Abstract
Introduction
This study aimed to evaluate the combined administration of anti-vascular endothelial growth factor (anti-VEGF) drugs before and during pars plana vitrectomy (PPV) and to explore its efficacy and safety in the treatment of patients with severe proliferative diabetic retinopathy (PDR).
Methods
This retrospective case series included consecutive patients who underwent PPV. Patients were categorized into two groups: the preoperative group was injected with anti-VEGF drugs before PPV, and the combination group was injected with anti-VEGF drugs before and during PPV. Preoperative, intraoperative, and postoperative clinical data were collected for analysis. The main outcome measures were changes in best-corrected visual acuity (BCVA) and central retinal thickness (CRT) and occurrence of postoperative vitreous cavity haemorrhage (POVCH).
Results
In total, 63 eyes of 60 patients with severe PDR were analysed. The operative duration and occurrence of intraoperative haemorrhage, iatrogenic retinal breaks, and silicone oil tamponade were similar between the two groups. The benefits on BCVA, and CRT after 1 week postoperatively, were more obvious in the combination group (P < 0.01). Combination therapy had the potential to reduce the incidence of POVCH. No ocular or systemic adverse events occurred in either group.
Conclusions
The combined use of anti-VEGF drugs before and during PPV in patients with severe PDR not only includes the advantages of preoperative injection, but also has more significant prognostic benefits and favourable safety profiles.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The treatment of patients with severe proliferative diabetic retinopathy (PDR) has gradually changed from pars plana vitrectomy (PPV) alone to PPV combined with anti-vascular endothelial growth factor (anti-VEGF) drug therapy. |
Pretreatment of anti-VEGF drugs before PPV and injection of anti-VEGF drugs immediately at the end of PPV for patients with PDR have different advantages respectively. |
Combined use of anti-VEGF drugs before and during PPV in patients with severe PDR may achieve better treatment outcomes. |
What was learned from the study |
Combined use of anti-VEGF drugs before and during PPV in patients with severe PDR had not only the benefits associated with preoperative injection, but also pronounced prognostic advantages. Compared with single-dose administration of anti-VEGF drugs before PPV, no additional side effects associated with combined use of anti-VEGF drugs were observed. |
Combined use of anti-VEGF drugs before and during PPV may be a safe and potential therapeutic approach for the management of severe PDR. |
Introduction
Diabetic retinopathy (DR) is a common microcirculatory complication in patients with diabetes and is clinically divided into two categories: non-proliferative and proliferative [1]. The hallmark of proliferative DR (PDR) is the presence of retinal or disc neovascularization [2]. These new blood vessels are extremely immature, both in structure and function, and prone to rupture, causing repeated haemorrhages of the retina and vitreous and resulting in accelerated vitreous contraction and fibrosis. Severe PDR is often accompanied by fibrovascular proliferation (FVP), vitreous haemorrhage (VH), and tractional retinal detachment (TRD), which can significantly impair visual function [3].
Panretinal laser photocoagulation (PRP) has been the standard treatment for patients with PDR since the Diabetic Retinopathy Study was published in the 1970s [4]. As anti-vascular endothelial growth factor (anti-VEGF) drugs play an increasingly important role in DR, the primary treatment for patients with PDR is PRP with or without the use of anti-VEGF drugs. Treatment interruptions are common among patients with diabetes, possibly due to non-compliance and financial constraints, which lead to rapid progression of PDR to advanced disease [5], especially in China without definite follow-up of patients with DR. Early pars plana vitrectomy (PPV) has been suggested for such severe cases (persistent VH and TRD) to provide media clarity and remove fibrovascular tissue and VH [6, 7]. However, patients with severe PDR often experience severe retinal damage, which causes significant difficulties in performing PPV [8]. Studies have shown administration of anti-VEGF drugs perioperative at two different timings have different advantages. Preoperative intravitreal injection of anti-VEGF drugs effectively reduces iatrogenic injury and intraoperative bleeding. Injection of anti-VEGF drugs immediately after PPV reduces the possibility of early postoperative vitreous cavity haemorrhage (POVCH) because PPV can cause high VEGF levels in the vitreous cavity[9, 10]. To date, the combined preoperative and intraoperative use of anti-VEGF drugs for the treatment of severe PDR has not been reported.
The purpose of the current study was to investigate the efficacy and safety of the combined use of anti-VEGF drugs before and during PPV in the treatment of severe PDR by evaluating baseline characteristics, intraoperative condition, operative duration, postoperative central retinal thickness (CRT), postoperative best-corrected visual acuity (BCVA) and postoperative complications.
Methods
Study Design
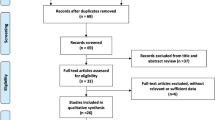
This was a single-centre, retrospective, case–control study. The data of patients admitted to our hospital and diagnosed with severe PDR according to the International Classification of Diabetic Retinopathy [11] were continuously collected from January 2019 to August 2022. Patients with TRD caused by fibrous proliferation or persistent VH were recruited. They were provided with detailed information about the two therapies and all patients understood that combination therapy would be more beneficial. Treatment was chosen on the basis of the patients’ economic or personal preferences, and all patients signed a surgical consent form. This study was a retrospective study. All patients signed a surgical consent form. This study complied with the Declaration of Helsinki, and ethics of combined use of anti-VEGF drugs for severe PDR was approved by the by the Institutional Ethics Committee of Changzhou No.2 People’s Hospital of Nanjing Medical University (YLJSA075).
Patients
Patients requiring PPV according to the Diabetic Retinopathy Preferred Practice Pattern were enrolled in this study [12]. The inclusion criteria were as follows: (1) non-clearing vitreous haemorrhage, (2) TRD encroaching the macula, (3) combined rhegmatogenous retinal detachment and TRD, and (4) dense premacular subhyaloid haemorrhage. The exclusion criteria were as follows: (1) previous PPV or intravitreal injection of anti-VEGF drugs, (2) other fundus lesions or neovascular glaucoma, (3) history of eye surgery other than that for cataract and refractive errors, and (4) history of thromboembolic events or coagulation system disorders, receiving anticoagulant or antiplatelet therapy, or other contraindications to surgery.
The recruited patients were categorized into two groups according to the time of injection of anti-VEGF drugs: patients in the preoperative group were injected with anti-VEGF drugs before PPV, and those in the combination group were injected with anti-VEGF drugs before and during PPV. The anti-VEGF drug class was selected on the basis of the wishes of the patients and their families. Standard 23-gauge 3-port PPV was performed by the same surgeon in each case. Both groups received intravitreal injections of anti-VEGF drugs 3–7 days before PPV. The combination group received anti-VEGF drug reinjections during PPV. PRP was performed in all eyes during PPV. Intraocular tamponade was performed using gas or silicone oil, if necessary. Tamponade was performed on the basis of the difficulty and complexity of the surgery.
Observed Metrics
Preoperative, intraoperative and postoperative data, including sex, age and duration of diabetes and other systemic diseases, were collected for all patients. Before surgery, all patients underwent slit-lamp microscopic fundus examination for mydriasis, ultrawide-field scanning laser ophthalmoscopy (UWF-SLO), optical coherence tomography (OCT), B-ultrasound, intraocular pressure examination, visual acuity inspection and other related inspections. Central retinal thickness (CRT) was measured using OCT (expressed in μm), and best-corrected visual acuity (BCVA) was evaluated using the international standard visual acuity chart (recorded as the logarithm of minimum resolution angle, logMAR). Counting finger vision, hand movement and light perception were recorded as 2.0 logMAR, 3.0 logMAR, and 4.0 logMAR, respectively.
All patients underwent preoperative OCT. Due to vitreous haemorrhage, the retinal interlayer thickness could not be clearly visualized in some patients. Therefore, all patients underwent CRT examination on the first day after PPV, and the measurements were considered as baseline data. Presence of intraoperative bleeding and iatrogenic retinal breaks and use of silicone oil were recorded. Intraoperative bleeding was graded according to the following grading system [13]: grade 0, no bleeding; grade 1, spontaneous cessation of minor bleeding or need of transient increase in perfusion pressure for achieving haemostasis; and grade 2, moderate-to-severe bleeding requiring intraocular electrocoagulation for achieving haemostasis or formation of large clots. Presence of POVCH was detected using fundus photography, UWF-SLO and SuperField slit-lamp lens. We defined early POVCH as haemorrhage evident from the first postoperative day or that occurred within 4 weeks postoperatively, and late POVCH as haemorrhage that occurred more than 4 weeks postoperatively after the vitreous cavity was verified to be clear [14]. Intraocular pressure (mmHg) and BCVA (logMAR) were recorded on the first postoperative day. Patients were followed up for 3 months, and fundus details, CRT, BCVA and intraocular pressure were recorded at 1 week, 1 month and 3 months postoperatively.
Statistical Analysis
Data were analysed using the SPSS version 26.0 software (IBM Corp., Armonk, NY). The Shapiro–Wilk test was used to test for the normality of continuous variables. Measurement data conforming to normal distribution are expressed as mean ± standard deviation (± s), and the independent sample Q-test or analysis of variance was used for the comparison between groups. Enumeration data are expressed by case (%), and the comparison between two groups was performed by χ2 test or Fisher’s exact probability method. All tests were two-sided, and the test level was α = 0.05.
Results
Patient Characteristics
In total, 63 eyes of 60 patients (31 men, 31 eyes; 29 women, 32 eyes) were enrolled, with 35 patients (38 eyes) in the preoperative group and 25 patients (25 eyes) in the combination group. The baseline characteristics and demographics of all patients in both groups are listed in Table 1. Sex, age, duration of diabetes, intraocular pressure, BCVA, history of PRP, duration of VH, rate of FVP and TRD, and class of anti-VEGF drugs administered (conbercept, ranibizumab or aflibercept) were not significantly different between the two groups (P > 0.05); baseline characteristics were similar between the two groups (Table 1).
Comparison of Intraoperative Condition and Operative Duration Between the Two Groups
The grades of intraoperative bleeding in the affected eyes were not significantly different between the two groups (P > 0.05) (Table 2). The haemorrhages in eyes of both groups were mainly grades 0 and 1. The average operative duration of PPV in preoperative and combination groups were 72.58 ± 7.16 min and 71.48 ± 6.33 min, respectively (P > 0.05). The occurrence of intraoperative iatrogenic retinal breaks in the preoperative and combination groups was 3/38 and 1/25, respectively (P > 0.05) and that of silicone oil tamponade in the preoperative and combination groups was 3/38 and 2/25, respectively (P > 0.05) (Table 3).
Comparison of Postoperative CRT Between the Two Groups
The CRT of the eyes of patients in the two groups 1 week, 1 month and 3 months postoperatively was decreased to different degrees compared with those 1 day postoperatively; 1 week after the operation, there was no significant difference in the CRT between the two groups (P > 0.01). However, at the 1 month and 3 months follow-up visits, the CRT in the preoperative group was significantly greater than that in the combination group (P < 0.01) (Table 3).
Comparison of Postoperative BCVA (logMAR) between the Two Groups
The BCVA of patients in both groups increased to different degrees 1 week, 1 month and 3 months postoperatively compared with that before the PPV. After 1 week, there was no significant difference in the BCVA between the two groups (P > 0.01). However, at the 1 month and 3 months follow-up visits, the BCVA of patients in the preoperative group was significantly higher than that of patients in the combination group (P < 0.01) (Table 3).
Comparison of Postoperative Complications between the Two Groups
In both groups, there was no transient intraocular hypertension or significant difference between the postoperative and preoperative intraocular pressures (P > 0.05). Early POVCH occurred in 15.8% of the eyes in the preoperative group and 4.0% of the eyes in the combination group (P = 0.23). Late POVCH was observed in 13.2% and 4.0% of the eyes in the preoperative and combination groups, respectively (P = 0.39). The overall incidence of POVCH was significantly lower in the combined group than in the preoperative group (P = 0.04). During follow-up, no ocular or systemic adverse events such as endophthalmitis, cardiovascular events or cerebrovascular events occurred in either group (Table 3).
Discussion
To the best of our knowledge, this work is the first study to investigate the efficacy and safety of the combined administration of anti-VEGF drugs before and PPV in the treatment of patients with severe PDR. Our results suggested that compared with single-dose use of anti-VEGF drugs before PPV, combined use of anti-VEGF drugs before and during PPV had pronounced prognostic advantages, with reduced intra- and postoperative complications.
PPV surgery is an effective treatment method for severe PDR. However, many neovascular membranes in the retina of patients with severe PDR re-bleed easily during the operation, not only increasing the difficulty of the operation, but also aggravating the postoperative inflammatory response due to the prolongation of the operative duration, thereby affecting the efficacy of surgery and the long-term prognosis of patients. In recent years, intravitreal injection of anti-VEGF drugs has become the mainstream treatment for diabetic retinopathy [15]. The treatment of patients with severe PDR has gradually changed from PPV alone to PPV combined with anti-VEGF drug therapy. Current clinical practice shows that injection of anti-VEGF drugs before PPV improves the success rate of surgery and reduces complications during surgery [16].
In eyes treated with PPV, POVCH is not rare. Wakabayashi et al. [17] suggested that VEGF levels in the vitreous cavity of patients with PDR after PPV are significantly increased to cope with surgical trauma and inflammation. High levels of VEGF lead to the re-proliferation of intraocular neovascularization, thereby affecting surgical efficacy. Cheema et al. [9] reported that the injection of anti-VEGF drugs at the end of PPV was effective for reducing the incidence of recurrent POVCH. Therefore, the injection of anti-VEGF drugs at different periods during the perioperative period of PPV has different advantages.
The present study found that both groups pretreated with anti-VEGF drugs had similar operative duration and incidence of intraoperative haemorrhage, intraoperative iatrogenic retinal breaks and silicone oil tamponade. These results are consistent with the findings of a meta-analysis by Zhao et al. [18], who reported that preoperative injection of anti-VEGF drugs promoted the regression of new blood vessels and fibrous membrane dissection and reduced intraoperative complications. However, in the present study, the preoperative group, which did not receive anti-VEGF drug injections at the end of surgery, did not show the same sustained effect as the combination group in terms of BCVA benefits, CRT reduction and other complications 1 week after surgery. As patients in the combination group were injected with anti-VEGF drugs at the end of PPV, higher concentrations of anti-VEGF drugs were maintained after vitrectomy. Ahn et al. [19] did not find substantial evidence to support the idea that preoperative injection of anti-VEGF drugs reduces the recurrence rate of POVCH, and suggested that injection of anti-VEGF drugs during PPV surgery may be a better option. Wakabayash et al. [17] found that high intraocular VEGF levels during vitrectomy were independent risk factors for POVCH. Although the differences between the two groups in terms of early or late POVCH were not significant in this study, the overall rate of POVCH in the combined group was significantly lower than that in the preoperative group, suggesting that combined intravitreal injections have the potential to reduce the incidence of POVCH.
The advantages of intraoperative reinjection of anti-VEGF drugs can be explained. Resection of the vitreous and repeated flushing of perfusate during PPV greatly reduce the concentration of anti-VEGF drugs injected before surgery, resulting in unsustainable postoperative benefits for patients. Gisladottir et al. [20] reported that pharmacokinetics change after PPV; the half-life of intravitreal injected drugs reduces, and the clearance increases because the vitreous body is a gel composed of collagen and glycosaminoglycan [21], which acts as a molecular barrier for drug diffusion. After PPV, the vitreous body is replaced by aqueous humour, leading to faster drug diffusion and lower drug concentration. The efficacy of the remaining anti-VEGF drugs is further decreased [22]. In addition, PPV leads to increased levels of VEGF in the eye in response to surgical trauma and inflammation, and high levels of VEGF lead to the re-proliferation of intraocular neovascularization. Therefore, injection of anti-VEGF drugs during PPV surgery not only supplements the eliminated drugs and reduces the decrease in drug efficacy due to pharmacokinetics, but also prevents the adverse effects of the VEGF surge caused by PPV. The present study of combined use of anti-VEGF drugs before and during PPV in combination group not only reduced intraoperative complications, but also improved the prognosis of patients.
Regarding the safety of intraoperative reinjection of anti-VEGF drugs, there was no significant difference in the occurrence of postoperative transient intraocular hypertension between the preoperative and combination groups, and no complications, such as endophthalmitis, cardiovascular events or cerebrovascular events, were observed in either group during follow-up. Marcus et al. [23] reported that standard dose (0.5 mg) and high-dose ranibizumab (1.0 or 2.0 mg) are well tolerated in patients with polypoidal choroidal vasculopathy. Li et al. [24] evaluated the safety and efficacy of multiple injections of 0.5 and 2.0 mg conbercept in patients with age-related macular degeneration and reported that conbercept treatment at a high dose (2.0 mg group) was generally safe and well tolerated. The present study showed that the reinjection of anti-VEGF drugs during PPV had a favourable safety profile.
Vitreous haemorrhage and silicone oil tamponade have a certain impact on CRT measurements. Many patients experience a large amount of preoperative vitreous haemorrhage, which greatly affects the accuracy of CRT measurement using OCT. We did not use preoperative CRT for statistical analysis. However, measurements performed 1 day after PPV were selected as the baseline standard, because at this time, the vitreous haemorrhage had cleared and CRT was easier to measure and the measurements were more accurate. Rabina et al. [25] suggested that silicone oil tamponade reduces the CRT of the affected eye and that the CRT of the affected eye after removing the silicone oil was similar to that of the contralateral healthy eye. Silicone oil tamponade may also affect the assessment of POVCH as blood is localised to the periphery of the posterior chamber. Therefore, caution should be exercised while interpreting the results of silicone oil tamponade.
This retrospective observational study has several limitations. First, postoperative complications and blood sugar fluctuations of the patients were not considered, and blood sugar levels were not followed up. Second, the focus of the present study was on the use of anti-VEGF drugs in the perioperative period of patients with severe PDR, and there was no significant difference in the classes of anti-VEGF drugs used between the two groups (P > 0.05); different anti-VEGF drugs may have affected the treatment efficacy, which should be further analysed in the future. Third, although there was no significant difference in the baseline data between the preoperative group and the combination group, the combination group required two injections of anti-VEGF drugs, which would impose a greater financial burden and therefore lead to drug selection bias. Moreover, the sample size of the present study was small; a multicentre prospective study with a larger sample size and a more complete and longer follow-up is needed to validate the results of the present study.
Conclusions
The combined use of anti-VEGF drugs before and during PPV in patients with severe PDR not only includes the advantages of preoperative injection, but also has greater significant prognostic benefits and favourable safety profiles. It may be a safe and potential therapeutic approach for the management of severe PDR.
Data Availability
Data are available upon reasonable request to the corresponding author.
References
Wong TY, Cheung CM, Larsen M, et al. Diabetic retinopathy. Nat Rev Dis Primers. 2016;17(2):16012. https://doi.org/10.1038/nrdp.2016.12.
Vaz-Pereira S, Zarranz-Ventura J, Sim DA, et al. Optical coherence tomography features of active and inactive retinal neovascularization in proliferative diabetic retinopathy. Retina. 2016;36(6):1132–42. https://doi.org/10.1097/IAE.0000000000000869.
Crabtree GS, Chang JS. Management of complications and vision loss from proliferative diabetic retinopathy. Curr Diab Rep. 2021;21(9):33. https://doi.org/10.1007/s11892-021-01396-2.
Everett LA, Paulus YM. Laser therapy in the treatment of diabetic retinopathy and diabetic macular edema. Curr Diab Rep. 2021;21(9):35. https://doi.org/10.1007/s11892-021-01403-6.
Berrocal MH, Acaba-Berrocal L. Early pars plana vitrectomy for proliferative diabetic retinopathy: update and review of current literature. Curr Opin Ophthalmol. 2021;32(3):203–8. https://doi.org/10.1097/ICU.0000000000000760.
Gross JG, Glassman AR, Liu D, et al. Five-year outcomes of panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA Ophthalmol. 2018;136(10):1138–48. https://doi.org/10.1001/jamaophthalmol.2018.3255.
Du W, Chen WQ, Yu WZ, et al. Analysis of factors affecting revitrectomy in patients with proliferative diabetic retinopathy. Zhonghua Yi Xue Za Zhi. 2022;102(18):1389–93. https://doi.org/10.3760/cma.j.cn112137-20210909-02055.
Simunovic MP, Maberley DA. Anti-vascular endothelial growth factor therapy for proliferative diabetic retinopathy: a systematic review and meta-analysis. Retina. 2015;35(10):1931–42. https://doi.org/10.1097/IAE.0000000000000723.
Cheema RA, Mushtaq J, Al-Khars W, et al. Role of intravitreal bevacizumab (avastin) injected at the end of diabetic vitrectomy in preventing postoperative recurrent vitreous hemorrhage. Retina. 2010;30(10):1646–50. https://doi.org/10.1097/IAE.0b013e3181d6def0.
West JF, Gregor ZJ. Fibrovascular ingrowth and recurrent haemorrhage following diabetic vitrectomy. Br J Ophthalmol. 2000;84(8):822–5. https://doi.org/10.1136/bjo.84.8.822.
Wilkinson CP, Ferris FLR, Klein RE, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110(9):1677–82. https://doi.org/10.1016/S0161-6420(03)00475-5.
Flaxel CJ, Adelman RA, Bailey ST, et al. Diabetic retinopathy preferred practice pattern®. Ophthalmology. 2020;127(1):66–145. https://doi.org/10.1016/j.ophtha.2019.09.025.
Arevalo JF, Lasave AF, Kozak I, et al. Preoperative bevacizumab for tractional retinal detachment in proliferative diabetic retinopathy: a prospective randomized clinical trial. Am J Ophthalmol. 2019;207:279–87. https://doi.org/10.1016/j.ajo.2019.05.007.
Smith JM, Steel DH. Anti-vascular endothelial growth factor for prevention of postoperative vitreous cavity haemorrhage after vitrectomy for proliferative diabetic retinopathy. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD008214.pub3.
Pandit Saagar, Ho AC, Yonekawa Yoshihiro. Advances in the management of proliferative diabetic retinopathy. Curr Opin Ophthalmol. 2023;34(3):232–6. https://doi.org/10.1097/ICU.0000000000000946.
Zhao XY, Xia S, Chen YX. Antivascular endothelial growth factor agents pretreatment before vitrectomy for complicated proliferative diabetic retinopathy: a meta-analysis of randomised controlled trials. Br J Ophthalmol. 2018;102(8):1077–85. https://doi.org/10.1136/bjophthalmol-2017-311344.
Wakabayashi Y, Usui Y, Tsubota K, et al. Persistent overproduction of intraocular vascular endothelial growth factor as a cause of late vitreous hemorrhage after vitrectomy for proliferative diabetic retinopathy. Retina. 2017;37(12):2317–25. https://doi.org/10.1097/IAE.0000000000001490.
Wang DY, Zhao XY, Zhang WF, et al. Perioperative anti-vascular endothelial growth factor agents treatment in patients undergoing vitrectomy for complicated proliferative diabetic retinopathy: a network meta-analysis. Sci Rep. 2020;10(1):18880. https://doi.org/10.1038/s41598-020-75896-8.
Ahn J, Woo SJ, Chung H, et al. The effect of adjunctive intravitreal bevacizumab for preventing postvitrectomy hemorrhage in proliferative diabetic retinopathy. Ophthalmology. 2011;118(11):2218–26. https://doi.org/10.1016/j.ophtha.2011.03.036.
Gisladottir S, Loftsson T, Stefansson E. Diffusion characteristics of vitreous humour and saline solution follow the stokes Einstein equation. Graefes Arch Clin Exp Ophthalmol. 2009;247(12):1677–84. https://doi.org/10.1007/s00417-009-1141-3.
Edington M, Connolly J, Chong NV. Pharmacokinetics of intravitreal anti-vegf drugs in vitrectomized versus non-vitrectomized eyes. Expert Opin Drug Metab Toxicol. 2017;13(12):1217–24. https://doi.org/10.1080/17425255.2017.1404987.
Niwa Y, Kakinoki M, Sawada T, et al. Ranibizumab and aflibercept: intraocular pharmacokinetics and their effects on aqueous vegf level in vitrectomized and nonvitrectomized macaque eyes. Invest Ophthalmol Vis Sci. 2015;56(11):6501–5. https://doi.org/10.1167/iovs.15-17279.
Marcus DM, Singh H, Fechter CM, et al. High-dose ranibizumab monotherapy for neovascular polypoidal choroidal vasculopathy in a predominantly non-Asian population. Eye (Lond). 2015;29(11):1427–37. https://doi.org/10.1038/eye.2015.150.
Li X, Xu G, Wang Y, et al. Safety and efficacy of conbercept in neovascular age-related macular degeneration: results from a 12-month randomized phase 2 study: AURORA study. Ophthalmology. 2014;121(9):1740–7. https://doi.org/10.1016/j.ophtha.2014.03.026.
Rabina G, Azem N, Barequet D, et al. Silicone oil tamponade effect on macular layer thickness and visual acuity. Retina. 2020;40(5):998–1004. https://doi.org/10.1097/IAE.0000000000002464.
Authorship
All authors in this report meet the authorship criteria from the International Committee of Medical Journal Editors (ICMJE), take full responsibility for the entire work and approved the final version of the manuscript.
Editorial Assistance
We would like to thank Editage (www.editage.com) for English language editing, which was funded by the authors.
Funding
This study, and the journal’s Rapid Service fee, were funded by grants from Changzhou High-Level Medical Talents Training Project (2022CZBJ075).
Author information
Authors and Affiliations
Contributions
Hu Liu and Xincheng Sun provided the conceptualisation and design of the study. Xianhuai Wang completed the data collection. Mengjiao Wang analysed and interpreted the data. Xincheng Sun and Xianhuai Wang wrote the manuscript. Xinyu Guo provided critical revisions to the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Xincheng Sun, Xianhuai Wang, Xinyu Guo, Mengjiao Wang and Hu Liu all confirm that they have no conflicts of interest to disclose.
Ethical Approval
This study was a retrospective study. All patients signed a surgical consent form. This study followed the tenets of the Declaration of Helsinki and ethics of combined use of anti-VEGF drugs for severe PDR was approved by the by the Institutional Ethics Committee of Changzhou No.2 People’s Hospital of Nanjing Medical University (YLJSA075).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sun, X., Wang, X., Guo, X. et al. Combined Use of Anti-VEGF Drugs Before and During Pars Plana Vitrectomy for Severe Proliferative Diabetic Retinopathy. Ophthalmol Ther 12, 3133–3142 (2023). https://doi.org/10.1007/s40123-023-00803-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00803-z