Abstract
Introduction
Lid-parallel conjunctival folds (LIPCOF) and conjunctivochalasis (CCH) are similar conditions that seem to be related to dry eye severity. In addition, there is a lack of studies on the topic of LIPCOF and CCH on dry eye symptoms in non-contact lens and contact lens (CL) wearers. Therefore, the aim of this study is to review the relationship of LIPCOF and CCH with dry eye symptoms in non-CL and CL wearers, as well as to report the treatment of dry eye disease (DED) in non-CL and CL wearers who present LIPCOF or CCH.
Methods
A literature review of full-length original studies in two databases, PubMed and Scopus, was performed. The search period included observational studies in humans published between April 21, 2009 and March 20, 2023.
Results
A total of 26 studies were included. The studies suggest that LIPCOF and CCH are significantly related to dry eye symptoms in non-CL and CL wearers. However, the impact of CL wear on LIPCOF and CCH may be complex and may vary depending on individual factors such as lens type, lens care regimen, and pre-existing ocular conditions. Regarding LIPCOF management, tear substitutes seem to significantly reduce LIPCOF and dry eye symptoms in non-CL wearers, while vectored thermal pulsation (VTP) and microblepharoexfoliation (MBE) are suggested as promising treatment for LIPCOF and dry eye symptoms in CL wearers. Regarding CCH management, surgical interventions may be effective in reducing CCH when medical treatments have no response. In addition, an ocular examination by slit lamp is necessary to distinguish both conditions.
Conclusions
Tear substitutes, VTP, MBE, and fitting CLs with low coefficient of friction (CoF) seem to reduce and prevent LIPCOF. However, surgical treatment options seem to be more effective in the complete elimination of CCH. An adequate evaluation and differentiation between LIPCOF and CCH are important, and they should be considered by practitioners in managing dry eye symptoms in non-CL and CL wearers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Lid-parallel conjunctival folds (LIPCOF) and conjunctivochalasis (CCH) are similar conditions that are related to dry eye disease (DED), suggesting different management approaches. |
Tear substitutes, vectored thermal pulsation, microblepharoexfoliation, and fitting contact lenses with low coefficient of friction seem to reduce and prevent lid-parallel conjunctival folds. |
High-frequency radiowave electrosurgery seems to be a promising treatment for the complete elimination of conjunctivochalasis, avoiding the postoperative complications of traditional surgical techniques. |
Differentiation between LIPCOF and CCH is important, and it should be considered by practitioners in managing dry eye symptoms. |
Introduction
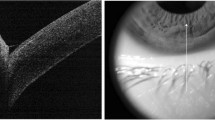
Lid-parallel conjunctival folds (LIPCOF) are folds located in the inferonasal and inferotemporal quadrants of the bulbar conjunctiva, parallel to the lower eyelid margin [1, 2], and were first described by Höh et al. [3]. Subsequent studies have suggested that LIPCOF are influenced by mechanical forces in blinks, being considered as a possible marker of dry eye symptoms [1, 4, 5]. In a comparative study, Veres et al. [6] evaluated the presence of LIPCOF in patients with dry eye and healthy controls by optical coherence tomography (OCT). The study reported that LIPCOF was more pronounced in patients with dry eye compared to healthy controls and that LIPCOF was significantly correlated with dry eye symptom severity. The presence and severity of LIPCOF may be influenced by demographic and contact lens (CL)-related factors [7,8,9,10]. In a recent study, Pult et al. [4] aimed to determine the relationship between blinking and LIPCOF in patients with and without dry eye symptoms. The results showed that LIPCOF were more pronounced in patients with dry eye symptoms compared to those without dry eye symptoms, and that blinking frequency and amplitude were lower in patients with dry eye symptoms. LIPCOF are observed with a slit lamp under high magnification (×25) in the area perpendicular to the temporal and nasal limbus above the lower eyelid (Fig. 1) [8] and are classified using a four-grade scale based on the number of folds present. Through this slit lamp ocular examination, LIPCOF should be differentiated from other ocular conditions such as conjunctivochalasis (CCH) (Fig. 2). CCH is defined as loose, redundant conjunctival folds, most typically in the inferior bulbar conjunctiva of both eyes that are considered to occur secondary to normal aging [11]. Although LIPCOF may represent the first mild stages of CCH, the differential diagnosis lies mainly in the shape of the folds. LIPCOF has regular and parallel folds, while CCH has wider and irregular folds. In addition, there are other features that aid in their differentiation, e.g., LIPCOF does not occur centrally and its cross-sectional area is much smaller than that of CCH, which suggests different management approaches are required [12, 13].
Images of the areas of observation for the identification of lid-parallel conjunctival folds (LIPCOF). a LIPCOF in the temporal region of the right eye without fluorescein (grade 2). b The area marked in yellow represents the area of the lower eyelid where LIPCOF can be observed, while the black lines indicate the location of the folds on the eyelid. c LIPCOF in the temporal region of the left eye with fluorescein (grade 2). Pictures were obtained with the S390L Firefly Wide Dynamic Range (WDR) slit lamp
CL wear provides numerous benefits such as improved visual acuity and enhanced quality of life [14, 15]. However, CL wear can also have negative impacts on ocular health [16, 17]. In addition, the prevalence of dry eye symptoms in CL wearers is higher than in non-CL wearers, which results in discomfort, and therefore reduces CL wearing time [18,19,20]. The influence of CL wear on LIPCOF and CCH is not fully understood [9, 13, 21,22,23]. Some studies have found that CL wear can exacerbate LIPCOF and CCH, possibly because of increased friction between the moving eyelid and the ocular surface when the normal tear film is disrupted by the presence of the CL [22,23,24,25,26].
Although LIPCOF and CCH also seem to increase dry eye symptom severity [6, 10, 11, 27, 28], this relationship remains unclear. In addition, to the best of our knowledge there is no review exploring all the literature available on the topic of LIPCOF and CCH on dry eye symptoms in non-CL and CL wearers. Therefore, the purpose of this review of the literature is to identify the relationship of LIPCOF and CCH with dry eye symptoms in non-CL and CL wearers, as well as to report the management of dry eye disease (DED) in non-CL and CL wearers with LIPCOF or CCH. Through this review, a comprehensive overview of the current evidence of LIPCOF and CCH on DED in non-CL and CL wearers is provided, enabling evidence-based decision-making and guiding future research directions.
Methods
Data Sources and Search Strategy
In this review of the literature, 168 articles published between April 21, 2009 and March 20, 2023 were identified through PubMed and Scopus databases. The data search strategy with Boolean operators was as follows: (lid-parallel conjunctival folds OR LIPCOF OR conjunctivochalasis) AND (dry eye symptoms OR meibomian gland dysfunction OR MGD OR non-contact lens wear OR non-CL wear OR contact lens wear OR CL wear OR treatment OR management). The references of the retrieved articles were reviewed to identify whether other related articles met the inclusion criteria.
Study Selection
All 168 articles identified through the search strategy were considered and analyzed. These articles were reviewed by two investigators who selected them according to the inclusion and exclusion criteria. For the inclusion, articles had to meet all of the following criteria: (1) human studies; (2) original full-length studies reporting on LIPCOF or CCH and its potential associations with dry eye symptoms in non-CL and CL wearers; and (3) full-length studies examining the effectiveness and safety of interventions for dry eye symptoms in non-CL and CL wearers who present LIPCOF or CCH. The same applies to the following exclusion criteria: (1) non-English publications and (2) unindexed journals. Before inclusion, it was confirmed that the studies clearly and correctly defined LIPCOF and CCH. In addition, no restrictions were placed on the country in which the study was conducted, the follow-up period, the sample size, or the results of the studies.
This article does not contain any studies with human participants or animals performed by any of the authors. Since all the reported data were obtained from the available published literature, neither institutional review board approval nor informed consent was required for the completion of this study.
Results and Discussion
Relationship Between LIPCOF and Dry Eye Symptoms in Non-CL and CL Wearers
A summary of the studies reporting the relationship between LIPCOF and dry eye symptoms is shown in Table 1. Several studies have extensively reported this relationship in non-CL wearers. In a comparative study, Veres et al. [6] reported that patients with dry eye had more severe LIPCOF than healthy controls. This study also showed that LIPCOF was significantly correlated with dry eye symptom severity. Similar results were reported by Németh et al. [10] with significant positive correlation between LIPCOF and dry eye symptom severity. In addition, Pult et al. [29] investigated the relationship between traditional test, new clinical tests such as LIPCOF stage and dry eye symptoms, and whether a combination of these tests can improve the ability to predict the development of dry eye symptoms. The results showed that the strongest relationship was found by combining non-invasive tear film breakup time (NIBUT) with nasal LIPCOF, which had the best predictive ability for detecting dry eye symptoms. In a different study, Pult and Bandlitz [27] determined the sensitivity and specificity of LIPCOF to predict dry eye symptoms with values of 83.6% and 54.8%, respectively. However, studies reporting the relationship between LIPCOF and dry eye symptoms in CL wearers are limited. To the best of our knowledge, Pult et al. [20] was the first article that reported the relationship between lid wiper epitheliopathy (LWE), LIPCOF and dry eye symptoms in soft CL wearers. A total of 61 patients were included in this study and were classified as either having dry eye symptoms or being asymptomatic on the basis of the contact lens dry eye questionnaire-8 (CLDEQ-8). The following clinical signs were evaluated: (1) LIPCOF, (2) LWE, (3) corneal fluorescein staining (CFS), (4) limbal and bulbar hyperemia, and (5) pre-lens tear breakup time (PLBUT). The results showed that LWE and LIPCOF severity scores were significantly higher in CL wearers with dry eye symptoms compared to non-CL wearers, but there were no significant differences in PLBUT, CFS, or hyperemia between both groups. In addition, the LIPCOF Sum severity scores were found to be the most predictive for dry eye symptoms. In a different study, Pult et al. [7] also reported that LIPCOF and NIBUT were significant discriminators for dry eye symptoms in 33 new soft CL wearers. Recently, Siddireddy et al. [23] aimed to determine whether clinical markers related to the eyelids and tear film could be used to predict symptoms of discomfort in CL wearers. The study evaluated the following clinical signs in 30 soft CL wearers: (1) LIPCOF, (2) tear evaporation rate with and without CLs, (3) palpebral conjunctival roughness, staining, hyperemia, and (4) meibomian gland evaluation which included meibum quality and expressibility, and the presence of capping, pouting, or foam at meibomian gland orifices. All patients also completed CLDEQ-8 to assess ocular discomfort. The results showed that LIPCOF, palpebral conjunctival health, tear evaporation rate, and clinical signs related to meibomian gland secretions and morphology may be useful in predicting symptoms of discomfort in CL wearers. It is important to mention that to the best of our knowledge, no studies have been published evaluating the relationship between LIPCOF and dry eye symptoms in rigid gas permeable (RGP) CL wearers. This may be because their use is more limited than soft CLs [30].
Overall, these findings suggest that LWE and LIPCOF are the main clinical signs that may be useful for predicting dry eye symptoms in non-CL and soft CL wearers. The development of both clinical signs may be related to the mechanical forces produced during blinking, which are increased in CL wearers. However, it is important to consider that the relationship between LIPCOF and dry eye symptoms is not yet fully understood, and the repeatability of LIPCOF as a measure is limited, which influences the results of studies.
DED Management in Non-CL and CL Wearers with LIPCOF
Soft Contact Lens-Related Design, Material, and Fitting Characteristics
A summary of the studies reporting the LIPCOF management is shown in Table 2. The mechanical forces between the anterior surface of CL and the lid wiper have been linked to CL discomfort and may also be related to the development of LIPCOF and LWE, increasing dry eye symptoms [21]. Reduction of mechanical forces can be achieved through various CL design, material, and fitting characteristics [31]. Regarding CL design, fitting CLs with low coefficient of friction (CoF) may reduce the mechanical forces between the CL and the lid wiper, which may improve CL discomfort and prevents LIPCOF and LWE [13]. A tribological perspective suggests that the ocular surface CoF is similar to that of hydrophilic polymer brushes at low sliding velocity, and that a fluid film between the sliding partners prevents wear at high velocity [13]. However, in patients with dry eye, the failure to maintain a full fluid film lubrication regime with high speeds like those that occur in blinking may lead to increased shear rates, deformation, and wear of the sliding pairs, potentially as a result of tear film viscosity [1, 13]. Therefore, it may be beneficial to address factors that affect tear film viscosity and proper ocular surface lubrication maintenance to prevent LIPCOF and LWE [14]. Moreover, a better understanding of the relationship between CoF and CL discomfort may also help prevent CL wear discontinuation [31].
Regarding CL material, some studies have evaluated CL comfort with silicone hydrogel CLs and conventional hydrogel CLs, concluding that both materials achieve similar levels of comfort [32, 33]. In a recent study, Insua Pereira and Lira [34] evaluated the level of comfort and ocular dryness during wear with six daily disposable CLs (stenfilcon A, delefilcon A, nelfilcon A, narafilcon A, nesofilcon A, and omafilcon A). The results showed that hydrogel silicone CLs (delefilcon A and narafilcon A) obtained the highest comfort ratings with less ocular dryness. Similar results were reported by Vidal-Rohr et al. [35] with a soft monthly disposable hydrogel silicone CL (formofilcon B) with an ultra-thin coating technology. However, it is important to consider that CL comfort is the result of the overall interaction of the lens with ocular tissues and depends on the mechanical characteristics, and CL wear modality of use [33]. Therefore, all these factors, which vary between patients, may have a large influence on the results of the studies. Pult et al. [26] evaluated the presence of LIPCOF, LWE, and dry eye symptoms after a 12-week follow-up period in 30 experienced CL wearers, who were randomly assigned to the following three groups: (1) discontinuing CL wear (SPEC group), (2) refitting with senofilcon A two-weekly replacement daily wear silicone hydrogel CLs (OAS group), and (3) continuing to wear their habitual lenses (HCL group). The results showed that there were no significant differences between the three groups for LIPCOF, LWE, and ocular surface disease index (OSDI) scores at baseline. However, the OAS group and SPEC group had significant improvements in LIPCOF, LWE, and OSDI scores at 12-week follow-up, while the HCL group showed no significant changes. These results suggest that refitting with senofilcon A daily wear silicone hydrogel lenses or discontinuing lens wear may be effective treatments for improving LIPCOF, LWE, and dry eye symptoms in experienced CL wearers. Regarding CL fitting characteristics, it is known that LIPCOF are impacted by lens movements in blinks [26]. Therefore, reduced CL movements or increased CL tightness may be associated with improved CL comfort and LIPCOF, as well as increased lens-induced limbal conjunctival staining and indentation [17, 31].
Tear Substitutes
Artificial tears are the main treatment for DED and dry eye-related conditions, such as CL discomfort [36]. Essa et al. [37] evaluated the presence of LIPCOF and dry eye symptoms in 50 patients with DED, who received the following artificial tears in a randomized order: Clinitas Soothe (Farmigea SpA., Pisa Italy), Hyabak (Laboratories Théa, Clermont-Ferrand, France), Tears Again (Optima Pharmazeutische GmbH, Freising, Germany), and TheraTears (Advanced Vision Research Inc., Massachusetts, USA). The results showed that LIPCOF, OSDI scores, and CFS were significantly improved with each of the four artificial tears at 4-week follow-up. These results suggest that tear substitutes may be an effective and safe treatment for LIPCOF, dry eye symptoms, and other variables related to the ocular surface such as tear film breakup time (TBUT) and CFS in non-CL wearers.
Vectored Thermal Pulsation
Vectored thermal pulsation (VTP) (TearScience, Morrisville, USA) is an in-office treatment designed to treat meibomian gland dysfunction (MGD) [38]. This system allows one to apply heat on the eyelids, while simultaneously performing a pulsatile pressure on them to evacuate the meibum from meibomian glands [39]. The efficacy and safety of VTP treatment has been reported in non-CL wearers with DED. In a randomized controlled study, Finis et al. [40] examined the effectiveness of a single VTP treatment in 31 patients with MGD, who were classified in the following groups: (1) VTP treatment group and (2) eyelid warming and massage group. The results showed that the VTP treatment group achieved significant improvement in OSDI scores compared to the eyelid warming and massage group at 3-month follow-up. LIPCOF, TBUT, lipid layer thickness (LLT), CFS, and meibomian gland secretions (MGS) were also improved with no statistically significant differences between groups. In a different study, Finis et al. [41] reported that the significant improvements achieved in LIPCOF remained significant after 6-month follow-up in the VTP treatment group.
However, the efficacy and safety of VTP treatment in CL wearers is limited because of the lack of studies. In a randomized clinical trial, Blackie et al. [42] reported that single VTP treatment significantly reduces LIPCOF and dry eye symptoms in soft CL wearers with MGD compared to the control group. MGS, TBUT, and LWE were also significantly improved. In addition, patients with VTP treatment reported significant increase in comfortable CL wearing time that was sustained for 3 months. All these findings suggest that VTP treatment may be an effective and safe option to reduce LIPCOF and dry eye symptoms in non-CL and soft CL wearers with MGD, as well as to increase comfortable CL wearing time.
Microblepharoexfoliation
Microblepharoexfoliation (MBE) (BlephEx LLC, Franklin, USA) is an in-office procedure that works by exfoliating the eyelid margins to remove the accumulated biofilm debris and epithelial keratinization, resulting in better meibum outflow [43]. Tear film and eyelid clinical signs improvements in non-CL wearers with DED have been reported after MBE treatment [44,45,46,47]. However, there have been no reported studies evaluating LIPCOF changes after MBE in non-CL wearers.
To the best of our knowledge, Siddireddy et al. [48] was the first randomized clinical trial to report significant LIPCOF and dry eye symptoms reduction in CL wearers after single MBE treatment compared to control group. They also reported that LWE, TBUT, tear volume, tear evaporation rate, lipid layer thickness, and variables related to meibomian glands such as meibomian glands orifices capping, foam, quality, and expressibility were significantly improved. These results suggest that MBE may be an effective treatment for LIPCOF, dry eye symptoms, and other variables related to the ocular surface in CL wearers.
Relationship Between CCH and Dry Eye Symptoms in Non-CL and CL Wearers
A summary of the studies reporting the relationship between CCH and dry eye symptoms is shown in Table 3. Some studies have reported this relationship in non-CL wearers. In a retrospective study, Dalianis et al. [49] reported that moderate and severe CCH produces significant increases in dry eye symptoms compared to minimal or medium CCH. This study also reported that patients with higher CCH severity showed significant reduction in TBUT. Chhadva et al. [28] analyzed the relationship between CCH location and dry eye signs and symptoms, reporting that patients with nasal CCH showed significant increase in dry eye symptoms compared to patients with non-nasal CCH and non-CCH. This study also reported that patients with nasal CCH showed significant reduction in Schirmer’s test, as well as significant increase in meibomian gland dropout compared to patients with non-nasal CCH and non-CCH. Similar results were obtained by Le et al. [50] who also reported that CCH has a negative impact on the patients’ quality of life, which is significantly correlated with disease severity and tear film abnormalities. However, the scientific literature on the relationship between CCH and dry eye symptoms in CL wearers is limited. To our knowledge, Mimura et al. [22] was the first article to report CCH in CL wearers. This study included 600 CL wearers and 579 non-CL wearers and reported that CCH prevalence and severity were significantly higher in CL wearers. In addition, this study also determined that RGP CL wearers showed significant increase in CCH severity compared to soft CL wearers. RGP CLs may cause more marked chronic stimulation of the conjunctiva than soft CLs because of their greater stiffness with a higher elastic modulus, which may lead to more severe CCH. In addition, it is important to mention that as Mimura et al. [22] did not evaluate variables related to DED, a relationship between CCH and dry eye symptoms could not be established.
DED Management in Non-CL and CL Wearers with CCH
A summary of the studies reporting the CCH management is shown in Table 4. For asymptomatic CCH, no treatment is required [11]. However, if the patient reports symptoms, medical or surgical treatment may be indicated [11, 51]. In general, the first-line treatment is medical, while surgical intervention may be considered when patients do not respond to medical treatment [51]. In addition, it is important to mention that some studies suggest that CCH may co-exist with DED [52,53,54]. Therefore, appropriate management of this condition should be required to achieve maximal symptoms relief in patients with CCH [11, 55].
Medical Treatment
Medical treatment aims to reduce CCH symptoms by using tears substitutes and non-steroidal anti-inflammatory medications. Kiss et al. [56] evaluated the efficacy of a preservative-free, inorganic salt-free artificial tear containing isotonic glycerol and 0.015% sodium hyaluronate in 20 patients with CCH. Patients were instructed to apply this artificial tear to both eyes four times a day during a 3-month follow-up. The results showed that CCH grading was significantly reduced from CCH grade 3 to CCH grade 2 or lower. In addition, OSDI scores, TBUT, and CFS also showed significant improvements. Similar results were reported by Cağlayan et al. [57] with significant reduction in OSDI scores after the combination of 0.5% ketorolac tromethamine and 0.15% sodium hyaluronate for a period of 4 weeks. However, there was no improvement in conjunctival parameters such as CCH grade and area.
Surgical Treatment
Surgical treatment aims to reconstruct and smooth the bulbar conjunctival surface. Although different surgical approaches have been proposed, conjunctival cauterization and surgical excision with or without amniotic membrane transplantation are the most popular [11, 51]. These treatments significantly reduce the mechanical effects of the redundant conjunctiva, which improves ocular symptoms and signs [58,59,60]. However, several postoperative complications associated with powerful cauterization and sutures in surgical excision have been reported [51]. High-frequency radiowave electrosurgery (HFR-ES) is a novel treatment that works by ablating the target conjunctiva with a fine-needle electrode and the 4.0-MHz radiowave system (Ellman International Inc., Hewlett, USA) [61]. In addition, this technique achieves shrinkage of the redundant conjunctiva without tissue charring, avoiding complications associated with conjunctival cauterization and surgical excision [51]. Some studies have evaluated HFR-ES treatment efficacy in CCH. Ji et al. [62] reported complete elimination of HCC in all patients at 1-month follow-up. This study also showed significant improvements in dry eye symptoms, TBUT, TMA, and CFS. Youm et al. [61] reported that 90% of patients recovered a smooth conjunctival surface with significant dry eye symptoms relief at 3-month follow-up. Similar results were reported by Trivli et al. [63] with no recurrence of CCH after 8-month follow-up. In addition, these studies reported minimal postoperative complications such as subconjunctival hemorrhage and mild conjunctival hyperemia, which was resolved after postoperative treatment.
Limitations
There are several limitations to consider when interpreting the results of previous studies on LIPCOF and CCH. First, many of the studies have used subjective tests to assess LIPCOF, CCH, and DED. These measures rely on self-report and may be subject to bias. Moreover, there is a lack of consistency in the methods used to assess LIPCOF, CCH, and DED across studies. Some studies have used different clinical grading scales to assess LIPCOF and CCH, while different subjective and objective tests have been used to evaluate DED. This lack of standardization makes it difficult to compare the results of different studies and therefore perform a systematic review with meta-analysis. Second, many of the studies have focused on specific subpopulations, such as CL wearers or individuals with MGD. This can limit the generalizability of the findings to a wider population. In addition, there is a lack of long-term follow-up data in many of the studies, making it difficult to determine the long-term effectiveness of the interventions for LIPCOF and CCH. Finally, there is a lack of understanding of the underlying biological mechanisms behind the influence of LIPCOF and CCH on dry eye symptoms. Therefore, systematic reviews with meta-analysis that include larger, strictly blind, multicenter randomized controlled studies using standardized methods to assess LIPCO and CCH are needed to understand these conditions more fully, as well as to identify effective and safe interventions.
Future Directions
There are several potential areas of future research in the study of LIPCOF and CCH. One potential line of research is to further investigate the influence of mechanical forces during blinks on LIPCOF and CCH. Although previous studies have suggested that mechanical forces may be related to LIPCOF and CCH, more research is needed to fully understand the mechanisms behind this relationship. This could include studying the effects of different types of CL on LIPCOF and CCH, as well as exploring the role of other factors such as blinking frequency and intensity. A second area of research could be focused on developing interventions to prevent or reduce the incidence of LIPCOF and CCH. Studies could explore the efficacy and safety of different materials, designs, replacement schedules of CLs, as well as other non-surgical or surgical interventions for LIPCOF and CCH. In addition, studies could be conducted to identify risk factors for the development of LIPCOF and CCH, such as certain occupations or activities that may increase the risk of mechanical forces on the eye. A third potential area of research would be to investigate the relationship between LIPCOF and dry eye symptoms in RGP CL wearers. While previous studies have found a link between LIPCOF and dry eye symptoms in non-CL and soft CL wearers, more research is needed to understand the nature of this relationship. A fourth area of research could be focused on evaluating the influence of CCH on dry eye symptoms in CL wearers. It would be interesting to perform studies that assess dry eye symptoms in CL wearers with CCH compared to those without CCH, as well as to analyze the correlation between CCH and dry eye symptoms in CL wearers. Finally, there is a need for more research on the long-term effects of LIPCOF and CCH on ocular health. Future studies could explore the potential for LIPCOF and CCH to lead to other ocular problems, such as vision loss or the development of other ocular conditions.
Conclusion
Our research provides new insights into the management of dry eye symptoms in both CL and non-CL wearers, particularly in the context of LIPCOF and CCH. We highlight the importance of tailored approaches for DED management, emphasizing the potential of combining NIBUT with LIPCOF assessments for more accurate prediction of dry eye symptoms. Our findings suggest that low CoF CLs, along with innovative eyelid treatments like VTP and MBE, can significantly enhance comfort for CL wearers by mitigating LIPCOF and improving tear film stability. Additionally, we underscore the effectiveness of tear substitutes in alleviating dry eye symptoms in non-CL wearers.
For CCH, our study points to the promising role of HFR-ES, offering a potential alternative to traditional surgical methods. These insights are expected to aid practitioners in more effectively addressing dry eye symptoms associated with LIPCOF and CCH, enhancing patient outcomes in both CL and non-CL populations.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Berry M, Pult H, Purslow C, Murphy PJ. Mucins and ocular signs in symptomatic and asymptomatic contact lens wear. Optom Vis Sci. 2008;85:E930–8.
Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15:539–74.
Schirra F, Höh H, Kienecker C, Ruprecht KW. Using LIPCOF (lid-parallel conjunctival fold) for assessing the degree of dry eye, it is essential to observe the exact position of that specific fold. Adv Exp Med Biol. 1998;438:853–8.
Pult H, Riede-Pult BH, Murphy PJ. The relation between blinking and conjunctival folds and dry eye symptoms. Optom Vis Sci. 2013;90:1034–9.
Bandlitz S, Purslow C, Murphy PJ, Pult H. Lid-parallel conjunctival fold (LIPCOF) morphology imaged by optical coherence tomography and its relationship to LIPCOF grade. Cont Lens Anterior Eye. 2019;42:299–303.
Veres A, Tapasztó B, Kosina-Hagyó K, Somfai GM, Németh J. Imaging lid-parallel conjunctival folds with OCT and comparing its grading with the slit lamp classification in dry eye patients and normal subjects. Invest Ophthalmol Vis Sci. 2011;52:2945–51.
Tapasztó B, Veres A, Kosina-Hagyó K, Somfai GM, Németh J. OCT imaging of lid-parallel conjunctival folds in soft contact lens wearers. Optom Vis Sci. 2011;88:1206–13.
Pult H, Murphy PJ, Purslow C. A novel method to predict the dry eye symptoms in new contact lens wearers. Optom Vis Sci. 2009;86:E1042–50.
Morgan PB, Murphy PJ, Gifford KL, et al. CLEAR—effect of contact lens materials and designs on the anatomy and physiology of the eye. Cont Lens Anterior Eye. 2021;44:192–219.
Németh J, Fodor E, Lang Z, et al. Lid-parallel conjunctival folds (LIPCOF) and dry eye: a multicentre study. Br J Ophthalmol. 2012;96:1380–5.
Marmalidou A, Kheirkhah A, Dana R. Conjunctivochalasis: a systematic review. Surv Ophthalmol. 2018;63:554–64.
Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276–83.
Pult H, Tosatti SGP, Spencer ND, Asfour J-M, Ebenhoch M, Murphy PJ. Spontaneous blinking from a tribological viewpoint. Ocul Surf. 2015;13:236–49.
Naroo SA, Morgan PB, Shinde L, Lee C, Ewbank A. Contact lens education for the practitioners of the future. Ophthalmic Physiol Opt. 2021;41:603–9.
Kandel H. Quality-of-life outcomes of long-term contact lens wear: a systematic review. Cont Lens Anterior Eye. 2022;45:101521.
Lim CHL, Stapleton F, Mehta JS. Review of contact lens-related complications. Eye Contact Lens. 2018;44(Suppl 2):S1-10.
Stapleton F, Bakkar M, Carnt N, et al. CLEAR—contact lens complications. Cont Lens Anterior Eye. 2021;44:330–67.
Stapleton F, Marfurt C, Golebiowski B, et al. The TFOS international workshop on contact lens discomfort: report of the subcommittee on neurobiology. Invest Ophthalmol Vis Sci. 2013;54:TFOS71-97.
Masoudi S, Zhao Z, Stapleton F, Willcox M. Contact lens-induced discomfort and inflammatory mediator changes in tears. Eye Contact Lens. 2017;43:40–5.
González-Mejiome JM, Parafita MA, Yebra-Pimentel E, Almeida JB. Symptoms in a population of contact lens and noncontact lens wearers under different environmental conditions. Optom Vis Sci. 2007;84:E296-302.
Pult H, Purslow C, Berry M, Murphy PJ. Clinical tests for successful contact lens wear: relationship and predictive potential. Optom Vis Sci. 2008;85:E924–9.
Mimura T, Usui T, Yamamoto H, et al. Conjunctivochalasis and contact lenses. Am J Ophthalmol. 2009;148:20.
Siddireddy JS, Tan J, Vijay AK, Willcox M. Predictive potential of eyelids and tear film in determining symptoms in contact lens wearers. Optom Vis Sci. 2018;95:1035–45.
Best N, Drury L, Wolffsohn JS. Predicting success with silicone-hydrogel contact lenses in new wearers. Cont Lens Anterior Eye. 2013;36:232–7.
Pult H. Relationships between meibomian gland loss and age, sex, and dry eye. Eye Contact Lens. 2018;44(Suppl 2):S318–24.
Pult H, Riede-Pult BH. Impact of soft contact lenses on lid- parallel conjunctival folds. Cont Lens Anterior Eye. 2019;42:415–9.
Pult H, Bandlitz S. Lid-parallel conjunctival folds and their ability to predict dry eye. Eye Contact Lens. 2018;44(Suppl 2):S113–9.
Chhadva P, Alexander A, McClellan AL, McManus KT, Seiden B, Galor A. The impact of conjunctivochalasis on dry eye symptoms and signs. Invest Ophthalmol Vis Sci. 2015;56:2867–71.
Pult H, Purslow C, Murphy PJ. The relationship between clinical signs and dry eye symptoms. Eye (Lond). 2011;25:502–10.
Morgan PB, Efron N, Woods CA. Determinants of the frequency of contact lens wear. Eye Contact Lens. 2013;39:200–4.
Stapleton F, Tan J. Impact of contact lens material, design, and fitting on discomfort. Eye Contact Lens. 2017;43:32–9.
Cheung SW, Cho P, Chan B, Choy C, Ng V. A comparative study of biweekly disposable contact lenses: silicone hydrogel versus hydrogel. Clin Exp Optom. 2007;90:124–31.
Guillon M. Are silicone hydrogel contact lenses more comfortable than hydrogel contact lenses? Eye Contact Lens. 2013;39:86–92.
Insua Pereira E, Lira M. Comfort, ocular dryness, and equilibrium water content changes of daily disposable contact lenses. Eye Contact Lens. 2018;44(Suppl 2):S233–40.
Vidal-Rohr M, Wolffsohn JS, Davies LN, Cerviño A. Effect of contact lens surface properties on comfort, tear stability and ocular physiology. Cont Lens Anterior Eye. 2018;41:117–21.
Pucker AD, Ng SM, Nichols JJ. Over the counter (OTC) artificial tear drops for dry eye syndrome. Cochrane Database Syst Rev. 2016;2:CD009729.
Essa L, Laughton D, Wolffsohn JS. Can the optimum artificial tear treatment for dry eye disease be predicted from presenting signs and symptoms? Cont Lens Anterior Eye. 2018;41:60–8.
Lane SS, Dubiner HB, Epstein RJ, et al. A new system, the LipiFlow, for the treatment of meibomian gland dysfunction. Cornea. 2012;31:396–404.
Majmudar PA, Group LS. A novel thermal pulsation treatment for obstructive Meibomian gland dysfunction: applying heat to the inner eyelid surfaces. Invest Ophthalmol Vis Sci. 2010;51:6281–6281.
Finis D, Hayajneh J, König C, Borrelli M, Schrader S, Geerling G. Evaluation of an automated thermodynamic treatment (LipiFlow®) system for meibomian gland dysfunction: a prospective, randomized, observer-masked trial. Ocul Surf. 2014;12:146–54.
Finis D, König C, Hayajneh J, Borrelli M, Schrader S, Geerling G. Six-month effects of a thermodynamic treatment for MGD and implications of meibomian gland atrophy. Cornea. 2014;33:1265–70.
Blackie CA, Coleman CA, Nichols KK, et al. A single vectored thermal pulsation treatment for meibomian gland dysfunction increases mean comfortable contact lens wearing time by approximately 4 hours per day. Clin Ophthalmol. 2018;12:169–83.
Zhu D, Gupta RR, Stein RL, et al. Randomized prospective evaluation of microblepharoexfoliation blephex as adjunctive therapy in the treatment of chalazia. Cornea. 2022;42:172.
Ngo W, Caffery B, Srinivasan S, Jones LW. Effect of lid debridement-scaling in Sjögren syndrome dry eye. Optom Vis Sci. 2015;92:e316–20.
Korb DR, Blackie CA. Debridement-scaling: a new procedure that increases meibomian gland function and reduces dry eye symptoms. Cornea. 2013;32:1554–7.
Murphy O, O’Dwyer V, Lloyd-McKernan A. The efficacy of tea tree face wash, 1,2-octanediol and microblepharoexfoliation in treating Demodex folliculorum blepharitis. Cont Lens Anterior Eye. 2018;41:77–82.
Mohammad-Rabei H, Arabi A, Shahraki T, Rezaee-alam Z, Baradaran-rafii A. Role of blepharoexfoliation in demodex blepharitis: a randomized comparative study. Cornea. 2023;42:44–51.
Siddireddy JS, Tan J, Vijay AK, Willcox MDP. The effect of microblepharon exfoliation on clinical correlates of contact lens discomfort. Optom Vis Sci. 2019;96:187–99.
Dalianis G, Trivli A, Terzidou C. The location of conjunctivochalasis and its clinical correlation with the severity of dry eye symptoms. Medicines (Basel). 2018;5:12.
Le Q, Cui X, Xiang J, Ge L, Gong L, Xu J. Impact of conjunctivochalasis on visual quality of life: a community population survey. PLoS ONE. 2014;9:e110821.
Marmalidou A, Palioura S, Dana R, Kheirkhah A. Medical and surgical management of conjunctivochalasis. Ocul Surf. 2019;17:393–9.
Tseng SCG, Di Pascuale MA, Espana EM, Kawakita T. Clinical characteristics of conjunctivochalasis with or without aqueous tear deficiency. Br J Ophthalmol. 2004;88:388–92.
Yokoi N, Komuro A, Nishii M, et al. Clinical impact of conjunctivochalasis on the ocular surface. Cornea. 2005;24:S24.
Balci O. Clinical characteristics of patients with conjunctivochalasis. Clin Ophthalmol. 2014;8:1655–60.
Tseng SCG. A practical treatment algorithm for managing ocular surface and tear disorders. Cornea. 2011;30(Suppl):1.
Kiss HJ, Németh J, Jhanji V. Isotonic glycerol and sodium hyaluronate containing artificial tear decreases conjunctivochalasis after one and three months: a self-controlled, unmasked study. PLoS ONE. 2015;10:e0132656.
Çağlayan M, Kösekahya P, Gürdal C, Saraç Ö. Comparison of electrocoagulation and conventional medical drops for treatment of conjunctivochalasis: short-term results. Turk J Ophthalmol. 2018;48:61–5.
Doss LR, Doss EL, Doss RP. Paste-pinch-cut conjunctivoplasty: subconjunctival fibrin sealant injection in the repair of conjunctivochalasis. Cornea. 2012;31:959–62.
Chan TCY, Ye C, Ng PKF, Li EYM, Yuen HKL, Jhanji V. Change in tear film lipid layer thickness, corneal thickness, volume and topography after superficial cauterization for conjunctivochalasis. Sci Rep. 2015;5:12239.
Santiago E, Yang Y, Conlon R, Compan J, Baig K, Ziai S. Surgical techniques for the treatment of conjunctivochalasis: paste-pinch-cut conjunctivoplasty versus thermal cautery conjunctivoplasty. Can J Ophthalmol. 2017;52:308–12.
Youm DJ, Kim JM, Choi CY. Simple surgical approach with high-frequency radio-wave electrosurgery for conjunctivochalasis. Ophthalmology. 2010;117:2129–33.
Ji YW, Seong H, Lee S, et al. The correction of conjunctivochalasis using high-frequency radiowave electrosurgery improves dry eye disease. Sci Rep. 2021;11:2551.
Trivli A, Dalianis G, Terzidou C. A quick surgical treatment of conjunctivochalasis using radiofrequencies. Healthcare (Basel). 2018;6:14.
Funding
No funding or sponsorship was received for this study or publication of this article.
Author information
Authors and Affiliations
Contributions
Antonio Ballesteros-Sánchez: Conceptualization, methodology, formal analysis, investigation, writing—original draft preparation, visualization. José-María Sánchez-González: Data curation, writing—review & editing, supervision, project administration. María Agustina Borrone: Investigation, resources, data curation, writing—review & editing. Davide Borroni: Validation, formal analysis, writing—review & editing. Carlos Rocha-de-Lossada: Conceptualization, methodology, resources, writing—review & editing, supervision.
Corresponding author
Ethics declarations
Conflict of Interest
The authors, Antonio Ballesteros-Sánchez, José-María Sánchez-González, María Agustina Borrone, Davide Borroni, and Carlos Rocha-de-Lossada, declare that they have no conflict of interest relevant to the content of this article.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors. Since all the reported data were obtained from the available published literature, neither institutional review board approval nor informed consent was required for the completion of this study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ballesteros-Sánchez, A., Sánchez-González, JM., Borrone, M.A. et al. The Influence of Lid-Parallel Conjunctival Folds and Conjunctivochalasis on Dry Eye Symptoms with and Without Contact Lens Wear: A Review of the Literature. Ophthalmol Ther 13, 651–670 (2024). https://doi.org/10.1007/s40123-023-00877-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00877-9