Abstract
Medication overuse headache (MOH) places both a physical and emotional burden on patients. MOH may occur as a consequence of a negative spiral of events comprising an increasing number of headache days while taking frequent or excessive amounts of medications for acute treatment of headaches or migraine. Despite acute and prophylactic treatment options, there remains a complex subset of patients who fail first-line oral prophylactic therapies due to insufficient response or failure to tolerate, and require access to new prophylactic treatment options, including calcitonin gene-related peptide (CGRP) inhibitors such as eptinezumab. In this article I present a series of clinical scenarios in which the use of eptinezumab may be beneficial, based on the extensive experience I have gained using the treatment, in more than 25 patients, (and over 40 infusions), over a 2-year period. Eptinezumab provides an additional therapeutic modality for patients who are refractory to other migraine medications, including other CGRP pathway monoclonal antibody (mAb) therapies. I discuss within this article the potential role for eptinezumab in various clinical scenarios such as refractory migraine, including MOH, in which the rapid bioavailability of the preparation may be of particular utility. It is important to tailor treatment plans to the individual patient needs and provide other lifestyle and non-drug-based recommendations when treating patients with MOH, who may be appropriate for treatment with eptinezumab.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Medication overuse headache (MOH) places both a physical and emotional burden on a patient. |
MOH occurs as a result of frequent or excessive use of medications for the acute treatment of headaches or migraine. |
Despite acute and prophylactic treatment options, there remains a complex subset of patients who require additional therapies due to insufficient response, or failure to respond. |
In complex-to-manage patients, newer calcitonin gene-related peptide (CGRP) pathway monoclonal antibody (mAb) therapies, such as eptinezumab, can be considered. |
Background
The international prevalence of chronic headache is reported to be between 4% and 5%, with the incidence of new-onset chronic migraine (CM) in patients with episodic migraine (EM) reported at 2.5% per annum [1]. Chronification of migraine can result from frequent or excessive use of medications for the acute treatment of headaches or migraine and in turn may result in medication overuse headache (MOH) [2]. MOH is estimated to affect 1–2% of the general population [3] and places both a physical and emotional burden on patients. While MOH is usually seen in patients with migraine, it can be seen in other types of headaches, including tension or cluster headaches [1]. The main diagnostic criteria for MOH, according to the International Classification of Headache Disorders (ICHD) [2], are presented in Table 1.
Eptinezumab, a humanized monoclonal immunoglobulin G1 (IgG1), selectively inhibits both the α and β forms of the human calcitonin gene-related peptide (CGRP) ligand [4]. CGRP is found in neurons in the trigeminal ganglia in the brain and is released during migraine attacks [5]. Elevated blood levels of CGRP can also trigger migraine. In Australia, eptinezumab is indicated for migraine prophylaxis in adult patients [4]. At the time of publication, eptinezumab is available to Australians by private prescription, however an application for government reimbursement has been submitted and government reimbursement is expected in the near future. Two other CGRP pathway monoclonal antibody (mAb) therapies (fremanezumab and galcanezumab) are reimbursed by the Australian government for eligible patients. A fourth CGRP pathway mAb therapy, erenumab, is available on private prescription.
Patients who have failed two to three prophylactic medications should be referred to a neurologist with experience in headache management [6, 7]. In some patients, intravenous eptinezumab at 12-week intervals is preferred to self-administered subcutaneous CGRP pathway mAb options. Eptinezumab provides an additional therapeutic modality for patients who are refractory to other migraine medications, including other CGRP pathway mAb therapies. Intravenous eptinezumab achieves rapid therapeutic levels [time to peak plasma concentration (Cmax) of 30 min], and a rapid onset of effect (typically within 1 day following administration). It is also useful in providing therapeutic cover in opioid-overuse medication overuse headache patients who are unable to attend in-patient detoxification.
From a practical perspective, I have found that eptinezumab is straightforward to administer intravenously in our headache clinic infusion facility. With access to infusion units, intravenous route of administration is not a barrier to use and is not more challenging than subcutaneous medications. The subcutaneous route of administration can, in my experience, present its own unique challenges, including patient preference to avoid self-injection.
Below I present a series of hypothetical clinical scenarios in which the management of migraine and MOH are discussed, with particular emphasis on how eptinezumab may be of utility.
Lifestyle Modifications
Scenario 1 During a consultation a patient comments that they want to discuss non-pharmaceutical treatment options for their migraine, and ways to minimise their risk of developing MOH. What advice can the clinician provide this patient? |
Age and sex have been identified as non-modifiable risk factors for MOH, with MOH being more frequently reported in women [1, 3] and adults between 30 and 50 years of age [1]. Modifiable risk factors include the type of drug used to treat the headache [1]. Recommendations regarding lifestyle modifications should be on the management of obesity, stress and avoidance of acute medication overuse [6].
In addition to considering CGRP pathway mAb therapy, non-drug interventions must be considered. These include the use of a headache diary – a key tool for both the treating clinician and the patient. Diaries can be used to record the frequency, severity and onset of symptoms, and help track the use of medications, lifestyle modifications and identify potential triggers. Several free resources are available for patients, including both hardcopy and electronic (mobile applications).
Education should focus on modifiable risk factors such as lifestyle interventions including diet and exercise, stress minimization, improved mental health, sleep and minimization of triggering events [6]. The role of education for both the patient and their family/ carers cannot be understated. All patients presenting with migraine should be educated on MOH [6]. For many patients, education on treatment adherence may also be required. The clinician should ensure that they use language which is non-judgemental and empathetic to the patient’s position.
Early Treatment of Patients with Migraine
Scenario 2 A 51-year-old male presents with recurrent migraine that is not responsive to initial treatment with simple analgesia. He has a history of obesity and depression. He believes that the intensity and frequency of his migraines are increasing over time. How should this patient be treated? What other advice should the clinician provide to this patient? |
Migraine may be treated acutely and/or prophylactically. Treatment of acute migraine aims to abort the headache stage within the first several hours, although it is not useful in the prodromal or postdromal stages [8]. The early use of analgesia, at the onset of migraine, has been shown to be effective [9]. The Act When Mild study found that, when patients with migraine took almotriptan (12.5 mg) when pain was mild and within 1 h of headache onset, 53% were pain free at 2 h, compared with 37.5% of patients who took treatment when pain was moderate to severe (p = 0.02) [10]. Prophylactic treatment is recommended for patients who have events that occur frequently or who are inconsistently responding to acute therapy, and those with disabling symptoms, particularly in patients who are at risk of MOH [8].
A review of the patient should also ensure that they are receiving optimal therapy for their hypertension and management of their depression. A sleep history should be taken with consideration of possible co-morbid conditions such as sleep apnoea.
The patient should be provided a stepwise medication plan to treat their migraines acutely. A stepped plan usually commences with an NSAID plus an antiemetic; if symptoms continue to persist after a period of 30–45 min, treatment with a triptan may be considered. Patients are also provided with clear guidance on how frequently an acute treatment should be used (no more than 15 days per month for simple analgesia and no more than 10 days per month for triptans). They should also be encouraged to keep a headache diary, a review of which will help inform future clinical decision-making if the patient fails to continue to respond to treatment.
Goals of Treatment in Patients Who Have Failed Prophylactics
Scenario 3 A 34-year-old mother of two children who has completed her family presents with recurrent migraines that are not responsive to initial treatment with simple analgesia. She has trialled and failed three oral migraine prophylactic agents. She believes that the number of migraine days now exceeds the number of days without migraines; she notes that their frequency is now affecting her quality of life. What are the goals of treatment in this patient? What other therapeutic approaches can be considered? |
Despite a range of treatment options, there remains a subset of patients who require additional therapies due to insufficient response, or failure to respond to initial treatments. Patients who have failed two to three prophylactic medications should be referred to a neurologist with experience in headache management [6, 7]. In these complex-to-manage patients, CGRP pathway mAb therapies may be considered.
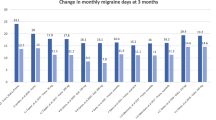
The DELIVER study (N = 865) found that, in adult patients with between two and four prior prophylactic treatment failures over the last 10 years, eptinezumab (100 mg and 300 mg) was efficacious in patients with EM or CM and provided significant migraine prophylactic effects compared with placebo [11]. The change in monthly migraine days (MMD) from baseline to weeks 1–12 was −4.8 [standard error (SE) 0.37] for eptinezumab 100 mg, −5.3 (SE 0.37) for eptinezumab 300 mg, and −2.1 (SE 0.38) for placebo [11]. The difference in change in mean MMD was significant for eptinezumab 100 mg compared with placebo (−2.7, confidence interval [CI] −3.4–−2.0, p < 0.0001) and eptinezumab 300 mg (−3.2, CI −3.9–−2.5, p < 0.0001) [11]. In this case study, I note that the patient has completed her family, and therefore a CGRP pathway mAb therapy may be considered; treatment with a CGRP pathway mAb therapy is not advised in pregnancy.
The effects of treatment with eptinezumab can potentially be seen early, with prophylactic efficacy reported within 1 day of the infusion [12].
Treatment of a Patient with MOH (Opioid-Overuse Headache)
Scenario 4 A 29-year-old male with a history of migraine (with and without aura) since his teenage years is referred to the specialist for treatment with onabotulinum toxin A therapy. A review of the patient’s headache diary indicates a 12-month history of daily headaches and migraine (chronic; 30 headache/migraine days per month). The patient notes that simple analgesics and triptans are no longer effective, and he has been managing his pain with codeine (daily). The patient has previously trialled and failed to respond to or experienced intolerable side effects from oral prophylactic migraine treatments including topiramate, pizotifen, amitriptyline and propranolol. How should the clinician treat this patient? |
Patients pain management needs change over time. In this example, the patient’s daily use of codeine meets the ICHD criteria for MOH (opioid-overuse headache).
In patients with MOH, detoxification is required; this can be undertaken in the community using a slow-tapering regimen, or in the case of opioid overuse, an in-patient treatment setting may be required. For many patients, the in-patient approach to detoxification may not be feasible due to employment or family commitments.
In my experience re-trialling therapies, such as triptans, may work with good effects despite previous treatment failures. In patients who present with MOH, it is important that the treatment team provide education about ongoing opioid use, including the potential for dependence or tolerance to other therapies. For example, a patient may resolve their dependence to one therapy while developing a dependence on another; patients should be provided a stepped acute treatment regimen.
In this clinical scenario, given the long history of migraine and current acuity, treatment with eptinezumab should be discussed with the patient. A sub-analysis of the PROMISE-2 study found that, in patients with both CM and MOH, those treated with eptinezumab had greater reductions in MMD. The change in MMD from baseline to weeks 1–12 were −8.4 for eptinezumab 100 mg and −8.6 for eptineuzamab 300 mg, and −3.0 for placebo [differences were statistically in favour of eptinezumab (100 mg, −3.0, p < 0.0001 versus placebo; 300 mg, −3.2, p < 0.0001 versus placebo)] [13]. Eptinezumab may be particularly important in this clinical scenario given the rapid onset of effect within 1 day after infusion [12] and the patient’s inability to attend in-patient detoxification. For patients who are unable to undertake a formal withdrawal program, an anti-CGRP pathway mAb therapy may be helpful [7].
Treatment of a Patient with MOH (Triptan-Overuse Headache)
Scenario 5 A 46-year-old female presents for management of a 25-year history of migraine (with or without aura). Over the past 5 years her migraines, which she manages with triptans (daily), have become chronic. She has a history of depression and sleep disturbance. The patient has previous trialled and failed to respond to, had insufficient response to, or experienced intolerable side effects with multiple prophylactic therapies including onabotulinum toxin A, topiramate, verapamil, propranolol, and amitriptyline. How should the clinician treat this patient? |
In this example, the patient’s daily use of triptans meets the ICHD criteria for MOH (triptan-overuse headache). Similar to the approach taken in Scenario 4, the clinician’s focus is on resolving the patient’s MOH and establishing a framework to treat the patient’s acute and chronic headache. This should include education about the appropriate use of treatment for acute migraines and the provision of a stepped therapy treatment plan. Patients may be anxious or resistant to ceasing medications [7].
Clinically, the treatment of MOH (both triptan or opioid overuse) can be considered according to the framework outlined by Sun-Edelstein et al. [7]: patient and carer education, weaning and detoxification of overused medications, prophylactic treatment and/or behavioural or non-drug strategies, establishing limits on future medication intake and regular follow-up visits to prevent MOH relapse. Within this framework it is important to develop individualized treatment strategies for patients, supported by a multidisciplinary team. This includes exploring CGRP pathway mAb therapy as a therapeutic option. A key difference in the management of triptan overuse is that withdrawal can be undertaken in a community setting; for patients with opioid overuse, an in-patient withdrawal program is advised so that withdrawal symptoms can be managed appropriately.
In this scenario, the use of treatments such as amitriptyline may be continued if they assist in the management of a patient’s comorbid conditions such as depression and sleep disturbance.
Treatment of Persistent MOH
Scenario 6 The patient from Scenario 5 returns for a follow up appointment, but their medication overuse persists. What treatment options should be considered in this patient? What might the reasons for the continued overuse be? What other considerations are important at this time? |
This patient should be considered for treatment with a CGRP pathway mAb therapy. Eptinezumab can be administered as a 100 mg dose, which is the recommended dose, or 300 mg in patients who require dose escalation. Treatment is administered via 30-min intravenous (IV) infusion every 12-weeks [4].
To assist with measurement of a patient’s response to treatment, a headache impact test-6 (HIT-6) and migraine disability assessment (MIDAS) should be performed pre- and post-treatment. The patient should be encouraged to maintain a headache diary; this should be reviewed by the treatment team at each clinical interaction.
In some circumstances a patient may have already trialled a CGRP pathway mAb therapy without effect or with inadequate response. In this setting the clinician and patient may discuss the trial of other CGRP pathway mAb therapies. Despite the previous lack of response, a trial of other CGRP pathway mAb therapies may result in a response to treatment; a retrospective analysis demonstrated that approximately 30% of patients may benefit from switching CGRP pathway mAb therapy classes (agents targeting the CGRP ligand or its receptor) [14].
Reasons for the patient’s continued use of triptans needs to be investigated by the clinician. A patient may feel anxious regarding ceasing medications [7], and the potential for increased headache pain, or may be experiencing a higher level of headache frequency. In this situation the clinician should continue to provide information about the stepped acute medication plan and education regarding headache management strategies. Advice could be reiterated regarding appropriate limitations of triptan usage to no more than 10 days per month.
Impact of Migraine on the Individual
Scenario 7 During a regular review of a patient, they mention to the clinician, in passing, that they are struggling to maintain their home and work activities to a level that is acceptable to them due to their migraines. What do we know about the impact of migraine on the individual, and what advice can the clinician provide this patient? |
In addition to the physical effects of chronic headache, the burden of disease is significant. The 2017 World Health Organization (WHO) Global Burden of Diseases Study found that headache ranked in the top three conditions in 1990 and 2007 for years lived with disease (YLD) in both males and females [15]. The indirect costs of MOH include absenteeism and reduced productivity, which account for 92% of the overall costs associated with this condition [3]. A 2018 Deloitte Access Economics Report estimated that 4.9 million people experience migraine in Australia, resulting in approximately AUD$35.7 billion indirect and direct costs per annum [16].
In this clinical scenario the patient’s migraines are impacting on their home and work activities, and given the severity of symptoms, the emphasis is for an escalated prophylactic option, where the clinician may consider prescribing eptinezumab. In addition to improvements in MMDs, eptinezumab (300 mg, IV, maximum dose used during pivotal trials) has been shown to improve quality of life (QOL) in patients with EM and CM over 2 years. The PREVAIL study [17] demonstrated that treatment improved patient MIDAS questionnaire scores, the patient’s most bothersome symptoms (MBS) associated with migraine, patient global impression of change (PGIC), and the HIT-6 responses. These improvements were seen in patients with EM and CM after the first treatment, which were then either maintained or improved over time and with additional treatments [17]. In patients who have failed two to four previous prophylactic migraine medications (DELIVER study) [11], those treated with eptinezumab (100 mg and 300 mg) reported improvements in patient-reported outcomes (PROs) and quality-of-life measures compared with those treated with placebo [18]. Improvements in PROs were seen from 4 weeks. At week 12 and week 24 compared with placebo, treatment with eptinezumab (both doses) improved the PGIC score (p < 0.0001) and MBS (p < 0.0001). At week 12 and week 24 the percentage of patients with a ≥ 5-point reduction in HIT-6 total score were higher (p < 0.0001) in patients treated with eptinezumab (both doses) compared with placebo [18].
There is an increased prevalence of depression and anxiety in patients with MOH [3]. The clinician should continue to discuss interventions (therapeutic and non-therapeutic) which may assist the patient and where appropriate referrals should be made to support this patient, for example, to a psychologist or psychiatrist.
Ongoing Review and Management of Patients
Scenario 8 A patient attends a consultation after commencing treatment with eptinezumab. They report good effect from treatment, with the number of headache days per month and MMD recorded in their headache diary decreasing from 25 headache days and 25 migraine days per month to 8 headache days and 6 MMD. Decreases in the patient’s HIT-6 and MIDAS are also reported. The patient is concerned that over time they may experience an increase in headache days and MMDs. What advice can the clinician provide this patient? |
It is important to provide education to the patient regarding the importance of regular review. By providing regular review the clinician and treatment team can continue to provide ongoing education, reinforce new limitations on acute analgesics, promote treatment adherence, assess treatment efficacy, and provide ongoing patient support. For patients who have experienced MOH, it is particularly important to develop a regular follow-up plan in an effort to minimize the risk of relapse [7] and identify any concerns early.
In my clinic, patients who have received eptinezumab are followed up with after the first infusion by a headache specialist nurse (1 day and 2 weeks after) and have a consultant neurological review at 3 months. In general, many neurologists consult a patient at 3–monthly intervals supported by the patient’s headache diary. For patients who achieve event control, moving from CM to low-frequency EM, 12-monthly specialist review is adequate in conjunction with general practitioner care.
Conclusion
I note in this commentary the clinical complexity of managing patients with EM or CM and MOH. New treatments, including CGRP pathway mAb therapy such as eptinezumab in combination with other interventions, should be considered in patients who have had an inadequate response to other therapies. In my clinical practice, the CGRP pathway mAb therapy eptinezumab has been used successfully with rapid and lasting outcomes.
This article discusses off-label use of some medicines based on the author’s clinical experience. Healthcare professionals are strongly encouraged to review the Approved Product Information of any medicine before prescribing.
References
Vandenbussche N, Laterza D, Lisicki M, Lloyd J, Lupi C, Tischler H, et al. Medication-overuse headache: a widely recognized entity amidst ongoing debate. J Headache Pain. 2018;19(1):50.
Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211.
Diener HC, Marmura MJ, Tepper SJ, Cowan R, Starling AJ, Diamond ML, et al. Efficacy, tolerability, and safety of eptinezumab in patients with a dual diagnosis of chronic migraine and medication‐overuse headache: subgroup analysis of PROMISE-2. Headache. 2021;61(1):125–36.
Therapeutic Goods Administration. Eptinezumab (Vyepti) concentrated injection product information Canberra: Commonwealth Government of Australia; 2021. https://www.ebs.tga.gov.au.
Ho TW, Edvinsson L, Goadsby PJ. CGRP and its receptors provide new insights into migraine pathophysiology. Nat Rev Neurol. 2010;6(10):573–82.
Ray JC, Macindoe C, Ginevra M, Hutton EJ. The state of migraine: an update on current and emerging treatments. Aust J Gen Pract. 2021;50(12):915–21.
Sun-Edelstein C, Rapoport AM, Rattanawong W, Srikiatkhachorn A. The evolution of medication overuse headache: history, pathophysiology and clinical update. CNS Drugs. 2021;35(5):545–65.
Jenkins B. Migraine management. Aust Prescr. 2020;43(5):148–51.
Diener HC, Antonaci F, Braschinsky M, Evers S, Jensen R, Lainez M, et al. European Academy of Neurology guideline on the management of medication-overuse headache. Eur J Neurol. 2020;27(7):1102–16.
Goadsby P. The ‘Act When Mild’ (AwM) Study: a step forward in our understanding of early treatment in acute migraine. Cephalalgia. 2008;28(2_suppl):36–41.
Ashina M, Lanteri-Minet M, Pozo-Rosich P, Ettrup A, Christoffersen CL, Josiassen MK, et al. Safety and efficacy of eptinezumab for migraine prevention in patients with two-to-four previous preventive treatment failures (DELIVER): a multi-arm, randomised, double-blind, placebo-controlled, phase 3b trial. Lancet Neurol. 2022;21(7):597–607.
Dodick DW, Gottschalk C, Cady R, Hirman J, Smith J, Snapinn S. Eptinezumab demonstrated efficacy in sustained prevention of episodic and chronic migraine beginning on day 1 after dosing. Headache. 2020;60(10):2220–31.
Diener HC, Marmura MJ, Tepper SJ, Cowan R, Starling AJ, Diamond ML, et al. Efficacy, tolerability, and safety of eptinezumab in patients with a dual diagnosis of chronic migraine and medication-overuse headache: subgroup analysis of PROMISE-2. Headache. 2021;61(1):125–36.
Overeem LH, Peikert A, Hofacker MD, Kamm K, Ruscheweyh R, Gendolla A, et al. Effect of antibody switch in non-responders to a CGRP receptor antibody treatment in migraine: a multi-center retrospective cohort study. Cephalalgia. 2022;42(4–5):291–301.
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–858.
Deloitte Access Economics. Migraine in Australia whitepaper. Canberra: Deloitte Access Economics Report. 2018.
Kudrow D, Cady RK, Allan B, Pederson SM, Hirman J, Mehta LR, et al. Long-term safety and tolerability of eptinezumab in patients with chronic migraine: a 2-year, open-label, phase 3 trial. BMC Neurol. 2021;21(1):126.
Goadsby PJ, Barbanti P, Lambru G, Ettrup A, Christoffersen CL, Josiassen MK, et al. Eptinezumab improved patient-reported outcomes and quality of life in patients with migraine and prior preventive treatment failures. Eur J Neurol. 2022;20:1089–1098.
Acknowledgements
Funding
The development of this manuscript was supported funded by Lundbeck.
Medical Writing and/or Editorial Assistance
Lundbeck funded medical writing fees and all publication fees. The authors thank Elizabeth Hutchings RN PhD of WriteSource Medical Pty Ltd, Sydney, Australia, for providing medical writing support funded by Lundbeck Australia Pty Ltd in accordance with Good Publication Practice 2022 (GPP2022) guidelines (https://www.ismpp.org/gpp-2022).
Author Contributions
Nicole Limberg conceptualised, designed, and contributed to drafting the manuscript.
Disclosures
Nicole Limberg reports payments for advisory boards from AbbVie, Eli Lilly, TEVA, and Lundbeck.
Compliance with Ethics guidelines
This manuscript presents clinical scenarios based on Nicole Limberg’s clinical experience; therefore, Ethics Committee Approval was required. No original data was presented in this manuscript.
Data Availability
There is no data in this manuscript. All presented cases are hypothetical, as stated in the manuscript. Therefore, no data availability statement is needed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Limberg, N. Managing Migraine: Medication Overuse Headache and Treatment with Eptinezumab. Pain Ther 12, 1283–1291 (2023). https://doi.org/10.1007/s40122-023-00534-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-023-00534-w