Abstract
Purpose
To investigate the precision and accuracy of IOP measurements using a pneumatonometer and a tonometer tip cover (Tono-Pen® tip cover) acting as a membrane between a cadaver eye model and pneumatonometer probe.
Methods
A total of 480 paired IOP measurements, with and without a Tono-Pen cover, were collected across 4 pressure levels of 7, 10, 20 and 30 mmHg. IOP measurements were obtained by three different pneumatonometer units paired with three different masked operators (three configurations). Four eyes were sampled for each eye pressure level. The sequence of eye pressure, configuration, and measurements with vs. without the Tono-Pen cover was randomized.
Results
With the Tono-Pen cover in place, there was a negative bias with a mean IOP difference of − 1.18 mmHg for all 480 paired samples compared with the measurements absent the cover. Compared with the test pressure settings (i.e., 7, 10, 20, 30 mmHg), the overall mean bias was + 0.35 mmHg with the Tono-Pen cover present. With the Tono-Pen cover present, the overall repeatability %CV (percent coefficient of variation) was 3.4% and the reproducibility %CV was 3.8% compared with a repeatability %CV of 3.2% and reproducibility %CV of 5.7% without the Tono-Pen cover.
Conclusion
Measurement of IOP via pneumatonometry with a Tono-Pen cover in place, also known as the excursion test method, yields precise, accurate and reproducible results. This developed method of pressure measurement is an acceptable and reliable form of IOP measurement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The excursion test method is a developed method of IOP measurement with pneumatonometry and a Tono-Pen cover gently touching the surface of the cornea. |
This method of IOP measurement was developed to work in concert with the Excursion multi-pressure dial, a modified version of the multi-pressure dial. |
The Excursion multi-pressure dial contains an access port within the lens of the goggles to allow pneumatonometry measurements while negative pressure is active without breaching the sealed environment. |
The excursion test method is a reliable and precise form of IOP measurement. |
Introduction
Open-angle glaucoma (OAG) is a leading cause of vision loss worldwide, and intraocular pressure (IOP) remains the only clinically validated, modifiable risk factor [1, 2]. Although glaucoma occurs at any level of IOP, elevated IOP is a significant risk factor, and strategies aimed at IOP reduction remain the foundation of treatment [1]. Despite the recent emergence of new medical and surgical options [3,4,5], current treatment options remain imperfect, and novel treatment strategies are desirable.
Recently, a non-drug, non-laser and non-surgical device has been introduced, known as the Multi-Pressure Dial, or MPD (Equinox Ophthalmic, Inc., CA, USA). The MPD consists of a pair of goggles that individually encloses each eye connected to a regulated vacuum capable of delivering a titratable level of negative pressure to the anterior globe. It is proposed that the device reduces IOP via application of negative pressure to the anterior microenvironment around the eye, and clinical studies have demonstrated the short- and long-term safety of the device [6, 7].
The negative pressure environment manufactured by the MPD is dependent on a sealed environment. Because of this, traditional methods to measure IOP while the MPD device is active with negative pressure are not plausible. To obtain an IOP measurement, a modified MPD system was created known as the Excursion MPD, which consists of an access port in the lens of the goggles to permit measurements with a Reichert Model 30® pneumatonometer. In addition, an Automated Ophthalmics Softips® Tono-Pen tip cover (in conjunction with a silicone tube frame) is placed within the port to gently contact the cornea surface while measurements are collected to maintain a seal. This modified system permits pneumatonometry measurement without breaching the sealed environment and enables IOP measurement during active negative pressure.
The goal of this study was to evaluate the precision and accuracy of the aforementioned method to measure IOP using a human anterior segment cadaver eye model; it will be denoted the “Excursion Test Method” throughout this report. More specifically, this study will evaluate the IOP measurements obtained with the Reichert Model 30 pneumatonometer through the Tono-Pen tip cover compared with pneumatonometry measurements without a Tono-Pen cover to also investigate the presence of bias with the Tono-Pen cover in place.
Methods
Study Materials
To investigate the precision and bias of the “Excursion Test Method,” the following materials were utilized:
Reichert Model 30 Pneumatonometer
Automated Ophthalmics Softips Tono-Pen Tip Cover (Tono-Pen cover)
Cadaver Eye Test Fixture
DMEM (Dulbecco’s Modified Eagle’s Medium) Column Manometer
Argon Medical Devices DTXPlus Pressure Transducer
Reference Documents
ANSI Z80.10-2014
Guidance for Industry and FDA Staff, Tonometers
Reichert, Model 30 Pneumatonometer User’s Guide
Study Design
The excursion test method of IOP measurement was developed and adapted to function with the MPD. An adapted model of the MPD, also known as the Excursion MPD, permits IOP measurements via the excursion test method to allow IOP measurements while the device is worn with active negative pressure. This study evaluates the variance and inter-observer variability in the IOP measurement method that is proposed when the Excursion MPD is worn and active negative pressure is applied.
The Excursion MPD, a modified version of the MPD, contains a 0.6″ diameter opening in each lens that creates an access port through which a pneumatonometer tip can safely be inserted. The 0.6″ diameter access port permits placement of an access cartridge that consists of a Tono-Pen cover with a silicone support tube. To maintain a sealed environment, the cartridge is placed and secured within the access port with the proximal end (containing the Tono-Pen cover) gently contacting the cornea. Through the open, distal end of the access port, the tip of the pneumatonometer is inserted and placed against the Tono-Pen cover on the cornea to measure IOP. Notably, this utilization of the Tono-Pen tip cover is comparable to its use with the FDA-approved Tono-Pen (Reichert Inc., Buffalo, NY, USA). An image of the Excursion MPD with the cartridge in place and pneumatonometer placed through the access port is shown in Fig. 1. A photo of the standard MPD is demonstrated in Fig. 2.
To test the accuracy and precision of this method of IOP measurement, a human anterior segment cadaver eye model was utilized to compare measurements with and without the Tono-Pen cover. Human eyes were obtained from the Minnesota Lion’s Eye Bank, dissected and placed in a modified Petri dish as previously described [8]. Cultured eyes were set to pre-determined pressures of 7, 10, 20 and 30 mmHg using a column manometer filled with Dulbecco’s Modified Eagle’s Medium (DMEM). These pressure settings were chosen to assess the clinically common IOP range of 7–30 mmHg, which is consistent with the IOP range categories in the ANSI guidelines (American National Standards Institute Z80.10—“Ophthalmic Instruments—Tonometers”). To modify the pressure setting, the DMEM level was raised or lowered in the manometer. Prior to pressure measurement via pneumatonometry, the actual pressure of the cadaver eye model was recorded. Operators trained on the use of pneumatonometry collected measurements at each eye pressure setting.
Three masked operators collected pressure measurements using three independent Model 30 pneumatonometers (paired combination of Model 30 and operator). Four eyes were measured with each configuration (1, 2, 3) at each of the four pressure settings: 7, 10, 20 and 30 mmHg; ten IOP measurements were obtained for each eye. IOP measurements obtained via the Model 30 pneumatonometer were collected in the “manual tonometry” mode, which displays the average and standard deviation of 40 readings per second for each successful measurement. The configurations, sequence of eye pressure levels (ranging from 7 to 30 mmHg) and use of Tono-Pen cover were randomly generated prior to collecting data and provided as a test matrix prior to the start of testing.
In the study protocol, to prevent bias from the individual (operator) performing the pneumatonometry readings, a reader, independent from the operators, modified test settings and recorded the IOP levels as measured by the pneumatonometer. Data were collected according to specified requirements put forth by ANSI including evaluation of IOP measurements with the excursion test method and followed tolerance levels (± 5 mmHg) between the test and reference tonometer in specified ranges of IOP. Notably, the pneumatonometer was used in “manual tonometry” mode, and values were not collected until usable measurements were available (e.g., standard deviation between readings < 1.0 mmHg for 3 s). Operators trained in the use of the pneumatonometer collected paired readings at each IOP level; the operator was masked to the IOP pressure levels with the pneumatonometer facing opposite the operator performing measurements. For the study, three different operators were used yielding a collective total of 480 measurements (120 measurements at each IOP setting). The protocol with the clearly defined roles of the proctor/operator is shown in detail in Table 1.
All procedures conducted were in accordance with the Aspire IRB and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Human eyes were obtained from the Minnesota Lion’s Eye Bank. For eyes obtained through the eye bank, Minnesota Lion’s Eye Bank received written consent from family to use eyes for research purposes.
Statistical Analysis
Analysis was conducted to determine accuracy and precision with and without the Tono-Pen cover in place on measures of IOP in a cadaver eye model. The study included three operators at three known pressure settings. For each IOP setting, the measurements with and without the Tono-Pen cover were summarized by the mean, estimated bias against the eye pressure setting level (i.e., observed mean IOP measurement—determined eye pressure setting level), standard deviation (SD), and minimum and maximum.
To evaluate variance components including the reproducibility and repeatability, the study was designed as a two-way random effects model. The two-way random effects model is shown below:
The two-way random effects model is \({\text{Y}}_{ijk} = + {\text{E}}_{i} + {\text{C}}_{j} + {\text{EC}}_{ij} +_{ijk}\) where
\(Y_{ijk}\) is the kth measurement from the ith eye and jth operator,
\(E_{i}\) is the effect of the ith eye (four for the study),
\(C_{j}\) is the effect of the jth operator (three for the study),
\(EC_{ij}\) is the effect of the interaction of \(E_{i}\) and \(C_{j}\),
\(\varepsilon_{ijk}\) is the error of the \(k{\text{th}}\) replicate measurement (ten for the study) from the ith eye and jth observer.
The estimates of the variance components for the model are (equation set 1):
For the study eyes, \({\text{VarComp}}\left( E \right) = \frac{{{\text{MS}}_{\text{E}} - {\text{MS}}_{\text{EC}} }}{{n_{\text{C}} n_{\text{Reps}} }}\)
For the study operators, \({\text{VarComp}}\left( C \right) = \frac{{{\text{MS}}_{\text{C}} - {\text{MS}}_{\text{EC}} }}{{n_{\text{E}} n_{\text{Reps}} }}\)
For the interaction, \({\text{VarComp}}\left( {\text{EC}} \right) = \frac{{{\text{MS}}_{\text{EC}} - {\text{MS}}_{\varepsilon } }}{{n_{\text{Reps}} }}\)
For the error, \({\text{VarComp}}\left( \varepsilon \right) = {\text{MS}}_{\varepsilon }\)
Repeatability and reproducibility for the study are calculated by (equation set 2):
\({\text{Repeatability}} = {\text{VarComp}}\left( \varepsilon \right)\)
\({\text{Reproducibility}} = {\text{VarComp}}\left( C \right) + {\text{VarComp}}\left( {\text{EC}} \right)\)
Intraclass correlation coefficient for observers (for consistency, two-way random model with multiple observers and measurements) is calculated by (equation set 3):
\({\text{ICC}} = \frac{{{\text{MS}}_{\text{E}} - {\text{MS}}_{\varepsilon } }}{{{\text{MS}}_{\text{E}} + \left( {{\text{MS}}_{\text{C}} - {\text{MS}}_{\varepsilon } } \right)/n_{\text{E}} }}\)
The variance components above were used to calculate ICC, repeatability and reproducibility. The standard deviation of repeatability and reproducibility were calculated using the square root of equation set 2. The standard deviation for repeatability is the expected standard deviation of results of multiple measurements of any one operator on a unique eye. The limit for repeatability is the expected absolute difference between two subsequent measures by the same observer. The standard deviation for reproducibility is the expected standard deviation for multiple observers on a unique eye. The limit for reproducibility is the expected absolute difference when multiple observers measure the same eye. Percent coefficient of variance is the standard deviation normalized to the mean and used to compare standard deviation where mean values vary.
Results
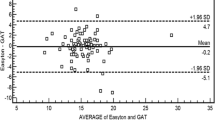
A total of 480 paired pressure readings were collected with and without the Tono-Pen cover by three independent operators at 7, 10, 20 and 30 mmHg. At 7 mmHg, the mean IOP with the Tono-Pen cover was 8.9 ± 1.0 mmHg and without the Tono-Pen cover was 10.6 ± 1.2 mmHg, indicating a mean difference of − 1.7 ± 01.3 mmHg. At 10 mmHg pressure, the mean IOPs with and without the Tono-Pen cover present were 11.1 ± 1.7 and 12.6 ± 1.3 mmHg, respectively. At this pressure setting, the mean difference was − 1.5 ± 1.3 mmHg. At 20 mmHg, the mean IOP measurement with the Tono-Pen cover was 20.2 ± 0.9 mmHg, while the mean IOP without the cover was 21.0 ± 1.2, resulting in a mean difference of − 0.9 ± 0.9 mmHg. At the 30 mmHg IOP setting, the mean IOP with the Tono-Pen cover was 28.2 ± 0.9 mmHg and without the Tono-Pen cover was 28.9 ± 1.7 mmHg. The mean difference at 30 mmHg was − 0.7 ± 1.3 mmHg. Table 2 compares the mean IOP values at each setting, and Fig. 3 demonstrates the agreement between measurements with and without the Tono-Pen cover using the Bland-Altman plot.
Compared with the pressure established by the DMEM column manometer (i.e., 7, 10, 20, 30 mmHg), the measurements with the Tono-Pen cover demonstrated a slightly positive bias at 7 mmHg, 10 mmHg and 20 mmHg with the mean IOP measured at 8.9 ± 1.0 mmHg, 11.1 ± 1.7 mmHg and 20.2 ± 0.9 mmHg. At the 30 mmHg setting, there was a small negative bias (− 1.8 mmHg), and the mean IOP measurement was 28.2 ± 0.9 mmHg. All 480 measurements were within ± 5 mmHg of the established test IOP setting at 7, 10, 20 and 30 mmHg. A summary of these values is shown in Table 3.
The intraclass correlation coefficient (ICC) was calculated to estimate the degree by which any given operator would agree with any other operator. Across the range of pressure settings with and without the Tono-Pen cover, the ICC was favorable with ICC values > 0.75 at all settings except the 20 mmHg pressure setting with the Tono-Pen cover in place (0.69). At all pressure settings, there was not a significant difference in ICC between the measurements with and without the Tono-Pen cover. These values are shown in Table 4.
Repeatability and Reproducibility
The summary of these analyses is shown in Table 4. For repeatability, the coefficient of variation (%CV) with the Tono-Pen cover in place at 7 mmHg was 5.0%. At 10, 20 and 30 mmHg, the repeatability %CV was 4.4%, 2.1% and 2.0%, respectively. Without the Tono-Pen cover in place, the repeatability %CV was 4.5% at 7 mmHg and 3.4% at 10 mmHg. At 20 and 30 mmHg, the %CV values were 2.7% and 2.4%, respectively. The standard deviation and limit for reproducibility were also calculated and are shown for comparison in Table 4.
For reproducibility, the %CV with the Tono-Pen cover was 6.0% at 7 mmHg and 4.9% at 10 mmHg. Similar to the repeatability measurements, the %CV was lower at 20 and 30 mmHg with values of 2.9% and 1.4%, respectively. With the Tono-Pen cover in place, the %CV was 5.8% (7 mmHg), 6.7% (10 mmHg), 4.2% (20 mmHg) and 6.2% (30 mmHg).
Discussion
The treatment of OAG remains a challenge for patients and physicians alike, largely because patients still progress despite achieving a “target” or “goal” IOP [9]. Novel techniques and devices are coveted by providers for IOP reduction and treatment, particularly those that are titratable and non-invasive. The MPD is a novel treatment device capable of transient, instantaneous IOP reduction while the device is worn with active negative pressure application [7]. It has tremendous potential for individualized treatment including titration of negative pressure to “dial in” a target IOP on demand. However, its unique mechanism prohibits measurement of IOP with traditional methods (e.g., Goldmann applanation, iCare, etc.) while the device is active because it requires a sealed environment to maintain its negative pressure microenvironment. Thus, this study aimed to evaluate a new technique for IOP measurement.
Early clinical data highlight the short- and long-term safety of the MPD [6, 7]. Additionally, a presentation by Swan et al. described the IOP-lowering capability of the MPD utilizing a modified MPD referred to as the Excursion MPD device, a specially adapted version of the goggles that allows pneumatonometry measurements during negative pressure (Fig. 3). These measurements were obtained using a technique akin to what was evaluated in the current study. Because a reliable and precise estimation of IOP is imperative for glaucoma patients and the measurement technique from the aforementioned report by Swan et al. is new, this present report aimed to evaluate the presence of bias and precision with this technique (excursion test method) and the impact of the Tono-Pen cover on measurements.
In this report, three different individuals (operators) collected IOP measurements at randomized test IOP settings with and without the Tono-Pen cover in place on four individual eyes. For all pressure settings with the Tono-Pen cover in place, denoted as the excursion test method, the results demonstrated a small positive bias of +0.4 mmHg, highlighting the accuracy of this mode of IOP measurement. At the extremes of the test pressure settings (7, 30 mmHg), the bias was greater with a positive bias of +1.9 mmHg at 7 mmHg and –1.8 mmHg at 30 mmHg; these results suggest the measurements may be more reliable in eyes with 10–20 mmHg, which closely approximates the normal range of IOP [10]. Overall, 100% of the measurements were within ± 5 mmHg of the established test pressure setting; both samples were within the guidelines for agreement within ± 5 mmHg at a 95% confidence interval. These results highlight the accuracy of this method of IOP measurement.
The precision results were favorable for all measurements, particularly with the Tono-Pen cover in place during data collection, which represents the excursion test method. Overall, there was a small negative bias with the Tono-Pen cover in place compared with measurements sans the Tono-Pen cover. For repeatability, the CV values were < 5% at all pressure settings with and without the Tono-Pen cover in place. In addition, the repeatability SD was < 0.7 at all test pressure settings, and the difference in repeatability SD was not significantly different at all pressure settings. For reproducibility, with the Tono-Pen cover in place, variation due to reproducibility was stable across the pressure settings with %CV values ranging from 1.4% to 6.0% and the mean %CV across all settings 3.8%. In addition, the reproducibility standard deviation was < 0.6 at all pressure settings with the cover in place. Without the Tono-Pen cover, there was slightly more variation with respect to reproducibility with %CV values > 4% at all pressure settings ranging from 4.2% to 6.7% with the overall mean 5.7% and the reproducibility SD ranging from 0.7 mmHg to 1.8 mmHg. Compared with established methods—Goldmann applanation tonometry (GAT), ocular response analyzer (ORA), dynamic contour tonometry (DCT)—the repeatability and reproducibility values in this study were favorable. In a study evaluating the precision of the three aforementioned methods by Wang et al. [11], the repeatability CV values were > 9% for both ORA and GAT while the DCT repeatability values were similar to those of this study with 3.7%. For reproducibility, GAT, ORA and DCT all had CV values > 6% while the excursion test method in this study had a CV value of 3.8%. These results favor the repeatability of this method as CV values < 5% are indicative of excellent repeatability results [12].
This study is not without limitations. The human anterior segment cadaver eye model is a well-studied and established model for laboratory investigation but may not translate exactly to how a real cornea with specific morphologic features (thickness, curvature) and biomechanical properties would behave with the pneumatonometer and the Tono-Pen cover present. In addition, given that this method of IOP measurement has not been previously described, it remains unclear whether bias and precision would improve over time with user experience. Moreover, it is well known that biomechanical properties of the cornea may affect IOP measurements but these parameters were not collected in this study. However, despite these limitations, this study yielded favorable results with minor bias and excellent precision and accuracy.
Conclusion
This study supports the reproducibility and repeatability of a new method of IOP measurement known as the excursion test method. Importantly, the Tono-Pen cover had minimal impact on pressure measurements and did not introduce a significant amount of bias at any IOP test setting. The excursion test method has clinical relevance as it permits IOP measurements with the MPD, a device with a novel mechanism for IOP reduction that represents a new approach to treatment of glaucoma. The favorable results of this study indicate the excursion test method is an acceptable and reliable method of IOP measurement.
References
Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002;120(10):1268–79.
Kingman S. Glaucoma is second leading cause of blindness globally. Bull World Health Organ. 2004;82:887–8. https://doi.org/10.1590/S0042-96862004001100019.
Weinreb RN, Ong T, Sforzolini BS, Vittitow JL, Singh K, Kaufman PL. A randomised, controlled comparison of latanoprostene bunod and latanoprost 0.005% in the treatment of ocular hypertension and open angle glaucoma: the VOYAGER study. Br J Ophthalmol. 2014. https://doi.org/10.1136/bjophthalmol-2014-305908.
Lavia C, Dallorto L, Maule M, Ceccarelli M, Fea AM. Minimally-invasive glaucoma surgeries (MIGS) for open angle glaucoma: a systematic review and meta-analysis. PLoS One. 2017;12(8):e0183142. https://doi.org/10.1371/journal.pone.0183142.
Shah M. Micro-invasive glaucoma surgery—an interventional glaucoma revolution. Eye Vis Lond Engl. 2019;6(1):29. https://doi.org/10.1186/s40662-019-0154-1.
Samuelson TW, Ferguson TJ, Radcliffe NM, et al. 8 hrs safety evaluation of a multi-pressure dial in eyes with glaucoma: prospective, open-label, randomized study. Clin Ophthalmol Auckl NZ. 2019;13:1947–53. https://doi.org/10.2147/OPTH.S217736.
Thompson VM, Ferguson TJ, Ahmed IIK, et al. Short-term safety evaluation of a multi-pressure dial: a prospective, open-label, non-randomized study. Ophthalmol Ther. 2019;82(11):887–9. https://doi.org/10.1007/s40123-019-0181-y.
Bahler CK, Fautsch MP, Hann CR, Johnson DH. Factors influencing intraocular pressure in cultured human anterior segments. Investig Opthalmol Vis Sci. 2004;45(9):3137. https://doi.org/10.1167/iovs.04-0154.
Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol. 2003;121(1):48–56. https://doi.org/10.1001/archopht.121.1.48.
Berdahl JP, Allingham RR, Johnson DH. Cerebrospinal fluid pressure is decreased in primary open-angle glaucoma. Ophthalmology. 2008;115(5):763–8. https://doi.org/10.1016/j.ophtha.2008.01.013.
Wang AS, Alencar LM, Weinreb RN, et al. Repeatability and reproducibility of Goldmann applanation, dynamic contour, and ocular response analyzer tonometry. J Glaucoma. 2013;22(2):127–32. https://doi.org/10.1097/IJG.0b013e3182254ba3.
Fujimura F, Kamiya K, Fujiwara K, Shoji N, Shimizu K. Repeatability and reproducibility of measurements using a NT-530P noncontact tono/pachymeter and correlation of central corneal thickness with intraocular pressure. Biomed Res Int. 2013;2013:1–5. https://doi.org/10.1155/2013/370592.
Acknowledgements
We thank the operators who performed the tasks described in this study to generate the data and study results.
Funding
The study and the rapid service fee for this publication were funded by Equinox Ophthalmic, Inc. There were no other funding sources.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Drs. Tanner J. Ferguson, Russell J. Swan and Michael Greenwood are consultants for Equinox Ophthalmic, Inc. Dr. John P. Berdahl is the founder and CEO of Equinox Ophthalmic, Inc. Mr. Richard Gorham, Ms. Catherine G. Knier, Ms. Kjerseten J. Monson, Dr Uttio Roy Chowdhury and Dr Michael P. Fautsch have no relevant financial disclosures.
Compliance with Ethics Guidelines
All procedures conducted were in accordance with the Aspire IRB and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Human eyes were obtained from the Minnesota Lion’s Eye Bank. For eyes obtained through the eye bank, Minnesota Lion’s Eye Bank received written consent from family to use eyes for research purposes.
Data Availability
The data set collected and analyzed for this present study is available from the corresponding author per reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.11771016.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/
About this article
Cite this article
Ferguson, T.J., Knier, C.G., Chowdhury, U.R. et al. Intraocular Pressure Measurement with Pneumatonometry and a Tonometer Tip Cover. Ophthalmol Ther 9, 127–137 (2020). https://doi.org/10.1007/s40123-020-00235-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-020-00235-z