Abstract
Introduction
The aim of this work is to utilize swept-source optical coherence tomography angiography (SS-OCTA) to assess the long-term changes in the choroidal and choriocapillaris (CC) layers of the fellow unaffected eye of patients with unilateral resolved chronic central serous chorioretinopathy (cCSC) following treatment with continuous oral eplerenone (EPL).
Methods
The study included 35 patients with cCSC and subretinal fluid (SRF) in one eye. SS-OCTA imaging was performed on the fellow cCSC eyes at baseline, 6 months, and 12 months during eplerenone therapy. CC OCT angiography was analyzed to determine the percentage of choriocapillaris flow deficits (FD%), the number of flow deficits (FDn), and the average area of flow deficits (FDa).
Results
The results demonstrated significant changes in CC flow deficits from baseline to follow-up visits. Specifically, there was a significant decrease in FD% from 28.9 ± 2.2% at baseline to 26.4 ± 1.9% at 6 months (p = 0.023), and further to 24.9 ± 1.7% at 12 months (p = 0.001). Additionally, the FD area gradually contracted over the follow-up period (p < 0.05). Conversely, there was a significant increase in the number of flow deficits compared to baseline (p < 0.05). No statistically significant changes were observed in best-corrected visual acuity (BCVA) at the follow-up visits (p > 0.05).
Conclusions
The findings of this study demonstrated long-term reperfusion of the choriocapillaris in unaffected fellow cCSC eyes during continuous oral eplerenone therapy. The beneficial effects of eplerenone therapy were observed after 6 months and maintained at 1 year. These results suggest that specific mineralocorticoid receptor (MR) antagonists may be effective in promoting choriocapillaris recovery in the unaffected eyes of patients with cCSC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
There is growing evidence indicating that eplerenone treatment for chronic central serous chorioretinopathy (cCSC) can potentially influence the vascular remodeling of choroidal tissue. Several studies have reported positive effects of eplerenone on choroidal vascular remodeling in eyes affected by CSC. |
The aim of this research was to employ swept-source optical coherence tomography angiography (SS-OCTA) for evaluating the enduring changes in the choroidal and choriocapillaris (CC) layers of the unaffected eyes impacted by previously treated cCSC using eplerenone. |
What was learned from the study? |
This study primarily focused on evaluating choriocapillaris parameters in the unaffected, non-exudative eyes affected by cCSC. The main outcome measures encompassed the following: (i) flow deficit percentage (FD%); (ii) flow deficit average area (FDa); flow deficit number (FDn); In addition to these primary outcomes, secondary measures were considered, including choroidal thickness (CT). |
By carefully assessing the OCT-A characteristics pre- and post-treatment, we gain insights into the efficacy of eplerenone therapy in promoting choriocapillaris recovery in the unaffected, non-exudative eyes affected by cCSC. |
This information can help guide treatment decisions, monitor disease progression, and evaluate the response to therapy in patients with chronic central serous chorioretinopathy. |
Introduction
Central serous chorioretinopathy (CSC) is a common retinal disease in the working age population [1]. This condition is characterized by serous macular detachment in one or more foci of the macular region [1]. Risk factors are represented by the use of corticosteroid, stress, pregnancy, and “type a” personality [2, 3]. This retinal disorder is habitually bilateral and the affected patients displayed signs of CSC in both eyes [4]. The acute form of CSC (aCSC) is defined as acute-onset, and spontaneously regresses within 3 or 4 months. Nevertheless, when SRF accumulation perseveres beyond 3 or 4 months, the pathology is intended chronic (cCSC) and could lead to gradual vision deterioration [4].
Although the pathogenesis of CSC is not yet clear, various authors speculate that choroidal alterations are the primary underlying mechanism of this retinal disorder [5]. The enlargement of Haller choroidal layer leads to mechanical compression on the RPE– Bruch’s membrane layer and the CC layer, causing CC ischemia and breakage of the RPE barrier [6]. This phenotype is part of the spectrum of “pachychoroid” disease [7]. Of note, the increased choroidal thickness is associated with enhanced vascular permeability [8]. Many authors have speculated that this abnormality is due to overexpression of the choroidal mineralocorticoids receptor (MR) [4]. Therefore, antagonists MR (eplerenone) has been widely used in the treatment of cCSC [9]. Previous papers have reported SRF resolution and a contraction of the choroidal thickness (CT), confirming the efficiency of mineralocorticoid antagonists in CSC eyes [10, 11]. However, it is crucial to acknowledge that the existing literature on the EPL therapy for cCSC is marked by notable discrepancies. Notably, the VICI study did not find any significant evidence in favor of the clinical benefit of eplerenone for the management of CSC [12].
With the introduction of swept-source OCTA technology, several authors have described retinal and choroidal remodeling in numerous retinal disorders [13]. Previous papers have focused on evaluating the CC modifications in CSC eyes, suggesting focal CC hypoperfusion [14]. Recently, Yun et al. suggested a correlation between the variations in CC vessel density and the underlying vascular choroidal enlargement in the fellow CSC eyes [7].
While several studies concentrated on choroidal structural fluctuations of eyes affected by cCSC with SRF following different therapies [15, 16], a recent study displayed choroidal vasculature recovery in both eyes of patients treated with oral EPL [4]. Nevertheless, the present literature did not reveal any long-term CC changes of the fellow cCSC eye during continuous oral EPL therapy. Taking this into account, it would be relevant to define the chronic EPL impact on the choroidal layer and CC status of the fellow cCSC eyes.
Therefore, considering the nature of pachychoroid diseases, this study aims to explore the long-term CC vasculature flow modifications in the fellow unaffected eye of patients with unilateral resolved chronic CSC following treatment with eplerenone by means of SS-OCTA.
Methods
Study Design
This observational retrospective study involved 35 eyes of 35 patients with chronic central serous chorioretinopathy (cCSC). This study comprised a subset of patients from our previously published research cohort [17]. Patients with unilateral exudative cCSC and their corresponding non-exudative fellow eyes were enrolled at the Department of Translational Biomedicine Neuroscience, University of Bari "Aldo Moro," Italy, between March 2021 and August 2022. The study adhered to the principles outlined in the Declaration of Helsinki. This study is retrospective in nature, and in accordance with Italian regulations, ethical approval is not necessary for such studies. Instead, only notification to the ethics committee is required. Written consent was obtained from all participants included in the study, allowing for the retrospective use of their clinical data.
For the purpose of this analysis, chronic CSC was defined as persistent SRF for a duration of at least 6 months before commencing therapy. Additionally, it is noteworthy that each patient enrolled in the study had not undergone any previous treatments. The diagnostic criteria for chronic central serous chorioretinopathy (cCSC) in this study included the use of various imaging modalities. These included fluorescein angiography, fundus autofluorescence, indocyanine green angiography (ICGA) using the Heidelberg Spectralis system (Heidelberg Engineering, Germany), and structural optical coherence tomography (OCT) using DRI OCT (Triton, Topcon Corp., Tokyo, Japan). These imaging techniques were employed to aid in the diagnosis and assessment of cCSC in the study.
Eplerenone Treatment
In accordance with our previous publication, all patients in this study received a daily dosage of 50 mg of eplerenone [17]. The administration of eplerenone began after obtaining approval from the patients' general practitioners. Throughout the study period, we closely monitored the potassium levels of the participants. Although we were prepared to exclude patients if any significant adverse events occurred, all patients were able to continue the eplerenone therapy as the observed adverse events were not considered significant.
Examinations
Ophthalmological assessments were conducted for all patients, including measurements of best-corrected visual acuity (BCVA), intraocular pressure (IOP), and fundus examination. Swept source (SS) OCTA imaging (DRI OCT, Triton, Topcon Corp., Tokyo, Japan) was performed on all patients. Data were collected at eplerenone initiation, as well as at 6 and 12 months of follow-up.
By the 12th month, all the exudative eyes affected by central serous chorioretinopathy associated with pachychoroid had achieved complete resolution of subretinal fluid.
Exclusion criteria were: (i) use of systemic steroids, (ii) previous PDT, (iii) other choroidal or retinal diseases, (iv) systemic contraindications to the MR antagonists administration, and (v) previous laser therapy or ocular surgery. Additionally, the presence of RPE-related artifacts (i.e., pigment epithelium detachment) in the fellow unaffected eye served as a significant exclusion criterion. Building upon earlier research [18, 19], it is important to note that artifactual changes in perfusion may significantly impact the outcomes of choriocapillaris imaging in these specific eyes.
Outcomes Measures
The primary outcome measures in this study focused on assessing choriocapillaris parameters in the fellow non-exudative eyes affected by chronic central serous chorioretinopathy (cCSC). These included: (i) flow deficit percentage (FD%): this parameter quantified the proportion of choriocapillaris flow deficit area compared to the total area of the choriocapillaris; (ii) flow deficit average area (FDa): it represented the average size of the flow deficit areas in the choriocapillaris; (iii) flow deficit number (FDn): this parameter indicated the count or number of flow deficit areas observed in the choriocapillaris. Additionally, secondary outcome measures were considered, which included: (i) choroidal thickness (CT): this measurement was acquired perpendicular to Bruch's membrane, extending to the chorioretinal interface at the central fovea. The CT measurement yielded insights into the thickness of the choroidal layer within the subfoveal region, a parameter of significance in the context of pachychoroid spectrum disease; (ii) best-corrected visual acuity (BCVA): the BCVA was measured and converted into the LogMAR scale, which provides a standardized measurement of visual acuity. It is important to highlight that in this study, we specifically chose to utilize SS-OCTA to examine chronic cCSC eyes that were not impacted by serous detachment. This decision aimed to prevent potential OCTA artifacts caused by masking effects. Notably, the work of Maltsev et al. [20] provided insight into this matter, suggesting that the thickness of the photoreceptor outer segment (PROS) layer holds substantial influence over the OCT signal at the level of the RPE as well as the OCT angiography flow signal within the choriocapillaris beneath the neurosensory detachment (NSD).
These outcome measures were used to assess the impact of eplerenone therapy on choriocapillaris parameters and secondary parameters such as choroidal thickness and visual acuity in the fellow non-exudative eyes affected by cCSC.
Imaging Analysis
All patients underwent SS-OCTA (DRI OCT, Triton, Topcon). The Triton swept-source OCT utilized in this study operates at a wavelength of 1050 nm and has a scan speed of 100,000 A-scans per second. The instrument incorporates an active eye tracker, which tracks eye movement, detects blinking, and adjusts the scan position accordingly, effectively minimizing motion artifacts during OCTA imaging. A 4.5 × 4.5 mm protocol was employed to scan all eyes. The OCTA software utilized in the study included an artifact removal option, which was utilized as part of the analysis.
To define the boundaries of the CC layer, the study utilized the semi-automated segmentation tool provided by the manufacturer [21]. This tool applied a choriocapillaris slab from the Bruch's membrane (BM) to 10.4 mm beneath the BM. In cases where automatic segmentation errors occurred, two expert retinal graders (P.V. and M.O.G.) manually performed the segmentation to ensure accurate results. To minimize the presence of shadow and/or projection artifacts [22], the regions of the choroidal circulation (CC) that were located beneath the superficial retinal vasculature were excluded from the analysis [23]. Poor-quality images with a quality score below 40 were eliminated from the investigation to ensure reliable and accurate results. Simultaneously, structural macular OCT scans were obtained using a volume scan protocol with dimensions of 12 × 9 mm.
Imaging Processing
Choriocapillaris Flow
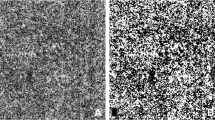
Each CC OCTA slab was examined with ImageJ software (National Institutes of Health, Bethesda, MD, USA). After exporting each CC en face OCTA image, they were analyzed using Fiji ImageJ software (version 2.0.0; National Institute of Health, Bethesda, MD, USA). The CC images were binarized using the Phansalkar method with a radius of 15 pixels, which was consistent with previous studies [24,25,26]. This process of binarization helped to convert the CC images into binary images, allowing for further quantitative analysis and assessment of the choriocapillaris flow. To quantify the CC FD metrics (FD%, FDa, and FDn), the “analyze particles” command was selected (Fig. 1).
Choriocapillaris swept-source optical coherence tomography angiography (SS-OCTA) scans in fellow chronic central serous chorioretinopathy (cCSC) pachychoroid eye continuously treated with eplerenone. SS-OCTA image of the choriocapillaris (CC) in unaffected cCSC pachychoroid eye was used to analyze choriocapillaris flow deficits parameters. The CC images were binarized by the Phansalkar method. Scans were acquired at baseline visit, and also at 6 months and 12 months. The figure shows the CC reperfusion area throughout the follow-up (white circle)
Choroidal Thickness (CT)
CT was measured using the caliper function of the structural OCT. The measurement was taken perpendicularly from Bruch's membrane to the chorioretinal interface at the central fovea. This was done using the caliper tool. The CT measurement provided information about the thickness of the choroidal layer at the subfoveal region.
Significantly, the OCT and OCTA measurements were conducted during the early morning hours. In order to assess the consistency of our measurements, all patients underwent a second OCTA measurement on a separate day, also conducted in the early morning hours.
Statistics Analysis
Quantitative variables were presented as mean ± standard deviation (SD) in the study. Normality of the data was assessed using the Shapiro–Wilk test for all variables. Pairwise comparisons with Bonferroni post hoc corrections between follow-up examinations were conducted using a paired t test to compare metrics such as best-corrected visual acuity (BCVA), OCT measurements, and OCTA metrics. The reproducibility between the two measurements was assessed using analysis of variance. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS Inc., version 20.0, Chicago, IL, USA). A chosen level of statistical significance was set at p < 0.05.
Results
Patients’ Characteristics
In this study, we included 35 White patients with chronic central serous chorioretinopathy. The majority of the patients were male (26 patients) and the mean age was 47.4 ± 2.7 years. None of the enrolled patients were using steroid therapy. Mean duration EPL therapy was 11.9 ± 0.4 months. Table 1 includes the subjects characteristics.
Analysis of the choriocapillaris using swept-source optical coherence tomography angiography showed a significant reduction in the flow deficit percentage (FD%) after EPL treatment. Compared to the baseline, the FD% decreased progressively from 28.9 ± 2.2% at baseline to 26.4 ± 1.9% at 6 months (p = 0.039), and further to 24.9 ± 1.7% at 12 months (p = 0.001) (Table 2). Additionally, there was a significant reduction in FD% at the last follow-up compared to the 6-month follow-up (p = 0.032). The FD average area (FDa) also showed a significant decrease at the follow-up visits, with a gradual contraction from baseline (97.1 ± 54.6) to 6 months (72.1 ± 39.3; p = 0.010), and further to 12 months (60.1 ± 32.3; p = 0.009). On the other hand, the FD number exhibited a relevant increase from baseline (12,994 ± 297.6) to 6 months (15,345 ± 362.3; p = 0.021), and further to 12 months (17,435 ± 387.8; p = 0.001) (Table 2).
Choroidal thickness (CT) analysis revealed a significant reduction from baseline (323.3 ± 68.1 μm) to the follow-up visits at 6 months (300.4 ± 66.4 μm, p = 0.015) and 12 months (298.2 ± 65.1 μm, p = 0.001). There was also a statistically significant CT reduction between the follow-up visits (p < 0.05).
Regarding best-corrected visual acuity (BCVA) in the fellow cCSC eyes, no significant changes were observed during the treatment period (p > 0.05) (Table 2).
Overall, the findings indicate a significant reduction in the flow deficit percentage and a contraction of the FD average area in the choriocapillaris layer of the fellow cCSC eyes following treatment with eplerenone. There was also a significant decrease in choroidal thickness. However, there were no significant changes in BCVA.
Importantly, the assessment of exudative eyes afflicted by CSC demonstrated a full resolution of subretinal fluid by the conclusion of the 12-month period. Additionally, it is noteworthy that none of the patients enrolled in the study experienced any relapses throughout the study's duration.
Adverse Events
Patients included in the study experienced mild adverse events, namely dizziness and dry mouth, following continuous eplerenone (EPL) therapy. However, these adverse events were well tolerated, and no significant alterations in potassium levels were observed. Despite these mild side effects, all patients were able to continue with the EPL therapy as the adverse events were not deemed significant or concerning.
Discussion
In this study, we aimed to assess the long-term effects of eplerenone on the fellow eyes affected by resolved chronic central serous chorioretinopathy (cCSC) within the context of pachychoroid spectrum disease. This study incorporated a subset of patients from a previously published research cohort [17]. We employed swept-source optical coherence tomography angiography (SS-OCTA) to evaluate the modifications in the choroidal and choriocapillaris (CC) layers of the fellow eyes before and during eplerenone therapy.
Our results demonstrated a significant reduction in choriocapillaris ischemia in the fellow cCSC eyes after only 6 months of continuous eplerenone treatment. This improvement was observed through quantitative measurements of the choriocapillaris vasculature using OCT angiography. Specifically, we observed a significant decrease in the flow deficit percentage (FD%) from baseline to 6 months and further improvement at 12 months. This indicates a restoration of choriocapillaris perfusion in the treated eyes.
Importantly, the administration of eplerenone was well tolerated by the patients, with minimal occurrence of adverse events. This suggests that eplerenone is a safe therapeutic option for the treatment of cCSC, as it does not lead to significant side effects.
However, it is important to keep in mind the potential systemic adverse effects, including hyperkalemia, dizziness, and dry mouth, which might hinder the continuation of the therapy [12].
The current primary therapeutic option for both acute and chronic central serous chorioretinopathy (CSC) is verteporfin photodynamic therapy (PDT) [27]. However, PDT is not without its potential side effects, although they are relatively uncommon. These side effects include the development of choroidal neovascularization (CNV), choroidal ischemia, and retinal pigment epithelium (RPE) atrophy [28]. It is worth noting that PDT treatment may not be as effective in eyes with pre-existing RPE atrophy [28]. Given these considerations, oral eplerenone emerges as a viable alternative therapeutic option for chronic CSC. Eplerenone's mechanism of action, which involves modulation of mineralocorticoid receptors, may provide a unique approach to addressing the pathophysiology of CSC and promoting resolution of subretinal fluid.
Antagonists of mineralocorticoid receptors are well-known drugs used to battle cardiovascular disease [29]. Interestingly, there is growing evidence suggesting that endogenous mineralocorticoid dysfunction may play a significant role in the pathogenesis of chronic central serous chorioretinopathy (CSC), particularly in relation to the hyperdynamic choroidal circulation observed in affected patients [30]. Studies conducted in animal models, specifically in rats, have demonstrated that the administration of corticosterone, a glucocorticoid hormone, leads to increased expression of mineralocorticoid receptors in the choroidal tissue. This upregulation of mineralocorticoid receptors is associated with choroidal thickening, a characteristic feature of CSC. However, the use of mineralocorticoid receptor antagonist agents has shown promise in reversing choroidal thickening and promoting resolution of the condition [31]. Based on these findings, the effects of continuous eplerenone treatment were investigated in this study. The chosen treatment regimen was 50 mg of eplerenone per day, following the protocol suggested by Bousquet et al. [11] and our previous publication [17].
Previous studies have described the impact of eplerenone on the patients with cCSC [3]. Using the MR antagonists (eplerenone and spironolactone), Bousquets et al. [11] obtained encouraging findings in the 3 months of therapy in terms of subretinal fluid, central macular thickness and BCVA. In the study with 28 eyes analyzed for 6 months, Gergely et al. [32] demonstrated the EPL safety and anatomical and functional improvement of chronic CSC eyes. Another retrospective study of 100 eyes [33] exhibited total subretinal fluid resolution during the first year of EPL therapy, which was sustained over successive years. These findings suggest that there may be a benefit to continuing maintenance eplerenone therapy on morpho-functional outcomes. Nevertheless, it is important to note that existing literature concerning the utilization of eplerenone for CSCs presents significant inconsistencies. Notably, the VICI study did not uncover substantial evidence supporting the clinical advantage of eplerenone for the management of central serous chorioretinopathy (CSCR) [12]. Importantly, many studies have been marked by relatively short follow-up periods or include patients who discontinue therapy upon observing elevated potassium levels.
Based on the recent theory of pachychoroid pigment epitheliopathy [34], we assessed the cCSC eyes who did not have active subretinal fluid to shed light on the eplerenone impact on CC flow and CT. Prior studies have demonstrated that alterations in the tissues above can influence the OCTA flow signal originating from the choriocapillaris [35]. This aspect gains particular significance when evaluating the perfusion of the choriocapillaris. Maltsev and colleagues [20] have substantiated this notion by providing evidence that the photoreceptor outer segment layer holds paramount importance in influencing the optical coherence tomography signal beneath the neurosensory detachment.
We displayed that the CC perfusion remodels after eplerenone treatment at 6 months, and it was sustained in the follow-up period. In detail, our results showed relevant CC FD% and FDa reduction after continuous eplerenone treatment. Recent evidence from OCTA studies suggests that microvascular CC ischemia may be part of the CSC pathogenesis and pachychoroid diseases. Rochepeau et al. [36] reported an increased choriocapillaris hypoperfusion and microvascular deficits in CSC eyes compared with healthy controls. Similarly, Yun et al. [7] described hypoperfusion CC areas in the fellow eyes of acute CSC eyes. These results supported the idea that the impaired choroidal vasculature dilation causes choriocapillaris compression, causing CC hypoperfusion. In addition, previous reports concentrated on the CC vessels changes in patients with unilateral CSC treating with different therapies. Ho et al. [37] speculated that both MLT and PDT promote choriocapillaris flow recovery. Nevertheless, these previous studies were limited to evaluating the exudative affected eye that might be impaired by OCTA artifacts. Therefore, our results suggest that cCSC fellow eye in pachychoroid spectrum without definite RPE changes is also characterized by intrinsic choroidal abnormalities and limited choriocapillaris elasticity. This latter is confirmed by the impact of continuous eplerenone treatment; the CC vasculature of non-affected cCSC eye showed a precursor flow damage followed by significant choroidal restoration at the follow-up period. In summary, our study represents the pioneering effort in presenting a comprehensive assessment of the choriocapillaris in the fellow eye affected by chronic cCSC within the context of the pachychoroid spectrum.
Moreover, we analyzed choroidal thickness changes of unaffected cCSC eyes. CT outcomes in the fellow eyes have varied in previous studies. Ghadialy et al. [38] did not find relevant CT modifications in CSC eyes treated with mineralocorticoid antagonists, although only two patients were being treated with eplerenone. On the contrary, Gergely et al. [32] showed relevant CT decrease in unaffected cCSC fellow eyes during the EPL therapy that returned to original values after stopping the treatment. We found a significant choroidal thickness reduction as early as 6 months of eplerenone therapy and this significant finding was sustained during the follow-up period.
In light of our findings, we hypothesize that the presence of long-standing enlarged choroidal vessels in chronic central serous chorioretinopathy (cCSC) may have an influence on the underlying choriocapillaris of the non-affected eye, leading to structural and functional alterations. However, our observations indicate that eplerenone treatment can restore and improve the choriocapillaris perfusion in the affected eye, suggesting a potential reverse effect on the choroidal vasculature.
Based on the long-term anatomical changes observed in this study, there may be a benefit to maintaining therapy with specific mineralocorticoid receptor antagonists like eplerenone. This therapeutic approach could potentially prevent further anatomical and functional impairments in both affected and non-affected eyes of patients with cCSC.
However, it is important to acknowledge the limitations of this study. The sample size was relatively small, and the study design was retrospective, which may introduce certain biases. Additionally, the use of 4.5 × 4.5-mm OCTA scans focused on the fovea may have limited the detection of vasculature changes in other choroidal areas. An additional limitation of our methodology is that the assessment of the choriocapillaris did not involve the implementation of a minimum threshold for particle size. Furthermore, the absence of a control group and the lack of differentiation between the effects of eplerenone and the natural disease course hinder the ability to determine the precise therapeutic regimen.
Conclusions
In conclusion, our study provides insights into the chronic anatomical and visual outcomes of patients with pachychoroid cCSC who received continuous oral eplerenone treatment. The non-affected eyes demonstrated flow deficit areas in the choriocapillaris initially, but these areas gradually improved following eplerenone therapy. Overall, our findings highlight the beneficial effects of eplerenone therapy in promoting choriocapillaris recovery and reperfusion in the fellow eyes affected by resolved cCSC. These results support the use of eplerenone as a valid therapeutic strategy to prevent further anatomical and functional impairment in the fellow eyes of patients with cCSC. Further randomized prospective trials comparing different medications in affected versus non-affected cCSC eyes are needed to better understand the specific treatment benefits and facilitate more individualized therapy approaches.
Data Availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
Daruich A, Matet A, Dirani A, Bousquet E, Zhao M, Farman N, et al. Central serous chorioretinopathy: recent findings and new physiopathology hypothesis. Prog Retin Eye Res. 2015;48:82–118.
Wong KH, Lau KP, Chhablani J, Tao Y, Li Q, Wong IY. Central serous chorioretinopathy: what we have learnt so far. Acta Ophthalmol. 2016;94:321–5.
Daruich A, Matet A, Dirani A, Gallice M, Nicholson L, Sivaprasad S, et al. Oral mineralocorticoid-receptor antagonists: real-life experience in clinical subtypes of nonresolving central serous chorioretinopathy with chronic epitheliopathy. Transl Vis Sci Technol. 2016;5:2.
Toto L, Ruggeri ML, Evangelista F, Viggiano P, D’Aloisio R, De Nicola C, et al. Choroidal modifications assessed by means of choroidal vascularity index after oral eplerenone treatment in chronic central serous chorioretinopathy. Eye (Lond). 2022;37(6):1214–8.
Sacconi R, Borrelli E, Querques G. Eplerenone for chronic central serous chorioretinopathy. Lancet (London, England). 2020;396:1556.
Dansingani KK, Balaratnasingam C, Naysan J, Freund KB. En face imaging of pachychoroid spectrum disorders with swept-source optical coherence tomography. Retina. 2016;36:499–516.
Yun C, Huh J, Ahn SM, Lee B, Kim JT, Hwang S-Y, et al. Choriocapillaris flow features and choroidal vasculature in the fellow eyes of patients with acute central serous chorioretinopathy. Graefe’s Arch Clin Exp Ophthalmol Albr von Graefes Arch fur Klin Exp Ophthalmol. 2019;257:57–70.
Van RTJ, Van DEHC, Yzer S, Ohno-matsui K, Keunen JEE, Schlingemann RO, et al. Progress in retinal and eye research central serous chorioretinopathy: towards an evidence-based treatment guideline. Prog Retin Eye Res. 2019;73: 100770.
Iacono P, Toto L, Costanzo E, Varano M, Parravano MC. Pharmacotherapy of central serous chorioretinopathy: a review of the current treatments. Curr Pharm Des. 2018;24:4864–73.
Zola M, Daruich A, Matet A, Mantel I, Behar-Cohen F. Two-year follow-up of mineralocorticoid receptor antagonists for chronic central serous chorioretinopathy. Br J Ophthalmol. 2019;103:1184–9.
Bousquet E, Beydoun T, Zhao M, Hassan L, Offret O, Behar-Cohen F. Mineralocorticoid receptor antagonism in the treatment of chronic central serous chorioretinopathy: a pilot study. Retina. 2013;33:2096–102.
Lotery A, Sivaprasad S, O’Connell A, Harris RA, Culliford L, Ellis L, et al. Eplerenone for chronic central serous chorioretinopathy in patients with active, previously untreated disease for more than 4 months (VICI): a randomised, double-blind, placebo-controlled trial. Lancet (London, England). 2020;395:294–303.
Gao SS, Jia Y, Zhang M, Su JP, Liu G, Hwang TS, et al. Optical coherence tomography angiography. Invest Ophthalmol Vis Sci. 2016;57(9):OCT27-36.
Shinojima A, Kawamura A, Mori R, Fujita K, Yuzawa M. Findings of optical coherence tomographic angiography at the choriocapillaris level in central serous chorioretinopathy. Ophthalmol J Int d’ophtalmologie Int J Ophthalmol Zeitschrift fur Augenheilkd. 2016;236:108–13.
Iovino C, Pellegrini M, Bernabei F, Borrelli E, Sacconi R, Govetto A, et al. Choroidal vascularity index: an in-depth analysis of this novel optical coherence tomography parameter. J Clin Med. 2020;9:595.
van Rijssen TJ, Singh SR, van Dijk EHC, Rasheed MA, Vupparaboina KK, Boon CJF, et al. Prospective evaluation of changes in choroidal vascularity index after half-dose photodynamic therapy versus micropulse laser treatment in chronic central serous chorioretinopathy. Graefe’s Arch Clin Exp Ophthalmol Albr von Graefes Arch fur Klin Exp Ophthalmol. 2020;258:1191–7.
Boscia G, Viggiano P, Marzulli F, Grassi MO, Puzo P, Dore S, et al. Continuous eplerenone treatment in chronic central serous chorioretinopathy: long-term results from a pilot study. Clin Ophthalmol. 2023;17:2003–12.
Burnasheva MA, Kulikov AN, Maltsev DS. Artifact-free evaluation of choriocapillaris perfusion in central serous chorioretinopathy. Vision 2021. 2020;5:3.
Ersöz MG, Hocaoğlu M, Muslubaş IS, Arf S, Yıldız E, Karaçorlu M. Artifact-removed quantitative analysis of choriocapillaris flow voids. Turk J Ophthalmol. 2023;53:37–43.
Maltsev DS, Kulikov AN, Kazak AA. Photoreceptor outer segment layer contributes to optical coherence tomography signal attenuation beneath neurosensory detachments. Eye (Lond). 2022;36:1795–8.
Ghasemi Falavarjani K, Al-Sheikh M, Akil H, Sadda SR. Image artefacts in swept-source optical coherence tomography angiography. Br J Ophthalmol. 2017;101:564–8.
Borrelli E, Viggiano P, Evangelista F, Toto L, Mastropasqua R. Eyelashes artifact in ultra-widefield optical coherence tomography angiography. Ophthalmic Surg Lasers Imaging Retin. 2019;50:740–3.
Garrity ST, Iafe NA, Phasukkijwatana N, Chen X, Sarraf D. Quantitative analysis of three distinct retinal capillary plexuses in healthy eyes using optical coherence tomography angiography. Invest Ophthalmol Vis Sci. 2017;58:5548–55.
Viggiano P, Grassi MO, Pignataro M, Boscia G, Borrelli E, Molfetta T, et al. Topographical analysis of the choriocapillaris reperfusion after loading anti-VEGF therapy in neovascular AMD. Transl Vis Sci Technol [Internet]. 2022;11:18.
Chu Z, Cheng Y, Zhang Q, Zhou H, Dai Y, Shi Y, et al. Quantification of choriocapillaris with Phansalkar local thresholding: pitfalls to avoid. Am J Ophthalmol. 2020;213:161–76.
Bakstytė V, Šniurevičiūtė L, Šimienė E, Skruodytė J, Janulevičienė I. Determination of referential rates for optical coherence tomography and optical coherence tomography angiography flow deficits in the macular choriocapillaris in ophthalmologically healthy children. Medicina (Kaunas). 2020;56(5):238.
Canakis C, Livir-Rallatos C, Panayiotis Z, Livir-Rallatos G, Persidis E, Conway MD, et al. Ocular photodynamic therapy for serous macular detachment in the diffuse retinal pigment epitheliopathy variant of idiopathic central serous chorioretinopathy. Am J Ophthalmol. 2003;136:750–2.
Koytak A, Erol K, Coskun E, Asik N, Öztürk H, Özertürk Y. Fluorescein angiography-guided photodynamic therapy with half-dose verteporfin for chronic central serous chorioretinopathy. Retina. 2010;30:1698–703.
Struthers A, Krum H, Williams GH. A comparison of the aldosterone-blocking agents eplerenone and spironolactone. Clin Cardiol. 2008;31:153–8.
Haimovici R, Rumelt S, Melby J. Endocrine abnormalities in patients with central serous chorioretinopathy. Ophthalmology. 2003;110:698–703.
Zhao M, Célérier I, Bousquet E, Jeanny JC, Jonet L, Savoldelli M, et al. Mineralocorticoid receptor is involved in rat and human ocular chorioretinopathy. J Clin Invest. 2012;122:2672–9.
Gergely R, Kovács I, Schneider M, Resch M, Papp A, Récsán Z, et al. Mineralocorticoid receptor antagonist treatment in bilateral chronic central serous chorioretinopathy: a comparative study of exudative and nonexudative fellow eyes. Retina. 2017;37:1084–91.
Petkovsek DS, Cherfan DG, Conti FF, Hom GL, Ehlers JP, Babiuch AS, et al. Eplerenone for the treatment of chronic central serous chorioretinopathy: 3-year clinical experience. Br J Ophthalmol. 2020;104:182–7.
Warrow DJ, Hoang QV, Freund KB. Pachychoroid pigment epitheliopathy. Retina. 2013;33:1659–72.
Estawro RG, Fayed AE, Gerges TK, Baddar DN. Choriocapillaris Island: an optical coherence tomography angiography finding observed in central serous chorioretinopathy. Int J Retin Vitr. 2021. https://doi.org/10.1186/s40942-020-00275-4.
Rochepeau C, Kodjikian L, Garcia MA, Coulon C, Burillon C, Denis P, et al. Optical coherence tomography angiography quantitative assessment of choriocapillaris blood flow in central serous chorioretinopathy. Am J Ophthalmol. 2018;194:26–34.
Ho M, Lai FHP, Ng DSC, Iu LPL, Chen LJ, Mak ACY, et al. Analysis of choriocapillaris perfusion and choroidal layer changes in patients with chronic central serous chorioretinopathy randomised to micropulse laser or photodynamic therapy. Br J Ophthalmol. 2021;105:555–60.
Ghadiali Q, Jung JJ, Yu S, Patel SN, Yannuzzi LA. Central serous chorioretinopathy treated with mineralocorticoid antagonists: a one-year pilot study. Retina. 2016;36:611–8.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Pasquale Viggiano, Giacomo Boscia and Enrico Borrelli. The first draft of the manuscript was written by Pasquale Viggiano and Francesco Boscia. Lisa Toto, Maria Oliva Grassi, Federica Evangelista, Ermete Giancipoli and Giovanni Alessio commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Pasquale Viggiano, Giacomo Boscia, Enrico Borrelli, Francesco Boscia, Lisa Toto, Maria Oliva Grassi, Federica Evangelista, Ermete Giancipoli and Giovanni Alessio have nothing to disclose.
Ethical Approval
This is a retrospective study and, as for the Italian legislation, this kind of study does not require ethical approval. Only a notification to the CE is needed. Written consent was obtained from all participants included in the study, allowing for the retrospective use of their clinical data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Viggiano, P., Boscia, G., Borrelli, E. et al. Choriocapillaris Reperfusion in Resolved Chronic Central Serous Chorioretinopathy Treated with Eplerenone: Long-Term Effects on the Fellow Eye. Ophthalmol Ther 12, 3199–3210 (2023). https://doi.org/10.1007/s40123-023-00816-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00816-8