Abstract
Introduction
In this work, our aim is to report the functional outcomes of cataract surgery with smaller-incision new-generation miniature telescope (SING IMT) implantation followed by rehabilitation training in patients with central visual loss due to late-stage age-related macular degeneration (AMD).
Methods
This retrospective study included patients who were monocularly implanted with SING IMT and then followed a rehabilitation program based on 6 biweekly sessions focused on visual abilities, reading, writing, visual motor integration and mobility. A total of 11 participants were included in this study. Reading acuity (RA), reading speed (RS), and fixation stability (FS) were assessed biweekly at 6-, 8-, 10-, 12-, 14-, and 16-week follow-up visits after SING IMT implantation and at a final assessment at 24 weeks. Best-corrected distance visual acuity (BCDVA) was also measured at baseline and at the same postoperative timepoints.
Results
Mean baseline BCDVA was 12.5 ± 8.6 letter score. Both RA and RS were found to be significantly improved from the first rehabilitation session (6 weeks after surgery) to the last session (24 weeks after surgery). At the end of the rehabilitation program, mean RA was 0.45 ± 0.19 LogMAR and mean RS was 30.9 ± 17.6 words per minute. Moreover, all patients achieved a FS of 15 s or more after the last rehabilitation session. Most patients (55%) achieved an improvement of 15 letters in BCDVA at the end of the study.
Conclusions
This study suggests that rehabilitation training can improve visual functions of patients with late-stage AMD implanted with SING IMT in real-world tasks such as reading skills.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Age-related macular degeneration (AMD) is a major cause of irreversible vision loss, affecting daily activities. Treatment options for central visual field loss in late-stage AMD are limited. Hence, the critical evaluation of novel technologies, such as the new-generation implantable telescope (SING IMT), assumes paramount significance. |
This evaluation aims to comprehensively assess the functional visual capabilities of patients with late-stage AMD. |
This study reports the functional outcomes of cataract surgery with SING IMT implantation followed by rehabilitation training in patients with central visual loss due to late-stage AMD. |
What was learned from the study? |
In this study of 11 participants (median age, 81 years), both reading acuity (RA) and reading speed (RS) significantly improved after rehabilitation at 24 weeks after surgery. RA improved by about 0.2 LogRAD, RS by 11.2 words per minute. |
All patients achieved a functional span of 15 s or more, and 55% showed a 15-letter improvement in best-corrected distance visual acuity. |
SING IMT implant surgery and rehabilitation enhance real-world visual abilities, such as reading, for patients with late-stage AMD, requiring a multidisciplinary approach in patient selection and postoperative care. |
Introduction
Age-related macular degeneration (AMD) represents a major cause of irreversible vision loss and legal blindness in ageing populations [1]. In advanced stages, AMD can lead to progressive macular atrophy and/or scarring with development of a central scotoma [2, 3]. This results in a central visual field loss (CFL) which reduces the ability to read, recognize faces, watch television, and drive, impairing patient independence and quality of life [4,5,6,7,8,9,10].
Treatment and surgical options to manage CFL due to AMD are extremely limited, especially for patients with end-stage AMD who remain an underserved population. In order to improve vision of patients with end-stage AMD, a variety of magnifying devices have been developed including low vision spectacles, external telescopes or magnifiers, and implantable vision-enhancing devices [11,12,13,14,15].
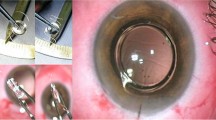
The smaller-incision new-generation implantable miniature telescope (SING IMT) is the first approved surgical treatment for bilateral central vision loss due to end-stage AMD. This device is indicated for monocular implantation in the capsular bag and acts as a Galilean telescope providing a 2.7 × magnification of the central visual field which can enhance visual details by reducing the size of the scotoma relative to the objects being viewed [16]. Recently, Toro et al. demonstrated a three lines or better improvement of best-corrected distance visual acuity (BCDVA) in 67–70% of the eyes at 3 months after SING IMT implantation [17]. These results confirmed similar outcomes observed in previous registered studies [18,19,20,21]. However, no data have yet been published regarding the functional performance, such as reading skills.
Reading performance, as speed and accuracy, is considered as a key function and one of the best predictors of patient-reported visual ability and vision-related quality of life. Reading rehabilitation represents an important goal to rescue quality of life in patients with low vision. This complex activity requires sufficient retinal resolution and perceptual span during one fixation [4,5,6,7]. Plasticity is defined as changes in brain or perceptual behavior following a disease, an injury or a surgery. It has been shown that visual plasticity following adult-onset deprivation may affect visual performance. Patients with CFL adopt a preferred retinal locus (PRL), which corresponds to the reference location for seeing on a region outside the scotoma [22]. This phenomenon, called oculomotor re-referencing, shows that plasticity is possible for patients with AMD with low vision, and that visual rehabilitation can be achieved by training or perceptual learning on a specific aspect of visual function [23, 24].
In this study, we evaluated the effect of SING IMT implantation followed by rehabilitation training on the functional visual performance in patients with end-stage AMD.
Methods
Study Design
This was a retrospective study conducted between February 2022 to June 2023 at the Policlinico Gemelli hospital in Rome which included participants with bilateral end-stage AMD. Informed consent to participate in the study was obtained from all participants. The study was performed according to the guidelines of Declaration of Helsinki and approved by the Ethics Committee of Policlinico Gemelli hospital (approval code: 4634).
Patient Screening and Selection
The screening process was performed by a staff composed of low-vision specialists and orthoptists. Patients were screened based on both non-clinical criteria (including realistic expectations, supportive family, familiarity with available low-vision devices) and medical history with no existing cognitive or communication problems, which represent important parameters correlated with improved health outcomes [25]. Moreover, patients were informed that the functional visual output from the implant would be a new type of functional vision rather than restoration of previous vision and will require a considerable investment in terms of effort and time. Inclusion criteria included cataract and bilateral geographic atrophy or disciform scar, ≥ 55 age, good peripheral vision, bilateral BCDVA comprised between 20/80 and 20/800 (0.6–1.6 logMAR), anterior chamber depth (ACD) ≥ 2.5 mm, endothelial cell density (ECD) ≥ 1600 cells/mm2. Moreover, the eye selected for the study needed to demonstrate a minimum improvement of five letters on the Early Treatment Diabetic Retinopathy Study Charts (ETDRS) scale through the use of an external telescope simulator (ETS 3.0X-FF; VisionCare Ophthalmic Technologies Ltd., Petah Tikva, Israel) before undergoing surgery. Patients who had active choroidal neovascularization (CNV) or had received CNV treatment in the preceding 6 months, a history of intraocular or corneal surgery, corneal stromal or endothelial dystrophies (including guttae), myopia exceeding 6.0 D, hyperopia exceeding 4.0 D, a record of steroid-induced increases in intraocular pressure (IOP), preoperative IOP of 22 mmHg or higher while on maximum medication, or uncontrolled glaucoma in the study eye were not included in the study. Individuals with ophthalmic conditions that could compromise peripheral vision in the fellow eye were also excluded. Lastly, patients exhibiting significant cognitive impairment evaluated according our clinical practice, potentially affecting their ability to comprehend instructions, follow guidelines, or participate in appropriate visual training or rehabilitation with the implant, were also excluded from the study. If both eyes were eligible for implantation, the dominant or preferred eye by the patient was selected for implantation.
Surgical Procedure and Postoperative Care
All surgeries were performed at the Policlinico Gemelli hospital by SR, AS, and TC using a previously published procedure [16]. Patients were anesthetized using sub-tenon block 10 min before surgery. A sclerocorneal incision of 8.0 mm was created at the 12 o’clock position, and then continuous manual circular anterior capsulorhexis with a diameter of at least 6.0 mm was carried out, and standard phacoemulsification was performed. SING IMT was inserted into the anterior chamber by means of a preloaded delivery system and positioned into the capsular bag with two haptics inferiorly and one superiorly. Then, the sclerocorneal incision was sutured using five single 10–0 monofilament nylon sutures. Finally, an iridectomy was performed at 12 o’clock position. Following surgery, patients received topical therapy with antibiotic and anti-inflammatory drops for 1 month and cycloplegic drops for 2 weeks (the iris was dilated during this period).
Rehabilitation Training Program
SING IMT is based on bi-ocular alternating vision. To optimize functional performance, a greater collaboration of the two eyes is required to autonomously exclude the image according to the patient’s visual needs. To do so, a rehabilitation training program was set up based on the expertise of the ophthalmologists, surgeons, and orthoptists of the Policlinico Gemelli Hospital. Prior to the program, a patient survey was conducted to understand the activities needed with the following results: reading (36%), writing (21%), watching TV (29%), and face recognition (14%). The program started after the dilation drop regimen at 6 weeks after surgery because the healing process and dilation could interfere with clear vision. It covered five different key skills including (1) visual abilities, (2) reading, (3) writing, (4) visual motor integration, and (5) mobility (Fig. 1). Training of each skill consisted of at least seven sessions for 1 h and a half each (with a 15-min break) every 2 weeks over a period of 6 months. For the reading training protocol, a series of exercises designed for macular degeneration (as ocular-manual coordination, ocular motility, number to number, fovea centration, identifying the center of a spot, image differences, identifying differences between two images) was performed in this study to improve the reading skills of patients. Lights and high-contrast shapes were used during the sessions. To improve reading skills, the patient needed to train the PRL in the implanted eye to be able to read progressively smaller letters, words, sentences, and numbers. Depending on the corneal astigmatism and presence of suture, prescription glasses were used for some patients during the reading training protocol. The full protocol for each skill is described in Supplementary Material #1.
Assessment of Baseline Characteristics and Postoperative Outcomes
Baseline characteristics (including BCDVA, axial length, and anterior chamber depth) were collected from medical records. Functional outcomes (including reading acuity, reading speed, and fixation stability) were then measured after rehabilitation sessions conducted at 6, 8, 10, 12, 14, 16, and 24 weeks after SING IMT implantation.
Ophthalmic Examinations and Ocular Imaging
BCDVA was assessed using the ETDRS charts. Slit-lamp anterior segment and fundus examination, followed by optical coherence tomography (OCT) was also performed (Optovue Solix Fullrange OCT). Axial length (AL) and anterior chamber depth (ACD) were evaluated using optical biometry (ZEISS IOLMaster® 500). Corneal endothelial cell density (ECD) was measured with specular microscopy (CSO Endothelial Microscope Perseus).
Reading Acuity Measurement
Reading acuity (RA) in LogMAR was evaluated monocularly with the Minnesota Reading (MNRead) test charts at 25 cm adding + 4 D spherical to the distance refractive correction.
Reading Speed Measurement
Reading speed (RS) was evaluated monocularly by counting the number of words read in 1 min on the International Reading Speed Texts (IREST) charts that allowed patients to read fluently, without making errors, the 0.6 M (5.9-character print) on MNRead charts.
Fixation Stability Measurement
Fixation stability (FS) was evaluated in seconds and measured the time to maintain the image with the implanted eye to view static objects at the distance of 4 m; the fellow eye was occluded, after the identification of the PRL (as object identification). Microperimetry was not technically possible due to the implant optical characteristics. Fifteen seconds was considered as a normal fixation stability as reported in the literature [26].
Visual Acuity Measurement
BCDVA was evaluated with the ETDRS and was expressed in letter score values at 3 m with the best refractive correction.
Statistical Analysis
All functional and visual outcomes were reported as mean ± standard deviation and paired t tests were used to compare them at baseline and different postoperative timepoints. All analyses were performed using GraphPad Prism 6 (GraphPad, San Diego, CA, USA).
Results
Patient Baseline Demographics and Clinical Characteristics
In total, 11 patients implanted with the SING IMT between February and June 2022 were included in this retrospective study. Baseline demographics and clinical characteristics of these patients are detailed in Table 1. All patients were white and presented geographic atrophy in both eyes. Most of the patients were male (72.7%, n = 8) and the mean age was 77.5 ± 8.0 years. SING IMT were monocularly implanted in the right eye in 63.6% of the patients. The baseline BCDVA (in letter score) was 12.5 ± 8.6, which corresponds approximatively to 1.45 LogMAR or 20/600 Snellen. No patient was lost for follow-up during this study.
Reading Acuity
After the first session of the rehabilitation program (6 weeks postoperatively), mean RA was 0.64 ± 0.26 LogMar (Fig. 2A). After the last session (24 weeks postoperatively), mean RA was 0.45 ± 0.19 LogMAR. This improvement of ~ 0.2 LogMar was found statistically different (p = 0.0181) from first session to last session. The maximum RA of each patient was achieved after four sessions of the rehabilitation program for most of the patients (55%, n = 6). (Fig. 2B).
Influence of rehabilitation program on the reading acuity of patients after SING IMT implantation. A Reading acuity of patients after SING IMT implantation and several rehabilitation sessions. *p < 0.05, **p < 0.005 compared to first rehabilitation session (corresponding to 6 weeks postoperatively). B Cumulative proportion of patients who achieved their maximal reading acuity value according to the number of rehabilitation sessions. RA reading acuity, SING IMT smaller-incision new-generation miniature telescope
Reading Speed
Similar to RA, mean RS improved from the second program session (16.9 ± 11.4 words per minute) to the last session (30.9 ± 17.6 words per minute) (p = 0.0057 between the first and the second to last session, however the p value not calculable between the first and the last session due to the lost to follow-up) (Fig. 3A). The maximum RS of each patient was achieved after five sessions of the rehabilitation program for most of the patients (64%, n = 7) (Fig. 3B).
Influence of rehabilitation program on the reading speed of patients after SING IMT implantation. A Reading speed of patients after SING IMT implantation and several rehabilitation sessions. *p < 0.05 compared to 1st rehabilitation session (corresponding to 6 weeks postoperatively) B Cumulative proportion of patients who achieved their maximal reading speed value according to the number of rehabilitation sessions. RS reading speed, SING IMT smaller-incision new-generation miniature telescope
Fixation Stability
The rehabilitation program was also shown to improve the fixation stability of patients after SING IMT implantation (Fig. 4). Most of the patients (55%, n = 6) required only two sessions to achieve 15 s or more of fixation stability. All patients achieved a fixation stability of at least 15 s after the last rehabilitation session.
Visual Acuity Outcomes
From baseline to the last follow-up visit, 82% of patients (n = 9) achieved an improvement of ten letters, 54.5% (n = 6) an improvement of 15 letters, and one patient an improvement of 25 letters (Fig. 5). At 24 weeks after SING IMT implantation, mean BCDVA was 28.5 ± 7.4 letter score which was significantly higher than baseline BCDVA (p < 0.0001). Moreover, BCDVA was found to be significantly improved between the first and the last rehabilitation sessions (p = 0.0125).
Discussion
The implantable miniature telescope SING IMT has been specifically designed to address visual acuity and functional visual outcomes in patients with late-stage AMD. The miniaturized device is a fixed-focus, monocular prosthetic telescope incorporating ultraprecise, quartz glass, wide-angle Galilean micro-optics, requiring no external devices or head motion to function. Compared to its previous generation, the SING IMT is designed with three foldable haptics and is pre-loaded in a delivery system which requires a smaller incision for the implantation, resulting in limited endothelial cell loss [16, 17]. To the best of our knowledge, it was the first time that functional outcomes have been investigated following SING IMT implantation. While BCNVA evaluates near vision clarity, reading speed quantifies the efficiency of reading, reading acuity determines the smallest legible print size at a standardized reading distance, and fixation time sheds light on the stability of gaze during reading.
Visual rehabilitation training usually aims to facilitate the integration of new visual inputs provided by a device with the patient’s vision in order to enhance quality of life and autonomy. The rehabilitation process can include in-clinic as well as community settings [27,28,29]. In addition to patient training, rehabilitation experts need to manage the expectations of patients and their families with regard to the degree of vision each patient will experience [30]. Reading skills can be affected by a range of parameters such as an eccentric location of the PRL, instability of fixation, poor visual acuity, crowding effect of the peripheral retina and deficient eye movement control [31]. Therefore, efforts have been made to design rehabilitation techniques aiming to improve oculomotor control by stabilizing fixation, to alleviate crowding effects by using fonts with larger spacing between the letters, and to enlarge visual span by relocating the PRL above or below the scotoma [32].
The rehabilitation training program described in this study included at least seven sessions over 24 weeks. All patients attended at least seven rehabilitation sessions, which required a strong commitment from the patient to achieve good visual functional outcomes. This commitment should be considered as a key selection criterion in future studies. Interestingly, the benefits on functional outcomes were achieved in 4–5 sessions for most patients. Finally, an improvement of 15 letters has been showed in this study, which is similar to what has been reported in another study [17]. These outcomes are very promising and clinically relevant considering the initial low vision of these patients.
Nevertheless, rehabilitation training has been found to be challenging for some of the patients, especially elderly ones with age-associated physical and psychological issues, co-morbidities, and transportation barriers. Telerehabilitation, i.e., providing rehabilitation services via the internet, could benefit these patients. However, more studies are still necessary to compare the effectiveness of telerehabilitation compared to face-to-face services [33]. Finally, patient expectations and motivation can be influenced by the level of knowledge of the pathology [4]. A background in the therapeutic area should be provided to give a better understanding of AMD-related low vision to the patients.
It is worth noting that the achievements described in this study were possible thanks to a collaborative group of experts, including low-vision specialists, eye surgeons, ophthalmologists, and orthoptists. Strict patient selection, precise surgical technique, and postoperative rehabilitation training all played an important role to guarantee successful postoperative functional outcomes. It is also important to remark that the baseline parameters such as intellectual level or emotional support were not taken into consideration during patient selection and may have been different in each patient. An intriguing prospect lies in evaluating the potential variability in the effectiveness of the rehabilitation program based on the initial intellectual capacity or psycho-emotional state of the patient.
This study also presents some limitations, including the retrospective design and the small patient cohort, which was an inherent outcome of the device's relatively specific indication. This study represents an initial exploration in this research domain, which also explains the low population size. Moreover, a comparative analysis was not possible since this study had no control arm. Moreover, this is a single-center study enrolling only white patients with geographic atrophy. Therefore, the results could not be generalized to a different population or location. Finally, the reading performance could not be compared between before and after SING IMT implantation, since most of the patients could not read before surgery.
Conclusions
In conclusion, the implantable miniature telescope SING IMT shows promise in addressing visual acuity and functional outcomes in patients with late-stage AMD. The results demonstrate significant improvements in reading skills and fixation stability, with most patients achieving benefits within 4–5 rehabilitation sessions. The collaborative effort of a multidisciplinary team and strict patient selection played crucial roles in achieving successful outcomes. While the study has limitations, such as a small sample size and single-center design, the findings highlight the potential of SING IMT and rehabilitation training in improving functional outcomes in patients with late-stage AMD. Further research is needed to validate these findings in larger and more diverse populations.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Change history
05 February 2024
A Correction to this paper has been published: https://doi.org/10.1007/s40123-024-00890-6
References
Lim LS, Mitchell P, Seddon JM, et al. Age-related macular degeneration. Lancet. 2012;379:1728–38.
Clemons TE, Milton RC, Klein R, et al. Risk factors for the incidence of advanced age-related macular degeneration in the age-related eye disease study (AREDS) AREDS report no. 19. Ophthalmology. 2005;112:533–539.
Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2:e106–16.
Rubin GS. Measuring reading performance. Vision Res. 2013;90:43–51.
Crossland MD, Rubin GS. Eye movements and reading in macular disease: further support for the shrinking perceptual span hypothesis. Vision Res. 2006;46:590–7.
Falkenberg HK, Rubin GS, Bex PJ. Acuity, crowding, reading and fixation stability. Vision Res. 2007;47:126–35.
Timberlake GT, Mainster MA, Peli E, et al. Reading with a macular scotoma. I. Retinal location of scotoma and fixation area. Invest Ophthalmol Vis Sci. 1986;27:1137–1147.
Casten RJ, Rovner BW. Update on depression and age-related macular degeneration. Curr Opin Ophthalmol. 2013;24:239–43.
Elliott DB, Trukolo-Ilic M, Strong JG, et al. Demographic characteristics of the vision-disabled elderly. Invest Ophthalmol Vis Sci. 1997;38:2566–75.
Owsley C, McGwin G, Lee PP, et al. Characteristics of low-vision rehabilitation services in the United States. Arch Ophthalmol. 2009;127:681–9.
Chung STL. The effect of letter spacing on reading speed in central and peripheral vision. Invest Ophthalmol Vis Sci. 2002;43:1270–6.
Tarita-Nistor L, González EG, Markowitz SN, Steinbach MJ. Plasticity of fixation in patients with central vision loss. Vis Neurosci. 2009;26:487–94.
Nilsson UL, Frennesson C, Nilsson SE. Location and stability of a newly established eccentric retinal locus suitable for reading, achieved through training of patients with a dense central scotoma. Optom Vis Sci. 1998;75:873–8.
Nilsson UL, Frennesson C, Nilsson SEG. Patients with AMD and a large absolute central scotoma can be trained successfully to use eccentric viewing, as demonstrated in a scanning laser ophthalmoscope. Vision Res. 2003;43:1777–87.
Sasso P, Silvestri V, Sulfaro M, et al. Perceptual learning in patients with Stargardt disease. Can J Ophthalmol. 2019;54:708–16.
Savastano A, Caporossi T, Sasso P, et al. A new intraocular telescopic device for age-related macular degeneration. Ophthalmol Retina. 2022;6:971–2.
Toro MD, Vidal-Aroca F, Montemagni M, et al. Three-month safety and efficacy outcomes for the smaller-incision new-generation implantable miniature telescope (SING IMT™). J Clin Med. 2023;12:518.
Hudson HL, Lane SS, Heier JS, et al. Implantable miniature telescope for the treatment of visual acuity loss resulting from end-stage age-related macular degeneration: 1-year results. Ophthalmology. 2006;113:1987–2001.
Hudson HL, Stulting RD, Heier JS, et al. Implantable telescope for end-stage age-related macular degeneration: long-term visual acuity and safety outcomes. Am J Ophthalmol. 2008;146:664–73.
Boyer D, Freund KB, Regillo C, et al. Long-term (60-month) results for the implantable miniature telescope: efficacy and safety outcomes stratified by age in patients with end-stage age-related macular degeneration. Clin Ophthalmol. 2015;9:1099–107.
Alió JL, Mulet EM, José M, et al. Intraocular telescopic lens evaluation in patients with age-related macular degeneration. J Cataract Refract Surg. 2004;30:1177–89.
Legge GE, Chung STL. Low vision and plasticity: implications for rehabilitation. Annu Rev Vis Sci. 2016;2:321–43.
Tarita-Nistor L, Brent MH, Steinbach MJ, et al. Reading training with threshold stimuli in people with central vision loss: a feasibility study. Optom Vis Sci. 2014;91:86–96.
Chung STL. Improving reading speed for people with central vision loss through perceptual learning. Invest Ophthalmol Vis Sci. 2011;52:1164–70.
Teutsch C. Patient-doctor communication. Med Clin North Am. 2003;87:1115–45.
Samet S, González EG, Mandelcorn MS, et al. Changes in fixation stability with time during binocular and monocular viewing in maculopathy. Vision (Basel). 2018;2:40.
Ghodasra DH, Chen A, Arevalo JF, et al. Worldwide argus II implantation: recommendations to optimize patient outcomes. BMC Ophthalmol. 2016;16:52.
Olmos de Koo LC, Gregori NZ. The Argus II retinal prosthesis: a comprehensive review. Int Ophthalmol Clin. 2016;56:39–46.
Dagnelie G, Christopher P, Arditi A, et al. Performance of real-world functional vision tasks by blind subjects improves after implantation with the Argus® II retinal prosthesis system. Clin Exp Ophthalmol. 2017;45:152–9.
Stronks HC, Dagnelie G. The functional performance of the Argus II retinal prosthesis. Expert Rev Med Devices. 2014;11:23–30.
He Y, Legge GE. Linking crowding, visual span, and reading. J Vis. 2017;17:11.
Crossland MD, Crabb DP, Rubin GS. Task-specific fixation behavior in macular disease. Invest Ophthalmol Vis Sci. 2011;52:411–6.
Bittner AK, Yoshinaga PD, Rittiphairoj T, Li T. Telerehabilitation for people with low vision. Cochrane Database Syst Rev. 2023;1:CD011019.
Acknowledgements
Medical Writing.
The authors would like to thank Clotilde Jumelle of Medivise Consulting for medical writing assistance. Funding for these services was provided by Samsara Vision.
Funding
Samsara Vision funded medical writing and publication, including the journal’s Rapid Service Fee.
Author information
Authors and Affiliations
Contributions
Conception/design: Paola Sasso, Alfonso Savastano, Faustino Vidal-Aroca and Stanislao Rizzo; Acquisition/analysis/interpretation of data: Paola Sasso, Alfonso Savastano, Faustino Vidal-Aroca, Angelo Maria Minnella, Giuseppe Francione, Leonardo Sammarco, Valentina Cima, Ritangela Ghiraldelli, Roberta Mattei and Stanislao Rizzo; Manuscript drafting/critical revision: Paola Sasso, Alfonso Savastano, Faustino Vidal-Aroca and Stanislao Rizzo; Agreement to be accountable for all aspects of the work: Paola Sasso, Alfonso Savastano, Faustino Vidal-Aroca, Angelo Maria Minnella, Giuseppe Francione, Leonardo Sammarco, Valentina Cima, Ritangela Ghiraldelli, Roberta Mattei and Stanislao Rizzo.
Corresponding author
Ethics declarations
Conflict of Interest
Faustino Vidal-Aroca reports being an employee of Samsara Vision during this study. Paola Sasso, Alfonso Savastano, Angelo Maria Minnella, Giuseppe Francione, Leonardo Sammarco, Valentina Cima, Ritangela Ghiraldelli, Roberta Mattei, Stanislao Rizzo have nothing to disclose.
Ethical Approval
The study was approved by the local ethics committee of Policlinico Gemelli hospital (approval code: 4634) and followed the tenets of the Declaration of Helsinki of 1964 and its later amendments. Informed written consent was obtained from all patients for both the participation in the study and the publication of the results.
Additional information
Prior Presentation: This work has been presented in part as a ‘‘free paper’’ at SISO (Società Italiana di Scienze Oftalmologiche), Rome, Italy, May 10–11, 2023 and Retina 4, Rome, Italy Sept 22–23, 2023.
The original online version of this article was revised to correct author name Giuseppe Francione.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sasso, P., Savastano, A., Vidal-Aroca, F. et al. Enhancing the Functional Performance of Patients with Late-Stage Age-Related Macular Degeneration Implanted with a Miniature Telescope using Rehabilitation Training. Ophthalmol Ther 13, 697–707 (2024). https://doi.org/10.1007/s40123-023-00871-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00871-1