these results.
Discussion
Cataract surgery is a common surgical intervention worldwide, with projected growth in demand as the population ages [26, 27]. Studies have investigated the influence of ophthalmology residents’ experience on surgical outcomes. Despite the overall high success rates, there is a recognized need for preoperative risk assessment systems to address potential surgical complications [14]. The pre-cataract risk score that is in use at the Hadassah Medical Center Ophthalmology Department and that was used in the analysis for the current study is based on the Buckinghamshire Healthcare NHS Trust system and inspired by Butler, Narendran, and others, and consistently demonstrates predictive capability in intraoperative complication studies [23, 28, 29]. Other risk stratification systems, such as Muhtaseb and the New Zealand Cataract Risk Stratification (NZCRS), aim to identify patients at increased risk of intraoperative complications [12, 30]. The current study examines the prevalence of risk factors among residents, the use of the pre-cataract risk score for complexity, and the impact of residents’ surgical experience, which is dictated by their structured training program on complications in cataract surgeries.
Risk Factors and Complications
The investigation revealed significant differences in complications based on various risk factors. In our preliminary analysis, patients with small pupils experienced higher incidence of ECCE, dropped lens occurrences, and wound leakage requiring sutures. However, these differences did not remain statistically significant after applying the Bonferroni correction, leading us to retain the null hypothesis. These outcomes may be attributable to the heightened technical challenges encountered during surgeries involving pseudoexfoliation syndrome (PXF). PXF is a known risk factor for both small pupil size and increased susceptibility to dropped lens incidents [31, 32]. Identifying populations with a heightened risk of specific complications enables the customization of surgical approaches, offering the potential to mitigate risk and enhance patient outcomes.
Residents’ Level of Operating Experience and Surgeries in At-Risk Patients
In terms of residents’ surgical experience with exposure to at-risk patients along residency years, the current study, in line with similar studies, suggests that less experienced residents often perform surgeries on a smaller percentage of patients with risk factors. Consistent with Magyar et al. [19], our study highlights that resident experience can predict specific complications. A similar pattern of decreasing complication rates throughout residency was reported by Bradley et al. [10] and Briszi et al. [33].
Gradual exposure to challenging cases is crucial for enhancing residents’ surgical skills, emphasizing the significance of structured training programs and mentorship opportunities in our department. This aligns with the observations of Low et al. [20], who suggested that restricted exposure may impact residents’ surgical proficiency. To address this, a pre-cataract score is employed to guide surgeon selection based on their level of experience.
Residents’ Level of Operating Experience with Surgical Complications During Cataract Surgery
Complication rates in phacoemulsification surgeries performed by residents as reported in the scientific literature range from 1.8 to 14.7%, emphasizing the need for a thorough assessment of surgical performance [5, 10, 13, 14, 17,18,19,20,21,22]. Major complications, such as posterior capsule rupture and vitreous loss, can potentially impact both surgical and visual outcomes.
The current study finds no substantial differences in mean complication rates between patients operated on by residents in their first 3 years compared to more experienced peers. However, fourth-year residents show a significantly higher mean complication rate, particularly those involving posterior capsule tear and vitreous loss, similar to former reports [13, 34, 35]. This trend may stem from supervisors who, perceiving well-developed skills in fourth-year residents, may reduce interventions, giving more independence to residents as they gain more experience, and contributing to increased complications. Alternatively, residents gained confidence, potentially leading to a greater sense of independence during the procedures.
Outcomes of Residents’ Cataract Surgery
The current study evaluated cataract surgery outcomes in residents, focusing on CDVA improvement. The mean post-surgery CDVA improvement was 0.47 ± 0.62 logMAR units, which represents a mean percentage improvement of 59 ± 36%. Notably, 97% of operated eyes either maintained or improved postoperatively, achieving a mean postoperative CDVA of 0.24 logMAR units. These results are consistent with those reported in other studies [36, 37]. Our analysis further revealed that residents’ experience had a significant impact on surgical outcomes. Third-year residents demonstrated greater improvement in CDVA than their more senior counterparts. Results indicated a progression in surgical skills over the first 3 years and a decline in the fourth year, stabilizing thereafter. This pattern may be attributed to the increased complexity of cases assigned to fourth-year residents relative to those in the earlier years of training. Additionally, during the first 3 years of residency, a single experienced surgeon guides the residents, whereas in the fourth year and beyond, residents gain greater independence and are mentored by various senior surgeons. By the fifth year, a decrease in complication rates was evident, signaling a maturation of surgical expertise and a significant improvement in visual acuity outcomes.
Complications varied, with first-year residents experiencing higher rates of anterior capsule tear. This aligns with another study that identified anterior capsulorhexis tear as a common complication in resident-performed surgeries, likely due to the learning curve associated with the procedure [38]. While anterior capsule tear is significant for junior residents, its impact on surgical outcomes tends to be less severe than that of complications such as posterior capsule tear and vitreous loss, which are more frequently reported in phacoemulsification surgeries by residents.
Our exclusive focus on residents in this study reveals a distinctive pattern of intraoperative complications during cataract surgery. Unlike other investigations, which excluded challenging cases from the analysis, we included all patients, indicating a higher incidence of posterior capsule tears (0.4–8.3%) [5, 7, 18, 19, 22, 37, 39, 40].
In the broader context of intraoperative complications and postoperative CDVA outcomes, the current study aligns with trends observed in comparable studies, showing similarities in overall complication rates and specific intraoperative issues such as anterior tears and vitreous loss. The comprehensive assessment of complications and risk factors in a residency training program spans consecutive years, offering valuable insights into challenges and experiences faced by residents throughout their learning curve. This approach contrasts with some reports in the literature that exclude challenging cases with various risk factors, potentially impacting up to 10% of resident-performed surgeries [10, 20, 22]. These exclusions, noted in previous research, disregard conditions such as pseudoexfoliation, brunescent cataracts, corneal pathology, high ametropia, monocular patients, shallow anterior chamber depth, or a history of ocular trauma, retinal detachment, diabetic macular edema, uveitis, or vitrectomy.
Study Limitations
This study, while yielding important findings, is subject to certain constraints. Its retrospective nature and the potential for missing or incomplete data introduce risks to outcome accuracy, although this has been mitigated by thorough data validation processes. Being conducted at a single center, the study may not fully represent the range of training environments. Additionally, the pre-cataract risk assessment system employed may not account for all possible complications. This analysis also omits patient-reported outcomes, focusing solely on surgical measures. Data from both eyes were included, potentially leading to inter-eye result correlation; this was addressed by a sensitivity analysis, which upheld the consistency of the findings using single-eye data. Finally, a conservative Bonferroni correction was applied to reduce the likelihood of type I errors, thereby reinforcing the significance of our results.
Conclusion
In conclusion, this study highlights the gradual exposure of ophthalmology residents to at-risk patients during their training in phacoemulsification cataract surgery. The integration of the pre-cataract score into the EMR system, as emphasized earlier, serves a dual purpose. First, it aids in aligning surgical assignments with residents’ experience levels, ensuring progressive and controlled exposure to complex cases. This approach has been shown to enhance residents’ skills development while maintaining patient safety. Second, the implementation of this score based on the existing literature has contributed to a noticeable trend of improved surgical outcomes. By systematically identifying and managing risks, the score aids in reducing complications, thus supporting the overall positive trajectory in residents’ performance and postoperative visual outcomes. The integration of the pre-cataract score into the training program and clinical practice not only underlines the importance of structured education and mentorship but also showcases the potential of data-driven tools in optimizing surgical training and patient care.
While overall positive postoperative visual outcomes were observed, careful and intensive supervision is crucial to ensure a safe training process for both residents and patients. During the learning curve phase of phacoemulsification, residents encounter potential complications. It was found that CDVA outcomes for fourth-year residents were less favorable than their preceding and subsequent years. This underscores the crucial role of instructors in redirecting attention, providing guidance, and offering support. Ensuring that residents’ confidence aligns with their evolving skills is paramount, addressing challenges and optimizing surgical outcomes. The positive trajectory observed in the fifth year signifies the beneficial impact of the experience gained from handling complex cases. The implementation of the pre-cataract score method makes it possible to adjust surgical difficulty based on the surgeon’s experience, enhancing surgical skills development and improving patient outcomes. Integrating this method into training programs can facilitate the advancement of surgical skills, emphasizing the importance of ongoing training and mentorship for ophthalmology residents.
Data Availability
Data are available on reasonable request.
References
Rossi T, et al. Original research: cataract surgery practice patterns worldwide: a survey. BMJ Open Ophthalmol. 2021;6:e000464.
Kauh CY, Blachley TS, Lichter PR, Lee PP, Stein JD. Geographic variation in the rate and timing of cataract surgery among US communities. JAMA Ophthalmol. 2016;134:267–76.
Gower EW, et al. Perioperative antibiotics for prevention of acute endophthalmitis after cataract surgery. Cochrane Database Syst Rev. 2017;2:214.
Raczyńska D, Glasner L, Serkies-Minuth E, Wujtewicz MA, Mitrosz K. Eye surgery in the elderly. Clin Interv Aging. 2016;11:407–17.
Payal AR, et al. Outcomes of cataract surgery with residents as primary surgeons in the Veterans Affairs Healthcare System. J Cataract Refract Surg. 2016;42:370–84.
Aaronson A, Viljanen A, Kanclerz P, Grzybowski A, Tuuminen R. Cataract complications study: an analysis of adverse effects among 14,520 eyes in relation to surgical experience. Ann Transl Med. 2020;8:1541–1541.
Ellis EM, et al. Complication rates of resident-performed cataract surgery: impact of early introduction of cataract surgery training. J Cataract Refract Surg. 2018;44:1109.
Rutar T, Porco TC, Naseri A. Risk factors for intraoperative complications in resident-performed phacoemulsification surgery. Ophthalmology. 2009;116:431–6.
Zaidi FH, Corbett MC, Burton BJL, Bloom PA. Raising the benchmark for the 21st century—the 1000 cataract operations audit and survey: Outcomes, Consultant-supervised training and sourcing NHS choice. Br J Ophthalmol. 2007;91:731–6.
Randleman JB, et al. The resident surgeon phacoemulsification learning curve. Arch Ophthalmol. 2007;125:1215–9.
Lee JS, Hou CH, Yang ML, Kuo JZC, Lin KK. A different approach to assess resident phacoemulsification learning curve: analysis of both completion and complication rates. Eye (Lond). 2009;23:683–7.
Han JV, et al. Auckland cataract study III: refining preoperative assessment with cataract risk stratification to reduce intraoperative complications. Am J Ophthalmol. 2019;197:114–20.
Mangan MS, Atalay E, Arici C, Tuncer İ, Bilgeç MD. Comparison of different types of complications in the phacoemulsification surgery learning curve according to number of operations performed. Turk J Ophthalmol. 2016;46:7.
Kaplowitz K, Yazdanie M, Abazari A. A review of teaching methods and outcomes of resident phacoemulsification. Surv Ophthalmol. 2018;63:257–67.
Allinson RW, Metrikin DC, Fante RG. Incidence of vitreous loss among third-year residents performing phacoemulsification. Ophthalmology. 1992;99:726–30.
Corey RP, Olson RJ. Surgical outcomes of cataract extractions performed by residents using phacoemulsification. J Cataract Refract Surg. 1998;24:66–72.
Al-Jindan M, et al. Assessment of learning curve in phacoemulsification surgery among the Eastern Province ophthalmology program residents. Clin Ophthalmol. 2020;14:113.
Woodfield AS, Gower EW, Cassard SD, Ramanthan S. Intraoperative phacoemulsification complication rates of second- and third-year ophthalmology residents: a 5-year comparison. Ophthalmology. 2011;118:954–8.
Magyar M, Sandor GL, Ujvary L, Nagy ZZ, Toth G. Intraoperative complication rates in cataract surgery performed by resident trainees and staff surgeons in a tertiary eyecare center in Hungary. Int J Ophthalmol. 2022;15:586.
Low SAW, Braga-Mele R, Yan DB, El-Defrawy S. Intraoperative complication rates in cataract surgery performed by ophthalmology resident trainees compared to staff surgeons in a Canadian academic center. J Cataract Refract Surg. 2018;44:1344–9.
Oliveira-Ferreira C, Leuzinger-Dias M, Tavares-Ferreira J, Macedo JP, Falcão-Reis F. Cataract phacoemulsification performed by resident trainees and staff surgeons: intraoperative complications and early postoperative intraocular pressure elevation. J Cataract Refract Surg. 2020;46:555–61.
Fong CSU, et al. Long-term outcomes of phacoemulsification cataract surgery performed by trainees and consultants in an Australian cohort. Clin Exp Ophthalmol. 2012;40:597–603.
Kim BZ, Patel DV, Sherwin T, McGhee CNJ. The Auckland cataract study: assessing preoperative risk stratification systems for phacoemulsification surgery in a teaching Hospital. Am J Ophthalmol. 2016;171:145–50.
Drivers License Levels|Israeli Ministry of Transport and Road Safety. 2023. https://www.gov.il/he/departments/guides/driving_licence_categories.
Virtanen P, et al. SciPy 1.0: fundamental algorithms for scientific computing in Python. Nat Methods. 2020;17:261–72.
Burton MJ, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health. 2021;9:e489–551.
Hatch WV, Campbell EDL, Bell CM, El-Defrawy SR, Campbell RJ. Projecting the growth of cataract surgery during the next 25 years. Arch Ophthalmol. 2012;130:1479–81.
Butler TKH. Risk stratification and assessment in cataract surgery. J Cataract Refract Surg. 2012;38:184.
Narendran N, et al. The Cataract National Dataset electronic multicentre audit of 55 567 operations: risk stratification for posterior capsule rupture and vitreous loss. Eye. 2009;23:31–7.
Muhtaseb M, Kalhoro A, Ionides A. A system for preoperative stratification of cataract patients according to risk of intraoperative complications: a prospective analysis of 1441 cases. Br J Ophthalmol. 2004;88:1242–6.
Shingleton BJ, Crandall AS, Ahmed IIK. Pseudoexfoliation and the cataract surgeon: preoperative, intraoperative, and postoperative issues related to intraocular pressure, cataract, and intraocular lenses. J Cataract Refract Surg. 2009;35:1101–20.
Ong AY, Shalchi Z. Outcomes of cataract surgery in pseudoexfoliation syndrome in England: 10-year retrospective cohort study. J Cataract Refract Surg. 2021;47:165–71.
Briszi A, Prahs P, Hillenkamp J, Helbig H, Herrmann W. Complication rate and risk factors for intraoperative complications in resident-performed phacoemulsification surgery. Graefe’s Arch Clin Exp Ophthalmol. 2012;250:1315–20.
Umali MIN, Castillo TR. Operative time and complication rates of resident phacoemulsification surgeries in a national university hospital: a five-year review. Clin Ophthalmol. 2020;14:4065.
Melega MV, et al. Comparing resident outcomes in cataract surgery at different levels of experience. Clin Ophthalmol. 2020;14:4523.
Han JV, et al. Auckland Cataract Study IV: Practical application of NZCRS cataract risk stratification to reduce phacoemulsification complications. Clin Exp Ophthalmol. 2020;48:311–8.
Jaycock P, et al. The Cataract National Dataset electronic multi-centre audit of 55 567 operations: updating benchmark standards of care in the United Kingdom and internationally. Eye. 2009;23:38–49.
Lee JS, Hou CH, Lin KK. Surgical results of phacoemulsification performed by residents: a time-trend analysis in a teaching hospital from 2005 to 2021. J Ophthalmol. 2022;2022:1.
Riley AF, et al. The Auckland cataract study: co-morbidity, surgical techniques, and clinical outcomes a public hospital service. Br J Ophthalmol. 2002;86:185–90.
Kim BZ, Patel DV, McGhee CNJ. Auckland cataract study 2: clinical outcomes of phacoemulsification cataract surgery in a public teaching hospital. Clin Exp Ophthalmol. 2017;45:584–91.
Acknowledgements
The authors express their gratitude to Dr. Ron Kaufman and Dr. Ori Saban for their valuable insights that enhanced this article. The authors thank the participants of the study.
Medical Writing/Editorial Assistance.
The authors utilized ChatGPT for assistance with language refinement during manuscript development. The final content was thoroughly examined and revised by the authors, who assume complete responsibility for the publication's content.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Yaacov Cnaany, Ayelet Goldstein, Itay Lavy, Michael Halpert, Itay Chowers and Hadas Ben-Eli. The first draft of the manuscript was written by Yaacov Cnaany, Ayelet Goldstein and Hadas Ben-Eli. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Yaacov Cnaany, Ayelet Goldstein, Itay Lavy, Michael Halpert, Itay Chowers and Hadas Ben-Eli have nothing to disclose.
Ethical Approval
The study was approved and performed in accordance with the institutional Helsinki committee of Hadassah Medical Center (study # HMO-0459-18). The committee exempts retrospective research from informed consent by the participants. Data were collected from the Ophthalmology Department database and anonymized before analysis. This study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments.
Additional information
Prior Presentation: A portion of this study has been accepted for poster presentation at the Annual Meeting of the Association for Research in Vision and Ophthalmology (ARVO) in 2024. No part of this manuscript has been published in a peer-reviewed journal.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Cnaany, Y., Goldstein, A., Lavy, I. et al. Ophthalmology Residents’ Experience in Cataract Surgery: Preoperative Risk Factors, Intraoperative Complications, and Surgical Outcomes. Ophthalmol Ther 13, 1783–1798 (2024). https://doi.org/10.1007/s40123-024-00947-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-024-00947-6