Abstract
Introduction
To compare the efficacy and safety of intravitreal injections of ranibizumab (IVR) before and at the end of vitrectomy in proliferative diabetic retinopathy (PDR) patients.
Methods
A prospective comparative study was performed on 60 eyes of 52 PDR patients who received ranibizumab injection (0.5 mg/0.05 ml) 3–5 days before vitrectomy (preoperative group) and 55 eyes of 50 PDR patients who received ranibizumab injection (0.5 mg/0.05 ml) at the end of vitrectomy (intraoperative group). Intra- and postoperative indices were collected for further comparison.
Results
Postoperative best-corrected visual acuity (BCVA) in preoperative group was better than in intraoperative group at 1 week after surgery (P < 0.05) but comparable at 1- and 3-month follow-up (P = 0.20 and P = 0.37, respectively). Central retinal thickness (CRT) in preoperative group was lower than in intraoperative group at 1 week postoperatively (P < 0.05), but comparable at 1- and 3-month follow-up (P = 0.39 and P = 0.77, respectively). The average surgery time was significantly shorter in preoperative group than in intraoperative group (61.50 ± 11.44 min vs. 74.49 ± 12.01 min, P < 0.01). The incidence of intraoperative bleeding was significant lower in preoperative group than in intraoperative group (21.7% vs. 40.0%, P < 0.05). Moreover, the incidence of intraocular electrocoagulation use, iatrogenic retinal breaks, relaxing retinotomy and silicone oil tamponade were all significantly lower in preoperative group than that in intraoperative group (P < 0.05, respectively). The incidences of postoperative vitreous hemorrhage (VH), neovascular glaucoma (NVG), recurrent retinal detachment, postoperative fibrovascular proliferation progression and reoperation showed no statistical differences between the two groups (P > 0.05, respectively). Both groups had no ocular or system adverse events during observation period.
Conclusion
In vitrectomy for PDR, preoperative IVR can significantly reduce surgery time and lower the incidence of intraoperative bleeding, intraocular electrocoagulation use, iatrogenic retinal breaks, relaxing retinotomy and silicone oil tamponade during surgery and gain short-term better postoperative BCVA and thinner CRT.
Trial registration: ClinicalTrials.gov (identifier, NCT05408416).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Pars plana vitrectomy (PPV) is an indispensable means for the treatment of proliferative diabetic retinopathy (PDR), which is one of the most serious blinding eye diseases. Anti-vascular endothelial growth factor (VEGF) drugs combined with PPV can certainly improve the efficiency of surgery. However, it is not clear whether different injection timing affects the outcomes of surgery. |
What was learned from the study? |
Compared to intraoperative intravitreal ranibizumab (IVR), preoperative IVR can significantly reduce surgery time and lower the incidence of intraoperative bleeding, intraocular electrocoagulation use, iatrogenic retinal breaks, relaxing retinotomy as well as silicone oil tamponade during surgery. |
Meanwhile, preoperative IVR can gain better postoperative best-corrected visual acuity (BCVA) and thinner central retinal thickness (CRT) in a short time after surgery for PDR. |
Introduction
Proliferative diabetic retinopathy (PDR) is the most common cause of irreversible blindness in diabetic retinopathy (DR) [1, 2]. It is characterized by progressive loss of vision, retinal edema, vitreous hemorrhage (VH), retinal neovascularization, fibrovascular proliferation, tractional retinal detachment (TRD) and neovascular glaucoma (NVG) [3, 4]. Although pars plana vitrectomy (PPV) is the cornerstone of treatment of advanced PDR, related postoperative complications such as recurrent VH, NVG and progressive fibrovascular proliferation may still cause serious visual impairment.
It is well known that vascular endothelial growth factor (VEGF) plays a leading role in neovascularization, vascular permeability and diabetic macular edema [5, 6]. Intravitreal injection of anti-VEGF drugs before or during PPV may be a good adjunct to vitreous surgery for PDR. Some studies have confirmed that the application of anti-VEGF drugs before vitrectomy for PDR patients can reduce the difficulty of surgery and improve postoperative best-corrected visual acuity (BCVA) [7,8,9], but very few studies have focused on the injections of anti-VEGF during surgery [10]. The lack of a well-structured prospective study makes it difficult to assess the benefit of these two different strategies. Therefore, we carried out this study to compare the effects of pre- and intraoperative intravitreal injections of ranibizumab (IVR) on vitrectomy outcomes for PDR patients.
Methods
Study Design
This was a prospective, single-center and randomized controlled clinical trial study which was registered at ClinicalTrials.gov (NCT05408416). This study was approved by Human Ethics Committee Institutional Review Board of Peking University People’s Hospital (2021PHB405-001). All procedures adhered to the tenets of the Declaration of Helsinki of 1964 and its later amendments. All participants provided informed consents before surgery; informed consent for publication was obtained from all participants.
Patients
PDR patients with indications for vitrectomy between September 2021 and February 2022 at Peking University People’s Hospital were screened for eligibility. Our inclusion criteria were as follows: (1) patients aged ≥ 18 years with type 1 or 2 diabetes who were clinically diagnosed with PDR; (2) had persistent VH for > 1 month or recurrent VH with or without panretinal photocoagulation (PRP); (3) had TRD detected by indirect ophthalmoscope or B-scan ultrasonography; (4) had an actively progressing fibrovascular proliferative membrane. The exclusion criteria included: (1) previous vitrectomy or intravitreal injection in the study eyes; (2) eyes with any ocular disease that may hinder visual improvement other than PDR, such as optic atrophy or macular hole or macular epiretinal membranes; (3) neovascular glaucoma; (4) eyes given gas tamponade or additional treatment like ranibizumab injection again or supplementary macular photocoagulation during follow-up periods; (5) poor control of diabetes mellitus (DM) with hemoglobin A1c (HbA1c) > 12%; (6) history of thromboembolic events (including cerebral vascular infarctions or myocardial infarctions) or coagulation system disorders or receiving anticoagulant or antiplatelet therapy; (7) having systemic conditions that may increase the risk of bleeding, such as respiratory disease or uncontrolled coughing. The enrolled eyes were randomly assigned according to the Central Randomization System with a ratio of 1:1 to preoperative IVR group and intraoperative IVR group.
Intervention and Measures
Patients received 0.5 mg/0.05 ml IVR 3–5 days before vitrectomy in preoperative IVR group and 0.5 mg/0.05 ml IVR immediately at the end of vitrectomy in intraoperative IVR group. All patients underwent 25-gauge transconjunctival sutureless vitrectomy using the 25-gauge Constellation system (Alcon, Fort Worth, TX, USA) under local or general anesthesia. A speed of 5000 cuts per minute was used for vitrectomy. The specific procedures were as follows: vitreous and hemorrhage were removed completely; preretinal fibrovascular proliferation membranes were peeled thoroughly or left as isolated residual pieces; intraoperative bleeding was controlled by either intraocular electrocoagulation or increased irrigation pressure; relaxing retinotomy was carried out when the existence of subretinal proliferative strips hindered retinal reattachment or peripheral thin retina adhered tightly by fibrovascular proliferation membrane leading to tractional retinal detachment; full PRPs were performed or complete in all eyes; silicone oil tamponade was used when there were retinal breaks combined retinal detachment. All surgical procedures were performed by the same experienced vitreoretinal specialist (QJF). All patients received antibiotics and 1% prednisolone eye drops with tapered frequency during the 4-week period after surgery.
Baseline demographics and systemic conditions including course of diabetes mellitus and hypertension were recorded. All patients underwent a full ophthalmic examination, including automatic refractometry, best-corrected visual acuity (BCVA), intraocular pressure (IOP), slit-lamp examination, indirect ophthalmoscopy, color fundus photography, spectral domain optical coherence tomography (SD-OCT) (CIRRUS HD-OCT Model 5000, Carl Zeiss Meditec, Germany), ultra-wide-field (UWF) fundus fluorescein angiography (FFA) using Optos 200Tx (Optos plc, Dunfermline, UK) and B-scan ultrasonography if necessary. BCVA was converted to logarithm of minimal angle of resolution (log MAR) scale for statistic analysis; counting fingers vision was recorded as 2.0 log MAR, and hand movement was recorded as 3.0 log MAR. Central retinal thickness (CRT) was measured on the same machine, using its tracking software known as FastTracTM retinal-tracking technology for each follow-up visit [11]. Extent of vitreoretinal adhesion was defined following the previous vitreoretinal adhesion grade (VAG) classification system: absence of any adhesion was grade 0; focal adhesion < 3 sites was grade 1; broad adhesion of ≥ 1 site or adhesion at the disc, macular, or vascular arcade was grade 2; vitreoretinal adhesion extending to the periphery was grade 3 [12]. Patients underwent all examinations at baseline, 1 day, 1 week, 1 month and 3 months after surgery.
Statistical Analysis
Baseline characteristics of all the patients were collected and analyzed using SPSS Statistics 19.0 software (IBM SPSS Inc., Chicago, IL, USA). Normally distributed continuous variables were presented as mean ± SD. Non-normally distributed continuous variables were presented as median [interquartile range (IQR)]. Student’s t-test was performed to compare normally distributed quantitative variables, while the nonparametric Wilcoxon signed rank test was used for abnormally distributed quantitative variables. Categorical data were analyzed using Pearson’s chi-square test or Fisher’s exact test. A threshold of P-value < 0.05 was set for statistical significance.
Results
Baseline Demographics
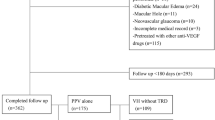
A total of 137 eyes of 120 patients were enrolled in the study and assigned randomly into two groups: 70 eyes of 60 patients in preoperative group and 67 eyes of 60 patients in intraoperative group. Three eyes withdraw (1 in preoperative group and 2 in intraoperative group) before PPV. Nineteen eyes were removed from the protocol for gas tamponade during surgery (1 in preoperative group and 2 in intraoperative group), additional treatment (6 in preoperative group and 5 in intraoperative group) and not showing up (2 in preoperative group and 3 in intraoperative group) during 3-month follow-up period. Finally, 60 eyes of 52 PDR patients in preoperative group and 55 eyes of 50 PDR patients in intraoperative group were included in the study (Fig. 1). Baseline characteristics and demographics of all included patients in both groups are listed in Table 1. There were no statistically significant differences in age, sex, BMI, type of diabetes, HbA1c level, duration of DM, hypertension, previous history of laser photocoagulation, status of lens, indication for surgery, baseline BCVA, IOP, baseline CRT and extent of VAG between the two groups (Table 1).
Surgical Procedures and Outcomes
The surgical procedures and outcomes are shown in Table 2. The average surgery time was 61.50 ± 11.44 min in preoperative group and 74.49 ± 12.01 min in intraoperative group (P < 0.01). The incidences of intraoperative bleeding were 13 (21.7) and 22 (40.0) in pre- and intraoperative group, respectively (P < 0.05). Moreover, the incidences of iatrogenic retinal breaks and relaxing retinotomy were significantly lower in pre- than intraoperative group (P < 0.05, respectively). Intraocular electrocoagulation use and silicone oil tamponade in preoperative group were less frequent than in intraoperative group (P < 0.05, respectively). There were no statistically significant differences in retinal reattachment between the two groups (P = 0.61).
No significant differences were found in sum numbers of postoperative events during 3-month follow-up between the two groups (VH recurrence, P = 0.88; NVG occurrence, P = 0.58; recurrent retinal detachment, P = 0.58, postoperative progressive fibrovascular proliferation, P = 0.93, and reoperation, P = 0.90) (Table 3).
Postoperative BCVA at 1-week follow-up visit was better in pre- than intraoperative group (P < 0.05), but not at the 1- and 3-month follow-up visits (P = 0.20 and P = 0.37, respectively) (Table 4 and Fig. 2). CRT in preoperative group was lower than that in intraoperative group at 1 week postoperatively (P < 0.05), but did not differ significantly at 1- and 3-month follow-up (P = 0.39 and P = 0.77, respectively) (Table 5 and Fig. 3).
No ocular or system adverse events such as endophthalmitis, cardiovascular or cerebral vascular events occurred in either group during our observation (Figs. 4, 5).
A 58-year-old woman underwent PPV for significant vitreous hemorrhage (A and E). Recurrent bleeding occurred 1 week after surgery (B and F). VH was significantly absorbed at 1 month (C) and parafovea retinal edema was observed too (G). VH was completely absorbed at 3 month (D), and PRP was clearly visible. The parafovea retinal edema was stable (H)
A 45-year-old male who had underwent incomplete PRP was prepared for PPV for diffuse FP (A) with hard exudation at parafovea (E). Supplemented intraoperative laser photocoagulation (B) and hard exudation at parafovea (F) can be observed at 1 week’s fundus and OCT images. Retinal patchy hemorrhage disappeared (C), and hard exudation was further absorbed (G) 1 month after surgery. At the 3rd month, the fundus was stable (D) with a good fovea structure (H)
Discussion
PDR is usually complicated with intraocular hemorrhage, fibrovascular proliferation and TRD, especially in eyes with active neovascularization membrane. The surgical procedures could be quite difficult because of fibrovascular membrane hemorrhage and iatrogenic retinal breaks, rendering extensive use of intraocular electrocoagulation and retinotomy necessary. Risks of recurrent VH, uncontrollable NVG, postoperative progressive fibrovascular proliferation, recurrent retinal detachment and reoperations are also high [13, 14]. VEGF has been proved to play an important role in neovascularization. Due to the immature vessel structure of neovascular membrane, it usually is accompanied by bleeding and leakage in the retina, leading to poor vision. Intravitreal injection of anti-VEGF agents can induce vascular endothelial cell apoptosis and reverse the progress of retina neovascularization, resulting in occlusion or regression of abnormal vessels as well as decreased fundus exudation and bleeding [15]. It can also increase pericyte numbers and promote angiogenesis as well as vascular maturation to maintain stability of the blood retinal barrier [15]. Therefore, intravitreal injection of anti-VEGF drugs has been proven to be a good adjunct to vitrectomy in PDR patients.
We compared two different injection timings during the perioperative period of vitrectomy and found that preoperative injection of ranibizumab can reduce the difficulty of surgery and lead better postoperative BCVA and thinner CRT in 1 week, but there were no differences in long-term vision and macular thickness. Chen et al. compared the effects of pre- versus postoperative injection of anti-vascular endothelial growth factor (VEGF) drugs in patients with vitreous hemorrhage secondary to polypoidal choroidal vasculopathy (PCV). They found that preoperative injection led to less subsequent injection frequency, lower incidence of recurrent vitreous hemorrhage, better BCVA and thinner fovea over a period of time, but the differences of the latter two disappeared after 3 months [16]. Preoperative anti-VEGF injection could promote regression of neovascularization and facilitate fibrovascular membrane dissection with less intraoperative bleeding during surgery, therefore causing lower incidence of intraocular electrocoagulation use, iatrogenic retinal breaks, relaxing retinotomy and silicone oil tamponade during surgery, which were also demonstrated in this study. However, due to the fast washout of anti-VEGF during surgery, there was no further effect on remnant neovascularization after the surgery. Therefore, we did not see the benefit of preoperative ranibizumab to BCVA continued after 1 week. On the other hand, although injection of anti-VEGF at the end of vitrectomy will not affect those parameters during surgery, eyes in intraoperative group could maintain a relatively high level of anti-VEGF after vitrectomy, which is expected to help against continuing regression of retinal neovascularization and macular edema. However, we did not find significant difference of BCVA at 1 or 3 months between the two groups. This may be explained by the shorter half-life of anti-VEGF in a vitrectomized eye. Vitrectomized eyes are filled by aqueous humor instead of vitreous, which will change the pharmacokinetics of anti-VEGF accordingly.
Previous studies reported that the half-life of ranibizumab in aqueous humor were shorter in vitrectomized eyes than in nonvitrectomized eyes of Macaque monkeys (1.4 and 2.3 days, respectively) [17]. Christoforidis et al. found that vitrectomy reduced the half-life of ranibizumab in rabbit eyes from 2.81 to 2.13 days [18]. The clearance rates of intravitreally placed medications such as bevacizumab, ranibizumab and triamcinolone acetonide have been shown to be faster after vitrectomy. VEGF levels fell below the level of detection for 1 week after intravitreal ranibizumab in vitrectomized eyes and for 4 weeks in non-vitrectomized eyes [19, 20]. Relevant studies in the human body showed that the half-life of ranibizumab was 7.15 days in normal human eyes, and intravitreal retention of ranibizumab was significantly reduced after vitrectomy [21]. Bressler SB et al. and Chen et al. also found that vitrectomized eyes required more frequent injections for improving BCVA and CRT than non-vitrectomized eyes [22, 23]. Koyanagi et al. showed significant BCVA and visual gain after intravitreal ranibizumab in nonvitrectomized eyes compared with vitrectomized eyes at each visit during 6-month follow-up [24]. Therefore, presumably higher intravitreal drug clearance in vitrectomized eyes could result in more rapid drug diffusion and lower drug concentration, implying limited exposure time of intravitreal drug to the retina and less benefit on visual gains as well as macular edema. With the self-repairing of the retinal vessel and diminishment of anti-VEGF effect, the benefit of anti-VEGF on BCVA and CRT will also disappear after a longer time, consistent with our results that BCVA and CRT at 1- and 3-month follow-up visits showed no significant differences between groups.
The effect of silicone oil on CRT measurement should also be considered. Silicone oil filling may accelerate the absorption of subretinal fluid and, in addition, reduce the thickness of the inner retina. Gilad et al. analyzed 51 silicone oil tamponade eyes of which the average filling time was 151 days. They found a mean change of 26 mm in the internal layers [25]. Albert et al. analyzed nine individuals receiving silicone oil endo-tamponade for 135 days on average and found the inner retinal layers became subsequently thinner. Ganglion cell and inner plexiform layers contribute most to this thinning, while outer retinal layers were not affected [26]. However, the follow-up period of our study was 3 months, which was significantly less than the above study duration. So, the effect of silicone oil tamponade on CRT is difficult to define. However, Kheir et al. reported that the mean CRT decreased 3 months after silicone oil tamponade, which was followed by an increase after silicone oil removal; however, these changes were not statistically significant (P = 0.44) [27]. Caution should be taken in interpreting these results because the follow-up time of 3 months was relatively short.
Postoperative VH, which had been reported to happen in 12–40% vitrectomized PDR patients, will hinder monitoring of disease course and require additional application of laser treatment, therefore delaying visual rehabilitation. The risk factors of postoperative VH include younger age, later detection of DM, poor diabetic and hypertension control, higher serum creatinine, broader area of active neovascularization, increased extent of membrane peeling, postoperative hypotony, postoperative residual neovascularization membrane, unrelieved vitreous retinal contraction and insufficient PRP [28, 29]. PRP plays a protective role in disease progression and surgical difficulty of PDR [30]. We also observed a trend of less intraoperative bleeding and fibrovascular proliferation in eyes treated with retinal photocoagulation before surgery. In our study, baseline characters including age, type and duration of DM, HbA1c, VAG grading and patient proportion with previous PRP was comparative between two groups, and PRP was performed or completed in all eyes during vitrectomies, which were all performed by one surgeon to minimize the selective bias and surgery heterogeneity. Although intraoperative IVR would not make vitrectomy easier compared to preoperative IVR, it was expected to induce vasoconstriction of the fragile retinal vessels that were injured during surgery, which could become a bleeding focus after surgery. Ahn et al. reported 1.25 mg/0.05 ml bevacizumab injection at the end of vitrectomy showed significantly decreased VH incidence (10.8%) compared to no injection within 1 month after the surgery but this benefit disappeared at 2- and 3-month follow-ups [12]. Our study found no significant difference between intra- and preoperative IVR, but the incidences of VH within 3 months after surgery in both groups were comparable to Ahn’s report. We did not have a no injection group as control, and in our study we included silicon oil tamponade patients, which were excluded in Ahn’s study.
This study had several limitations. First, the sample size of this study was relatively small. Second, different types of diabetes may influence the postoperative results but this was not analyzed in our study. Third, the follow-up period of 3 months was relative short. Furthermore, as a single-center study, the generalizability of the conclusion of this study has yet to be confirmed. Future studies with larger sample size, longer observation period and multi-center participation are needed to confirm the findings of this study.
Conclusion
Compared to intraoperative IVR, preoperative IVR can significantly reduce surgery time and lower the incidence of intraoperative bleeding, intraocular electrocoagulation use, iatrogenic retinal breaks, relaxing retinotomy as well as silicone oil tamponade during surgery. Preoperative IVR can gain better postoperative BCVA and thinner CRT in a short time after surgery for PDR.
References
Yang W, Lu J, Weng J, Jia W, Ji L, Ji Q, Xiao J, Shan G, Shan Z, Liu J, Tian H, Zhu D, Ge J, Lin L, Chen L, Guo X, Zhao Z, Li Q, Zhou Z, He J, China National D, Metabolic Disorders Study G. Prevalence of diabetes among men and women in China. New Engl J Med. 2010;362:1090–101. https://doi.org/10.1056/NEJMoa0908292.
Tseng VL, Greenberg PB, Scott IU, Anderson KL. Compliance with the American academy of ophthalmology preferred practice pattern for diabetic retinopathy in a resident ophthalmology clinic. Retina (Philadelphia, Pa). 2010;30:787–94. https://doi.org/10.1097/IAE.0b013e3181cd47a2.
Bressler SB, Qin H, Melia M, Bressler NM, Beck RW, Chan CK, Grover S, Miller DG, Diabetic Retinopathy Clinical Research N. Exploratory analysis of the effect of intravitreal ranibizumab or triamcinolone on worsening of diabetic retinopathy in a randomized clinical trial. JAMA Ophthalmol. 2013;131:1033–40. https://doi.org/10.1001/jamaophthalmol.2013.4154.
Ehrlich R, Harris A, Ciulla TA, Kheradiya N, Winston DM, Wirostko B. Diabetic macular oedema: physical, physiological and molecular factors contribute to this pathological process. Acta Ophthalmol (Oxford, Engl). 2010;88:279–91. https://doi.org/10.1111/j.1755-3768.2008.01501.x.
Wang X, Wang G, Wang Y. Intravitreous vascular endothelial growth factor and hypoxia-inducible factor 1a in patients with proliferative diabetic retinopathy. Am J Ophthalmol. 2009;148:883–9. https://doi.org/10.1016/j.ajo.2009.07.007.
Ferenchak K, Duval R, Cohen JA, MacCumber MW. Intravitreal bevacizumab for postoperative recurrent vitreous hemorrhage after vitrectomy for proliferative diabetic retinopathy. Retina (Philadelphia, Pa). 2014;34:1177–81. https://doi.org/10.1097/IAE.0000000000000058.
Comyn O, Wickham L, Charteris DG, Sullivan PM, Ezra E, Gregor Z, Aylward GW, Da Cruz L, Fabinyi D, Peto T, Restori M, Xing W, Bunce C, Hykin PG, Bainbridge JW. Ranibizumab pretreatment in diabetic vitrectomy: a pilot randomised controlled trial (the RaDiVit study). Eye (Lond). 2017;31:1253–8. https://doi.org/10.1038/eye.2017.75.
Simunovic MP, Maberley DAL. Anti-vascular endothelial growth factor therapy for proliferative diabetic retinopathy a systematic review and meta-analysis. Retina (Philadelphia, Pa). 2015;35:1931–42. https://doi.org/10.1097/IAE.0000000000000723.
di Lauro R, De Ruggiero P, di Lauro R, di Lauro MT, Romano MR. Intravitreal bevacizumab for surgical treatment of severe proliferative diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol. 2010;248:785–91. https://doi.org/10.1007/s00417-010-1303-3.
Ren X, Bu S, Zhang X, Jiang Y, Tan L, Zhang H, Li X. Safety and efficacy of intravitreal conbercept injection after vitrectomy for the treatment of proliferative diabetic retinopathy. Eye (Lond). 2019;33:1177–83. https://doi.org/10.1038/s41433-019-0396-0.
Rosenfeld PJ, Durbin MK, Roisman L, Zheng F, Miller A, Robbins G, Schaal KB, Gregori G. ZEISS Angioplex™ spectral domain optical coherence tomography angiography: technical aspects. Dev Ophthalmol. 2016;56:18.
Ahn J, Woo SJ, Chung H, Park KH. The effect of adjunctive intravitreal bevacizumab for preventing postvitrectomy hemorrhage in proliferative diabetic retinopathy. Ophthalmology. 2011;118:2218–26. https://doi.org/10.1016/j.ophtha.2011.03.036.
Suzuki Y, Suzuki K, Yokoi Y, Miyagawa Y, Metoki T, Nakazawa M. Effects of intravitreal injection of bevacizumab on inflammatory cytokines in the vitreous with proliferative diabetic retinopathy. Retina (Philadelphia, Pa). 2014;34:165–71. https://doi.org/10.1097/IAE.0b013e3182979df6.
Cheung NMD, Mitchell PP, Wong TYP. Diabetic retinopathy. Lancet (Brit edn). 2010;376:124–36. https://doi.org/10.1016/S0140-6736(09)62124-3.
Kohno R-I, Hata Y, Mochizuki Y, Arita R, Kawahara S, Kita T, Miyazaki M, Hisatomi T, Ikeda Y, Aiello LP, Ishibashi T. Histopathology of neovascular tissue from eyes with proliferative diabetic retinopathy after intravitreal bevacizumab injection. Am J Ophthalmol. 2010;150:223-229.e221. https://doi.org/10.1016/j.ajo.2010.03.016.
Chen L, Qu L, Gui Q, Wang S, Mao J, Fu X, Li W, Wang Y, Yi Q. Effects of anti-vascular endothelial growth factor drugs before and after pars plana vitrectomy in patients with polypoidal choroidal vasculopathy and vitreous hemorrhage. J Ocular Pharmacol Therap. 2021;37:591–6. https://doi.org/10.1089/jop.2021.0039.
Niwa Y, Kakinoki M, Sawada T, Wang X, Ohji M. Ranibizumab and aflibercept: intraocular pharmacokinetics and their effects on aqueous vegf level in vitrectomized and nonvitrectomized macaque eyes. Invest Ophthalmol Vis Sci. 2015;56:6501–5. https://doi.org/10.1167/iovs.15-17279.
Christoforidis JB, Williams MM, Wang J, Jiang A, Pratt C, Abdel-Rasoul M, Hinkle GH, Knopp MV. Anatomic and pharmacokinetic properties of intravitreal bevacizumab and ranibizumab after vitrectomy and lensectomy. Retina (Philadelphia, Pa). 2013;33:946–52. https://doi.org/10.1097/IAE.0b013e3182753b12.
Kakinoki M, Sawada O, Sawada T, Saishin Y, Kawamura H, Ohji M. Effect of vitrectomy on aqueous VEGF concentration and pharmacokinetics of bevacizumab in macaque monkeys. Invest Ophthalmol Vis Sci. 2012;53:5877–80. https://doi.org/10.1167/iovs.12-10164.
Chin HS, Park TS, Moon YS, Oh JH. Difference in clearance of intravitreal triamcinolone acetonide between vitrectomized and nonvitrectomized eyes. Retina. 2005;25:556–60. https://doi.org/10.1097/00006982-200507000-00002.
Krohne TU, Liu Z, Holz FG, Meyer CH. Intraocular pharmacokinetics of ranibizumab following a single intravitreal injection in humans. Am J Ophthalmol. 2012;154:682-686.e682. https://doi.org/10.1016/j.ajo.2012.03.047.
Bressler SBSB, Melia MM, Glassman ARAR, Almukhtar TT, Jampol LMLM, Shami MM, Berger BBBB, Bressler NMNM. Ranibizumab plus prompt or deferred laser for diabetic macular edema in eyes with vitrectomy prior to anti-vascular endothelial growth factor therapy. Retina (Philadelphia, Pa). 2015;35:2516–28. https://doi.org/10.1097/IAE.0000000000000617.
Chen Y-Y, Chen P-Y, Chen F-T, Chen Y-J, Wang J-K. Comparison of efficacy of intravitreal ranibizumab between non-vitrectomized and vitrectomized eyes with diabetic macular edema. Int Ophthalmol. 2017;38:293–9. https://doi.org/10.1007/s10792-017-0462-1.
Koyanagi Y, Yoshida S, Kobayashi Y, Kubo Y, Yamaguchi M, Nakama T, Nakao S, Ikeda Y, Ohshima Y, Ishibashi T, Sonoda K-h. Comparison of the effectiveness of intravitreal ranibizumab for diabetic macular edema in vitrectomized and nonvitrectomized eyes. Ophthalmologica (Basel). 2016;236:67–73. https://doi.org/10.1159/000446992.
Rabina G, Azem N, Barequet D, Barak A, Loewenstein A, Schwartz S. Silicone oil tamponade effect on macular layer thickness and visual acuity. Retina (Philadelphia, Pa). 2020;40:998–1004. https://doi.org/10.1097/IAE.0000000000002464.
Caramoy A, Droege KM, Kirchhof B, Fauser S. Retinal layers measurements in healthy eyes and in eyes receiving silicone oil-based endotamponade. Acta Ophthalmol (Oxford, Engl). 2014;92:e292–7. https://doi.org/10.1111/aos.12307.
Kheir WJ, Mehanna C-J, Koaik M, Bashshur Z. Macular changes on optical coherence tomography before, during, and after silicone oil tamponade for macula-on retinal detachment: a case series. J Vitreo Retinal Dis. 2018;2:297–301. https://doi.org/10.1177/2474126418785538.
Ding Y, Yao B, Hang H, Ye H. Multiple factors in the prediction of risk of recurrent vitreous haemorrhage after sutureless vitrectomy for non-clearing vitreous haemorrhage in patients with diabetic retinopathy. BMC Ophthalmol. 2020;20:292. https://doi.org/10.1186/s12886-020-01532-8.
Kameda Y, Saeki T, Hanai K, Suzuki Y, Uchigata Y, Babazono T, Kitano S. Is chronic kidney disease affecting the postoperative complications of vitrectomy for proliferative diabetic retinopathy? J Clin Med. 2021. https://doi.org/10.3390/jcm10225309.
Gonzalez VH, Wang P-w, Ruiz CQ. Panretinal photocoagulation for diabetic retinopathy in the RIDE and RISE trials: not “1 and done.” Ophthalmology (Rochester, Minn). 2021;128:1448–57. https://doi.org/10.1016/j.ophtha.2019.08.010.
Acknowledgements
Funding
This study was funded by the Capital Clinical Diagnosis and Treatment Technology Research and Demonstration Application Project of China (grant: Z191100006619029) and the National Key R&D Program of China (no. 2020YFC2008200). The study sponsors also funded the journal’s Rapid Service Fee.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole and have given their approval for this version to be published.
Author Contributions
Concept and design: Siying Li; Methodology: Zongyi Wang; Data collection: Linqi Zhang; Statistical analysis: Jiyang Tang; Drafting the manuscript: Siying Li; Preparing figures: Xinyao Han; Supervision: Jinfeng Qu.
Disclosures
Siying Li, Jiyang Tang, Xinyao Han, Zongyi Wang, Linqi Zhang, and JinFeng Qu declare that they have no competing interests.
Compliance with Ethics Guidelines
This study was approved by Human Ethics Committee/Institutional Review Board of Peking University People’s Hospital (2021PHB405-001). All procedures adhered to the tenets of the Declaration of Helsinki of 1964 and its later amendments. All participants provided informed consent before surgery, and informed consent for publication was obtained from all participants.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Li, S., Tang, J., Han, X. et al. Prospective Comparison of Surgery Outcome Between Preoperative and Intraoperative Intravitreal Injection of Ranibizumab for Vitrectomy in Proliferative Diabetic Retinopathy Patients. Ophthalmol Ther 11, 1833–1845 (2022). https://doi.org/10.1007/s40123-022-00550-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00550-7