Abstract
Introduction
Fibromyalgia is a form of chronic pain that affects a large number of women. It can start at any age and last a lifetime, with no cure. The Mediterranean diet is said to have an anti-inflammatory effect. Therefore, this study was conducted to investigate possible beneficial effects of a personalized Mediterranean diet in patients with fibromyalgia.
Methods
Outpatients with fibromyalgia were recruited and invited to participate in the study, including clinical, nutritional, and dietary assessments. Patients received a personalized Mediterranean diet (DIET group) or a general balanced diet (NODIET group) to be followed for 8 weeks. All tests were carried out at baseline and repeated after 4 and 8 weeks.
Results
In total, 100 subjects were included, 84 of whom completed the study. Most of the patients showed incorrect habits in terms of food choices, timing of meals and composition of nutrients. The DIET group showed an improvement in most of the fibromyalgia parameters, including the disability scores, fatigue, and anxiety.
Conclusions
The habit of eating inflammatory foods and/or eating meals with the wrong nutritional content would increase the negative status of patients with fibromyalgia. With this study, we confirm that proper attention to feeding habits would improve the quality of life of such patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Fibromyalgia is a disabling disorder without effective pharmacological remedies. |
Nutrition could act on pain and reduce inflammation. |
In total, 39 patients with fibromyalgia were prescribed a personalized Mediterranean diet (DIET group), while 42 patients agreed to a general balanced diet (NODIET group). |
Patients who followed the Mediterranean diet showed significant improvement in fibromyalgia disability scores, as well as in anxiety and depression, 2 months after the start of the diet. |
Since incorrect eating habits could be a cause of fibromyalgia, the Mediterranean diet could have a positive effect owing to its anti-inflammatory actions. |
Introduction
Fibromyalgia (FM) is a disabling pathology that still does not respond adequately to pharmacological agents [1]. It meets the requirements of nociplastic pain, a condition in which central sensitization associated with central synaptic remodeling persists [2].
Among the causes unrelated to the specific causes of central sensitization is inflammation [3]. Inflammation consists of a dynamic sequence of phenomena manifested in an intense vascular response and, above all, the release of endogenous substances: the chemical mediators of inflammation [4].
Diet can cause inflammation. Inflammatory conditions of the digestive system can trigger the release of cytokines, which can have effects on the central nervous system [5]. In particular, tumor necrosis factor-alpha (TNF-α), interleukin-1β (IL-1β), and interleukin-6 (IL-6) are proinflammatory cytokines and also mediators of chronic pain. Following an inflammatory state, changes in intestinal permeability can also be seen with loosening of tight junctions and passage of harmful substances/toxins into the circulation. Dietary interventions are used to treat many diseases, as a healthy diet improves physical fitness, mental health and cognitive abilities [6]. Currently, there is limited evidence for the effect of specific diets in FM [7].
In a recent meta-analysis [8], only two studies on the Mediterranean diet in musculoskeletal pain, particularly in patients with rheumatoid arthritis, were reported [9, 10]. The results were encouraging and suggested a positive effect on pain, although further evidence is needed.
The aim of the present randomized controlled trial was to determine the effect of a personalized Mediterranean diet in patients with FM; a common variant was the complete exclusion of dairy products and eggs. The hypothesis was that such a diet could reduce the inflammatory processes within the FM mechanisms, leading to an improvement in the main index of FM severity.
Methods
The randomized (1:1) controlled trial was approved by the ethics committee of the General Hospital of the Aldo Moro University of Bari (approval number 7173 2022 1 22.). The patients signed an informed consent form. The study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments.
Outpatients were randomized in a 1:1 ratio to:
-
1.
A generalized balanced diet adapted to individual body mass index (BMI; NODIET group)
-
2.
A personalized Mediterranean diet (DIET group)
The inclusion criteria were: diagnosis of FM according to the 2016 American College of Rheumatology (ACR) criteria [11], which recommends the use of the widespread pain index (WPI) and the symptoms severity scale (SS); age between 18 and 65 years; and the persistence of diffuse pain and symptoms of FM despite the taking of medication in the 3 months prior to inclusion in the study. In accordance with the routine approach of our center, all patients were prescribed pharmacological treatment with antiepileptic drugs (pregabalin 150–300 mg) and antidepressants (duloxetine 60 mg) [12].
The exclusion criteria were: general medical conditions, including any form of diabetes, and all other neurological disorders that do not meet the FM criteria (including primary headaches and depression).
Participants were expected to be met three times: visit 1 (baseline), visit 2 (1-month follow-up), and visit 3 (2-month follow-up). However, since most patients in the NODIET group did not attend the last check-up after 2 months (visit 3), this was restricted to patients in the DIET group.
Personalized Mediterranean Diet
The dietary recommendations were drawn up by a team of nutritionists from the University of Siena, who assessed each case and gave each participant individualized dietary recommendations. For all subjects, the diet was assessed according to body mass index (BMI), age, and food allergies (if indicated), as suggested in the Nutrient and Energy Reference Values for the Italian Population (LARN IV Revision) [13]. Calorie intake was planned as follows: 1700 to 1900 kcal/day for patients categorized as normal weight, 1400 to 1600 kcal/day for patients categorized as overweight, and 1100 to 1300 kcal/day for patients categorized as obese.
The proposed diet consisted of five meals a day (breakfast, lunch, dinner, and two snacks) with daily adjustment (from Monday to Sunday) for 4 weeks.
The daily energy intake was divided as follows:
-
50% from complex carbohydrates with a limit of sugar and sweeteners
-
30% from fats, with an adequate intake of polyunsaturated fatty acids (PUFA), mainly from extra virgin olive oil, fish and nuts.
-
20% from proteins, ranging from 0.9 to 1.1 g/kg/die.
In addition, there was a daily intake of fiber ≥ 20 g/die from fruits, vegetables, and starchy foods.
In the DIET group, the daily intake of nutrients was based on the pattern of the Mediterranean diet [14,15,16]. The diet did not include milk and dairy products (the consumption of which is classified as “moderate” in the Mediterranean dietary pattern [17], as the likelihood of lactase enzyme deficiency and associated gastrointestinal problems was considered to be high.
Outcome Measures
Patients with FM who met the inclusion/exclusion criteria underwent clinical assessment and online contact with the Siena biological team for the diet prescription.
Patients were asked to fill in the following questionnaires:
The eating attitude test (EAT), which indicates the presence of an eating disorder [18], consists of 26 questions to which the respondent can answer: always (3), usually (2), often (1), sometimes (0), rarely (0), or never (0). If the sum is ≥ 20, an eating disorder can be suspected.
The brief pain inventory (BPI) measures both the intensity of pain and how much the pain interferes with the patient’s life. It also asks the patient about pain relief, pain quality and the patient’s perception of the cause of the pain. The BPI uses scales from 0 to 10 to rate the patient [19].
The numeric rating scale (NRS) for pain is a unidimensional measure of pain intensity in adults. The usual format is a horizontal bar or line. The NRS is a single 11-point numeric scale where 0 represents one extreme of pain (e.g., “no pain”) and 10 represents the other extreme of pain (e.g., “worst pain imaginable”).
The self-rating anxiety scale (SAS) introduced by Zung [20] is frequently used in research and clinical practice to assess anxiety. It consists of 20 questions individually scored with 1–4 points, resulting in a raw score of 20–80 points; the standard score is then calculated by int (1.25 raw score) and classified as: 25–49, no anxiety; 50–59, mild anxiety; 60–69, moderate anxiety; and 70–100, severe anxiety.
The self-rating depression scale (SDS) [21] consists of 20 questions individually scored with 1–4 points, resulting in a raw score of 20–80 points; the standard score is then calculated by int (1.25 raw score) and classified as: 25–49, no depression; 50–59, mild depression; 60–69, moderate depression; and 70–100, severe depression.
The multidimensional assessment of fatigue (MAF) scale is a self-administered survey that provides a global fatigue index. It covers four dimensions of fatigue: severity, burden, interference with activities of daily living, and frequency and change over the past week. Overall, 15 questions result in a global value [global fatigue index (GFI)]. The 16th question (“To what extent has your fatigue changed in the last week?”) does not contribute to the GFI. [22]
The fibromyalgia impact questionnaire (FIQ) is a fibromyalgia-specific outcome instrument designed to assess health status, progress and outcomes in patients with fibromyalgia. It contains ten subscales that are combined into a total score. [23].
Body mass index (BMI) was calculated from measurements of weight (using an electronic scale) and height (using a stadiometer) using the Quetelet equation [body mass (kg) / height2 (m2)] (Borga et al. 2018). The BMI data were analyzed as follows: normal weight: BMI 18–25, overweight: BMI 25–30, and obese: BMI 30 + [24].
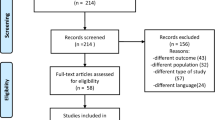
The experimental design is summarized in Fig. 1.
Statistical Analysis
Considering a 10% change in FIQ score as the primary outcome measure with a 95% confidence interval, a total population of 96 patients was required. The parametric distribution was tested using the Kolmogorov–Smirnov test. As for visit 1 and visit 2, a repeated measures analysis of variance (ANOVA) model with visits as within factor and group as between factor was used to analyze normal data. Visit 3 was not included in this analysis because the control group did not complete visit 3. Hence the DIET group was further analyzed considering the three visits. For this, a one-way repeated measures ANOVA with the factor visit (3 levels: visit 1, visit 2, and visit 3) was used. For the sake of brevity, the data from visit 3 in the DIET group are included in the figures. Statistica® software (StatSoft Inc, Tulsa, USA) was used. The statistical significance was set at p < 0.05.
Results
Of 210 consecutive patients diagnosed with FM between January 2021 and June 2022, 100 patients met the exclusion/inclusion criteria and signed the informed consent form to participate in the study (Fig. 1). Table 1 shows the demographic data (Table 1).
The eating attitude test (EAT) was administered to 52 patients. The EAT score results were 36/52 below 20 (i.e., within the normal range) and 16/52 equal to or higher than 20 (i.e., in the nonnormal range), indicating the presence of possible eating disorders in these patients. In particular, 10/36 patients from the DIET group and 6/16 patients from the NODIET group had scores above 20.
Outcome Measures
The patients who adhered to the anti-inflammatory diet (DIET group) reported significant improvements in most of the parameters of interest compared with the NODIET group, whose parameters remained stable. It should be noted that the widespread pain index (WPI), which measures the number of painful tender points, only tended to be lower in the DIET group at visit 2 compared with visit 1. This is confirmed by the one-way ANOVA applied to the three visits carried out only in the DIET group, with no significant differences among visits (Fig. 2).
Widespread pain index (WPI) determined in patients with fibromyalgia (FM) in the personalized Mediterranean diet (DIET) and general balanced diet (NODIET) groups during visit 1 and visit 2 (repeated measures ANOVA F 2.17; groups as factor: F 0.062) mean ± SEM. The comparison among the three visits for the DIET group was not significant (F 0.96)
ANOVA showed no significant differences in the symptoms severity scale (SS) values between visits in both groups, although there was a tendency for lower scores in the DIET group at visit 2 compared with visit 1.
While the WPI and SS parameters remained stable, significant effects were recorded for the other measures. ANOVA applied to all of the brief pain inventory (BPI) scale values for the two groups (DIET, NODIET) during visit 1 and visit 2 showed significance of the interaction Group × visit [disability owing to pain: F (1,75) = 4.4 p < 0.05; impairment of motor activity: F (1,75) = 5.3, p < 0.05; impairment of work activity: F (1,75) = 4.5, p < 0.05; pain intensity: F (1,74) = 5.8, p < 0.01], which in all scales can be attributed to the lower values in the DIET group at visit 2 compared with visit 1 (Fig. 3). For the global index of impairment, ANOVA revealed the significance of visit [F (1,75) = 8.1, p < 0.01].
Brief pain inventory (BPI) determined in patients with fibromyalgia (FM) in the DIET and NODIET groups during visit 1, visit 2, and visit 3 (only the DIET group). a Index of general disability due to pain; b index of pain interference in motor activity; c index of pain interference in work activities; d index of global severity of pain; e index of global disability owing to pain.
**p < 0.01.
***p < 0.001 versus visit 1 of the same group.
DIET, personalized Mediterranean diet; IAL, index of pain interference in work activities; IDB, index of general disability due to pain; IVE, index of pain interference in motor activities; NODIET, general balanced diet
The comparison of the DIET group’s values at the three visits revealed significant differences in all scales: pain-related disability [F (2,74) = 5.5, p < 0.01], impairment of motor activity [F (2,74) = 7.3 p = 0.001], impairment of work activity [F (2,74) = 7.7, p < 0.001], pain severity [F (2,72) = 6.9, p = 0.001], and global index of severity [F (2,74) = 7.8, p < 0.001]. In all cases, post-hoc analysis showed a significant reduction in scores from visit 1 to visit 2 (p < 0.01 for all) and from visit 1 to visit 3 (p < 0.05 for all; Fig. 3).
Regarding the numerical rating scale (NRS) measuring pain intensity, the comparisons of the two groups during visit 1 and visit 2 did not show significant differences between groups or between visits (p > 0.05). However, the effect became significant at visit 3, as shown by the analysis of the NRS in the DIET group [visit: F (2,74) = 3.93, p < 0.05]. This was owing to the fact that the values at visit 3 were significantly lower than at visit 1 (p < 0.01; Fig. 4).
ANOVA applied to the self-rating anxiety scale (SAS) scores during visit 1 and 2 revealed a significant interaction group × visit [F (1,75) = 10.7, p < 0.01], as the scores for the DIET group were lower at visit 2 than at visit 1 (p < 0.001) and were lower than the NODIET group at visit 2 (p < 0.05; Fig. 5a). One-way ANOVA applied to the three visits of the DIET group revealed a significant difference [F (2,74) = 17.5, p < 0.001], as the scores were lower at visit 2 and visit 3 than at visit 1 (p < 0.01; Fig. 5a).
a Self-rating anxiety scale (SAS); b self-rating depression scale (SDS) determined in patients with fibromyalgia (FM) in the personalized Mediterranean diet (DIET) and general balanced diet (NODIET) groups during visit 1, visit 2, and visit 3 (only the DIET group).
***p < 0.001 versus visit 1 of the same group,
#p < 0.05,
###p < 0.001 versus visit 2 of NODIET group. Mean ± SEM
ANOVA applied to the self-rating depression scale (SDS) scores during visit 1 and 2 revealed a significant interaction group × visit [F(1, 75) = 6.2, p = 0.01], as the scores obtained in the DIET group were lower at visit 2 than at visit 1 (p < 0.01) and were lower than the NODIET group at visit 2 (p = 0.001; Fig. 5b). One-way ANOVA applied to the three visits of the DIET group revealed a significant difference [F(2,74) = 8.3, p < 0.001], as the scores at visit 2 and visit 3 were lower than at visit 1 (p < 0.001; Fig. 5b).
ANOVA applied to the multidimensional assessment of fatigue (MAF) scores during visit 1 and 2 revealed a significant interaction group × visit [F(1, 74) = 6.8, p = 0.01], as the scores obtained in the DIET group were lower at visit 2 than at visit 1 (p < 0.01) and were lower than the NODIET group at visit 2 (p < 0.001; Fig. 6). One-way ANOVA applied to the three visits of the DIET group revealed a significant difference [F(2,74) = 4.9, p = 0.01], as the scores at visit 2 and visit 3 were lower than at visit 1 (p < 0.01; Fig. 6).
Multidimensional assessment of fatigue (MAF) determined in patients with fibromyalgia (FM) in the personalized Mediterranean diet (DIET) and general balanced diet (NODIET) groups during visit 1, visit 2 and, visit 3 (only the DIET group).
**p < 0.01 versus visit 1 of the same group,
###p < 0.001 versus visit 2 of the NODIET group. Mean ± SEM
ANOVA applied to the fibromyalgia impact questionnaire (FIQ) scores during visit 1 and 2 revealed a significant interaction group × visit [F(1, 75) = 9.1, p < 0.01], as the DIET group scores were lower at visit 2 than at visit 1 (p < 0.05), the NODIET group values were higher at visit 2 than at visit 1 (p < 0.05), and at visit 2 the DIET group had lower values than the NODIET group (p = 0.001; Fig. 7). One-way ANOVA applied to the three visits of the DIET group revealed a significant difference [F(2,74) = 4.3, p = 0.01], as visit 2 and visit 3 scores were lower than those of visit 1 (p < 0.05 and p < 0.01, respectively; Fig. 7).
Fibromyalgia impact questionnaire (FIQ) determined in patients with fibromyalgia (FM) in the personalized Mediterranean diet (DIET) and general balanced diet (NODIET) groups during visit 1, visit 2 and, visit 3 (only the DIET group).
*p < 0.05,
**p < 0.01 versus visit 1 in the same group,
###p < 0.001 versus visit 2 of the NODIET group. Mean ± SEM
Repeated measures ANOVA revealed no significant differences in BMI for the factor visit (p > 0.05) or for the interaction visit × group (p > 0.05). ANOVA applied to BMI in the DIET group during the three visits showed a significant difference [F(2,50) = 4.7, p = 0.01], as BMI was lower at visit 2 (p < 0.05) and visit 3 (p < 0.01) than at visit 1 (Fig. 8).
Discussion
This randomized controlled trial focused on the possibility of improving the quality of life of patients with fibromyalgia by changing their dietary habits. We proposed two types of diet, one with a simple reduction in calorie intake, the other specifically based on the Mediterranean diet with the elimination of foods with potential inflammatory effects. Clinical symptoms improved in the patients following the anti-inflammatory Mediterranean diet, especially in terms of overall disability.
We proposed dietary prescriptions to a total of 100 patients; the first thing to be noted is that, as confirmed by the eating attitude test, a high number of these patients presented eating disorders, in terms of kind of food, amount, and order of meals. Many patients were aware of this bias in their life. Eating is often chosen as a reward without considering that the pleasure is often followed by physical and psychological impairment. In the present study patients had no problem following the dietary indication and once arrived at the end of the first month continued for another month. The group of patients receiving the personalized Mediterranean diet already improved in many parameters after one month and most of them also showed better results at the end of the second month. Thus, while the short term result of dietary prescription seems good, the possibility that patients would continue with this dietary regimen requires long-term confirmation.[25].
In recent years, several studies have highlighted the detrimental effect of certain kinds of foods on gut health [26]; the loss of impermeability from the gut structures allows the abnormal contact of digested/not digested elements with the gut immune system and possible increase in inflammatory elements in the blood. Although these elements rarely induce pain in the gut, their circulation in the body can lower pain threshold, for instance in muscles. Fibromyalgia is well known to have diffuse pain, without evident alterations in the painful areas. The presence of gut function alterations can explain these conditions. For this reason the improvement in the general condition observed in the DIET group was possible, although these patients were in chronic pain for many years.
The results of the present study is in line with other evidence showing that the incidence of chronic pain or inflammation is significantly lower in people who eat a mainly plant-based diet than in people who eat like the average American [27].
Possible mechanisms of action behind the health benefits of dietary manipulation and the elimination of possible offending foods, may include significant changes in intestinal microbiota, highly sensitive to food nature. Gut microbiota is well known to participate in the digestive processes with the production of essential elements for gut health (i.e., short-chain fatty acid), thus, among the different hypotheses to explain the origin of FM, we could consider the alterations of other systems directly and/or indirectly involved in gut structure and functions. Once the intestinal barrier is damaged (by infection and/or food), inflammation can occur in the intestinal immune system, releasing substances that in certain cases can enter the CNS through the altered blood–brain barrier.
It is conceivable, therefore, that poor dietary habits in patients with FM, together with other predisposing factors, could be a cause of their chronic pain. Fibromyalgia represents a model of nociplastic pain in which the mechanism of central sensitization predominates as the pathophysiological basis [28]. The role of diet and eating habits in the development and maintenance of central sensitization is widely recognized [29]. In the present study, we have confirmed the poor dietary habits in FM patients. We also found that most patients were overweight, another factor that could predispose to chronic pain [30].
Patients in the intervention group received a personalized diet on the basis of the general principles of the Mediterranean diet. This version of the Mediterranean diet, in which dairy products and eggs were excluded, was used to achieve a greater impact of the diet on the patient’s habits. Already after 1 month, positive results were achieved in the DIET group, unlike in the control group. Pain disability scores improved in the DIET group compared with the control group. Interestingly, the ‘specific’ FM measures (WPI and SS) did not change significantly even 2 months after the start of the 4-week diet, while the key measures indicating disability did improve, especially the FIQ and the subscores of the BPI, which relate to disability and pain’s interference with physical and occupational activities. Apart from the positive effect on mood through the general improvement of everyday abilities, the antiinflammatory Mediterranean diet could directly improve the symptoms of anxiety and depression, as numerous studies have suggested [30, 31]. This is particularly important in people with FM, as symptoms of depression are very common and contribute to the diagnosis. The patients in the present study were under the pharmacological therapies recommended for FM, such as duloxetine and pregabalin, with a slight-moderate effect on pain. Both drugs have effects on anxiety and depression, but the comparison between the different dietary interventions shows that the specific Mediterranean diet we prescribed could have a significant additional impact on mood.
Although the main clinical aspects of FM did not change significantly in both groups, the same symptoms had a lower impact on the patients’ activity, since many other clinical aspects improved, such as fatigue, one of the most disabling symptoms. This was not merely related to weight loss, since BMI, albeit decreased in the DIET group, did not correlate with the main clinical indices.
Nutritional intervention is a complex factor that requires many elements to function. In particular, we must take into account the quantity of food, its components, the time of intake, the quality of the food, the allergies/intolerances of the patients, the age of the patients, their BMI, their work/physical activity. All these aspects must be considered when planning a diet. In the present study, a comprehensive interview was conducted with all subjects to assess all possible elements that should be included in the diet preparation. In addition to the possible direct effect of the foods included in meals, participation in a diet program by a patient must be considered as additional attention to their status. Indeed, the request for regular time/quantity/components of meals probably acts as ‘overattention’ in patients, which may contribute to their well-being. In the present protocol, however, both groups were interviewed and controlled, but only the patients in the DIET group received a personalized diet with specific eating habits and the adoption of typical Italian foods and seasonal components. The central effect of diet is considered in the treatment of CNS disorders, so the evidence is in favor of the Mediterranean diet improving brain function and cognitive performance [32,33,34].
Subjective pain perception decreased in the DIET group only after 2 months, which is consistent with our previous findings on the lack of a short-term effect of hormonal modulation on subjective pain measures but great effects on the quality of life of all patients [35].
Study Limitations
Considering the low adherence of patients to the protocol, more cases are needed to confirm the present results. Moreover, a longer follow-up could be performed to verify a possible change in the main FM symptoms and their possible resolution.
Prescription of a diet should be a starting program for people with FM, without the use of medication, given its low to moderate effect. In this way, more evidence could be added for an understanding of the benefits of diet alone or diet in conjunction with medication.
Conclusions
People with fibromyalgia have poor eating habits, which could be a cause of the disease. A personalized Mediterranean diet with fewer proinflammatory substances seems to reduce the disability and fatigue associated with FM.
Although further studies are needed to support the present results in a long-term follow-up with a larger number of cases, our generally positive outcomes suggest that the dietary approach should be adopted for the treatment of fibromyalgia.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Sarzi-Puttini P, Giorgi V, Atzeni F, Gorla R, Kosek E, Choy EH, et al. Fibromyalgia position paper. Clin Exp Rheumatol. 2021;130(3):186–93 (Epub 2021 May 13. PMID: 34001303).
Fitzcharles MA, Cohen SP, Clauw DJ, Littlejohn G, Usui C, Häuser W. Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet. 2021;397(10289):2098–110. https://doi.org/10.1016/S0140-6736(21)00392-5. (PMID: 34062144).
Descalzi G, Ikegami D, Ushijima T, Nestler EJ, Zachariou V, Narita M. Epigenetic mechanisms of chronic pain. Trends Neurosci. 2015;38:237–46.
Abdulkhaleq LA, Assi MA, Abdullah R, Zamri-Saad M, Taufiq-Yap YH, Hezmee MNM. The crucial roles of inflammatory mediators in inflammation: a review. Vet World. 2018;11:627–35.
Speciani AF, Piuri G. Measuring biomarkers for an innovative personal food profile. J Am Coll Nutr. 2015;34:34–8.
Maddox EK, Massoni SC, Hoffart CM, Takata Y. Dietary effects on pain symptoms in patients with fibromyalgia syndrome: systematic review and future directions. Nutrients. 2023;15(3):716. https://doi.org/10.3390/nu15030716. (PMID:36771421; PMCID:PMC9921865).
Kurapati M, Carreira D. Diet composition’s effect on chronic musculoskeletal pain: a narrative review. Pain Phys. 2023;26(7):527–34 (PMID: 37976478).
Sköldstam L, Hagfors L, Johansson G. An experimental study of a Mediterranean diet intervention for patients with rheumatoid arthritis. Ann Rheum Dis. 2003;62:208–14.
McKellar G, Morrison E, McEntegart A, Hampson R, Tierney A, Mackle G, Scoular J, Scott JA, Capell HA. A pilot study of a Mediterranean type diet intervention in female patients with rheumatoid arthritis living in areas of social deprivation in Glasgow. Ann Rheum Dis. 2007;66:1239–43.
Lewis JD, Albenberg L, Lee D, Kratz M, Gottlieb K, Reinisch W. The importance and challenges of dietary intervention trials for inflammatory bowel disease. Inflamm Bowel Dis. 2017;23:181–91.
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Häuser W, Katz RL, et al. 2016 revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016;46(3):319–29. https://doi.org/10.1016/j.semarthrit.2016.08.012.
Macfarlane GJ, Kronisch C, Dean LE, et al. EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. 2017;76:318–28.
(SINU) (2014) Italian Society of Human Nutrition. Dietary Reference Values of Nutrients and Energy for the Italian Population - IV revision . s.l. : SICS, 2014
Fitó M, Cladellas M, de la Torre R, Martí J, Muñoz D, Schröder H, et al. Antiinflammatory effect of virgin olive oil in stable coronary disease patients: a randomized, crossover, controlled trial. Eur J Clin Nutr. 2008;62(4):570–4.
Maiorino MI, Bellastella G, Petrizzo M, Scappaticcio L, Giugliano D, Esposito K. Antiinflammatory effect of Mediterranean diet in type 2 diabetes is durable: 8-year follow-up of a controlled trial. Diabetes Care. 2016;39(3):e44–5.
Schönenberger KA, Schüpfer AC, Gloy VL, et al. Effect of anti-inflammatory diets on pain in rheumatoid arthritis: A systematic review and meta-analysis. Nutrients. 2021;13(12):4221.
Prabhakaran D, Khandelwal S, Martínez-González MA, Tong TY, Forouhi NG, Trichopoulou A, Mozaffarian D, de Lorgeril M. Definitions and potential health benefits of the Mediterranean diet: views from experts around the world. BMC Med. 2014;12:112.
Dotti A, Lazzari R. Validation and reliability of the Italian EAT-26. Eat Weight Disord. 1998;3:188–94. https://doi.org/10.1007/BF03340009.
Stanhope J. Brief pain inventory review. Occup Med. 2016;66(6):496–7.
Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12(1):63–70.
Zung WW. Self-Rating Anxiety Scale (SAS). 1971
Starz TW, Sinclair JD, Okifuji A, Turk DC. Putting the finger on fibromyalgia: the manual tender point survey. J Musculoskelet Med. 1997;14:61–70.
Belza BL. Comparison of self-reported fatigue in rheumatoid arthritis and controls. J Rheumatol. 1995;22(4):639–43.
Borga M, West J, Bell JD, Harvey NC, Romu T, Heymsfield SB, et al. Advanced body composition assessment: from body mass index to body composition profiling. J Investig Med. 2018;66:887–95.
Correa-Rodríguez M, El Mansouri-Yachou J, Tapia-Haro RM, Molina F, Rus A, RuedaMedina B, Aguilar-Ferrandiz ME. Mediterranean diet, body composition, and activity associated with bone health in women with fibromyalgia syndrome. Nurs Res. 2019;68(5):358–64. https://doi.org/10.1097/NNR.0000000000000361. (PMID: 30939528).
Smedslund G, Byfuglien MG, Olsen SU, Hagen KB. Effectiveness and safety of dietary interventions for rheumatoid arthritis: a systematic review of randomized controlled trials. J Am Diet Assoc. 2010;110(5):727–35. https://doi.org/10.1016/j.jada.2010.02.010. (PMID: 20430134).
Towery P, Guffey JS, Doerflein C, Stroup K, Saucedo S, Taylor J. Chronic musculoskeletal pain and function improve with a plant-based diet. Complement Ther Med. 2018;40:64–9. https://doi.org/10.1016/j.ctim.2018.08.001. (Epub 2018 Aug 6 PMID: 30219471).
Arendt-Nielsen L, Morlion B, Perrot S, Dahan A, Dickenson A, Kress HG, Wells C, Bouhassira D, Drewes AM. Assessment and manifestation of central sensitisation across different chronic pain conditions. Eur J Pain. 2018;22(2):216–41. https://doi.org/10.1002/ejp.1140. (Epub 2017 Nov 5 PMID: 29105941).
Nijs J, Tumkaya Yilmaz S, Elma Ö, Tatta J, Mullie P, Vanderweeën L, et al. Nutritional intervention in chronic pain: an innovative way of targeting central nervous system sensitization? Expert Opin Ther Targets. 2020;24(8):793–803. https://doi.org/10.1080/14728222.2020.1784142. (Epub 2020 Jun 28 PMID: 32567396).
Kadayifci FZ, Bradley MJ, Onat AM, Shi HN, Zheng S. Review of nutritional approaches to fibromyalgia. Nutr Rev. 2022;80(12):2260–74. https://doi.org/10.1093/nutrit/nuac036. (PMID: 35674686).
Walaszek M, Kachlik Z, Cubała WJ. Low-carbohydrate diet as a nutritional intervention in a major depression disorder: focus on relapse prevention. Nutr Neurosci. 2024;21:1–14. https://doi.org/10.1080/1028415X.2024.2303218. (PMID: 38245881).
Suárez-López LM, Bru-Luna LM, Martí-Vilar M. Influence of nutrition on mental health: scoping review. Healthcare (Basel). 2023;11(15):2183. https://doi.org/10.3390/healthcare11152183. (PMID:37570422; PMCID:PMC10418505).
McEvoy CT, Jennings A, Steves CJ, Macgregor A, Spector T, Cassidy A. Diet patterns and cognitive performance in a UK Female Twin Registry (TwinsUK). Alzheimers Res Ther. 2024;16(1):17. https://doi.org/10.1186/s13195-024-01387-x. (PMID: 38263271).
Al-Darsani Z, Jacobs DR Jr, Bryan RN, Launer LJ, Steffen LM, Yaffe K, Shikany JM, Odegaard AO. Measures of MRI brain biomarkers in middle age according to average modified Mediterranean diet scores throughout young and middle adulthood. Nutr Healthy Aging. 2023;8(1):109–21. https://doi.org/10.3233/NHA-220192. (PMID:38013773; PMCID:PMC10475985).
Aloisi AM, Ceccarelli I, Carlucci M, Suman A, Sindaco G, Mameli S, Paci V, Ravaioli L, Passavanti G, Bachiocco V, Pari G. Hormone replacement therapy in morphine-induced hypogonadic male chronic pain patients. Reprod Biol Endocrinol. 2011;18(9):26. https://doi.org/10.1186/1477-7827-9-26. (PMID:21332999; PMCID:PMC3049183).
Acknowledgements
The authors thank all the patients who accepted to be involved in this study, their University, all collaborators, and specialists for the fundamental help.
Medical Writing, Editorial, and Other Assistance
The English style was corrected online with Editor—InstaText | Written like a native speaker and further edited by a native English speaker. The editing service was funded by DiBrain Department, Bari Aldo Moro University.
Funding
No funding or sponsorship was received for this study or for publication of this article. The Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Anna Maria Aloisi and Marina de Tommaso designed the study, performed data analysis, prepared the manuscript, and supervised the study; Valeria Ladisa and Ilenia Casini performed data collection, database management, and data analysis; Livio Clemente and Marianna Delussi performed data collection and database management.
Corresponding author
Ethics declarations
Conflict of Interest
Ilenia Casini, Valeria Ladisa, Livio Clemente, Marianna Delussi, Elvira Rostanzo, Sofia Peparini, Anna Maria Aloisi, and Marina de Tommaso declare no conflicts of interest.
Ethical Approval
The study was approved by the ethics committee of the General Hospital of the Aldo Moro University of Bari (approval number 7173 2022 1 22.). The patients signed an informed consent form.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Casini, I., Ladisa, V., Clemente, L. et al. A Personalized Mediterranean Diet Improves Pain and Quality of Life in Patients with Fibromyalgia. Pain Ther 13, 609–620 (2024). https://doi.org/10.1007/s40122-024-00598-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-024-00598-2