Abstract
Introduction
Here we investigate the clinical features of foveal detachment (FD), full-thickness macular hole (MH), and macular hole retinal detachment (MHRD) in myopic traction maculopathy (MTM).
Methods
In the retrospective observational case series, 314 eyes of 198 patients with myopic retinoschisis in Beijing Tongren Hospital were enrolled. We recorded gender, age, and axial length and evaluated fundus characteristics using optical coherence tomography. Epiretinal membranes (ERMs), vitreoretinal traction, and paravascular abnormalities (PVAs) were used to describe the vitreoretinal interface condition. Different retinoschisis layers (inner, middle, and outer retinoschisis) and the location with a range of outer retinoschisis were evaluated to reveal the retinal condition. Five patterns of the scleral shape: dome-shaped, sloped toward the optic nerve, symmetrical or asymmetrical around the fovea, and irregular were assessed to show retina-sclera condition. We regarded the FD, full-thickness MH, and MHRD as the advanced stage in MTM. Multivariate logistic regression assessed significant factors for the advanced stage with odds ratios (OR) and 95% confidence intervals (CI).
Results
There were 76 eyes with FD, 6 eyes with full-thickness MH, and 7 eyes with MHRD. The mean age was 52.9 ± 12.3 years. On univariate analysis, the eyes with the advanced stage were older and had higher rates of ERMs, PVAs, middle retinoschisis, outer retinoschisis, and irregular sclera shape. The number of retinoschisis layers and the grade of outer retinoschisis were higher in eyes with the advanced stage. After multivariate logistic regression, ERMs (OR 1.983; 95% CI 1.093–3.595; P = 0.024), middle retinoschisis (OR 2.967; 95% CI 1.630–5.401; P < 0.001), and higher grades of outer retinoschisis (OR 2.227; 95% CI 1.711–2.898; P < 0.001) remained associated with the advanced stage.
Conclusion
ERMs, middle retinoschisis, and more extensive outer retinoschisis were significant characteristics of the advanced stage in MTM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
With a sharp increase in the prevalence of high myopia, people are meeting more challenges in myopic traction maculopathy (MTM). |
The advanced stage of MTM, including foveal detachment, full-thickness macular hole, and macular hole retinal detachment, could cause irreversible visual impairment. It is significant for clinical management to identify associated characteristics of the stage. |
What was learned from the study? |
Epiretinal membranes, middle retinoschisis, and higher grades of outer retinoschisis were significant characteristics of the advanced stage in MTM. |
Based on the results, we suggest the non-advanced, pre-advanced, and advanced stages for MTM. We hope the study can provide evidence for clinical management and further investigation in MTM. |
Introduction
With a sharp increase in the prevalence of high myopia, people are meeting more challenges in myopic maculopathy, especially in East Asians. It was estimated 938 million people with high myopia globally by 2050 [1]. In a meta-analysis, the pooled prevalence of myopic macular degeneration worldwide was 2.1% and 47.4% in people with high myopia [2]. Myopic macular degeneration mainly includes myopic atrophy maculopathy, myopic traction maculopathy (MTM), and myopic neovascular maculopathy [3]. In 2004, Panozzo et al. first proposed MTM through optical coherence tomography (OCT), including myopic retinoschisis (MR), retinal detachment, and macular hole (MH) [4]. Some studies showed that 9–34% of highly myopic patients with posterior staphyloma had retinoschisis as a common complication [5,6,7]. In China, MR has become the most frequent myopic maculopathy in OCT [8]. In the long-term observation, the state of MTM has uncertainty. As an early stage of MTM, MR could be asymptomatic, be stable for a long time, and even have a spontaneous resolution. However, some cases may progress rapidly with noticeable vision decline in a short period [9,10,11,12]. It is critical to identify the relevant characteristics for the advanced stage.
The fundus lesions of MTM are complex and involve multiple fundus structures. Previous studies showed that both vitreoretinal interface abnormalities and retina-scleral features, such as epiretinal membranes (ERMs), paravascular abnormalities (PVAs), and the shape of the sclera, might affect the disease progression [13,14,15,16,17]. The retinoschisis condition has different evaluation systems. Shimada et al. classified MR on the basis of the location and range of outer retinoschisis [9]. Some people describe MR condition according to the schisis in different retinal layers [13, 18]. The layers, location, and range of retinoschisis are essential features of the retina itself and, to some extent, reflect the severity of lesions.
The severity of the disease and clinical management are different according to clinical manifestations. Visual acuity may not be affected if MTM only behaves as macular schisis. When MTM is combined with FD or MH, significant vision loss always occurs. At that time, surgical intervention is required [19, 20]. Given the tractional component in the ATN classification [3], we regard FD, full-thickness MH, and macular hole retinal detachment (MHRD) as the advanced stage, which represents a more severe stage in MTM, and try to analyze associated characteristics of the advanced stage from the vitreoretinal interface condition, retinoschisis condition, and retina-sclera condition in the study.
Methods
Patients Enrolled and Ocular Examination
In the retrospective observational case series study, we reviewed highly myopic patients with an axial length (AXL) ≥ 26 mm or a spherical equivalent refractive error ≤ −6 diopters or posterior staphyloma in Beijing Tongren Hospital from October 2018 to December 2020 [3]. The eyes with retinoschisis were enrolled for further analysis. In the study, we excluded patients with the following criteria: vitreoretinal surgery history; combined with other ocular diseases involving fundus lesions, including age-related macular degeneration, diabetic retinopathy, retinal vein occlusion, glaucoma, uveitis, and so on; patients without available fundus images or OCT results, such as the opacity of refractive media, poor quality, and image dropout. The study adhered to the Declaration of Helsinki and was approved by the Ethics Committee of Beijing Tongren Hospital (TRECKY2021-018). In the retrospective study, patients’ data were unidentifiable, and thus informed consent was not required.
The patients underwent regular ophthalmologic examinations, including slit-lamp biomicroscopy, fundoscopy, intraocular pressure, refraction with an assessment of best-corrected visual acuity (BCVA), A-mode ultrasonography to measure an AXL, and fundus photography. We used two types of OCT (Heidelberg Inc., Germany, or Optovue, Inc., Fremont, CA, USA) to obtain vertical and horizontal B-scans through the fovea in a rectangular area, or radial B-scans centered on the fovea to show the macular characteristics.
Images Analysis
For OCT images, we analyzed the fundus condition from three aspects, vitreoretinal interface condition, retinoschisis condition, and retina-sclera condition. In the vitreoretinal interface assessment, we recorded the presence of ERMs, vitreoretinal traction (VT), and PVAs. PVAs were divided into paravascular microfolds, paravascular retinal cysts, and paravascular lamellar holes [21,22,23].
In the description of the retinoschisis condition, we defined three layers of retinoschisis: inner retinoschisis (schisis in retinal nerve fiber layer and/or retinal ganglion cells), middle retinoschisis (schisis in inner plexiform layer and/or inner nuclear layer), and outer retinoschisis (schisis in the outer plexiform layer and/or outer nuclear layer), and recorded numbers of retinoschisis layers (Fig. 1) [13]. In addition, we followed the grade proposed by Shimada et al. to assess the severity of the outer retinoschisis: S0, no macular retinoschisis; S1, extra-foveal; S2, fovea-only; S3, foveal but not entire macular area; and S4, entire macular area [9]. If there was no outer retinoschisis, but the inner retinoschisis and/or middle retinoschisis existed, we classified it into S0.
The optical coherence tomography image of a highly myopic eye with different retinoschisis layers. ➤ inner retinoschisis (schisis in retinal nerve fiber layer and/or retinal ganglion cells).  middle retinoschisis (schisis in inner plexiform layer and/or inner nuclear layer). ★ outer retinoschisis (schisis in the outer plexiform layer and/or outer nuclear layer)
middle retinoschisis (schisis in inner plexiform layer and/or inner nuclear layer). ★ outer retinoschisis (schisis in the outer plexiform layer and/or outer nuclear layer)
In assessing the retina-sclera condition, we referred to the previous study to describe the sclera shape in the macula [17]. The inner scleral surface shape was divided into five patterns: pattern 1: dome-shaped macula (DSM), pattern 2: sloped toward the optic nerve; pattern 3: symmetrical around the fovea; pattern 4: asymmetrical around the fovea; pattern 5: irregular [17, 24].
According to the tractional component in the ATN classification, we regarded FD, full-thickness MH, and MHRD as the advanced stage in MTM [3]. All the images were analyzed by a trained investigator (JX.T.) two times and regularly supervised by a panel of experienced ophthalmologists (CX.L., Y.Q.). For results with disagreement in the two analyses, the panel of experienced ophthalmologists was consulted to make a final decision.
Statistical Analyses
The advanced group was defined as MR eyes with FD, full-thickness MH, and MHRD. The control group was defined as the eyes without FD, full-thickness MH, and MHRD. The differences in clinical characteristics between the two groups were analyzed. Mean values (standard deviation) and count (frequencies) were used to describe continuous and categorical data. An independent-sample t-test with homogeneity of variances and a Mann–Whitney U test separately analyzed continuous variables with normal and abnormal distributions. Categorical data were assessed with the chi-square test, continuous correction chi-square test, Fisher’s exact test, Cramer’s V coefficient, and post hoc testing. Spearman’s rank correlation was performed to test the relationship between two variables when at least one was a rank variable. Bonferroni corrections were used to adjust an alpha value of 0.05. After univariate analysis, multivariate logistic regression was performed to assess significant factors for the advanced stage with odds ratios (OR) and 95% confidence intervals (CI). All two-sided P values < 0.05 were considered statistically significant. Commercial software (SPSS version 24.0; SPSS, Inc., Chicago, IL, USA) was used for all statistical analyses.
Results
From October 2018 to December 2020, 314 eyes of 198 patients with MR met the criteria and enrolled in this study. The mean age was 52.9 ± 12.3 years, ranging from 17 to 79. Clinical characteristics of the eyes are summarized in Table 1. For the advanced stage, 76, 6, and 7 eyes were with FD, full-thickness MH, and MHRD, respectively. The grade of the outer retinoschisis was positively associated with the number of retinoschisis layers (r = 0.469, P < 0.001). The grade of the outer retinoschisis and the number of retinoschisis layers were not associated with AXL (r = −0.018, P = 0.173; r = −0.022, P = 0.709). The advanced group had older age and worse BCVA than the control group (P = 0.018; P < 0.001). The mean AXL was still not significantly different between the two groups (P = 0.467; Table 2).
The Association in Vitreoretinal Interface Condition with the Advanced Stage
The results show that the advanced group had more ERMs than the control group (P = 0.038). More PVAs were found in the advanced group, mainly composed of paravascular cysts (P = 0.039; P = 0.018). The difference in VT between the two groups was insignificant (P = 0.151; Table 2).
The Association in Retinoschisis Condition with the Advanced Stage
The middle and outer retinoschisis rates were higher in the advanced group than in the control group (all P < 0.001). The number of retinoschisis layers and the grade of the outer retinoschisis were both associated with the advanced stage (Cramer’s V coefficient = 0.365, P < 0.001; Cramer’s V coefficient = 0.508, P < 0.001). The retinoschisis involving the entire macular area was most frequent, followed by the fovea but not the entire macula. There was no significant difference in the occurrence of inner retinoschisis between the reference and the advanced group (P = 0.257; Table 2).
The Association in Retina-Sclera Condition with the Advanced Stage
For the shape of the inner scleral surface, the irregular type was the most frequent pattern in both groups, followed by the asymmetrical curvature around the fovea (Table 2). Therefore, we further divided the retina-sclera characteristics into two categories: irregularity and non-irregularity. The result showed that the irregular type was more common in the advanced group than in the control group (57.3% versus 43.6%, P = 0.028). The assessment with five sclera types showed no significant difference between the two groups (P = 0.083).In addition, the rate of DSM in the advanced group was similar to that in the control group (12.4% versus 12.0%, P = 0.930).
Clinical Factors Associated with the Advanced Stage
Based on the above, age, ERMs, paravascular cysts, the middle retinoschisis, the outer retinoschisis, the number of retinoschisis layers, grades of the outer retinoschisis, and the irregular sclera shape were significant factors for the advanced stage. Among these factors, the outer retinoschisis and the grades of the outer retinoschisis were non-independent variables. The grade of outer retinoschisis covers the evaluation of whether outer retinoschisis exists. Therefore, we did not incorporate “the outer retinoschisis” in the multiple-factor analysis. The grade of outer retinoschisis was also correlated with the number of retinoschisis layers. In the analysis of the association in retinoschisis characteristics with the advanced stage, grades of outer retinoschisis showed a higher Cramer’s V coefficient than the number of retinoschisis layers. Besides, middle retinoschisis and the grades of outer retinoschisis, as two independent factors, could indirectly reflect the number of retinoschisis layers. Therefore, we ruled out the number of retinoschisis layers as a covariant. Finally, we enrolled age, ERMs, paravascular cysts, the middle retinoschisis, the grades of the outer retinoschisis, and the irregular sclera shape as independent variables to construct the multivariate logistic regression model. The results showed ERMs (OR 1.983; 95% CI 1.093–3.595; P = 0.024), the middle retinoschisis (OR 2.967; 95% CI 1.630–5.401; P < 0.001), and higher grades of outer retinoschisis (OR 2.227; 95% CI 1.711–2.898; P < 0.001) were significant factors for the advanced stage (Table 3).
Discussion
The risk factors for MTM have been of great concern for a long time [7]. Some cases could have good visual acuity and be stable. However, some cases may progress rapidly to FD or MH. The management and prognosis also change accordingly. Here, we regarded FD, full-thickness MH, and MHRD as the advanced stage and aimed to identify the associated characteristics. The results showed that ERMs, middle retinoschisis, and higher grades of outer retinoschisis were significant features of the stage. According to the evaluation of the outer retinoschisis, higher grades of outer retinoschisis imply more extensive outer retinoschisis [9].
The relationship between age and MTM has been discussed in many studies. In some research, MTM was regarded as a degenerative ocular disease and analyzed patients aged 40 or over [13, 25,26,27]. Older patients could be more inclined to have MTM, and the severity of MTM increases with aging [26, 28]. However, in the study performed by Matsumura et al., age was not associated with MTM in people aged 40 or over [27]. In some studies, age could be associated with MTM on univariate analysis but not multivariate analysis [13, 29]. Here, we also found that the advanced group was older than the control group. However, it was unrelated to the severe stage after adjusting for other factors. Aging might be associated with multi-factors, such as ERMs, the shape of the sclera, and the degree of outer retinoschisis. After correcting those elements, aging was not an independent risk factor for the advanced stage.
The association in AXL with MTM was also worth further exploration. Some studies have testified that a longer AXL was a risk factor for MTM [8, 26, 27]. Other studies showed that eyes with MR had a significantly shorter AXL than highly myopic eyes without MR [13, 16]. Here, we found that AXL was not associated with the advanced stage, which was indirectly consistent with the result showing AXL was not related to the grade of the tractional component in the ATN classification [28]. As we all know, axial elongation is one of the leading causes of myopic maculopathy. However, the accuracy of the AXL measurement is a great challenge due to posterior staphyloma or irregular globe contour. The posterior staphyloma height or the shape of the scleral wall also may have a more prominent effect on MTM development than axial elongation [17, 30, 31].
Biomechanics was the primary pathogenesis of MTM. Parolini et al. had a detailed analysis and summarized a new staging system for tangential and perpendicular evolution [31]. They also proposed corresponding management based on the classification, such as performing macular buckling for macular detachment or vitrectomy for MHRD [19]. In our study, we tried to identify more clinical characteristics of the advanced stage and assist the pre-advanced stage recognition in MTM. According to the anatomical features, we summarized the fundus characteristics into three layers: the vitreoretinal condition, the retinal condition, and the retina-sclera condition.
ERMs, VT, and PVAs were assessed to describe the condition of the vitreoretinal interface. Many studies have demonstrated that epiretinal traction was a crucial factor for MTM [27, 31, 32]. Higher rates of ERMs, VT, and PVAs were observed in highly myopic eyes with retinoschisis [22, 29, 32,33,34,35,36]. VT on retinal vessels might be a more significant factor than on the fovea, which could induce PVAs [13, 22, 32]. In MTM, paravascular cyst was the most frequent type, followed by paravascular microfolds and paravascular lamellar holes, which was in accord with the previous investigation [22]. On univariate analysis, PVAs, mainly paravascular cysts, were associated with the advanced stage. (Fig. 2). However, the relationship also was insignificant on multivariate analysis. The spatial distance from the paramacular to the foveal area might limit the impact of paravascular traction in disease progression. By contrast, ERMs had a remarkable correlation with the advanced stage. Compared with VT and PVAs, ERMs might provide more vital traction on the macular lesion. In addition, the VT could be less visible on OCT [31].
The optical coherence tomography image of a 63-year-old woman with epiretinal membranes (☆), paravascular abnormalities (△), three layers of retinoschisis (➤ inner retinoschisis;  middle retinoschisis; ★ outer retinoschisis), and macular hole (▼). The axial length was 29.62 mm. The outer retinoschisis involved the entire macular area. The sclera shape is asymmetrical around the fovea
middle retinoschisis; ★ outer retinoschisis), and macular hole (▼). The axial length was 29.62 mm. The outer retinoschisis involved the entire macular area. The sclera shape is asymmetrical around the fovea
Some studies on the retinal condition demonstrated that more extensive outer retinoschisis was a significant risk factor for FD [9, 37]. Fujimoto et al. found that multi-layer retinoschisis was associated with FD development [18]. Our results showed that both factors were associated with the advanced stage (Fig. 3). Besides, the middle schisis in the inner plexiform and inner nuclear layers was a critical predictor for the stage. The outer retinoschisis might be more susceptible to posterior-directed traction, such as axial elongation. The inner retinoschisis could more easily result from vitreous traction. No traction acts on the middle layers directly. Therefore, we believe the middle retinoschisis indicates potent traction on the retina. Some studies showed that inner retinoschisis was associated with the disease progression [18, 38, 39]. The relationship between the number of retinoschisis layers and the advanced stage indirectly supported the opinion. However, we did not find a direct correlation between inner retinoschisis and the advanced stage. The inner retina might be susceptible to the vitreous state. When FD and MH develop, the vitreous body is prone to liquefy and further alleviate the traction on the inner retinoschisis layer. Some studies showed that ellipsoid zone disruption or the out lamellar MH was a significant factor for the advanced stage [20, 40, 41]. In our study, all the MR eyes with outer lamellar MH presented various degrees of FD, consistent with the perspective.
The posterior sclera’s morphology and material properties have changed as AXL grows. In the study by Ohno-Matsui et al., the macular sclera shape was divided into five patterns, and the MR eyes were more likely to present an irregular sclera shape [30]. Here, the rate of irregular sclera shape in the advanced group was also higher than in the control group (Fig. 4). However, the relationship was insignificant on multivariate analysis. We inferred that the scleral shape was more of an accompanying sign of aging, axial elongation, and disease evolution rather than an independent risk factor for the advanced stage. As an inward macular elevation, DSM might alleviate the posterior-directed force by decreasing AXL [42]. Some studies showed that DSM was a protective factor for foveoschisis but a risk factor for extrafoveal retinoschisis [43, 44]. Other studies proved that DSM was a risk factor for retinal detachment in high myopia, especially for those with a macular bulge height of over 350 μm, that may destroy the original choroidal blood flow blood–retinal barrier and cause serous retinal detachment [45, 46]. Here, we believe that the effect of DSM manifests mainly in AXL. As we did not find a significant difference in AXL between the two groups, we also did not find a correlation between DSM and the advanced stage, which was in line with the study by Li et al. [28].
Based on the results and previous studies, we had some suggestions for clinical management aiming at the risk factor for the advanced stage (Table 4) [19, 47,48,49]. The outer retinoschisis was a critical factor for the advanced stage. We suggested regarding the inner and middle retinoschisis but without outer schisis as grade 1. In the study, eyes with inner and middle schisis but without outer schisis were rare, and they did not show the advanced stage. Therefore, we did not emphasize the significance of middle retinoschisis in grade 1. On that basis, we further analyzed the rate of the advanced stage between groups with different grades of outer retinoschisis. The results showed that S4 was significantly more likely to combine with the advanced stage than the other grades (P < 0.001; P < 0.001; P < 0.001; P < 0.001). According to that, we suggested that S1 to S3, which means partial outer retinoschisis, were regarded as grade 2. Both grade 1 and grade 2 belong to the non-advanced stage, which was relatively stable for FD and MH. In this stage, posterior sclera reinforcement is recommended [49] Patients who refuse posterior sclera reinforcement should have regular follow-ups. The entire macular outer retinoschisis was classified as grade 3 and pre-advanced stage. In this stage, we suggested regarding middle retinoschisis and ERMs as plus lesions to underline the associated characteristics of the advanced stage. The pre-advanced stage has significant risk factors for FD and MH. Therefore, we advise performing posterior sclera reinforcement. If patients have eyes that lose two or more lines of BCVA in 3 months, we suggest vitreoretinal surgery or macular buckling. MTM eyes with FD, full-thickness MH, and MHRD are regarded as grade 4, grade 5, and grade 6, respectively. The three grades are classified into the advanced stage. In this stage, vitreoretinal surgery or macular buckling is necessary. Besides, posterior scleral reinforcement is recommended for patients undergoing vitrectomy to improve postoperative visual acuity and prevent disease progression [47].
The limitations of the study need to be noted. Firstly, as a cross-sectional study, the result of the study still needs verification in longitudinal observation. Second, we summed up FD, full-thickness MH, and MHRD in the advanced stage. The lamellar MH, which also influenced MTM, was not investigated. To facilitate the clinical application of the results, we preliminarily selected qualitative variables to evaluate the fundus condition. In the follow-up studies, the description of the fundus characteristics could be quantitative and more detailed to investigate the mechanism of MTM, for example, measuring the state of posterior vitreous detachment, retinal thickness, posterior staphyloma height, and so on. The study was performed on the basis of the hospital to enlarge the sample size and perhaps had a selective bias. Some patients with MR with good visual acuity may not be enrolled. A population study can provide more solid evidence for the conclusion.
Conclusions
Above all, our study preliminarily demonstrated that ERMs, schisis in the inner plexiform layer and/or inner nuclear layer, and more extensive outer retinoschisis were significant characteristics associated with the advanced stage in MTM. The impact of other factors, such as aging, VT, and the shape of the posterior sclera, could be investigated. Despite the shortcomings, we hope this study could provide suggestions for clinical management and further investigation for MTM.
References
Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–42.
Zou M, Wang S, Chen A, et al. Prevalence of myopic macular degeneration worldwide: a systematic review and meta-analysis. Br J Ophthalmol. 2020;104(12):1748–54.
Ruiz-Medrano J, Montero JA, Flores-Moreno I, Arias L, García-Layana A, Ruiz-Moreno JM. Myopic maculopathy: current status and proposal for a new classification and grading system (ATN). Prog Retin Eye Res. 2019;69:80–115.
Panozzo G. Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol. 2004;122(10):1455–60.
Takano M, Kishi S. Foveal retinoschisis and retinal detachment in severely myopic eyes with posterior staphyloma. Am J Ophthalmol. 1999;128(4):472–6.
Baba T, Ohno-Matsui K, Futagami S, et al. Prevalence and characteristics of foveal retinal detachment without macular hole in high myopia. Am J Ophthalmol. 2003;135(3):338–42.
Benhamou N, Massin P, Haouchine B, Erginay A, Gaudric A. Macular retinoschisis in highly myopic eyes. Am J Ophthalmol. 2002;133(6):794–800.
You QS, Peng XY, Xu L, Chen CX, Wang YX, Jonas JB. Myopic maculopathy imaged by optical coherence tomography: the Beijing Eye Study. Ophthalmology. 2014;121(1):220–4.
Shimada N, Tanaka Y, Tokoro T, Ohno-Matsui K. Natural course of myopic traction maculopathy and factors associated with progression or resolution. Am J Ophthalmol. 2013;156(5):948–57.
Shimada N, Ohno-Matsui K, Baba T, Futagami S, Tokoro T, Mochizuki M. Natural course of macular retinoschisis in highly myopic eyes without macular hole or retinal detachment. Am J Ophthalmol. 2006;142(3):497–500.
Gaucher D, Haouchine B, Tadayoni R, et al. Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol. 2007;143(3):455–62.
Li S, Li T, Wang X, et al. Natural course of myopic traction maculopathy and factors influencing progression and visual acuity. BMC Ophthalmol. 2021;21(1):347.
Takahashi H, Tanaka N, Shinohara K, et al. Importance of paravascular vitreal adhesions for development of myopic macular retinoschisis detected by ultra-widefield OCT. Ophthalmology. 2021;128(2):256–65.
Ikuno Y, Gomi F, Tano Y. Potent retinal arteriolar traction as a possible cause of myopic foveoschisis. Am J Ophthalmol. 2005;139(3):462–7.
VanderBeek BL, Johnson MW. The diversity of traction mechanisms in myopic traction maculopathy. Am J Ophthalmol. 2012;153(1):93–102.
Shinohara K, Tanaka N, Jonas JB, et al. Ultrawide-field OCT to investigate relationships between myopic macular retinoschisis and posterior staphyloma. Ophthalmology. 2018;125(10):1575–86.
Ohno-Matsui K, Akiba M, Modegi T, et al. Association between shape of sclera and myopic retinochoroidal lesions in patients with pathologic myopia. Invest Ophthalmol Vis Sci. 2012;53(10):6046–61.
Fujimoto M, Hangai M, Suda K, Yoshimura N. Features associated with foveal retinal detachment in myopic macular retinoschisis. Am J Ophthalmol. 2010;150(6):863–70.
Parolini B, Palmieri M, Finzi A, Frisina R. Proposal for the management of myopic traction maculopathy based on the new MTM staging system. Eur J Ophthalmol. 2021;31(6):3265–76.
Shimada N, Ohno-Matsui K, Yoshida T, Sugamoto Y, Tokoro T, Mochizuki M. Progression from macular retinoschisis to retinal detachment in highly myopic eyes is associated with outer lamellar hole formation. Br J Ophthalmol. 2008;92(6):762–4.
Sayanagi K, Ikuno Y, Gomi F, Tano Y. Retinal vascular microfolds in highly myopic eyes. Am J Ophthalmol. 2005;139(4):658–63.
Shimada N, Ohno-Matsui K, Nishimuta A, et al. Detection of paravascular lamellar holes and other paravascular abnormalities by optical coherence tomography in eyes with high myopia. Ophthalmology. 2008;115(4):708–17.
Ohno-Matsui K, Hayashi K, Tokoro T, Mochizuki M. Detection of paravascular retinal cysts before using OCT in a highly myopic patient. Graefes Arch Clin Exp Ophthalmol. 2006;244(5):642–4.
Gaucher D, Erginay A, Lecleire-Collet A, et al. Dome-shaped macula in eyes with myopic posterior staphyloma. Am J Ophthalmol. 2008;145(5):909–14.
Yan Y, Wang Y, Yang Y, et al. Ten-year progression of myopic maculopathy: the Beijing eye study 2001–2011. Ophthalmology. 2018;125(8):1253–63.
Chen Q, He J, Hu G, Xu X, Xu X. Morphological characteristics and risk factors of myopic maculopathy in an older high myopia population—based on the new classification system (ATN). Am J Ophthalmol. 2019;208:356–66.
Matsumura S, Sabanayagam C, Wong CW, et al. Characteristics of myopic traction maculopathy in myopic Singaporean adults. Br J Ophthalmol. 2021;105(4):531–7.
Li J, Liu B, Li Y, et al. Clinical characteristics of eyes with different grades of myopic traction maculopathy: based on the new classification system. Retina. 2021;41(7):1496–501.
Wu PC, Chen YJ, Chen YH, et al. Factors associated with foveoschisis and foveal detachment without macular hole in high myopia. Eye (Lond). 2009;23(2):356–61.
Park U, Ma D, Ghim W, Yu H. Influence of the foveal curvature on myopic macular complications. Sci Rep. 2019;9(1):16936.
Parolini B, Palmieri M, Finzi A, et al. The new myopic traction maculopathy staging system. Eur J Ophthalmol. 2021;31(3):1299–312.
Ripandelli G, Rossi T, Scarinci F, Scassa C, Parisi V, Stirpe M. Macular vitreoretinal interface abnormalities in highly myopic eyes with posterior staphyloma: 5-year follow-up. Retina. 2012;32(8):1531–8.
Li T, Wang X, Zhou Y, et al. Paravascular abnormalities observed by spectral domain optical coherence tomography are risk factors for retinoschisis in eyes with high myopia. Acta Ophthalmol. 2018;96(4):515–23.
Vela JI, Sánchez F, Díaz-Cascajosa J, Mingorance E, Andreu D, Buil JA. Incidence and distribution of paravascular lamellar holes and their relationship with macular retinoschisis in highly myopic eyes using spectral-domain OCT. Int Ophthalmol. 2016;36(2):247–52.
Kamal-Salah R, Morillo-Sanchez MJ, Rius-Diaz F, Garcia-Campos JM. Relationship between paravascular abnormalities and foveoschisis in highly myopic patients. Eye (Lond). 2015;29(2):280–5.
Song M, Shen M, Zhou Y, et al. Observation of vitreous features using enhanced vitreous imaging optical coherence tomography in highly myopic retinoschisis. Retina. 2019;39(9):1732–41.
Cheng C, Teo K, Tan CS, et al. Myopic retinoschisis in Asians: structural features and determinants of visual acuity and prognostic factors for progression. Retina. 2016;36(4):717–26.
Sayanagi K, Ikuno Y, Tano Y. Tractional internal limiting membrane detachment in highly myopic eyes. Am J Ophthalmol. 2006;142(5):850–2.
Fang D, Su J, Chen L, Zhang S. The role of internal limiting membrane as a biomarker in the evolution of myopic traction maculopathy. Front Med (Lausanne). 2021;8:802626.
Sun CB, Liu Z, Xue AQ, Yao K. Natural evolution from macular retinoschisis to full-thickness macular hole in highly myopic eyes. Eye (Lond). 2010;24(12):1787–91.
Hsia Y, Ho TC, Yang CH, Hsieh YT, Lai TT, Yang CM. Clinical characteristics and long-term evolution of lamellar macular hole in high myopia. PLoS One. 2020;15(5):e0232852.
Wang SW, Hung KC, Tsai CY, Chen MS, Ho TC. Myopic traction maculopathy biomarkers on optical coherence tomography angiography—an overlooked mechanism of visual acuity correction in myopic eyes. Eye (Lond). 2019;33(8):1305–13.
Fang D, Zhang Z, Wei Y, et al. The morphological relationship between dome-shaped macula and myopic retinoschisis: a cross-sectional study of 409 highly myopic eyes. Invest Ophthalmol Vis Sci. 2020;61(3):19.
García-Ben A, Blanco MJ, Piñeiro A, Mera P, Rodriguez-Alvarez MX, Capeans C. Relationship between macular bending and foveoschisis in myopic patients. Optom Vis Sci. 2014;91(5):497–506.
Hocaoglu M, Ersoz MG, Sayman Muslubas I, Arf S, Karacorlu M. Factors associated with macular complications in highly myopic eyes with dome-shaped macular configuration. Graef Arch Clin Exp Ophthalmol. 2019;257(11):2357–65.
Liang IC, Shimada N, Tanaka Y, et al. Comparison of clinical features in highly myopic eyes with and without a dome-shaped macula. Ophthalmology. 2015;122(8):1591–600.
Qi Y, Duan AL, You QS, Jonas JB, Wang N. Posterior scleral reinforcement and vitrectomy for myopic foveoschisis in extreme myopia. Retina. 2015;35(2):351–7.
Fujimoto S, Ikuno Y, Nishida K. Postoperative optical coherence tomographic appearance and relation to visual acuity after vitrectomy for myopic foveoschisis. Am J Ophthalmol. 2013;156(5):968–73.
Chen CA, Lin PY, Wu PC. Treatment effect of posterior scleral reinforcement on controlling myopia progression: a systematic review and meta-analysis. PLoS One. 2020;15(5):e0233564.
Acknowledgements
The authors thank Beijing Tongren Hospital, Capital Medical University for help and support. The authors would also like to thank the participants of the study.
Funding
This work was supported by Beihang University-CMU, Advanced Innovation Center for Big Data-Based Precision Medicine. No funding or sponsorship was received for publication of this article.
Author Contributions
Jiaxin Tian, Yue Qi, and Ningli Wang: study concept and design and manuscript revision. Jiaxin Tian, Caixia Lin, and Yue Qi: performed study. Jiaxin Tian: drafted the manuscript. Yuxin Fang, Anli Duan, Yue Qi, Ningli Wang: revised the manuscript. Jiaxin Tian, Yuxin Fang, and Kai Cao: statistical analysis. Ningli Wang: administrative, technical, material support, or study supervision. All authors participated in and provided help for the study.
Disclosures
Jiaxin Tian, Caixia Lin, Yuxin Fang, Kai Cao, Anli Duan, Yue Qi, Ningli Wang declare no conflict of interest.
Compliance with Ethics Guidelines
The study adhered to the tenets of the declaration of Helsinki and was approved by the Ethics Committee of Beijing Tongren Hospital (TRECKY2021-018). In the retrospective study, patients’ data were unidentifiable; thus, informed consent was not required.
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tian, J., Lin, C., Fang, Y. et al. Multimodal Analysis on Clinical Characteristics of the Advanced Stage in Myopic Traction Maculopathy. Ophthalmol Ther 12, 2569–2581 (2023). https://doi.org/10.1007/s40123-023-00745-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00745-6




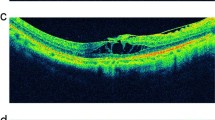



 ) and outer retinoschisis (★). The axial length was 27.86 mm. The outer retinoschisis involved the entire macular area. The sclera shape is asymmetrical around the fovea
) and outer retinoschisis (★). The axial length was 27.86 mm. The outer retinoschisis involved the entire macular area. The sclera shape is asymmetrical around the fovea