Abstract
Introduction
We investigated the frequency of uveitic macular edema (UME) in patients with different types of noninfectious uveitis and present the primary treatment methods for UME at a specialized eye center in Shaanxi Province, China.
Methods
We conducted a retrospective, noninterventional, observational survey involving 1946 patients with noninfectious uveitis (2816 eyes). The collected data included sex, age of uveitis onset, age of UME onset, anatomical classification of uveitis, and the treatment administered to UME patients.
Results
Of the 1946 patients with noninfectious uveitis, 929 (47.74%) were male and 1017 (52.26%) were female. The average age of all participants in the study was 42.19 ± 15.34 years, with average age at uveitis onset of 39.50 ± 15.52 years. Among the patients, 1003 (51.54%), 239 (12.28%), 410 (21.07%), and 294 (15.11%) had anterior uveitis, intermediate uveitis, posterior uveitis, and panuveitis, respectively. UME was observed in 134 (6.89%) of the uveitis patients. The average age of UME patients was 47.33 ± 17.17 years, with average age at uveitis onset of 45.78 ± 17.20 years. Out of the 134 UME patients, 3 (0.30%), 15 (6.28%), 47 (11.46%), and 69 (23.47%) had anterior uveitis, intermediate uveitis, posterior uveitis, and panuveitis, respectively. Among them, 37 were lost to follow-up, 44 received adalimumab (ADA) combined with low-dose prednisone and with or without conventional immunosuppressants, 19 received interferon-α2a therapy, 14 received intravitreal corticosteroid injections (such as dexamethasone implant or fluocinolone acetonide), 11 received low-dose corticosteroids combined with conventional immunosuppressants, 5 received only oral prednisone, and 4 received repeated peribulbar or subconjunctival injections of triamcinolone acetonide.
Conclusions
At our tertiary ophthalmic center in Shaanxi Province, China, only 6.89% of patients with noninfectious uveitis were diagnosed with UME. The primary treatment modality for UME in our center is ADA, in accordance with treatment guidelines and the Chinese medical insurance reimbursement system.
Plain Language Summary
Macular edema is a common complication that can cause vision loss in patients with uveitis. However, there is limited information about the occurrence of uveitic macular edema in the past two decades, and existing data mainly focus on developed countries such as the Netherlands and Italy. There are no relevant data for Asian countries such as China or Japan. In this study, we examined the frequency of uveitic macular edema in 1946 patients (2816 eyes) with different types of noninfectious uveitis who received treatment at a specialized eye center in Shaanxi Province, China, between January 2021 and October 2022. Among the uveitis patients, only 134 (6.89%) had uveitic macular edema. Out of these 134 patients, 3 (0.30%), 15 (6.28%), 47 (11.46%), and 69 (23.47%) had anterior uveitis, intermediate uveitis, posterior uveitis, and panuveitis, respectively. Additionally, we analyzed the treatment methods used for uveitic macular edema patients. In our center, the primary treatment approach for uveitic macular edema is adalimumab, in accordance with treatment guidelines and the Chinese medical insurance reimbursement system. Other treatment strategies include interferon-α2a therapy, intravitreal dexamethasone implants, and low-dose corticosteroids combined with conventional immunosuppressants. Our research provides valuable insights into the occurrence of uveitic macular edema in noninfectious uveitis patients and the current treatment practices at a single medical center in Shaanxi, China.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Macular edema (ME) is a common vision-threatening complication in patients with uveitis. Uveitic ME (UME) significantly differs in frequency and type across populations. Various treatment options are available for UME. This is a retrospective analysis of the frequency of UME in 1946 patients with noninfectious uveitis visiting the uveitic service of a tertiary eye care center in Northwest China and the relevant treatment regimens. |
What was learned from the study? |
Our findings suggest that the frequency of UME in patients with noninfectious uveitis was only 6.89%. As there is no strict three-level referral system in China, many patients with mild uveitis visit our center, which may explain the lower rates of UME recorded in our study compared with those reported previously. Moreover, adalimumab was the primary treatment option for UME in our study, followed by interferon-α2a, intraocular corticosteroid, and low-dose corticosteroids combined with conventional immunosuppressants. Determining the treatment regimen depends on comprehensive factors, including the patient’s condition, medical insurance, financial condition, and desires. |
Introduction
Uveitis accounts for 5–20% of cases of blindness in developed countries and up to 25% of cases of blindness in developing countries [1, 2]. Based on its etiology, uveitis can be divided into infectious and noninfectious uveitis. Further, based on its anatomical structure, uveitis can be divided into four subtypes: anterior uveitis, intermediate uveitis, posterior uveitis, and panuveitis. This classification is based on the criteria recommended by the Standardization of Uveitis Nomenclature (SUN) working group. The location of inflammation affects the occurrence of complications and the prognosis of visual acuity [3, 4].
Macular edema (ME) is a common structural ocular complication in patients with uveitis. ME leads to vision loss and is the main reason for declined visual acuity in patients with uveitis [5]. Because uveitis is a group of highly heterogeneous diseases, there are considerable differences in the incidence and types of uveitis in different populations influenced by socioeconomic environments, ethnicities, and geographic distribution. Similarly, the above-mentioned factors affect the incidence of uveitic ME (UME) [4, 5]. Sungur et al. reported that UME was less common in African patients (26.5%) than in Asian (42.6%) or Caucasian (46.0%) patients with intermediate uveitis [6, 7]. Unfortunately, data on UME incidence are limited in the previous 20 years. Relevant data have only been reported for developed countries, such as the Netherlands and Italy; data for Asian countries, such as China or Japan, are currently missing.
UME often occurs in patients with chronic uveitis. This condition can be stable for a long time following drug treatment. A decade ago, conventional immunosuppressants were the mainstream drugs for noninfection uveitis treatment in China. However, with the advent of novel biologics, chronic noninfectious uveitis is increasingly being treated using targeted therapy, including tumor necrosis factor antagonists. Simultaneously, systemic corticosteroids, peribulbar corticosteroids, interferon-α2a (IFN-α2a), and intraocular corticosteroids including 0.7-mg dexamethasone intravitreal implant and 0.18-mg fluocinolone acetonide intravitreal implant are being used to treat UME. The preference for the UME treatment modality may differ worldwide. Considering that various therapeutic options are available, the final treatment plan is based on individual patient factors, the healthcare system, and insurance reimbursement.
The present study evaluated the frequency of UME in patients with different anatomical types of noninfectious uveitis who visited our uveitis service at a tertiary ophthalmic center in Shaanxi Province, China between January 2021 and October 2022. Optical coherence tomography (OCT) was used as the detection method. We also analyzed the number of patients who received different treatment regimens.
Methods
Study Population
In this retrospective, nonrandomized study, we screened 2122 consecutive patients with uveitis who visited the uveitis service of the ophthalmology department at Xi’an People’s Hospital (Xi’an Fourth Hospital) (Shannxi, China) between January 2021 and October 2022. The inclusion criterion for the patients was a confirmed diagnosis of noninfectious uveitis. Among these patients, 97 were excluded from the study for the following reasons: OCT image was not distinguishable owing to the opacity of the refractive medium, not willing to undergo OCT, and not meeting the inclusion criterion. Finally, 1946 patients (2816 eyes) were included. Our ophthalmic department is the tertiary referral center in Shaanxi Province, China. Apart from accepting referred patients, our institution also primarily caters to direct patient care, similar to all tertiary medical institutions in China. Eyes with any coexisting ocular diseases, including age-related macular degeneration, diabetic retinopathy, hypertensive retinopathy, or retinal vein occlusion, were excluded. A retrospective analysis of the clinical data was performed in accordance with the principles of the Declaration of Helsinki. This study has been reviewed by the Ethics Committee of Xi'an People's Hospital (Xi’an Fourth Hospital). Considering the retrospective nature of this study, informed consent was waived.
Data Collection
The patients provided detailed demographic data and clinical history records and underwent ocular examinations, including slit-lamp examination and funduscopic and auxiliary examinations such as OCT. After undergoing all examinations, the anatomical site of the inflammation was used to classify the uveitis based on SUN criteria [8]. After that, for patients receiving systemic treatment or intravitreal corticosteroid injections, we conducted additional laboratory tests, including routine blood tests, C-reactive protein and erythrocyte sedimentation rate, liver and kidney function tests, blood sugar levels, tuberculosis interferon-gamma release assay, antinuclear antibody assay, and chest computed tomography. For patients receiving local steroid therapy, including the use of eye drops, peribulbar, or subconjunctival steroids, we did not necessarily conduct the above-mentioned examinations. The onset time of uveitis was recorded, and the changes in intraocular inflammation were followed up. OCT was performed at least once a month for patients with concurrent UME for observation until the UME completely subsided or improved.
UME Treatment
The treatment regimens for patients with UME were as follows:
-
Peribulbar or subconjunctival injection of triamcinolone acetonide (TA)
-
Only systemic oral corticosteroids (initial dose of ≥ 0.5 mg/kg prednisone)
-
Low-dose corticosteroids (initial dose of < 0.5 mg/kg prednisone, which was reduced to no more than 7.5 mg/day or discontinued within 8 weeks) combined with one or two conventional immunosuppressants (either cyclosporine [≤ 200 mg/day] or tacrolimus [≤ 2 g/day], with/without either methotrexate [≤ 17.5 mg/week] or azathioprine [≤ 150 mg/day])
-
Adalimumab (ADA, Humira; AbbVie, Chicago, IL, USA; or Anjianning; Bioray, Taizhou, Zhejiang province, CHN; starting dose of 80 mg, 40 mg after 1 week, after that, 40 mg every 2 weeks for adults, and for children weighing < 30 kg, half the dose was used) combined with low-dose corticosteroids (prednisone starting dose of < 0.5 mg/kg, which was gradually reduced to no more than 7.5 mg/day or discontinued within 8 weeks) and without or with conventional immunosuppressants (either methotrexate [≤ 17.5 mg/week] or azathioprine [≤ 150 mg/day])
-
IFN-α2a (Intefen; 3SBIO INC., Shenyang, Liaoning province, CHN; at an initial dose of 3 million international units (MIU)/day subcutaneously during the first 2 weeks, followed by 3 MIU every 2–3 days as a maintenance dose according to the patient’s response)
-
Intravitreal injection of 0.7 mg dexamethasone (Ozurdex; Allergan, Inc., Irvine, CA, USA)
-
Intravitreal injection of fluocinolone acetonide intravitreal implant 0.18 mg (Yutiq; EyePoint Pharmaceuticals, Watertown, MA, USA)
The doctors (Y.C. and J.-A.X.) introduced the aforementioned treatment regimens to patients with UME. They recommended the most suitable one for patients based on the duration of uveitis, the presumed etiology, recurrence frequency, combined systemic comorbidities, age, and other factors. However, some patients do not accept the treatment regimen the doctor recommends. Instead, they select the regimen based on their medical insurance, financial conditions, and personal desires. If patients did not respond to the administered treatment regimen, the doctors recommended switching to the following regimen according to the flow diagram of treatment regimens at our center (Fig. 1). If the duration of uveitis was ≤ 3 months, oral corticosteroids or peribulbar/subconjunctival injection of TA was initially recommended; if the duration of uveitis was > 3 months or patients showed a possible association with systemic immune diseases, low-dose prednisone combined with one or two conventional immunosuppressants, or ADA combined with low-dose corticosteroids and with/without conventional immunosuppressants was recommended initially. If the duration of uveitis was > 3 months and the patient’s age was > 65 years, intravitreal injection of corticosteroids was recommended first. IFN-α2a was not recommended initially.
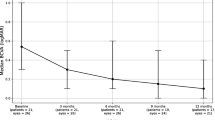
Observation of UME on OCT
All patients underwent horizontal, vertical, and two oblique scans of spectral-domain OCT (Spectralis, Heidelberg Engineering, Germany). UME was diagnosed by two experienced ophthalmologists (Y.C. and J.-A.X.): the presence of intraretinal or subretinal cysts, with/without central macular thickening (≥ 240 μm) on OCT indicated UME. UME was not diagnosed if an edema cyst or submacular fluid was not observed on any of the four B-scans. Patients with Vogt–Koyanagi–Harada syndrome with exudative retinal detachment were not included in the case of UME. Whether UME improved was judged by the above-mentioned two ophthalmologists through comparing the OCT scans obtained before and after treatment. The OCT images of patients after receiving different treatment regimens were obtained at the following time points: at the beginning of treatment in the fourth week for patients who received peribulbar or subconjunctival injections of TA, medium- or high-dose systemic oral corticosteroids, IFN-α2a, and intravitreal injection of 0.7 mg dexamethasone; at least 2 months after prednisone reduction to ≤ 7.5 mg/day for those who received low-dose corticosteroids combined with one or two conventional immunosuppressants and who received ADA combined with low-dose corticosteroids and with/without conventional immunosuppressants (azathioprine/methotrexate); in the third month after injection for those who received an intravitreal injection of 0.18 mg fluocinolone acetonide. Improvement of UME was specifically defined as intraretinal and subretinal cysts completely subsided or a ≥ 20% reduction in central foveal thickness as measured by the OCT images, not requiring the resolution of all cystoid spaces.
Statistical Methods
Statistical analysis of the collected data was conducted to determine the average and standard deviation (SD) values for age, the number of patients with different anatomical types of uveitis, and the number of patients with unilateral or bilateral uveitis. Further, descriptive analysis was performed, where categorical variables are presented as frequencies and percentages. A corrected P value of < 0.05 was considered statistically significant.
Results
The study subjects were 1946 consecutive patients (2816 eyes) who were diagnosed with noninfectious uveitis at the uveitis service of the ophthalmology department at Xi’an People’s Hospital (Xi'an Fourth Hospital) from January 2021 to October 2022. Of the total uveitis cases, 75% were from Shaanxi Province, 19% were from nearby Gansu Province, while the remaining patients from the Qinghai, Xinjiang, and Ningxia provinces or other northwestern regions of China. All patients were managed and followed up by two ophthalmologists (Y.C. and J.-A.X.). In total, 929 (47.74%) men and 1017 (52.26%) women were included. The age of all patients at study participation was 42.19 ± 15.34 years, which is significantly less than the age of patients with UME at study participation, which was 47.33 ± 17.17 years (P < 0.05). Similarly, the age of all patients at onset of uveitis was 39.50 ± 15.52 years, significantly younger than the age of patients with UME at onset of uveitis of 45.78 ± 17.20 years (P < 0.05). The most common type of uveitis was anterior uveitis (1003 [51.54%]), followed by posterior uveitis (410 [21.07%]), panuveitis (294 [15.11%]), and intermediate uveitis (239 [12.28%]). Among the 1946 patients with noninfectious uveitis, 134 (6.89%) had UME. The most common anatomical type of UME was panuveitis (23.47% [69/294]), followed by posterior uveitis (11.46% [47/410]), intermediate uveitis (6.28% [15/239]), and anterior uveitis (0.30% [3/1003]) (Table 1). Our study results suggest that patients with bilateral uveitis are more prone to UME than those with monocular uveitis (10.57% versus 3.90%, P < 0.005). Further, in patients with panuveitis in both eyes, the frequency of UME was as high as 24.04% (Table 2).
Application of Treatment Regimens for UME
In total, 134 patients had UME. Of these, 37 were lost to follow-up. Therefore, the outcomes of only 97 patients were determined. If a patient was sequentially treated with more than one regimen because the previous regimens were ineffective, the patient was classified into the last effective treatment regimen group. UME improved in 44 patients who received ADA combined with low-dose prednisone and with/without conventional immunosuppressants. Among the patients who received IFN-α2a therapy, UME showed improvement in all 19 individuals. Notably, of these patients, five patients who initially received ADA treatment and experienced treatment failure subsequently switched to IFN-α2a therapy, leading to successful control of UME. However, UME still recurred after 6 months in one patient who was switched to IFN-α2a therapy. UME also improved in 13 patients who received an intravitreal injection of 0.7 mg dexamethasone and in one who received an intravitreal injection of 0.18 mg fluocinolone acetonide. UME was found to be controlled in five patients who received only systemic prednisone therapy with a dosage of 10–20 mg/day. UME also improved in 11 patients who received low-dose prednisone combined with conventional immunosuppressants. Four patients received repeated peribulbar or subconjunctival injections of TA to control UME, and the relapse was frequent.
Discussion
We retrospectively analyzed the frequency of and treatment regimens for UME in patients with noninfectious uveitis who visited the uveitis service of a tertiary ophthalmic center in Shaanxi Province, China between January 2021 and October 2022.
We observed that the frequency of UME in 1946 consecutive patients with noninfectious uveitis was 6.89%; this is significantly lower than that reported by Rothova et al., Lardenoye et al., and van Kooij et al. (26%, 33%, and 44%, respectively) [9,10,11]. This difference can be attributed to the fact that the proportion of nonanterior uveitis, including intermediate uveitis, posterior uveitis, and panuveitis, was relatively lower in our study (48.46%) than in the three studies mentioned above (53.94%, 55.43%, and 93%). Moreover, it is well known that nonanterior uveitis is the primary anatomic subtype complicated by UME. Because the ophthalmology department at Xi’an People's Hospital is not only a referral center but also a center catering to direct patient care, a high number of anterior uveitis cases are observed at the uveitis services, while the studies of Rothova et al., Lardenoye et al., and van Kooij et al. were conducted in centers that combine secondary and tertiary ophthalmological care, resulting in a bias toward more complicated intermediate uveitis, posterior uveitis, or panuveitis cases [9,10,11]. Therefore, our data may reflect the unskewed incidence of UME in Shaanxi Province, China. Similar to our data sources, Mercanti et al. provided their results from a direct care facility and a referral center. In their study, the frequency of anterior uveitis was as high as 58.02%, and nonanterior uveitis accounted for 41.98% of cases, resulting in the frequency of UME being only 1.53% [12]. The type of uveitis may be closely related to socioeconomic conditions, ethnicities, regions, periods, and other factors, leading to differences in concurrent UME. The patients included in the studies by Rothova et al., Lardenoye et al., and van Kooij et al. were from the Dutch population between the 1990s and 2008 [9,10,11]. Most patients in our study were from Shaanxi, China, in 2021 and 2022, with a small number of patients living in Northwest China, including Gansu, Qinghai, Xinjiang, and other places. This may explain the discrepancy in the frequency of UME between our study and that reported in the other three studies. Moreover, we found that the patients with bilateral uveitis were more prone to UME than those with unilateral uveitis. We believe that patients with bilateral uveitis have more pronounced systemic immune disorders, resulting in more severe eye inflammation in these patients, thereby increasing the risk of UME.
UME can be treated using various drugs, including systemic or local corticosteroids, conventional or biological immunosuppressants, and interferons [13]. In our study, most patients received ADA combined with low-dose corticosteroids and with/without immunosuppressants (methotrexate or azathioprine). The main reason for this was that there are well-defined recommended guidelines for using ADA to treat noninfectious intermediate uveitis, posterior uveitis, and panuveitis, which are anatomical types of uveitis having a relatively higher risk to complicate UME [14, 15]. Furthermore, ADA use is covered by medical insurance in most parts of China, and the price after reimbursement is relatively low. After reimbursement, the total monthly treatment price is approximately 700–1000 RMB (equivalent to 120 US dollars); as a result, long-term treatment costs are affordable for most patients. Although there is accumulated evidence on using conventional immunosuppressants to treat uveitis, their use is relatively less among our patients with UME. This is because we are inclined to believe that ADA could have a superior efficacy when compared with conventional immunosuppressants such as cyclosporine and methotrexate in controlling autoimmune diseases [16]. Furthermore, medical insurance does not cover conventional immunosuppressants when used to treat uveitis. Therefore, their total monthly treatment cost is higher than that for ADA after reimbursement. As a result, our patients prefer to use biological immunosuppressants. Nevertheless, ADA is ineffective in a minority of UME cases complicated by noninfectious uveitis. We recommend that patients undergo IFN-α2a or intraocular corticosteroid therapy when there is treatment failure. In our study, five patients with UME who did not respond to ADA treatment underwent IFN-α2a therapy, with their UME being more effectively controlled. Unfortunately, UME relapsed in one patient with sympathetic ophthalmia who received IFN-α2a for 6 months. We believe that IFN-α2a had a significantly superior efficacy toward improving UME in our clinical practice. Several reports also suggest that IFN-α2a is very effective in treating refractory UME [17,18,19,20], possibly because IFN-α2a enhances the blood–retina barrier function [21]. Owing to the low price of IFN-α2a, some patients who cannot afford ADA or do not have health insurance tend to have to accept IFN-α2a therapy when treated for the first time. Therefore, in our study, the number of patients who received interferon-α2a therapy for UME was second only to those who received ADA.
Only patients > 65 years, those at a higher risk for systemic immunosuppressive therapy, or those with refractory UME with multiple treatment failures received intraocular corticosteroids. Therefore, the number of these patients was not significant. For patients unwilling to accept the long-term use of immunomodulators and intraocular corticosteroids, we used only repeated periorbital corticosteroid injections or systemic corticosteroids; however, UME was poorly controlled due to recurrence.
Thirty-seven patients were lost to follow-up. Most of them lived far away from our study center. Moreover, during the observation period between January 2021 and October 2022, China had a strict policy of repeated regional closure and control of the COVID-19 pandemic, making it inconvenient for patients to seek medical treatment. Therefore, they switched to local or other hospitals for treatment.
Our study has certain limitations that should be acknowledged. Firstly, it is crucial to recognize that this analysis was conducted as a retrospective study within a single center, which introduces a potential indication bias. In our study, UME diagnosis was based on OCT findings. Although OCT offers a more accurate assessment of macular edema, we conducted limited scans, including horizontal, vertical, and two oblique B-scans. Consequently, there is a possibility of missing UME diagnosis in some patients with small intraretinal edema cysts not detected in the obtained B-scans. Additionally, a study by Kempen et al. has reported that 40% of patients without cystoid macular edema on OCT showed macular leakage on fundus fluorescein angiography (FFA), indicating that the detection rate of UME using OCT may be lower than that of FFA [22].
Furthermore, some patients only made a single visit to our center and were subsequently lost to follow-up. Therefore, it was impossible to determine whether UME developed in the later stages for these individuals. These factors may have resulted in an underestimation of the true frequency of UME. Additionally, since our study is based on real-world analysis, some patients declined certain examinations due to limitations in medical insurance coverage or personal financial circumstances. As a result, effective classification of cases based on their etiologies was not feasible, and treatment options could not be adequately tailored to specific etiologies.
Conclusions
In summary, our research provides evidence regarding the incidence of UME among patients with noninfectious uveitis, which was found to be 6.89% in our single-center analysis conducted in Shaanxi, China. Various treatment options are available for UME, and our study revealed that ADA has emerged as the primary treatment modality, followed by IFN-α2a and intraocular corticosteroid therapies. The choice of treatment strategy was based on comprehensive considerations, including the patient’s clinical condition, available medical insurance coverage, financial resources, and personal preferences.
References
Miserocchi E, Fogliato G, Modorati G, et al. Review on the worldwide epidemiology of uveitis. Eur J Ophthalmol. 2013;23:705–17.
Thorne JE, Suhler E, Skup M, et al. Prevalence of non-infectious uveitis in the United States: a claims-based analysis. JAMA Ophthalmol. 2016;134(11):1237–45.
Bloch-Michel E, Nussenblatt RB. International Uveitis Study Group recommendations for the evaluation of intraocular inflammatory disease. Am J Ophthalmol. 1987;103:234–5.
Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of Uveitis Nomenclature(SUN)Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140:509–16.
Durrani OM, Tehrani NM, Marr JE, et al. Degree, duration, and causes of visual loss in uveitis. Br J Ophthalmol. 2004;88:1159–62.
Sungur G, Yakin M, Uzman S, Balta O, Orman G, Ornek F. Clinical features and prognosis of uveitis in a Turkish patient population with ankylosing spondylitis: incidence and management of ocular complications. Ocul Immunol Inflamm. 2019;27(4):551–9.
Niederer RL, Sharief L, Bar A, Lightman SL, Tomkins- NO. Predictors of long-term visual outcome in intermediate Uveitis. Ophthalmology. 2017;124(3):393–8.
Iannetti L, Spinucci G, Abbouda A, de Geronimo D, Tortorella P, Accorinti M. Spectral-domain optical coherence tomography in uveitic macular edema: morphological features and prognostic factors. Ophthalmologica. 2012;228:13–8.
Rothova A, Suttorp-van Schulten MS, Frits Treffers W, Kijlstra A. Causes and frequency of blindness in patients with intraocular inflammatory disease. Br J Ophthalmol. 1996;80:332–6.
Lardenoye CWTA, van Kooij B, Rothova A. Impact of macular edema on visual acuity in uveitis. Ophthalmology. 2006;113(8):1446–9.
van Kooij B, Probst K, Fijnheer R, Roest M, de Loos W, Rothova A. Risk factors for cystoid macular oedema in patients with uveitis. Eye (Lond). 2008;22(2):256–60.
Mercanti A, Parolini B, Bonora A, Lequaglie Q, Tomazzoli L. Epidemiology of endogenous uveitis in north-eastern Italy. Analysis of 655 new cases. Acta Ophthalmol Scand. 2001;79(1):64–8.
Li YH, Hsu SL, Sheu SJ. A review of local therapy for the management of cystoid macular edema in uveitis. Asia Pac J Ophthalmol (Phila). 2021;10(1):87–92.
Dick AD, Rosenbaum JT, Al-Dhibi HA, et al. Fundamentals of Care for Uveitis International Consensus Group. Guidance on noncorticosteroid systemic immunomodulatory therapy in non-infectious uveitis: Fundamentals of Care for UveitiS (FOCUS) Initiative. Ophthalmology. 2018;125:757–73.
Levy-Clarke G, Jabs DA, Read RW, Rosenbaum JT, Vitale A, Van Gelder RN. Expert panel recommendations for the use of anti-tumor necrosis factor biologic agents in patients with ocular inflammatory disorders. Ophthalmology. 2014;121:785-96.e3.
Jaffe GJ, Dick AD, Brézin AP, et al. Adalimumab in patients with active non-infectious uveitis. N Engl J Med. 2016;375:932–43.
Deuter CM, Kötter I, Günaydin I. Efficacy and tolerability of interferon alpha treatment in patients with chronic cystoid macular oedema due to non-infectious uveitis. Br J Ophthalmol. 2009;93(7):906–13.
De Simone L, Sangiovanni A, Aldigeri R. Interferon Alpha-2a Treatment for Post-Uveitic Refractory Macular Edema. Ocul Immunol Inflamm. 2020;28(2):322–8.
Deuter CM, Koetter I, Guenaydin I. Interferon alfa-2a: a new treatment option for long lasting refractory cystoid macular edema in uveitis? A pilot study Retina. 2006;26(7):786–91.
Stiefel HC, Kopplin LJ, Albini T. Treatment of refractory cystoid macular edema with pegylated interferon alfa-2A: a retrospective chart review. Ocul Immunol Inflamm. 2021;29(3):566–71.
Gillies MC, Su T. Interferon-alpha 2b enhances barrier function of bovine retinal microvascular endothelium in vitro. Microvasc Res. 1995;49(3):277–88.
Kempen JH, Sugar EA, Jaffe GJ. Multicenter Uveitis Steroid Treatment (MUST) Trial Research Group. Fluorescein angiography versus optical coherence tomography for diagnosis of uveitic macular edema. Ophthalmology. 2013;120(9):1852–9.
Acknowledgments
Funding
This research did not receive any external funding. The journal’s Rapid Service fee was covered by the authors.
Editorial Assistance
We want to express our gratitude to Medjaden Biosciences Ltd. for providing English language editing support. Editorial support was funded by the authors.
Author Contributions
Chen Ying and Yan-Qi Xue designed the study and prepared the manuscript. Chen Ying, Jin-An Xiao, and Yan-Qi Xue collected the data. All authors have reviewed and approved the final manuscript.
Disclosures
Yan-Qi Xue, Jin-An Xiao, and Chen Ying confirm that they have no competing interests to declare.
Compliance with Ethics Guidelines
A retrospective analysis of the clinical data was performed in accordance with the principles of the Declaration of Helsinki. This study has been reviewed by the Ethics Committee of Xi'an People's Hospital (Xi’an Fourth Hospital). Considering the retrospective nature of this study, the need for informed consent was waived.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Xue, YQ., Xiao, JA. & Chen, Y. Frequency and Treatment Regimens of Macular Edema in 1946 Consecutive Patients with Noninfectious Uveitis at a Tertiary Ophthalmic Center in Shaanxi, China. Ophthalmol Ther 12, 2609–2619 (2023). https://doi.org/10.1007/s40123-023-00763-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00763-4