Abstract
Introduction
To evaluate real-world efficacy, safety, and treatment patterns with the dexamethasone intravitreal implant (DEX) in diabetic macular edema (DME) in France.
Methods
In this prospective, multicenter, observational, noncomparative, post-reimbursement study, consecutively enrolled patients with DME had a baseline evaluation on day 0. Those treated with DEX on day 0 were to be reevaluated at week 6 and months 6, 12, 18, and 24. DEX retreatment and/or alternative therapies were allowed during follow-up. The primary outcome measure was the maximum best corrected visual acuity (BCVA) gain from baseline during follow-up. Secondary outcome measures included time to maximum BCVA gain, patients (%) with prespecified BCVA gains from baseline at each visit, maximum central retinal thickness (CRT) reduction from baseline, patients (%) with CRT reduction ≥ 20% from baseline at each visit, patients (%) with DME resolution (per investigator judgement), and adverse events (AEs).
Results
Of 112 patients/eyes with DME for 3.5 years (mean) at baseline, 80 (including 86.1% previously treated) received DEX on day 0 and were analyzed for efficacy. Early study termination precluded collection of ≥ 12-month efficacy data. Patients received 1.4 DEX injections over 8.3 months (averages). The maximum BCVA gain from baseline was 3.6 letters, reached after 77.2 days (averages); 24.6% (week 6) and 15.0% (month 6) of patients experienced ≥ 10-letter BCVA gains from baseline. The mean maximum CRT reduction from baseline was −146.4 µm; 61.4% (week 6) and 36.0% (month 6) of patients had CRT reductions ≥ 20% from baseline, and 68.1% reported DME resolution at least once during follow-up. Ocular hypertension (n = 8, 12.1%) was the most frequent treatment-related AE.
Conclusions
LOUVRE 3 confirmed that DEX improves BCVA and CRT, even in a patient population that had predominantly received DEX before enrollment in the study, and showed that DME resolution was observed during follow-up. DEX tolerability was consistent with published data, supporting treatment benefits in DME.
ClinicalTrials.gov Identifier
NCT03003416.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.


Why carry out this study? |
Diabetic macular edema (DME) is a main cause of vision loss in diabetic patients. |
Although anti-vascular endothelial growth factor (anti-VEGF) therapies have become the standard of care for DME, not all affected individuals respond optimally to anti-VEGF therapy. |
The LOUVRE 3 study evaluated real-world efficacy, safety, and treatment patterns with the dexamethasone intravitreal implant (DEX) in DME in France. |
What was learned from the study? |
LOUVRE 3 confirmed that DEX improves best corrected visual acuity and central retinal thickness, even in a population consisting mostly of patients who had received DEX before enrollment in the study, and showed that DME resolution was observed over the 8.3-month follow-up period. |
Despite a shorter follow-up than anticipated, the study results show that positive outcomes are still achievable with DEX in the aforementioned population. |
Digital Features
This article is published with digital features, i.e. an infographic feature to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.21922275.
Introduction
Diabetic retinopathy and diabetic macular edema (DME) are main causes of vision loss in diabetic patients [1,2,3]. An estimated 25% of individuals with long-standing type 1 or type 2 diabetes are affected [4], which is concerning as the number of adults (20–79 years of age) diagnosed with diabetes worldwide is expected to rise from approximately 537 million (2021) to 783 million by 2045 [5]. In France, over 5 million people are reportedly diabetic (92% of whom have type 2 diabetes [6]), and the estimated prevalence of DME (based on 2016 data) is 3% of the diabetic population (i.e., > 100,000 individuals) [7].
The onset of DME has been strongly associated with inadequate control of blood glucose levels and blood pressure [8, 9]. Accordingly, DME management emphasizes the importance of controlling those parameters [10]. From a mechanistic standpoint, however, DME results from impairment of the blood–retinal barrier, which leads to fluid accumulation in the retina and release of proinflammatory and proangiogenic factors, including vascular endothelial growth factor (VEGF) [4, 11, 12]. Elucidation of this mechanism led to the development of intravitreal anti-VEGF therapies such as ranibizumab (Lucentis, Genentech Inc., South San Francisco, CA, USA) and aflibercept (Eylea, Regeneron Pharmaceuticals Inc., Tarrytown, NY, USA), which have become standard of care for DME in France, as they reduce retinal thickness and improve visual acuity [13,14,15,16,17,18,19].
Considering that not all individuals with DME respond optimally to anti-VEGF therapy [20], and that intravitreal corticosteroids have been shown to provide broader antiinflammatory effects, inhibiting synthesis of VEGFs as well as other proinflammatory mediators of DME [20, 21], the biodegradable intravitreal dexamethasone implant (DEX; Ozurdex 0.7 mg, Allergan, an AbbVie company, North Chicago, IL, USA) was developed as an alternative to available therapies. Releasing dexamethasone in the posterior segment for up to 6 months, DEX reduces the need for frequent injections and the potential complications associated with repeated intravitreal injections [22].
In Europe, DEX is approved for treatment of DME in patients who are pseudophakic or refractory to non-corticosteroid therapy, and for whom non-corticosteroid therapy is contraindicated. Following regulatory approval of DEX for DME, the French National Authority for Health (Haute Autorité de Santé) requested that an observational study (LOUVRE 3) be conducted to inform the following: clinical characteristics of patients at initiation of DEX treatment in clinical settings [e.g., hemoglobin A1c (HbA1c) levels and prior treatments]; frequency of DEX administration and follow-up visits; criteria determining reinjection versus treatment discontinuation; as well as the efficacy and tolerability up to 24 months in the overall population of DEX-treated patients and subgroups who were pseudophakic, refractory to non-corticosteroid therapy, or for whom non-corticosteroid therapy was contraindicated. Although the study was terminated prematurely due to a product recall [23] that also limited the number of patients with available data at ≥ 12 months, efficacy and safety findings up to 6 and 12 months, respectively, are presented herein for the overall enrolled population.
Methods
Study Design
This prospective, multicenter, observational, longitudinal, noncomparative, post-reimbursement study (ClinicalTrials.gov Identifier: NCT03003416) was conducted at injection centers located in metropolitan areas of France between 27 October 2017 and 19 December 2018. The centers were randomly selected from a comprehensive nationwide list of intravitreal injection centers, on the basis of a protocol-specified ratio of 80% public to 20% private sites and the average number of DME cases seen monthly in consultation at the sites.
Prior to study start, the protocol was approved by the Comité Consultatif sur le Traitement de l’Information en Matière de Recherche dans le Domaine de la Santé (CCTIRS), Commission Nationale de l’Informatique et Libertés (CNIL), and Conseil National de l’Ordre des Médecins (CNOM). The study was conducted in accordance with the ethical principles of the Declaration of Helsinki [24], French Public Health Code and French Act on Data Processing, Data Files, and Individual Liberties [25], Good Epidemiological Practices [26], and guidelines from the Haute Autorité de Santé on post-registration studies [27]. Written informed consent was obtained from all patients.
Study Population and Treatment
Consecutively presenting patients (≥ 18 years of age) with type I or type II diabetes and DME (treatment-naïve or previously treated with DEX and/or other agents) seen in consultation during the enrollment period were recruited. Patients who did not reside in metropolitan France and/or were concurrently participating in a non-observational study were excluded. There were no requirements in terms of best corrected visual acuity (BCVA) or central retinal thickness (CRT) at baseline, and no other eligibility criteria.
Enrolled patients had a baseline evaluation (including medical history and ocular examination) on day 0, after which decisions related to treatment selection, including the type and frequency of therapy, were made by the investigators on the basis of their clinical judgement. DEX was supplied by the clinic or practitioner.
Visits and Assessments
All enrolled patients attended the day-0 visit. For patients who received DEX treatment on day 0, visits were also planned at week 6 (± 1 month) and months 6 (± 2), 12 (± 3), 18 (± 3), and 24 (± 3). The timing of each visit followed that of typical French clinical practice, while scheduling flexibility was reflective of the real-world nature of the study. Additional visits, including those following retreatment with DEX or an alternative therapy, were scheduled as deemed necessary by the investigator and recorded. Patients not treated with DEX on day 0 were not followed prospectively and were not included in the efficacy analyses.
Patient demographics, baseline characteristics, and the reasons for treating or not treating with DEX on day 0 were collected on that day. BCVA (using a logMAR or Monoyer chart), intraocular pressure (IOP, assessed per standard practice), and CRT (evaluated by optical coherence tomography) were assessed bilaterally on day 0 in all enrolled patients, and at each follow-up visit in patients who received DEX on day 0. Information on retreatment (if performed) was also recorded for each study eye at each follow-up visit. Adverse events (AEs) were recorded on day 0 in all enrolled patients, and at all follow-up visits in patients who received DEX on day 0. Study discontinuations were recorded throughout the study.
Outcome Measures
The primary outcome measure was the mean maximum gain in BCVA (in Early Treatment Diabetic Retinopathy Study letters) from baseline during follow-up. Secondary outcome measures included the mean time to maximum BCVA gain from baseline; proportion of patients with ≥ 10- and ≥ 15-letter BCVA gains from baseline at each visit; maximum reduction in CRT from baseline during follow-up; proportion of patients with a ≥ 20% reduction in CRT from baseline at each visit; proportion of patients with DME resolution (defined as CRT < 300 µm or disappearance of DME per investigator judgment) during follow-up; characteristics of patients and DME treated with DEX on day 0 (compared with those of patients not treated with DEX on day 0); proportion of patients retreated during follow-up (along with the type of and reason for retreatment); mean number of injections; and mean treatment interval. Reports of AEs, their relationship to treatment, and severity were collected. Per protocol, the proportions of patients with IOP ≥ 25 mmHg and ≥ 35 mmHg despite IOP-lowering treatment were also reported.
All outcomes were reported on a per-patient basis, consistent with the objective of refining understanding of patients’ clinical characteristics at initiation of DEX treatment in this real-world, post-reimbursement study. In patients treated bilaterally, the eye with worse CRT at enrollment was considered the study eye; if the CRT values were equal in both eyes, the right eye was selected as study eye.
Statistical Analyses
Per the protocol, the primary and secondary efficacy outcome measures were to be analyzed in all patients treated with DEX on day 0 who had baseline data available and attended ≥ 1 follow-up visit, as well as subgroups of patients who were pseudophakic, refractory to non-corticosteroid therapy, or for whom non-corticosteroid therapy was contraindicated. However, as a result of the product recall, physicians were advised to consider alternative therapies (on the basis of potential risks and benefits) for their patients. As switches to other therapies were expected to bias the analyses, the study steering committee recommended that the analysis population should only include patients who completed at least 1 scheduled visit before 4 October 2018 (the recall date). One exception was AEs, which were analyzed in all patients treated with DEX on day 0, regardless of when they completed the scheduled visit(s). Subgroup analyses were performed for patients who, on enrollment in this study, were naïve of all treatments, DEX-naïve, and previously treated with DEX.
Statistical analyses were performed using SAS software version 9.3 or higher (SAS Institute, Inc., Cary, NC, USA), without imputation for missing values (unless otherwise noted). Quantitative variables were summarized by mean and standard deviation (SD), while qualitative variables were summarized by frequency and percentage. Comparative analyses were supported by 95% confidence intervals (CIs) when allowed by the sample size. Statistical significance of the mean change in BCVA from baseline was evaluated with Student’s t-test (if normal distribution was verified) or Wilcoxon signed-rank test for matched series.
The sample size was based on information from the prospective, randomized, sham-controlled, phase 3 MEAD study, which led to marketing authorization of DEX for DME in Europe and showed a statistically significant difference in BCVA between baseline and week 6 (period during which the greatest BCVA gain was observed). Using the sample size equation N = 1.962/i2 × SD2 with i = 1 (desired precision in terms of letter) and SD = 7.2, a minimal sample size of 199 patients was required to determine the greatest BCVA gain from baseline with an accuracy of 95%. Assuming that 30% of patients would not have data available at week 6, enrollment of 260 patients was planned.
Results
Patient Disposition, Demographics and Baseline Characteristics
In total, 112 patients were enrolled by 27 ophthalmologists at 14 injection centers (public, n = 10, 71.4%; private, n = 4, 28.6%) before the product recall date of 4 October 2018. Two additional patients were enrolled after the recall date and only included in the AE analysis. Of the 112 patients enrolled pre-recall, 32 (28.6%) did not receive DEX on day 0 (mostly because an alternative therapy was used instead), while 80 (71.4%) were treated with DEX that day and followed prospectively (Figs. 1, 2). Of those 80 patients, 62 (78.8%), 29 (36.3%), and 2 (2.5%) completed the week-6, month-6, and month-12 visits before 4 October 2018, respectively. All patients treated with DEX on day 0 discontinued the study before the month-18 visit, the main reason (n = 79, 98.8%) being early termination of the study (Fig. 1). Due to the low number (or lack) of patients whose follow-up extended beyond the 6-month visit, the study steering committee recommended that efficacy data presentation be limited to the 6-week and 6-month visits in the overall population.
At baseline, there were no statistically significant differences between patients treated and not treated with DEX on day 0 in terms of age, BCVA, CRT, duration of diabetes and DME, presence of central exudates, lens status, history of cataract, or any other baseline variable, except prior treatment status (Tables 1, 2).
Of the 80 patients treated with DEX on day 0, 51 (64.6%) were pseudophakic (Table 1), 30 (37.5%) had not responded to prior non-corticosteroid therapy, and 14 (17.5%) had contraindications to non-corticosteroid therapy. Of the 79 patients treated with DEX on day 0 who had data regarding treatment status at baseline, 11/79 (13.9%) were treatment-naïve, 8/79 (10.1%) were DEX-naïve, and 60/79 (75.9%) had received prior DEX treatments. Of the 32 patients not treated with DEX on day 0 who had data regarding treatment status at baseline, 9.4% were treatment-naïve, 40.6% were DEX-naïve, and 50.0% had received prior DEX treatments (Table 2).
Treatment
On average (SD), the 80 patients treated with DEX on day 0 were followed for 8.3 (3.4) months, completed 2.5 (1.0) visits, and received 1.4 (0.6) DEX injections, with 134.0 (44.9) days between injections (Table 3).
During follow-up of patients who were treated with DEX on day 0, 44/79 (55.7%) did not require retreatment, 32/79 (40.5%) were retreated with DEX at least once, and 3/79 (3.8%) were retreated with alternative therapies only (Table 3). The main reason given for retreating at least once with DEX was increased CRT following initial reduction (n = 24/32, 75.0%; Table 3). The most frequently reported reasons for not retreating with DEX were the initial treatment being successful in managing DME (n = 42/84, 50.0%), followed by ineligibility for retreatment (n = 8/84, 9.5%), use of another therapy (n = 5/84, 6.0%), patient refusal (n = 2/84, 2.4%), and other reasons (n = 27/84, 32.1%).
Efficacy in Patients Treated with DEX on Day 0 (Overall)
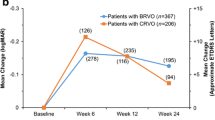
Among patients with data available (n = 79/80), the mean maximum (SD) improvement in BCVA from baseline during follow-up (primary outcome measure) was 3.6 (8.0) letters (95% CI, 1.5, 5.7; n = 59), and the mean (SD) time to reaching maximum BCVA improvement was 77.2 (48.2) days (95% CI, 65.0, 89.5; n = 62). Mean (SD) baseline BCVA was 61.4 (16.5) letters (95% CI, 57.6, 65.1; n = 76), while mean (SD) peak BCVA during follow-up was 65.5 (14.8) letters (95% CI, 61.7, 69.2; n = 62).
At 6 weeks and 6 months, 24.6% and 15.4% of patients gained ≥ 10 letters in BCVA from baseline, while 12.3% and 7.7% gained ≥ 15 letters in BCVA from baseline, respectively (Table 4).
The mean (SD) maximum CRT reduction from baseline reported during follow-up was −146.4 (158.9) µm (95% CI, −187.1, −105.8; n = 61). Mean (SD) baseline CRT was 456.9 (188.8) µm (95% CI, 408.5, 505.2; n = 61), while the mean (SD) minimum CRT was 310.5 (92.0) µm (95% CI, 286.9, 334.1; n = 61).
The proportion of patients whose CRT decreased by ≥ 20% from baseline was 61.4% at week 6 and 36.0% at month 6 (Table 4). During the 8.3-month follow-up (mean), DME resolution (as defined in the Outcome measures section) was reported at least once in 49/72 (68.1%) patients with available data.
Efficacy in Patients Treated with DEX on Day 0, by Treatment Status at Baseline
In subgroup analyses comparing patients who, at baseline, were treatment-naïve (n = 11/79), DEX-naïve (n = 8/79), and previously treated with DEX (n = 60/79), there was no statistically significant difference between subgroups in terms of mean maximum BCVA change from baseline; mean time to reaching the maximum BCVA improvement; and proportions of patients who gained ≥ 10 and ≥ 15 letters in BCVA from baseline at week 6 and month 6 (Supplemental Table 1). Likewise, there was no statistically significant difference between subgroups in terms of mean maximum reduction in CRT from baseline; proportion of patients whose CRT decreased by ≥ 20% from baseline at week 6 and month 6; and proportion of patients with DME resolution during follow-up (Supplemental Table 1).
Safety
Of the total enrolled population (N = 114; Fig. 1), 30 (26.3%) patients reported 66 AEs (Table 5); 45 (68.2%) were ocular in nature, 18 (27.3%) were nonocular, and 3 (4.5%) had missing information. A total of 44 (66.7%) of the 66 AEs resolved without sequelae, 4 (6.1%) resolved with sequelae, 15 (22.4%) were ongoing at study end, and 3 (4.5%) had missing details (patients having been lost to follow-up). Overall, 5 (4.4%) patients discontinued treatment due to AEs, including cataract (n = 3, 2.6%), panophthalmitis (n = 1, 0.9%, in the fellow/non-study eye), and ocular hypertension (n = 1, 0.9%, reported post-recall).
Of the aforementioned 66 AEs, 30 (45.5%) were reported as treatment related (TRAEs) by the investigator. The most frequently reported TRAEs were ocular hypertension (n = 8, 12.1%), cataract development/progression (n = 7, 10.6%, including two eyes of one patient that required surgery), and subconjunctival hemorrhage (n = 5, 7.6%) (Table 5). A total of 17 (25.8%) of the 66 AEs were serious AEs, of which 3 (4.5%) were considered treatment related by the investigator (Table 5).
Among patients treated with DEX on day 0 who had available data, 4/56 (7.1%) reported an IOP increase > 10 mmHg from baseline at week 6, compared with 1/26 (3.8%) at month 6 (Fig. 3). IOP-lowering medication was prescribed in 30.6% (n = 19/62) of patients at week 6 and 41.4% (n = 12/29) at month 6, compared with 21.3% (n = 17/80) at baseline. IOP ≥ 25 mmHg was reported in 6.9% (n = 4/58) and 3.7% (n = 1/27) of patients at week 6 and month 6, while IOP ≥ 35 mmHg was only reported once at week 6 (1.7%; n = 1/58), despite IOP-lowering treatment. Importantly, no laser treatments or filtration surgeries were required to control IOP during follow-up.
Discussion
In this study, 80/112 patients with DME received 1.4 DEX injections over 8.3 months (means), and had a mean maximum BCVA gain of 3.6 letters from baseline. The limited clinical significance could have been due to the large number of patients treated with DEX on day 0 who had received DEX before study entry, which in turn could explain the relatively high mean BCVA at baseline (61.4 letters, compared with 56.1 letters in the pivotal randomized, phase 3 MEAD study [28] and 50.5 letters in the real-world, French, Reldex study [29]), as well as the limited BCVA gain (ceiling effect) observed herein. The fact that 37.5% of patients had not responded to prior non-corticosteroid therapy and that 35.4% were phakic at baseline could also have contributed to the small maximum BCVA gain observed [30,31,32,33,34,35,36,37,38]. However, the low number of DEX injections administered during this study suggests a low risk of developing cataract that argues against lens status being a contributing factor.
The mean time to achieving the maximum BCVA gain in our study (77.2 days) was in line with that reported by Rosenblatt et al. [39] (81.9 days) and Pareja-Rios et al. [40] (~ 90 days). Mean age was similar across these studies [67.3 (our study), 66.3 [39], and 69 [40] years], and the mean number of injections reported herein (1.4 over 8.3 months ≈ 2.0 over 12 months) was higher than that in the aforementioned studies (~ 1.2 [39] versus 1.4 [40] over 12 months).
It seems reasonable to think that the maximum BCVA gain from baseline observed in our study population could have been greater had the study not been terminated prematurely. We cannot, however, exclude the possibility that the duration of DME prior to enrollment (42.4 months in this study; 24.4 months [39]) might have impacted the outcome, as clinical evidence and expert consensus support an association between early treatment and positive visual outcomes [31, 39, 41,42,43,44]. Whether the inclusion of 40.2% of patients with proliferative retinopathy (at baseline) in the current study could have lessened the effects of DEX on outcomes is also unknown, but it is worth noting that of the other studies cited above, only one included such patients, albeit in a lower proportion (11.1%) [30]. In addition, it is possible that the large proportion of patients with an HbA1c > 8% at baseline, 33.3% in our study versus 3.4% in the REINFORCE study [45] (for example), may have dampened the outcomes described herein. Nonetheless, in our study, 24.6% and 15.4% of patients experienced ≥ 10-letter BCVA gains from baseline at week 6 and month 6, respectively.
The reduction in mean maximum CRT from baseline of −146.4 µm observed in this study was statistically significant, clinically meaningful, and in line with that of other published studies (ranging from ~ −120 to −200 µm [30, 39, 40, 45]), despite apparent differences in baseline CRT (range, 424.6–537.6 µm), proportions of treatment-naïve patients (range, 0–100%), and proportion of phakic patients (range, 25.9–60.3%) in those studies [30, 39, 40, 45]. In addition, 61.4% (week 6) and 36.0% (month 6) of patients exhibited CRT reductions ≥ 20%, and 68.1% reported DME resolution at least once during follow-up.
Although PubMed searches identified several publications describing real-world studies of > 1 injections of DEX in DME, few prospectively [30, 40, 45, 46] or retrospectively [39] reported the mean maximum BCVA gain or CRT reduction from baseline during follow-up, and only three reported both outcomes [39, 40, 45]. In a 12-month, multicenter, phase 4 study of 180 eyes (177 patients) with treatment-naïve (6.2%) or previously treated (93.8%) DME that received a mean of 2.0 DEX injections, 99 (55%) eyes received DEX without additional therapy [45]. In this subgroup, the mean maximum CRT reduction from baseline [mean, 424.6 µm (overall population)] was −134.7 µm (n = 74), with mean maximum BCVA improvements from baseline [mean, 54.4 letters (overall population)] of 9.4, 7.3, and 7.9 letters after the first (n = 92), second (n = 51), and third (n = 31) injection, respectively [45]. In a single-center, 12-month study of 113 eyes (84 patients) that received a mean of 1.4 DEX injections, including 9.7% of eyes that were treatment-naïve, mean maximum BCVA increases of 9.7 and 8.8 letters from baseline (43.5 and 56.5 letters) were observed at 3 months in the overall population and treatment-naïve subgroup, respectively [40]. On the other hand, CRT reductions appeared to peak between months 1 and 3 in both the total population (~ −100 µm) and treatment-naïve subgroup (~ −200 µm) [40]. In a multicenter analysis of 340 eyes (287 patients) with treatment-naïve (35%) or previously treated (65%) DME that received a mean of 2.1 DEX injections over 1.8 years (mean follow-up), the mean maximum CRT reduction from baseline [mean, 498 µm (overall population)] was −174 µm, and the mean maximum BCVA gain from baseline [mean, 61.9 letters (overall population)] was 6.8 letters. In both analyses, there were no statistically significant differences between treatment-naïve and previously treated patients [39], consistent with our findings.
In the current study, the definition of TRAEs was broad, including those that were probably or possibly due to the implant itself or injection procedure, and those for which there was uncertainty regarding causality. Nonetheless, our safety findings were consistent with those of other real-world studies of > 1 injection of DEX for DME [29, 30, 39, 40, 45, 47,48,49], as well as the product labeling [50, 51]. There were no unexpected AEs, and ocular hypertension/IOP increase from baseline was the most frequently recorded TRAEs. Regardless, no patients required laser treatment or filtration surgery to control IOP during follow-up, and the proportion of patients requiring topical IOP-lowering medications at 6 months (41.4%) is in line with that reported in the multicenter, retrospective, observational, French SAFODEX and SAFODEX-2 tolerability studies, which involved ≥ 421 eyes that received ≥ 1 DEX injection for macular edema of various etiologies with a relatively long follow-up [52, 53]. Cataract development/progression is also a common, known side effect of DEX [50, 51]; in this study, seven cases were reported during follow-up, including two that required surgery. Notably, the proportion of phakic patients who reported cataract progression or surgery during the study (14.0%) was similar to that reported in two retrospective studies (9% [54] and 13% [55]) and greater than that reported in two prospective studies (≤ 4.5% [56, 57]), but considerably lower than that reported in other prospective (67.9% [28]) and retrospective studies (21.7–73.3% [28, 29, 35, 58,59,60,61,62,63]).
Study limitations included early termination that precluded full enrollment, restricted the number of patients with completed 12-, 18-, and 24-month visits, and prevented statistical analysis of relevant efficacy data at these visits. The lack of a statistically significant difference in outcomes between the patient subgroups that, at baseline, were treatment-naïve, DEX-naïve, and previously treated with DEX should also be interpreted with caution due to the small sample sizes. Moreover, since assessment of DME resolution relied on a definition that was (at least partially) subjective, corresponding findings should be interpreted with caution.
Conclusions
Overall, our findings support real-world efficacy of DEX in improving BCVA and CRT through month 6 in DME, and indicate that DEX continues to be used preferentially in pseudophakic patients; almost two-thirds of patients treated with DEX on day 0 were pseudophakic at baseline. Even as the population that received DEX on day 0 had DME for a mean of 3.7 years and included 75.9% of patients who had received prior DEX treatment before enrollment in this study, 61.4% and 36.0% of patients exhibited CRT reductions ≥ 20% at 6 weeks and 6 months, respectively. In addition, ≤ 7.1% of patients reported an IOP increase > 10 mmHg at those time points, and no laser treatments or filtration surgeries were required to control IOP, confirming DEX’s tolerability. Despite a shorter follow-up than anticipated, the study results show that in a population consisting mostly of patients being already actively treated for relatively long-standing DME, positive outcomes are still achievable with DEX.
References
Frank RN. Diabetic retinopathy. N Engl J Med. 2004;350(1):48–58.
Porta M, Bandello F. Diabetic retinopathy—a clinical update. Diabetologia. 2002;45(12):1617–34.
Lee R, Wong TY, Sabanayagam C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis (Lond). 2015;2:17.
Das UN. Diabetic macular edema, retinopathy and age-related macular degeneration as inflammatory conditions. Arch Med Sci. 2016;12(5):1142–57.
International Diabetes Federation. Diabetes facts & figures. Brussels: International Diabetes Federation; 2019. https://www.idf.org/aboutdiabetes/what-is-diabetes/facts-figures.html.
Mandereau-Bruno L, Fosse-Edorh S. Prévalence du diabète traité pharmacologiquement (tous types) en France en 2015. Disparités territoriales et socio-économiques. Bull Epidémiol Hebd. 2017;27–28:586–91.
Massin P, Feldman-Billard S. Référentiel pour le dépistage et la surveillance des complications oculaires du patient diabétique—2016. Validé par la Société Francophone du Diabète (SFD) et par la Société Française d’Ophtalmologie (SFO). Méd Mal Métab. 2016;10:774–84.
U.K. Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317(7160):703–13.
Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, Davis M, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86.
Wong TY, Sun J, Kawasaki R, Ruamviboonsuk P, Gupta N, Lansingh VC, et al. Guidelines on Diabetic Eye Care: the International Council of Ophthalmology recommendations for screening, follow-up, referral, and treatment based on resource settings. Ophthalmology. 2018;125(10):1608–22.
Mesquida M, Drawnel F, Fauser S. The role of inflammation in diabetic eye disease. Semin Immunopathol. 2019;41(4):427–45.
Miller K, Fortun JA. Diabetic macular edema: current understanding, pharmacologic treatment options, and developing therapies. Asia Pac J Ophthalmol (Phila). 2018;7(1):28–35.
Heier JS, Korobelnik JF, Brown DM, Schmidt-Erfurth U, Do DV, Midena E, et al. Intravitreal aflibercept for diabetic macular edema: 148-week results from the VISTA and VIVID studies. Ophthalmology. 2016;123(11):2376–85.
Korobelnik JF, Do DV, Schmidt-Erfurth U, Boyer DS, Holz FG, Heier JS, et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology. 2014;121(11):2247–54.
Brown DM, Nguyen QD, Marcus DM, Boyer DS, Patel S, Feiner L, et al. Long-term outcomes of ranibizumab therapy for diabetic macular edema: the 36-month results from two phase III trials: RISE and RIDE. Ophthalmology. 2013;120(10):2013–22.
Rajendram R, Fraser-Bell S, Kaines A, Michaelides M, Hamilton RD, Esposti SD, et al. A 2-year prospective randomized controlled trial of intravitreal bevacizumab or laser therapy (BOLT) in the management of diabetic macular edema: 24-month data: report 3. Arch Ophthalmol. 2012;130(8):972–9.
Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L, et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119(4):789–801.
Mitchell P, Bandello F, Schmidt-Erfurth U, Lang GE, Massin P, Schlingemann RO, et al. The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118(4):615–25.
Michaelides M, Kaines A, Hamilton RD, Fraser-Bell S, Rajendram R, Quhill F, et al. A prospective randomized trial of intravitreal bevacizumab or laser therapy in the management of diabetic macular edema (BOLT study) 12-month data: report 2. Ophthalmology. 2010;117(6):1078-86.e2.
Schmidt-Erfurth U, Garcia-Arumi J, Bandello F, Berg K, Chakravarthy U, Gerendas BS, et al. Guidelines for the management of diabetic macular edema by the European Society of Retina Specialists (EURETINA). Ophthalmologica. 2017;237(4):185–222.
Amoaku WM, Saker S, Stewart EA. A review of therapies for diabetic macular oedema and rationale for combination therapy. Eye (Lond). 2015;29(9):1115–30.
Sampat KM, Garg SJ. Complications of intravitreal injections. Curr Opin Ophthalmol. 2010;21(3):178–83.
Agence Nationale de Securite du Medicament et des Produits de Sante. Ozurdex 700 microgrammes, implant intravitréen avec applicateur—Allergan France—Rappel de lots. Saint-Denis: Agence nationale de securite du medicament et des produits de sante; 2018. https://ansm.sante.fr/informations-de-securite/ozurdex-700-microgrammes-implant-intravitreen-avec-applicateur-allergan-france-1.
World Medical Association. 1964 World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. Helsinki: World Medical Association; 2013. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/.
Commission Nationale de l'Informatique et des Libertés. Loi Informatique et Libertés Act N° 78-17 of 6 January 1978 on Information Technology, Data Files and Civil Liberties. Paris: Commission Nationale de l'Informatique et des Libertés; 1978. https://www.cnil.fr/sites/default/files/typo/document/Act78-17VA.pdf.
Association des Epidémiologistes de Langue Française (ADELF). Recommendations for professional standards and good epidemiological practices. Bordeaux: Association des Epidémiologistes de Langue Française (ADELF); 2007. https://www.constances.fr/base-documentaire/2015/1421662226-adelf-recommendations-english.pdf.
Haute Autorité de Santé. Les études post-inscription sur les technologies de santé (médicaments, dispositifs médicaux et actes) - Principes et methodes. Saint-Denis La Plaine: Haute Autorité de Santé; 2011. https://has-sante.fr/upload/docs/application/pdf/2012-01/etudes_post_inscription_technologies_sante.pdf.
Boyer DS, Yoon YH, Belfort R Jr, Bandello F, Maturi RK, Augustin AJ, et al. Three-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology. 2014;121(10):1904–14.
Malclès A, Dot C, Voirin N, Agard É, Vié AL, Bellocq D, et al. Real-life study in diabetic macular edema treated with dexamethasone implant: the Reldex Study. Retina. 2017;37(4):753–60.
Chatziralli I, Theodossiadis P, Parikakis E, Dimitriou E, Xirou T, Theodossiadis G, et al. Dexamethasone intravitreal implant in diabetic macular edema: real-life data from a prospective study and predictive factors for visual outcome. Diabetes Ther. 2017;8(6):1393–404.
Bux AV, Fortunato F, Barone A, Russo V, DelleNoci N, Iaculli C. Early treatment with dexamethasone intravitreal implants in diabetic macular edema: naïve versus refractory patients. Eur J Ophthalmol. 2021;32(3):1619–26.
Iglicki M, Busch C, Zur D, Okada M, Mariussi M, Chhablani JK, et al. Dexamethasone implant for diabetic macular edema in naive compared with refractory eyes: the International Retina Group real-life 24-month multicenter study. The IRGREL-DEX Study. Retina. 2019;39(1):44–51.
Neves P, Ornelas M, Matias I, Rodrigues J, Santos M, Dutra-Medeiros M, et al. Dexamethasone intravitreal implant (Ozurdex) in diabetic macular edema: real-world data versus clinical trials outcomes. Int J Ophthalmol. 2021;14(10):1571–80.
Wang JK, Huang TL, Hsu YR, Chang PY. Effect of dexamethasone intravitreal implant for refractory and treatment-naive diabetic macular edema in Taiwanese patients. J Chin Med Assoc. 2021;84(3):326–30.
Akıncıoğlu D, Küçükevcilioğlu M, Durukan AH, Aykaş S, Ayyıldız Ö, Erdurman FC. Outcomes of intravitreal dexamethasone implant in the treatment of recalcitrant diabetic macular edema. Turk J Ophthalmol. 2017;47(5):274–8.
Figueira J, Henriques J, Amaro M, Rosas V, Alves D, Cunha-Vaz J. A nonrandomized, open-label, multicenter, phase 4 pilot study on the effect and safety of ILUVIEN® in chronic diabetic macular edema patients considered insufficiently responsive to available therapies (RESPOND). Ophthalmic Res. 2017;57(3):166–72.
Moon BG, Lee JY, Yu HG, Song JH, Park YH, Kim HW, et al. Efficacy and safety of a dexamethasone implant in patients with diabetic macular edema at tertiary centers in Korea. J Ophthalmol. 2016;2016:9810270.
Nicolò M, Musetti D, Marenco M, Cotti L, Bonetto M, Giacomini M, et al. Real-life management of diabetic macular edema with dexamethasone intravitreal implant: a retrospective analysis of long-term clinical outcomes. J Ophthalmol. 2020;2020:4860743.
Rosenblatt A, Udaondo P, Cunha-Vaz J, Sivaprasad S, Bandello F, Lanzetta P, et al. A collaborative retrospective study on the efficacy and safety of intravitreal dexamethasone implant (Ozurdex) in patients with diabetic macular edema: the European DME Registry Study. Ophthalmology. 2020;127(3):377–93.
Pareja-Ríos A, Ruiz-de la Fuente-Rodríguez P, Bonaque-González S, López-Gálvez M, Lozano-López V, Romero-Aroca P. Intravitreal dexamethasone implants for diabetic macular edema. Int J Ophthalmol. 2018;11(1):77–82.
García Layana A, Adán A, Ascaso FJ, Cabrera F, Donate J, Escobar Barranco JJ, et al. Use of intravitreal dexamethasone implants in the treatment of diabetic macular edema: expert recommendations using a Delphi approach. Eur J Ophthalmol. 2020;30(5):1042–52.
Song W, Singh RP, Rachitskaya AV. The effect of delay in care among patients requiring intravitreal injections. Ophthalmol Retina. 2021;5(10):975–80.
Sadda SR, Campbell J, Dugel PU, Holekamp NM, Kiss S, Loewenstein A, et al. Relationship between duration and extent of oedema and visual acuity outcome with ranibizumab in diabetic macular oedema: a post hoc analysis of Protocol I data. Eye (Lond). 2020;34(3):480–90.
Yassin SA, ALjohani SM, Alromaih AZ, Alrushood AA. Optical coherence tomography patterns of diabetic macular edema in a Saudi population. Clin Ophthalmol. 2019;13:707–14.
Singer MA, Dugel PU, Fine HF, Capone A Jr, Maltman J. Real-world assessment of dexamethasone intravitreal implant in DME: findings of the prospective, multicenter REINFORCE Study. Ophthalmic Surg Lasers Imaging Retina. 2018;49(6):425–35.
Comet A, Gascon P, Ramtohul P, Donnadieu B, Denis D, Matonti F, et al. INVICTUS: intravitreal anti-VEGF and dexamethasone implant comparison for the treatment of diabetic macular edema: a 12 months follow-up study. Eur J Ophthalmol. 2020;127(3):754–8.
Gutiérrez-Benítez L, Millan E, Arias L, Garcia P, Cobos E, Caminal M. Dexamethasone intravitreal implants for diabetic macular edema refractory to ranibizumab monotherapy or combination therapy. Arch Soc Esp Oftalmol. 2015;90(10):475–80.
Mello Filho P, Andrade G, Maia A, Maia M, Biccas Neto L, Muralha Neto A, et al. Effectiveness and safety of intravitreal dexamethasone implant (Ozurdex) in patients with diabetic macular edema: a real-world experience. Ophthalmologica. 2018;241(1):9–16.
Nair U, Gupta V, Sharma M, Joshi S, Sudhalkar A, Altangerel U, et al. Postmarketing safety surveillance of dexamethasone intravitreal implant in the treatment of visual impairment due to diabetic macular edema in India. BMC Ophthalmol. 2020;20(1):405.
Allergan (an AbbVie company). Highlights of prescribing information—OZURDEX® (dexamethasone intravitreal implant) for intravitreal injection. Madison: Allergan, an AbbVie company; 2018. https://media.allergan.com/actavis/actavis/media/allergan-pdf-documents/product-prescribing/20180515-OZURDEX-USPI-v1-0USPI3348.pdf.
European Medicines Agency. Ozurdex (dexamethasone)—an overview of Ozurdex and why it is authorised in the EU. Amsterdam: European Medicines Agency; 2019. https://www.ema.europa.eu/en/documents/overview/ozurdex-epar-medicine-overview_en.pdf.
Rezkallah A, Mathis T, Abukhashabah A, Voirin N, Malclès A, Agard É, et al. Long-term incidence and risk factors of ocular hypertension following Dexamethasone-implant injections. The SAFODEX-2 study. Retina. 2020;41(7):1438–45.
Malclès A, Dot C, Voirin N, Vié AL, Agard É, Bellocq D, et al. Safety of intravitreal dexamethasone implant (Ozurdex): the SAFODEX study. Incidence and risk factors of ocular hypertension. Retina. 2017;37(7):1352–9.
Zhioua I, Semoun O, Lalloum F, Souied EH. Intravitreal dexamethason implant in patients with ranibizumab persistent diabetic macular edema. Retina. 2015;35(7):1429–35.
Yucel OE, Can E, Ozturk HE, Birinci H, Sullu Y. Dexamethasone implant in chronic diabetic macular edema resistant to intravitreal ranibizumab treatment. Ophthalmic Res. 2017;57(3):161–5.
Bilgic A, Sudhalkar A, Kodjikian L, Vasavada V, Vasavada S, Bhojwani D, et al. Pro re nata dexamethasone implant for treatment-naive phakic eyes with diabetic macular edema: a prospective study. Ophthalmol Retina. 2019;3(11):929–37.
Özata K, Atum M, Çelik E, Doğan E, Alagöz G. Efficacy of intravitreal dexamethasone implant in persistent diabetic macular edema after primary treatment with intravitreal ranibizumab. J Curr Ophthalmol. 2019;31(3):281–6.
De Geronimo D, Giorno P, Scarinci F, Boninfante A, Varano M, Parravano M. Treatment of diabetic macular edema with multiple dexamethasone intravitreal implants: evidence from real-life experience. Ophthalmologica. 2020;243(6):413–9.
Lam WC, Albiani DA, Yoganathan P, Chen JC, Kherani A, Maberley DA, et al. Real-world assessment of intravitreal dexamethasone implant (0.7 mg) in patients with macular edema: the CHROME study. Clin Ophthalmol. 2015;9:1255–68.
Mathis T, Lereuil T, Abukashabah A, Voirin N, Sudhalkar A, Bilgic A, et al. Long-term follow-up of diabetic macular edema treated with dexamethasone implant: a real-life study. Acta Diabetol. 2020;57(12):1413–21.
Medina-Baena M, Cejudo-Corbalán O, García-Pulido JI, Huertos-Carrillo MJ, Girela-López E. Intravitreal dexamethasone implant in naïve and previously treated patients with diabetic macular edema: a retrospective study. Int J Ophthalmol. 2020;13(10):1597–605.
Rajesh B, Zarranz-Ventura J, Fung AT, Busch C, Sahoo NK, Rodriguez-Valdes PJ, et al. Safety of 6000 intravitreal dexamethasone implants. Br J Ophthalmol. 2020;104(1):39–46.
Ratra D, Sharma U, Dalan D. Efficacy and safety of intravitreal dexamethasone implant in treatment naïve eyes with diabetic macular edema: real world experience. Eur J Ophthalmol. 2020;31(4):899–906.
Acknowledgements
We acknowledge the following institutions (investigators/participating physicians) for their participation in the study: Centre Hospitalier Universitaire Avicennes (Audrey Giocanti); Centre Hospitalier Universitaire de Brest (Béatrice Cochener, Yvan Delafoy); Centre Hospitalier Universitaire Pasteur 2 (Stéphanie Baillif, David Martiano); Centre Hospitalier Régional Universitaire (Benjamin Jany, Solange Milazzo, Nabil Taright); Centre MGM (Sébastien Guigou, Pierre-Yves Mérité, Franck Meyer); Centre Ophta.Kervision (Alexandre Bourhis); Centre Rétinien Gallien (Marcel Dominguez, Éric Fourmaux, Laurence Rosier, Laurent Velasque); Clinique Monticelli (Frédéric Matonti, Christophe Morel); Hôpital de la Croix-Rousse (Laurent Kodjikian); Hôpital d'Instruction des Armées Desgenettes (Corinne Dot); Hôpital Lariboisière APHP (Ramin Tadayoni); Hôpital Nord Marseille (Alban Comet); Hôpital Pellegrin (Marie-Nöelle Delyfer, Jean-François Korobelnik, Marie-Bénédicte Rougier, Camille Séguy); Hôpital Poissy (Corinne Biton).
The authors would like to thank all the patients who participated in this study, which was sponsored by Allergan (prior to its acquisition by AbbVie Inc., North Chicago, IL), as well as Andrew Shirlaw (AbbVie Inc.) for his support with the study oversight, Doris Barnier-Ripet and Karol-Anne Cage (Axonal-Biostatem) for project management, Estelle Jouanneau (Axonal-Biostatem) as clinical trial assistant, Marina Duplessis and Lilia Babouche (Axonal-Biostatem) as clinical research assistants, Marie Laborde (Axonal-Biostatem) as clinical research associate, and Gwendoline Moreau and Muriel Tounsi (Axonal-Biostatem) as study statisticians.
Funding
The study, creation, and publication of the graphical abstract, and journal’s Rapid Service Fee were funded by Allergan, an AbbVie company. The sponsor participated in the study design, data management, analysis, and interpretation, as well as preparation, review, and approval of the manuscript.
Medical Writing, Editorial, and Other Assistance
Writing and editorial assistance were provided to the authors by Michele Jacob, PhD, of Evidence Scientific Solutions, Inc (Philadelphia, PA) and funded by AbbVie Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) authorship criteria, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. Neither honoraria nor payments were made for authorship.
Author Contributions
Study conception and design: Laurent Kodjikian, Cécile Delcourt, Catherine Creuzot-Garcher, Pascale Massin, John Conrath, and Marie-Ève Velard. Data acquisition, analysis, and/or interpretation: all authors. Writing, original draft preparation: Thibaut Lassalle, Sybil Pinchinat, and Laure Dupont-Benjamin. Writing, review and editing: all authors. Approval of the final version of the manuscript: all authors.
Disclosures
Financial arrangements of the authors with companies whose products may be related to the present report follow, as declared by the authors. Laurent Kodjikian is a consultant for Allergan (an AbbVie company), Bayer, Laboratoires Théa, Novartis, and Roche. Cécile Delcourt is a consultant for Allergan (an AbbVie company), Bausch + Lomb, Laboratoires Théa, and Novartis. Catherine Creuzot-Garcher is a consultant for AbbVie, Allergan (an AbbVie company), Bausch + Lomb, Bayer, Horus Pharma, Novartis, and Laboratoires Théa. Pascale Massin is a consultant for Allergan (an AbbVie company) and Novartis. John Conrath is a consultant for Alcon, Alimera, Allergan (an AbbVie company), Bayer, Ellex, Novartis, and Roche. Marie-Ève Velard and Laure Dupont-Benjamin are employees of AbbVie Inc and may hold AbbVie stock/share options. Thibaut Lassalle was an employee of Axonal-Biostatem (the contract research organization in charge of the study) at the time the study was conducted; he is a current employee of Excelya. Sybil Pinchinat is an employee of Axonal-Biostatem.
Compliance with Ethics Guidelines
Before the study start, the protocol was approved by the Comité Consultatif sur le Traitement de l’Information en Matière de Recherche dans le Domaine de la Santé (CCTIRS; reference number, 16.105), Commission Nationale de l’Informatique et Libertés [CNIL; reference number, MMS/HGT/AR177119 (Authorization number: DR-2017-124)], and Conseil National de l’Ordre des Médecins (CNOM; reference number, 16-246-071). The study adhered to the principles of the Declaration of Helsinki and later amendments [24], French Public Health Code and French Act on Data Processing, Data Files, and Individual Liberties [25], Good Epidemiological Practices [26], and guidelines from the Haute Autorité de Santé on post-registration studies [27]. Each patient provided written informed consent to participate in the study before study initiation, and all authors consented to publication of the manuscript.
Data Availability
AbbVie is committed to responsible data sharing regarding the clinical trials we sponsor. This includes access to anonymized, individual, and trial-level data (analysis datasets), as well as other information (e.g., protocols, clinical study reports, or analysis plans), as long as the trials are not part of an ongoing or planned regulatory submission. This includes requests for clinical trial data for unlicensed products and indications.
These observational study data can be requested by any qualified researchers who engage in rigorous, independent scientific research, and will be provided following review and approval of a research proposal and statistical analysis plan (SAP) and execution of a data sharing agreement (DSA). Data requests can be submitted at any time after approval in the US and Europe and after acceptance of this manuscript for publication. The data will be accessible for 12 months, with possible extensions considered. For more information on the process, or to submit a request, visit the following link: https://www.abbvieclinicaltrials.com/hcp/data-sharing/.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kodjikian, L., Delcourt, C., Creuzot-Garcher, C. et al. Prospective, Observational, Multicenter, Real-World Study of the Efficacy, Safety, and Pattern of Use of the Dexamethasone Intravitreal Implant in Diabetic Macular Edema in France: Short-Term Outcomes of LOUVRE 3. Ophthalmol Ther 12, 1671–1692 (2023). https://doi.org/10.1007/s40123-023-00662-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00662-8