Abstract
Introduction
Sacroiliac joint (SIJ) pain is a relatively common cause of low back pain. Percutaneous radiofrequency (RF) techniques for SIJ are limited to ablation of the posterior SIJ innervation. Different techniques have been described for SIJ radiofrequency ablation, including conventional thermal, cooled RF, pulsed RF, bipolar RF, and specialized tip RF needle (i.e., multi-tined); however, additional costs may limit these applications.
Methods
This new technique for SIJ denervation uses anatomical landmarks and a single RF cannula. Two spinal needles are placed lateral to the posterior S1 and S2 sacral foramina; then, with caudal tilt we get a coaxial view of the sacral bone, we advance an 18-G curved 15-mm active tip RF cannula just lateral to the aligned finder needles. Ablation is performed, and then the RF cannula is retracted 2 cm and ablation is repeated for a total of four lesions.
Results
The two spinal needles placed lateral to the posterior sacral foramina S1 and S2 guide the final needle in the posterior aspect of the sacrum, lateral to the sacral foramina, where the lateral sacral branches are located.
Conclusion
We introduce a cost and time efficient technique to perform radiofrequency ablation of the sacral lateral branches using a single RF needle. This technique utilizes the sacrum’s reliable anatomy and angulation and maximizes the surface area of the active tip lesioning. This technique creates a strip lesion lateral to the sacral foramina and reduces time and cost efficacy compared to several of the other techniques and/or commercially available special devices designed for sacroiliac denervation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Patients with sacroiliac joint pain have a marked impairment in quality of life that is generally worse than in many chronic health conditions, with a prevalence in the US ranging from 10−30% and rising |
Currently, there are different techniques and devices to treat sacroiliac joint pain, and there is no gold standard within current treatments or procedures |
What was learned from the study? |
In this study we propose a potentially simple and practical technique for performing an ablation of the sacral lateral branches in patients with sacroiliac joint pain |
In this technique description, we rely on finder needles, which, when aligned, guide us through the posterior aspect of the sacrum and delimit the sacral foramens medially |
Introduction
The sacroiliac joint (SIJ) is a complex joint that is closely associated with the lower back yet is underappreciated in its contribution to lower back pain (LBP) [1]. SI joint dysfunction can cause pain in the low back, buttock, groin, thigh, and occasionally the calf [2] and is an accepted cause of LBP with a prevalence in the US in the range of 10–30% and rising [3]. SIJ pain represents up to 15% of all patients seen in outpatient clinics with chronic LBP, and up to 75% of patients who undergo lumbar fusion surgery have degeneration at 5 years post-surgery [1].
Over the last decade there has been interest in longer term interventional treatments for SIJ pain utilizing different techniques with traditional RF needles, cooled RFA equipment, larger shaped RF needles, a multi-electrode radiofrequency probe, endoscopic radiofrequency neurotomy, and lateral and posterior SI joint fusion techniques. These new modalities also come with an additional cost and limited worldwide availability, compounded by the paucity of literature demonstrating greater efficacy [4].
The lack of comparative data has led to neuroablative procedures targeting the SI joint to be increasingly deemed experimental by national payers in the USA, further compounding the need for a cost-effective alternative for patients who now have greater out of pocket costs.
This article hereby describes a practical, anatomy informed, time and cost-efficient method to perform a strip lesion of the sacral lateral branch nerves using conventional RF. This technique utilizes a caudad view, in-plane, or ‘gun barrel’ approach to sacroiliac joint ablation using a single large bore, radiofrequency cannula without the need for specialized equipment that may be unavailable or restricted because of cost [5, 6].
Methods/Technique
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
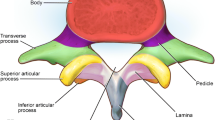
This anatomy-informed technique utilizes radiologic landmarks of the sacrum. Sacral size and subsequent measurements across populations are generally stable, with differences in foraminal location between sexes separated by only several millimeters [7]. Because of this consistency, techniques for sacral access based on measurements have been published for sacral neuromodulation, dorsal root ganglion stimulation, and intraoperative hardware placement during surgery [8, 9].
Regular perioperative care as per standard radiofrequency protocols [10] places particular attention on implantable devices such as defibrillators, neurostimulators, pumps, and other devices prevalent in the pain population. The procedure requires a fluoroscopic unit, compatible table, radiofrequency unit, probe, grounding pad, and cannulas. As with many procedures that require multiple AP and lateral views, a set up with one in AP and one laterally may be more efficient, if available [11].
An 18-gauge radiofrequency cannula has the optimal width and length as the diameter of the cannula creates a greater lesion size over time. Longer needle length, such as a 15 cm or 20 cm cannula, is typically required given the target depth. An active tip of 15 mm creates an ellipsoidal lesion with a length of approximately 20 mm × 11 mm wide circumferentially, compared to 13.4 mm × 9.9 mm with a 10-mm active tip [12]. A curved tip needle provides better steerability. The depth of the lesion compensates for some of the irregularities of the dorsal aspect of the posterior sacrum [13]. Conventional radiofrequency should be carried out at 90° for 90 s.
Technique
Anesthetic preference should be a balance of patient- and surgeon-specific needs, as the need for sedation is optional. After informed consent and discussion of risks vs. benefits, the patient is brought into the operative suite and placed in the prone position on the fluoroscopic table with or without a pillow for comfort. The patient should have standard ASA monitors with supplemental O2.
After appropriate sterile preparation with chlorhexidine solution, the patient, surgeon, and fluoroscopic unit should be draped in normal sterile fashion.
Sacral Alignment
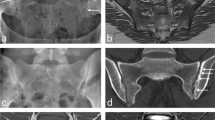
The measurements of the sacrum are performed from the aligned sacral promontory (SP), which needs to be approximately 30° cephalad to compensate for the lumbosacral angle. With a skin marker, draw a line over the sacral promontory and a line down the midline of the aligned sacrum. The superior border of the S3 approximates the inferior portion of the SI joint on fluoroscopy. (Fig. 1A.)
Place Finder Needles
The location of the sacral foramen is relatively stable among populations. Place 22-g finder needles lateral to the S1 and the S2 foramen. The lateral border of the S1 foramen is approximately 3.1 cm from the midline and 3 cm from the SP. The S2 foramen is approximately 5 cm from the SP and 1.5–2 cm from midline, but we will also place the second finder needle 3.5 cm from midline. These needles demarcate a safety boundary lateral to the sacral foramen, and their tips demarcate the osseous border of the posterior sacrum. [14] (Fig. 1B).
Reposition Fluoroscopy to Working View
Take a caudal tilt with the fluoroscope 45° from the midline anterior-posterior position over the sacrum. Align the previously placed finder needles. Their aligned tips represent the posterior plate of the sacrum. The aligned shafts represent the medial border of our target needle trajectory. (Fig. 2A and B).
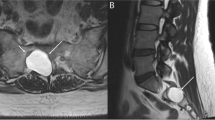
Target for RF Cannula Just Lateral to the Tips of the Superimposed Finder Needles
Advance the curved tip RF cannula just lateral to the spinal needle tips in the coaxial view. (Fig. 2A). Use the curved tip of the needle to steer and stay as close to the posterior sacrum as possible in the lateral position. See Fig. 3B. The final needle position should be close to the rostral border of the sacrum in the 30° cephalad angulation view (Fig. 3C).
After confirmation on AP and lateral views until the tip of the RF needle is in the dorsal ramus of L5, motor stimulation should be performed before radiofrequency lesion.
If using a 15-mm active tip needle, after RF is completed, retract the needle approximately 2 cm and repeat lesioning for a total of four lesions. If 10-mm active tip needles are used, a total of six lesions are required (Fig. 4).
Limitations: This technique was conceptualized as an alternative, cost-effective option for the treatment of chronic sacroiliac joint dysfunction. While preliminary results are promising, further research is required to demonstrate the effectiveness of this technique compared to existing techniques and technology. Additionally, this single-needle and electrode technique does not allow for bipolar radiofrequency. If bipolar is recommended, it will require an additional cannula placed adjacent to the initial cannula.
Conclusion
We present a novel method of lateral branch RF denervation of the sacroiliac joint as an alternative to current techniques. Awareness of chronic pain stemming from the SI joint is growing, and this technique offers practitioners who do not have access to multi-electrode probes, multi-tined expanding RF electrodes, or separate cooled technology an alternative. This single-puncture technique creates a strip lesion size adjacent to the sacrum in the plane of the lateral branch nerves in a cost- and time-effective manner.
References
Buchanan P, Vodapally S, Lee DW, Hagedorn JM, Bovinet C, Strand N, Sayed D, Deer T. Successful diagnosis of sacroiliac joint dysfunction. J Pain Res. 2021;14:3135–43. https://doi.org/10.2147/JPR.S327351. (PMID: 34675642; PMCID: PMC8517984).
Fallowski A. Review and algorithm in the diagnosis and reatment of sacroiliac joint pain. J Pain Res. 2020;13:3337–48.
Dreyfuss P, Dreyer SJ, Cole A, Mayo K. Sacroiliac joint pain. J Am Acad Orthop Surg. 2004;12(4):255–65. https://doi.org/10.5435/00124635-200407000-00006.
Russo M, Santarelli D, Wright R, Gilligan C. A history of the development of radiofrequency neurotomy. J Pain Res. 2021;24(14):3897–907. https://doi.org/10.2147/JPR.S334862. (PMID: 34992451; PMCID: PMC8714970).
Silva-Ortiz VM, Plancarte-Sanchez R, Reyes I, Gulati A. A practical access for fluoroscopically-guided percutaneous sacroplasty: case report. Pain Pract. 2022. https://doi.org/10.1111/papr.13192. (Epub ahead of print. PMID: 36478396).
Silva-Ortiz VM. Imaging optimization for fluoroscopically guided caudal epidural coaxial view. Intervent Pain Med. 2022;1(2):100080. https://doi.org/10.1016/j.inpm.2022.100080.
Başaloğlu H, Turgut M, Taşer FA, Ceylan T, Başaloğlu HK, Ceylan AA. Morphometry of the sacrum for clinical use. Surg Radiol Anat. 2005;27(6):467–71. https://doi.org/10.1007/s00276-005-0036-1. (Epub 2005 Oct 7 PMID: 16211321).
Chapman KB, Sayed D, Lamer T, Hunter C, Weisbein J, Patel KV, Dickerson D, Hagedorn JM, Lee DW, Amirdelfan K, Deer T, Chakravarthy K. Best practices for dorsal root ganglion stimulation for chronic pain: guidelines from the American Society of Pain and Neuroscience. J Pain Res. 2023;14(16):839–79. https://doi.org/10.2147/JPR.S364370. (PMID: 36942306; PMCID: PMC10024474).
Adelstein SA, Lee W, Gioia K, Moskowitz D, Stamnes K, Lucioni A, Kobashi KC, Lee UJ. Outcomes in a contemporary cohort undergoing sacral neuromodulation using optimized lead placement technique. Neurourol Urodyn. 2019;38(6):1595–601. https://doi.org/10.1002/nau.24018. (Epub 2019 May 1 PMID: 31044466).
Sowder T, Sayed D, Concannon T, Pew SH, Strand NH, Abd-Elsayed A, Wie CS, Gomez Ramos DE, Raslan AM, Deer TR. The American Society of Pain and Neuroscience (ASPN) guidelines for radiofrequency ablative procedures in patients with implanted devices. J Pain Res. 2023;16:3693–706. https://doi.org/10.2147/JPR.S419594.
Bayerl SH. Radiofrequency denervation for treatment of sacroiliac joint pain—comparison of two different ablation techniques. Neurosurg Rev. 2018. https://doi.org/10.1007/s10143-018-1016-3.
Cosman ER Jr, Dolensky JR, Hoffman RA. Factors that affect radiofrequency heat lesion size. Pain Med. 2014;15(12):2020–36. https://doi.org/10.1111/pme.12566. (Epub 2014 Oct 14 PMID: 25312825).
Cheng JS, Song JK. Anatomy of the sacrum. Neurosurg Focus. 2003;15(2):E3. https://doi.org/10.3171/foc.2003.15.2.3. (PMID: 15350034).
Chapman KB, van Helmond N, Kallewaard JW, Vissers KC, Patel KV, Motivala S, Hagedorn JM, Deer TR, Dickerson DM. An anatomy-informed, novel technique for S1 dorsal root ganglion stimulation lead placement. Pain Med. 2022;23(10):1750–6. https://doi.org/10.1093/pm/pnac062. (PMID: 35426940; PMCID: PMC9527614).
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors. No funding or sponsorship was received for this study or publication of this article.
Author information
Authors and Affiliations
Contributions
Study conception and design: Victor M Silva-Ortiz and Kenneth B. Chapman. Data collection Victor M Silva-Ortiz and Kenneth B. Chapman. Analysis and interpretation of results: Victor M Silva-Ortiz, Kenneth B. Chapman, George C. Chang Chien, Sudhir Diwan, Alaa Abd-Elsayed. Draft manuscript preparation: Victor M Silva-Ortiz, KBC, George C. Chang Chien, Sudhir Diwan, Alaa Abd-Elsayed. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Victor M Silva-Ortiz is a consultant and reports personal fees from Axon Productos Medicos. Kenneth B. Chapman, George C. Chang Chien, Sudhir Diwan, and Alaa Abd-Elsayed are Editorial Board Members for Springer Nature.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Silva-Ortiz, V.M., Chapman, K.B., Chang Chien, G.C. et al. Sacroiliac Joint Denervation—A Novel Approach to Target Sacral Lateral Branches: A Practical Approach. Pain Ther 13, 281–286 (2024). https://doi.org/10.1007/s40122-024-00585-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-024-00585-7