Abstract
Introduction
There is limited real-world evidence on the burden of migraine among patients with prior preventive treatment failure (PPTF). In the BECOME Swiss subanalysis, we aimed to assess current prevalence of PPTF in patients with migraine seen at specialised headache centres in Switzerland and burden of migraine in these patients. Furthermore, we assessed this burden in subgroups stratified by monthly migraine days (MMDs) and number of PPTFs.
Methods
BECOME was a prospective, multicentre, non-interventional two-part study conducted in 17 countries across Europe and Israel. This subanalysis includes patients visiting ten headache specialist centres in Switzerland. In part 1, patients visiting the centres over 3 months were screened by physicians for frequency of PPTF, MMD and other migraine characteristics. Patients with ≥ 1 PPTF and ≥ 4 MMDs were invited to take part in part 2. The primary endpoint was the proportion of patients with ≥ 1 PPTF (part 1). Other endpoints included proportion of patients specified by number of PPTF and MMD (part 1, part 2), and impact of migraine on patient-reported outcomes (PROs; part 2).
Results
Patients (1677) from ten Swiss centres were included in part 1, of which 855 (51.0%) reported ≥ 1 PPTF. One hundred fifty-five patients were included in part 2: 6.5% reported ≥ 4 PPTFs and 43.2% reported ≥ 15 MMDs. Mean EuroQoL 5 and EuroQoL visual analogue scale (EQ-VAS) were 0.8 ± 0.2 and 69.6 ± 20.2, respectively, suggesting a mild level of impairment in the daily functioning and self-reported health of the patients. Mean six-item Headache Impact Test (HIT-6) and modified Migraine Disability Assessment (mMIDAS) scores were 63.3 ± 6.5 and 22.7 ± 21.8, respectively, corresponding to severe migraine burden. Patients also reported impairment in work-related productivity and general activities (48.6 ± 22.8) but no associations of anxiety (7.2 ± 4.4) or depression (6.0 ± 4.4) with migraine were noted. Burden of migraine increased with increasing frequency of PPTF and MMD.
Conclusions
Migraine-related quality of life, as well as work productivity are significantly affected in Swiss patients with migraine. Increasing migraine burden is associated with increasing migraine frequency and prior treatment failures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Many cross-sectional studies have been conducted in the Swiss population on various characteristics of migraine disorder. However, real-world prospective data on the prevalence and burden of migraine in patients with prior preventive treatment failure (PPTF) from Switzerland are limited. | |
This subgroup analysis of the prospective, multicentre, non-interventional two-part BECOME study assessed the burden and impact of migraine on patient-reported outcomes in patients with PPTF who visited ten headache specialist centres in Switzerland. | |
The analysis revealed high burden of migraine among Swiss patients with migraine, and the burden increased with increasing migraine frequency and number of PPTF. The impact of headache and disability due to migraine were severe. | |
Results from this study show the need for an effective treatment that reduces the disease burden and improves the wellbeing of patients with migraine. |
Introduction
Migraine is a debilitating neurological condition characterised by recurring attacks of headache and associated symptoms of hypersensitivity [1]. The Global Burden of Disease study estimated that 1.04 billion people had migraine in 2016, resulting in 45.1 million disability-adjusted life-years [2]. Globally, migraine is the second leading cause of years lived with disability among all age groups and the leading cause among those < 50 years of age [3, 4]. Migraine significantly impairs health-related quality of life (QoL) [5,6,7] and is associated with a high socioeconomic burden [8].
Multiple studies have established the high burden of migraine on QoL in patients unsuccessful with prior preventive therapies, either due to a lack of efficacy and/or tolerability [6, 7, 9, 10]. Furthermore, in Europe, patients with migraine often consult general or primary care physicians rather than specialists [6, 7, 11], despite high prevalence of prior preventive treatment failures (PPTFs) [12,13,14,15]. The treatment practices, reimbursement bodies and guidelines in Europe differ across countries, and it is therefore imperative to examine the local data of migraine in Swiss population [16]. Cross-sectional studies on various attributes of migraine or headache disorders were conducted across Swiss patients with migraine [17, 18], but prospective data on the real-world prevalence and burden of migraine in patients with PPTF from Switzerland are limited.
This subanalysis of the ‘Burden of migrainE in specialist headache Centres treating patients with prOphylactic treatMent failurE (BECOME)’ study [19] reports a cross-section of the real-world burden of migraine, including the impact of failure of preventive therapy, in patients visiting specialised headache centres in Switzerland.
Methods
Study Design
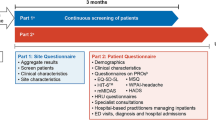
The design of the BECOME study has been detailed previously [19]. Briefly, BECOME was a two-part, prospective, non-interventional study conducted between 27 November 2017 and 5 October 2018 to assess the burden of migraine in patients with migraine attending specialised headache centres across 17 European countries and Israel. The study was restricted to specialised headache centres to ensure a more consistent diagnosis of disease within the screening population. In part 1, all patients with migraine visiting the study centres over a 3-month period were counted on a weekly basis, and clinical characteristics were collected. In part 2, patients with ≥ 1 PPTF and ≥ 4 monthly migraine days (MMDs) are identified and were invited to a single study visit within 14 days of consent. During the onsite visit, patient-specific data on clinical characteristics and burden of migraine were collected using validated questionnaires (Fig. 1). Here we report the subanalysis of the study from the Swiss population.
BECOME study design. aParts 1 and 2 of the study were conducted concurrently. bExperiencing migraine headache, time since diagnosis of migraine, migraine duration, reason for treatment failure, type of migraine, medication overuse, medication overuse headache, first visit to centre, follow-up visit to centre, inpatient, outpatient with ED visit, outpatient without ED visit. cIntended for all patients and completed within 1 day. BECOME Burden of migrainE in specialist headache Centers treating patients with preventive treatMent failurE, EQ-5D-5L EuroQol 5 dimensions, five-level questionnaire, HADS Hospital Anxiety and Depression Scale, HIT-6 six-item Headache Impact Test, MMD monthly migraine day, mMIDAS modified Migraine Disability Assessment, MSQ Migraine-Specific Quality of Life questionnaire, N total number of patients, PPTF prior preventive treatment failure, PRO patient-reported outcome, WPAI Work Productivity and Activity Index
Eligibility Criteria
For part 1, patients aged 18–65 years with migraine diagnosed prior to or on the day of the visit were included. Patients from part 1 could then proceed to part 2 if they had ≥ 4 MMDs in the previous 3 months (as per International Classification of Headache Disorders, third edition, beta version) [20], had evidence of efficacy failure in the past 5 years or tolerability failure, or were not suitable for at least one prophylactic treatment in a lifetime; and if they were newly seeking care or required treatment re-evaluation due to unsatisfactory treatment in the previous 3 months. Patients willing to answer all patient-reported outcome (PRO) questionnaires were identified by the investigators and enrolled. Participation in any interventional migraine study precluded inclusion.
Endpoints
The primary endpoint of the study (part 1) was the proportion of patients with at least one PPTF among all patients visiting the specialised headache centres during the 3-month observation period. Other part 1 endpoints included the proportion of patients with migraine stratified by frequency of MMDs (< 4, 4–7, 8–14, ≥ 15), PPTFs (0, 1, 2, 3 or ≥ 4), new versus follow-up visit, and by medication overuse. In part 2, clinical characteristics of all patients and PRO questionnaires [EuroQoL 5 dimensions 5 level (EQ-5D-5L), Headache Impact Test-6 (HIT-6), modified Migraine Disability Assessment (mMIDAS), Migraine-Specific Quality of Life (MSQ, Work Productivity and Activity Impairment for headache (WPAI-headache), and Hospital Anxiety and Depression Scale (HADS)] including total scores and domain scores were assessed in the overall population and by subgroups of PPTF, MMD, disease duration and medication overuse headache (MOH).
Health status was assessed using the EQ-5D-5L questionnaire [21]. The EQ-5D-5L consists of a descriptive system and the EuroQoL visual analogue scale (EQ-VAS). The descriptive system assesses the functioning of a patient in five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression, each at five levels (no problems, slight problems, moderate problems, severe problems and extreme problems). Patients’ responses were pooled and a weighted EQ-5D index score derived, which represents the overall health status with a possible range from 0 to 1. The EQ-VAS assesses patients’ self-reported health on a scale ranging from 0 (worst imaginable health) to 100 (best imaginable health). Higher scores on the index score and VAS indicate better health status.
Headache-related disability was assessed using the mMIDAS questionnaire [22]. The MIDAS is a five-item self-administered questionnaire that assesses headache-related disability of a patient over a 3-month period incorporating missed days of work, missed household chores, missed non-work activity and at least 50% reduced productivity at professional or personal work. The MIDAS scores are categorised into four grades [grade I for minimal or infrequent disability (0–5), grade II for mild or infrequent disability (6–10), grade III for moderate disability (11–20) and grade IV for severe disability (21+)]. The higher the score, the higher the disability as a result of headache. Since BECOME was a non-interventional cross-sectional study, an mMIDAS questionnaire with a recall period of 1 month (as opposed to 3 months) was used. For consistency of reporting with the universal MIDAS score (recall period of 3 months), the mMIDAS total score in this study was multiplied by three.
The adverse impact of headache was assessed using the HIT-6 questionnaire [23]. The self-administered questionnaire measures the adverse impact of headache on a patient at any time point using six items: headache pain, social functioning, role functioning, vitality, cognitive functioning and psychological distress. The pooled scores of six items are used to derive the total HIT-6 score ranging from 36 to 78 and categorised into four severity categories [little or no impact (≤ 49), some impact (50–55), substantial impact (56–59) and severe impact (60–78)]. The higher the score, the greater the impact of headache on daily life. Daily work activity and emotional function was assessed using the MSQ questionnaire [24]. The 14-item MSQ measures the impact of migraine on QoL of the patient in three domains: role function-restrictive (RFR, how migraines limit daily social and work‐related activities), role function-preventive (RFP, how migraines prevent daily social and work‐related activities) and emotional function (EF, emotions associated with migraines). Patient’s response scores to each domain at six levels are pooled and rescaled on a 0–100 scale, where higher scores indicate better QoL.
Anxiety and depression as a result of migraine were assessed using the HADS questionnaire [25]. The HADS questionnaire consists of HADS-Anxiety and HADS-Depression subscales, with seven items each. The scale detects the subjective experience of anxiety and depression during the preceding week, rated on 0 to 3 (maximum symptom severity) levels for each of the seven items. The sum of each subscale (score range 0–21) is used to indicate normal (0–7), suggested presence (score 8–10) or probable presence (score ≥ 11) of anxiety or depression. Any impairment of work or daily activity experienced by the patient was assessed using the WPAI questionnaire [26]. The self-administered WPAI instrument assesses the impact of migraine on patients’ work and activity impairment in the previous 7 days. Patient’s response scores to four metrics [absenteeism (% work time missed due to health), presenteeism (% impairment at work due to health), work productivity loss (combined absenteeism and presenteeism impairment estimate) and activity impairment (% impairment in daily activities due to health)] are pooled and rescaled on a scale of 0–100, where higher scores indicate higher impairment.
Statistical Analysis
No statistical hypothesis testing, or inferential statistical analysis were performed in the study. Patient characteristics and PRO data were descriptively summarised. Absolute numbers and relative frequencies were used to present categorical data. Statistical analyses were conducted using Statistical Analysis System software (SAS version 9.4.3).
Ethics Approval
The study was conducted in accordance with the Guidelines for Good Pharmacoepidemiology Practices of the International Society for Pharmacoepidemiology [27] and with the ethical principles laid down in the Declaration of Helsinki. The study protocol, informed consent form and questionnaires were reviewed and approved by an independent ethics committee or the relevant institutional review board at all participating centres (Table S1 in the supplementary material). All participants provided informed consent prior to enrollment in the study.
Results
A total of 1677 patients presented at ten specialised headache centres in Switzerland during the 3-month prospective period and were enrolled in part 1 of the study. Of these, 155 patients with ≥ 1 PPTF and ≥ 4 MMDs were identified by the investigators and enrolled in part 2 (Table 1).
Study Population in Part 1
Among the 1677 patients, 1050 (62.6%) patients attended the specialised headache centres as follow-up visits, and 627 (37.4%) were visiting for the first time (Table 1); 855 (51.0%) patients reported ≥ 1 PPTF and 139 (8.3%) reported ≥ 4 PPTFs. Overall, 1046 (62.4%) patients reported ≥ 4 MMDs and 260 (15.5%) met the criteria for a diagnosis of chronic migraine (CM) (≥ 15 headache days per month, of which ≥ 8 were MMDs) (Fig. 2). MOH was reported by 204 (12.2%) patients (Table 1).
Frequency of patients with PPTF (A and C), MMD (B and D) in part 1 (n = 1677) and part 2 (n = 155), and frequency of patients with MMD by number of PPTFs in part 2 (n = 155) (E). a ≥ 15 headache days per month with ≥ 8 MMDs. MMDs monthly migraine days, N total number of patients, n number of patients, PPTF prior preventive treatment failure
Study Population in Part 2
The mean ± standard deviation (SD) age of patients was 40.0 ± 13.0 years (Table 1). One hundred twenty-eight (82.6%) participants were female and 56.1% (n = 87) were employed. The most common types of migraine diagnosed in this population were migraine without aura (65.2%), migraine with aura (20.6%) and CM (7.1%). Among 155 patients, a total of 103 (66.5%) patients had presented for follow-up visit, 115 (74.2%) were from non-emergency outpatient clinics, 22 (14.2%) presented at emergency outpatient clinic, 49 (31.6%) had MO and 37 (23.9%) had MOH. Overall, patients reported an average 22.0 ± 13.3 years of migraine history, and 15.4 ± 11.7 years from the first diagnosis (Table 1), suggesting a delay in diagnosis of migraine by 6.6 years. A total of 264 treatment failures were reported, of which 150 (56.8%) were due to efficacy failure (Table 1). Only one PPTF was reported by 89 (57.4%) patients and ≥ 4 PPTF by 10 (6.5%). Fifty-nine (38.1%) patients met the criteria for CM (Fig. 2) and five (8.5%) of them reported ≥ 4 PPTFs (Table 2).
Burden of Disease in Part 2
Table 3 presents the mean ± SD score of PROs assessed during study visit. The impairment of health status and self-reported health as measured by EQ-5D-5L utility index score and EQ-VAS were 0.8 ± 0.2 and 69.6 ± 20.2, respectively. The impact of headache on daily life and disability because of migraine, assessed using HIT-6 and mMIDAS scores, were 63.3 ± 6.5 and 22.7 ± 21.8, respectively.
Among the three domains of the MSQ, patients reported mean ± SD higher scores for daily activities in the RFP domain (63.2 ± 23.3) compared with daily social and work-related activities and emotions in the RFR and EF domains (48.6 ± 22.8 and 54.5 ± 27.0, respectively). The WPAI-headache score was lowest in the domain reflecting absenteeism and similar across the domains representing presenteeism, work productivity loss and activity impairment. The study population reported both anxiety and depression because of headache, reflected by the HADS overall score (13.2 ± 8.1).
Burden of Disease by Subgroups
The PRO scores of the part 2 population were also analysed by various subgroups. Greater reductions in EQ-5D utility and EQ-VAS scores were seen with increasing numbers of PPTF beyond 1 PPTF (Fig. 3). Similarly, higher number of PPTF was associated with higher HIT-6 and mMIDAS scores. Furthermore, the impact of migraine on the MSQ, WPAI and HADS scores was worse with subsequent versus first treatment failure.
Scores of patient-reported outcomes of part 2 population, by treatment failure (n = 155). For explanations and ranges of these scores, consult the Methods section. Dotted line indicates the threshold score of ‘severity’ for the individual patient-reported outcome measure. EF emotional functioning, EQ-5D-5L EuroQol 5 dimensions, five-level questionnaire, EQ-VAS EuroQol visual analogue scale, HADS Hospital Anxiety and Depression Scale, HIT-6 six-item Headache Impact Test, mMIDAS modified Migraine Disability Assessment, MSQ Migraine-Specific Quality of Life questionnaire, N total number of patients, n number of patients, RFP, role function-preventive, RFR role function-restrictive, TF treatment failure, WPAI Work Productivity and Activity Impairment
Similar to the higher PPTF subgroups, increasing frequency of MMD was associated with worse PRO scores (Fig. 4). However, those with greater disease duration (15–28 years and > 28 years of disease duration) reported higher scores on the functioning and health status questionnaires, lower impact of headache on daily life, lower disability because of migraine, higher scores across all domains of the MSQ and lower scores in the WPAI scale as well as HADS scales (Fig. 5). Similarly, patients with MOH reported higher EQ-5D utility, EQ-VAS and MSQ scores across all domains, and lower HIT-6, mMIDAS scores, WPAI and HADS scores compared with those without MOH (Fig. 6).
Scores of patient-reported outcomes of part 2 population, by frequency of MMD (n = 155). For explanations and ranges of these scores, consult the Methods section. Dotted line indicates the threshold score of ‘severity’ for the individual patient-reported outcome measure. EF emotional functioning, EQ-5D-5L EuroQol 5 dimensions, five-level questionnaire, EQ-VAS EuroQol visual analogue scale, HADS Hospital Anxiety and Depression Scale, HIT-6 six-item Headache Impact Test, mMIDAS modified Migraine Disability Assessment, MMD monthly migraine day, MSQ Migraine-Specific Quality of Life questionnaire, N total number of patients, n number of patients, RFP role function-preventive, RFR role function-restrictive, WPAI Work Productivity and Activity Impairment
Scores of patient-reported outcomes of part 2 population, by disease duration (n = 155). For explanations and ranges of these scores, consult the Methods section. Dotted line indicates the threshold score of ‘severity’ for the individual patient-reported outcome measure. EF emotional functioning, EQ-5D-5L EuroQol 5 dimensions, five-level questionnaire, EQ-VAS EuroQol visual analogue scale, HADS Hospital Anxiety and Depression Scale, HIT-6 six-item Headache Impact Test, mMIDAS modified Migraine Disability Assessment, MSQ Migraine-Specific Quality of Life questionnaire, N total number of patients, n number of patients, RFP role function-preventive, RFR role function-restrictive, WPAI Work Productivity and Activity Impairment
Scores of patient-reported outcomes of part 2 population, by MOH (n = 155). For explanations and ranges of these scores, consult the Methods section. Dotted line indicates the threshold score of ‘severity’ for the individual patient-reported outcome measure. EF emotional functioning, EQ-5D-5L EuroQol 5 dimensions, 5 levels questionnaire, EQ-VAS EuroQol visual analogue scale, HADS Hospital Anxiety and Depression Scale, HIT-6 six-item Headache Impact Test, mMIDAS modified Migraine Disability Assessment, MOH medication overuse headache, MSQ Migraine-Specific Quality of Life questionnaire, N total number of patients, n number of patients, RFP role function-preventive, RFR role function-restrictive, WPAI Work Productivity and Activity Impairment
Comparison between Swiss Cohort and Overall Cohort
This analysis only includes data from Switzerland, but the BECOME study was conducted in 17 countries in Europe and Israel [19]. Here we compare severity and burden of disease in the Swiss cohort with the overall cohort.
Severity of the Disease
Compared with the overall cohort, the Swiss cohort showed a numerically lower proportion of patients with ≥ 4 PPTFs (part 1 and part 2), ≥ 1 PPTF, ≥ 4 MMDs and CM (Table 4).
Burden of Disease
Most of the demographic characteristics in part 2, including the mean time since first headache, were comparable between the Swiss and overall cohort (22.0 years versus 23.5 years). Also, the mean time since diagnosis of migraine was comparable between the Swiss and overall cohorts (15. 4 years versus 15.7 years). All the PRO outcomes within the Swiss cohort were comparable to those of the overall cohort. In line with the overall cohort, increasing number of PPTFs was associated with greater reductions in the mean EQ-5D utility (0.8 Swiss versus 0.8 overall cohort) and mean EQ-VAS scores (69.6 Swiss versus 67.3 overall cohort). The same observation was made with increasing number of MMD. In both cohorts, higher PPTFs and MMDs were associated with higher HIT-6 and mMIDAS scores. Similarly, the impact of migraine on the MSQ, WPAI and HADS scores was worse with increasing number of PPTF and MMDs in both cohorts.
Discussion
The results of this Swiss subanalysis of the BECOME study exclusively focuses on current prevalence of PPTF, and burden of migraine in patients visiting ten specialised headache centres in Switzerland. Slightly more than 50% of patients reported at least one PPTF and 62.4% reported ≥ 4 MMDs in part 1. The PROs measured on various scales revealed low QoL, severe impact and disability because of migraine, and limitations on social and work-related activities among patients with prior treatment failure (part 2).
Previous studies in the Swiss population have reported prevalence and burden of migraine in small or community-based cohorts [17, 18]. The current study reveals a high burden of disease among a representative Swiss cohort visiting specialised headache centres, spanning ten cities across the country. The prevalence of CM (≥ 15 days of headache with ≥ 8 MMDs) in 15.5% of the study population is considerably higher than the 8.8% reported in a general population from the USA, reflecting selection of more severe clinical cases at tertiary headache centres [28].
Among patients with ≥ 1 PPTF (part 2), a high proportion (66.5%) had more than one visit (follow-up) to a specialised headache centre, indicating the severity of the disease. Conversely, the other third of patients (33.5%) with ≥ 1 PPTF made their first visit to a specialist centre due to lack of treatment benefit (lower efficacy of medication or unsatisfactory therapeutic effect) at primary care centres. This signifies an unmet medical need for appropriate management of patients with prior treatment failure, further supported by a higher proportion of efficacy vs safety failures (56.8% versus 42.0%). The relative contributions of efficacy and safety to treatment failure reported here are consistent with the findings from a previous study on migraine-preventive medication [29].
For the overall health improvement of patients with migraine, in addition to reduction in MMDs, it is essential to evaluate disease attributes such as QoL; impact and disability because of migraine; emotional and physical functioning; reduction in the use, severity and duration of migraine-specific acute drugs; and work productivity among patients. In this study, we employed a number of PROs to capture multiple aspects of the migraine disease burden and so gain a comprehensive assessment of the impact of migraine on health.
In this study, among six PRO measures assessing the burden of migraine on patients’ lives, three were generic and three were specific to migraine. The EQ-5D-5L utility index and EQ-VAS scores were closer to the best imaginable health status, indicating a mild level of impairment in the daily functioning and self-reported health of the patients. The mean HIT-6 (63.3 ± 6.5) and mMIDAS score (22.7 ± 21.8) reveal the severe impact of headache on daily life and disability because of migraine experienced by these patients, which is also reflected by the high proportion of patients attending the specialised centres for follow-up visits (66.5%). Overall, the study population scores on three domains of QoL were balanced with higher scores in the daily activities’ domain and slightly lower scores in the daily social and work-related activity and EF domains. While most of the patient-reported measures on the burden of disease reported by the Swiss cohort are in line with findings from recent studies conducted in European population with migraine [6, 7, 29], the normal levels of anxiety and depression are an unexpected observation in this difficult-to-treat population.
Furthermore, the PRO measures showed higher burden of migraine with increasing MMD frequency, and MOH. However, the uneven variations in scores observed in certain PRO measures among subgroups of patients with PPTF may be a result of the lower number of patients in subgroups with three and four PPTFs (14 and 10, respectively) compared with subgroups with one and two PPTFs (89 and 42, respectively). The findings on the PRO questionnaires in patients with one PPTF are in line with a recent survey reports on burden of migraine, collected via internet and mobile applications, among a representative European population surveyed from 11 countries [6, 7].
The BECOME study identified a high prevalence of PPTF among patients visiting headache centres in Europe and Israel, and that migraine had a severe impact on patients’ QoL including personal, professional and social activities. In the BECOME Swiss subanalysis, the impact of migraine on health-related quality of life was mild. However, on migraine-specific measures, it severely impacted their daily social and work-related activities. Though no statistical test between the overall cohort (n = 20,837) and the Swiss cohort (n = 855) were undertaken to compare, the latter was characterised by a numerically smaller proportion of patients with severe migraine than the overall cohort. A correlation between an increasing burden of migraine and MMD frequency and PPTFs was observed in both the overall and Swiss cohorts.
Limitations
The limitations of the study are, to an extent, those of the BECOME primary study [19]. The BECOME study was conducted in patients visiting specialised headache centres and so reflects only a selected population of patients with migraine. The results may not be representative of the overall migraine population managed in general clinics and those who consult with general physicians in primary healthcare settings across the country. Furthermore, the findings from the current analysis cannot be compared with the findings from the BECOME primary study, conducted across 17 countries from Europe and Israel [19]. As with any non-interventional study, recall bias may be a factor for self-reported elements of PROs. Hence, the QoL data need to be interpreted with caution.
Conclusions
The Swiss subanalysis of the BECOME study in patients with migraine who failed at least one prior preventive treatment confirms a high burden of disease, which increases with frequency of monthly migraine days as well as number of treatment failures. There is a continuing need for improved pharmacological and non-pharmacological therapies to reduce the disease burden and ameliorate QoL.
References
Arnold M. Headache classification committee of the international headache society (IHS) the international classification of headache disorders. Cephalalgia. 2018;38(1):1–211.
Feigin VL, Nichols E, Alam T, Bannick MS, Beghi E, Blake N, et al. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):459–80.
Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–59.
Steiner TJ, Stovner LJ, Vos T, Jensen R, Katsarava Z. Migraine is first cause of disability in under 50s: will health politicians now take notice?. Springer; 2018. p. 1–4.
Steiner TJ, Stovner LJ, Katsarava Z, Lainez JM, Lampl C, Lantéri-Minet M, et al. The impact of headache in Europe: principal results of the Eurolight project. J Headache Pain. 2014;15(1):1–11.
Martelletti P, Schwedt TJ, Lanteri-Minet M, Quintana R, Carboni V, Diener H-C, et al. My Migraine Voice survey: a global study of disease burden among individuals with migraine for whom preventive treatments have failed. J Headache Pain. 2018;19(1):1–10.
Vo P, Paris N, Bilitou A, Valena T, Fang J, Naujoks C, et al. Burden of migraine in Europe using self-reported digital diary data from the migraine buddy© application. Neurol Therapy. 2018;7(2):321–32.
Agosti R. Migraine burden of disease: From the patient's experience to a socio‐economic view. Headache J Head Face Pain. 2018;58:17–32
Huber CA, Agosti R, Näpflin M, Blozik E. Treatment patterns in patients using triptan and prophylactic medication: an analysis of clinical practice prior to the introduction of CGRP antagonists. J Pain Res. 2019;12:2211.
Ruscheweyh R, Müller M, Blum B, Straube A. Correlation of headache frequency and psychosocial impairment in migraine: a cross‐sectional study. Headache: J Head Face Pain. 2014;54(5):861–71
Bloudek L, Stokes M, Buse D, Wilcox T, Lipton R, Goadsby P, et al. Cost of healthcare for patients with migraine in five European countries: results from the International Burden of Migraine Study (IBMS). J Headache Pain. 2012;13(5):361–78.
Kainth P, Murphy N, Rossi S, Talabardon J-N, Pedrazzoli M, Mascagni L, et al. Management of migraine and the accessibility of specialist care—findings from a multi-national assessment of 28 healthcare networks. Eur Neurol Rev. 2018;13(2):103–10.
Schramm S, Uluduz D, Gouveia RG, Jensen R, Siva A, Uygunoglu U, et al. Headache service quality: evaluation of quality indicators in 14 specialist-care centres. J Headache Pain. 2016;17(1):1–14.
Tassorelli C, Farm I, Kettinen H, de la Torre ER, Stretenovic S, Thomas W, et al. Access to care-an unmet need in headache management? J Headache Pain. 2014;15(1):1–4.
Katsarava Z, Mania M, Lampl C, Herberhold J, Steiner TJ. Poor medical care for people with migraine in Europe–evidence from the Eurolight study. J Headache Pain. 2018;19(1):1–9.
World Health Organization. Regional office for Europe, European observatory on health systems and policies, De Pietro, Carlo, Camenzind, Paul, Sturny, Isabelle. et al. (2015). Switzerland: health system review. World Health Organization. Regional Office for Europe. https://apps.who.int/iris/handle/10665/330252
Sokolovic E, Riederer F, Szucs T, Agosti R, Sándor PS. Self-reported headache among the employees of a Swiss university hospital: prevalence, disability, current treatment, and economic impact. J Headache Pain. 2013;14(1):1–8.
Maercker A, Perkonigg A, Preisig M, Schaller K, Weller M. The costs of disorders of the brain in Switzerland: an update from the European Brain Council Study for 2010. Swiss Med Week. 2013;143 (online)
Pozo-Rosich P, Lucas C, Watson DP, Gaul C, Ramsden E, Ritter S, et al. Burden of migraine in patients with preventive treatment failure attending european headache specialist centers: real-world evidence From the BECOME study. Pain Ther. 2021;10(2):1691–708.
The International Classification of Headache Disorders. 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808.
Xu R, Insinga RP, Golden W, Hu XH. EuroQol (EQ-5D) health utility scores for patients with migraine. Qual Life Res. 2011;20(4):601–8.
Yang M, Rendas-Baum R, Varon SF, Kosinski M. Validation of the Headache Impact Test (HIT-6™) across episodic and chronic migraine. Cephalalgia. 2011;31(3):357–67.
Kosinski M, Bayliss M, Bjorner J, Ware J, Garber W, Batenhorst A, et al. A six-item short-form survey for measuring headache impact: the HIT-6™. Qual Life Res. 2003;12(8):963–74.
Bagley CL, Rendas‐Baum R, Maglinte GA, Yang M, Varon SF, Lee J, et al. Validating migraine‐specific quality of life questionnaire v2. 1 in episodic and chronic migraine. Headache J Head Face Pain. 2012;52(3):409–21.
Snaith RP. The hospital anxiety and depression scale. Health Qual Life Outcomes. 2003;1(1):1–4.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–65.
Guidelines for good pharmacoepidemiology practices (GPP). Pharmacoepidemiol Drug Saf. 2008;17(2):200–8.
Adams AM, Serrano D, Buse DC, Reed ML, Marske V, Fanning KM, et al. The impact of chronic migraine: the chronic migraine epidemiology and outcomes (CaMEO) study methods and baseline results. Cephalalgia. 2015;35(7):563–78.
Hepp Z, Dodick DW, Varon SF, Chia J, Matthew N, Gillard P, et al. Persistence and switching patterns of oral migraine prophylactic medications among patients with chronic migraine: a retrospective claims analysis. Cephalalgia. 2017;37(5):470–85.
Acknowledgements
We would like to express our gratitude to all study participants. We thank the BECOME study steering committee members: David Watson, Paolo Martelletti, Patricia Pozo-Rosich, Charly Gaul, Christian Lucas. We thank all participating study sites (principal investigators): Cabinet Dozier Carouge (C. Dozier), Cabinet Myers Geneva (P. Myers), Centre Hospitalier Universitaire Vaudois (P. Ryvlin), Kantonsspital Aarau (O. Findling), Kantonsspital St. Gallen (D. Flügel), Kopfwehzentrum Hirslanden Zürich (R. Agosti), Neurologie am Schaulager Münchenstein (M. Stallmach), Ospedale Regionale di Lugano (C. Zecca), RehaClinic Bad Zurzach (A. Gantenbein), Universitätsspital Zürich (J. A. Petersen).
Funding
The study was funded and supported by Novartis Pharma AG and Novartis Pharma Schweiz AG, Switzerland. Novartis will sponsor the journal’s Rapid Service Fees.
Medical Writing Assistance
Medical writing support for the manuscript was provided by Sashi Kiran Goteti, Rohita Sri Gattoju, and Praful Narayan Kamble of Novartis Healthcare Pvt. Ltd, Hyderabad, India, which was funded by Novartis Pharma AG, Basel, Switzerland, in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Authorship
All named authors meet the International Committee of Medical Journal Editors criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors’ Contributions
All authors have made substantial contributions to the study concept, design, data collection, and/or analysis of the research; the drafting of the manuscript; and have reviewed and accepted the contents of the manuscript prior to its submission.
Disclosures
Reto Agosti has received honoraria for advisory board participation and lectures from Novartis, Lilly, Teva/Mepha, Abbvie, Allergan, Merz, Almirall, and Biogen. Catherine Parzini has nothing to disclose. Oliver Findling has received honoraria for lectures and advisory board participation as well as research and travel support from Biogen, Novartis, Almirall, Bayer Schweiz AG, Teva, Merck, Sanofi Genzyme, Roche, and the Swiss MS Society. Peter Myers has nothing to disclose. Jens A. Petersen received honoraria for research and advisory board participation from Novartis, Almirall, and Eli Lilly. Philippe Ryvlin has received speaker or consulting fees from Novartis and Eli Lilly. Peter Sandor has nothing to disclose. Matthias Stallmach has received honoraria for advisory board participation and lectures as well as travel support from Biogen, Novartis, Roche, Sanofi, Teva and DePuy Synthes. Chiara Zecca, Ente Ospedaliero Cantonale (employer) received compensation for C.Z.’s speaking activities, consulting fees, or research grants from Almirall, Biogen Idec, Bristol Meyer Squibb, Lundbeck, Merck, Novartis, Sanofi, Teva Pharma, Roche. CZ is recipient of a grant for senior reseachers provided by AFRI (Area Formazione accademica, Ricerca e Innovazione), and EOC. Josefin Snellman and Shannon Ritter are employees of Novartis and hold stocks in Novartis. Michael E. Arzt is an employee of Novartis. Simon Rohrer was an employee of Novartis during study conduct. Andreas R. Gantenbein has received honoraria for lectures and consulting fees from Allergan, Almirall, Curatis, Eli Lilly, Grünenthal, Lundbeck, Mepha/Teva, Novartis and Sanofi.
Compliance with Ethics Guidelines
The study was approved by an independent ethics committee or relevant institutional review board at all participating centres and conducted in accordance with the ethical principles laid down in the Declaration of Helsinki. All participants provided informed consent before study initiation.
Data Availability
De-identified study data may be made available on request to researchers who submit a proposal that is approved by the principal investigator.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Agosti, R., Parzini, C., Findling, O. et al. Prevalence and Burden of Migraine in Switzerland: Cross-Sectional Study in ten Specialised Headache Centres from the BECOME Study. Pain Ther 12, 575–591 (2023). https://doi.org/10.1007/s40122-023-00484-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-023-00484-3