Abstract
Introduction
Thoracic paravertebral block (TPVB) and subcostal transverse abdominis plane block (TAP) have been considered to provide an effective analgesic effect for laparoscopic and thoracoscopic surgery, respectively. The purpose of this randomized, controlled, and prospective study was to evaluate the analgesic effect of TPVB combined with TAP in patients undergoing total minimally invasive Mckeown esophagectomy.
Methods
Between February 2020 and December 2021, a total of 168 esophageal cancer patients undergoing McKeown esophagectomy at the Cancer Center of Sun Yat-Sen University, China, were randomly assigned to receive patient-controlled epidural analgesia alone (group PCEA, n = 56), patient-controlled intravenous analgesia alone (group PCIA, n = 56), and TPVB combined with TAP and patient-controlled intravenous analgesia (group PVB, n = 56). The primary outcome was a visual analogue scale (VAS) pain score on movement 48 h postoperatively. Secondary endpoints were pain scores at other points, intervention-related side effects, surgical complications, and length of intensive care unit and hospital stay. For the VAS pain score, the Kruskal–Wallis method was conducted for comparison of 3 treatment groups and further pairwise comparison with Bonferroni correction.
Results
On movement, the VAS in the PVB group was higher than that in the PCEA group at 48 h, 72 h, 96 h, and 120 h postoperatively (p < 0.05) except in the postoperative anesthesia care unit (PACU) and 24 h postoperatively. The VAS in the PCIA group was higher than the PCEA and PVB groups in the first 4 days after surgery. The pulmonary complication rate in the PCIA group was significantly higher than the rate in the PCEA [95% Confidence Interval 0.214 (0.354, 0.067), p = 0.024].
Conclusions
Combined TPVB and TAP was more effective than intravenous opioid analgesia alone, while PCEA was more effective than TPVB combined with TAP and intravenous opioid analgesia for patients after McKeown esophagectomy.
Trial Registration
Chinese Clinical Trial Registry; ChiCTR2000029588.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
More and more patients will benefit from thoraco-laparoscopic esophagectomy, as it appears to be associated with reduced pain. Even though it is considered to be a less invasive procedure, patients after thoracoscopic surgery also experience moderate-to-severe pain. |
Thoracic paravertebral block (TPVB) and subcostal transverse abdominis plane block (TAP) have been considered to provide effective analgesic effects for laparoscopic and thoracoscopic surgery, respectively. |
We hypothesized that, in McKeown esophagectomy, TPVB combined with TAP was superior to thoracic epidural analgesia (TEA) and intravenous opioid analgesia for postoperative anaesthesia. |
What was learned from the study? |
The adjunct of TEA or TPVB combined with TAP with general anesthesia could significantly relieve postoperative pain for patients after McKeown esophagectomy. |
PCEA was more effective than TPVB combined with TAP and intravenous opioid analgesia for patients after McKeown esophagectomy. |
The use of a multimodal analgesia program based on a TPVB combined with TAP block was a viable alternative to TEA for total minimally invasive McKeown esophagectomy. |
Introduction
McKeown esophagectomy [1] is a common procedure for nonmetastatic esophageal cancer. It is a cervico-thoraco-abdominal procedure, and the wound extends to these three regions, making postoperative pain control difficult. Good pain control with adequate medication facilitates thoracic wall mobility and expansion [2, 3], which allows good pulmonary function and early mobilization after surgery. This contributes to a reduction in pulmonary complications after esophagectomy [3, 4].
In China, postoperative intravenous analgesia with opioids is the most common, but the analgesic effect is rather poor. Thoracic epidural analgesia (TEA) has been considered the gold standard for postoperative pain management after esophagectomy [5]. Although it is an effective mode of pain control, epidural analgesia has some limitations, such as a high failure rate and serious complications [6,7,8,9]. Currently, most esophagectomies are performed via a minimally invasive approach [10]. With the development of endoscopic technology and the accumulation of experience of thoracic surgeons, more and more patients will benefit from thoracoscopic laparoscopic esophagectomy [11], as it appears to be associated with reduced pain. Blackshaw et al. believed that the prognosis of thoracic surgery combined with paravertebral block (PVB) is not worse than that of thoracic surgery combined with TEA [12]. Levy et al. found that transverse abdominis plane (TAP) blocks and patient-controlled intravenous analgesia (PCIA) are another choice for pain control in patients undergoing esophagectomy, which can reduce hypotension and volume resuscitation requirements for similar pulmonary complications [13]. Expected advantages of an ultrasound-guided nerve block include a higher successful rate of the nerve block, improving the degree and duration of the block [14]. However, few studies have evaluated the analgesic effects of combined ultrasound-guided TPVB with TAP in patients undergoing total minimally invasive Mckeown esophagectomy. To date, only one retrospective study [15] has investigated the early postoperative analgesic effects of PVB in combination with subcostal TAP block in patients undergoing minimally invasive esophagectomy (MIE) for esophageal cancer. However, the small sample size and the retrospective study design could have made the clinical effect of blocks in the immediate postoperative period not readily apparent and thus limited the interpretation.
This randomized, controlled, and prospective study aimed to compare the analgesic efficacy of combined TPVB with TAP, TEA, and intravenous analgesia following thoraco-laparoscopic McKeown esophagectomy. The clinical significance of this study is to provide clinicians with a new multi-mode analgesia, and so relieve pain for patients. In addition, more controlled studies are required to substantiate the effects of combined TPVB and subcostal TAP block on patients receiving MIE.
Methods
Patients
This study was a randomized, controlled, and prospective trial. A total of 177 patients scheduled to undergo thoraco-laparoscopic McKeown esophagectomy at the Cancer Center of Sun Yat-Sen University, China, were provided with written information prior to surgery. A total of 168 patients completed the study from February 2020 to December 2021. Written informed consent was obtained on the morning of surgery. Patients were randomly allocated to receive patient-controlled epidural analgesia alone (group PCEA, n = 56), patient controlled intravenous analgesia alone (group PCIA, n = 56), and TPVB combined with TAP and patient-controlled intravenous analgesia (group PVB, n = 56) group with a computer-generated randomization sequence (http://www.randomization.com).
Eligible patients were 18 years of age or older and undergoing thoraco-laparoscopic McKeown esophagectomy. Exclusion criteria were a known contra-indication to either epidural or local anesthetic, inability to give informed consent, open resections, patients with a history of chronic pain issues requiring a regular opioid analgesia sequence with concealed allocation, lack of suitability for single lung ventilation, prior lung surgery, or psychological, family, social factors, and patient refusal that led to an absence of informed consent.
Ethics
Ethical approval for this study (B2019-163) was provided by the Ethics Committee of Cancer Center of Sun Yat-Sen University, Guangzhou City, Guangdong Province, China. The trial was registered in the Chinese Clinical Trial Registry (ChiCTR2000029588, Principal investigator: Renchun Lai, Date of registration: 2020-02-16). The study was in accordance with the Declaration of Helsinki and its later amendments.
Randomization
According to a computer-generated random sequence, once eligibility was confirmed, the patients were randomly assigned in a 1:1:1 ratio into 1 of the 3 groups by using the block randomization method by anesthetists who did not perform the anesthesia protocol for this study. Sequentially numbered, opaque sealed envelopes were used to maintain allocation concealment. Postoperative assessment was performed by the nursing staff who were blinded to the patients’ group.
Analgesic Technique
For the PCEA group, an epidural catheter was inserted between T6 and T9 using a standard technique according to institutional practices. Before the surgical incision was made, 10–20 ml of 0.2% ropivacaine was administered incrementally through the epidural catheter to establish a block. The epidural analgesia regimen for the PCEA group was 0.15% ropivacaine and 0.12 mg/kg morphine with normal saline (NS) to 100 ml, 2 ml/h with a 4-ml bolus, and a lockout time of 60 min.
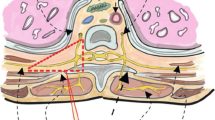
All patients randomized to the PVB group received ultrasound-guided TPVB before the operation. With the patient in a lateral decumbent position and the skin sterilized, we performed T4 and T7 PVB with 0.33% ropivacaine 15 ml at each level, respectively, with a L38 linear ultrasound probe (Sonosite Micromaxx, Bothell, WA, USA) in a sagittal plane from medial to lateral at the mid-thoracic level.
The TAP blocks included both a lateral approach and subcostal TAP blocks placed according to the New York Society of Regional Anesthesia for bilateral TAP blocks [16]. Before the abdominal operation, with patients in the supine position, by using an in-plane approach, a broadband linear array probe (Sonosite Micromaxx) with a frequency of 5–10 MHz was placed in the clavicle midline, a 22-G 100-mm needle was inserted between the internal oblique and the transverse abdominis muscle. After careful negative aspiration, 20 ml of 0.25% ropivacaine was injected into the fascial plane on each side of the abdomen and was observed to spread between the two layers on either side.
Perioperative Care and Anesthesia
All patients received a standard anesthetic by a team of experienced anesthetists. All patients were provided analgesia for 48 h postoperatively. The intravenous analgesia regimen for the PCIA and PVB groups was 100 mg oxycodone with NS to 100 ml, 1 ml/h with a 2-ml bolus, and a lockout time of 5 min. All patients were given oxycodone if they were in pain after removing the analgesic pump.
In all patients, general anesthesia was induced using 0.4–0.5 µg/kg sufentanil, 1.5–2 mg/kg propofol, and 0.2 mg/kg cisatracurium to facilitate endotracheal intubation. Anesthesia was maintained with oxygen and an inhalational agent (sevoflurane/desflurane), cisatracurium, and remifentanil. Patients were monitored by electrocardiogram, pulse oximetry, arterial blood pressure, arterial blood gas, and urethral catheterization. The need for intravenous fluids and vasopressors was determined by the anesthetists.
Patients were transferred from the operating room to the intensive care unit (ICU), where they remained until the criteria for discharge to ward were met. Similarly, patients remained on the ward until the criteria for discharge home were fulfilled.
Outcomes
The primary outcome was the pain score on movement during the first 48 h after surgery. Pain scores were recorded at rest and movement on a visual analogue scale (VAS) from 0 to 10 in the postoperative anesthesia care unit (PACU) and at 24 h, 48 h, 72 h, 96 h, and 120 h postoperatively. Scores were recorded by nursing staff independent from the study. Secondary endpoints were the opioid consumption on 48 h postoperatively, intervention-related side effects (nausea and vomiting), intraoperative blood loss, fluid requirements, need for vasoactive medication, time in operating room and PACU, surgical complications (hemorrhage, stress ulcer, anastomotic fistula, wound infection, recurrent nerve injury, and pulmonary complications), and length of ICU and hospital stay. According to recommendations by the European Perioperative Clinical Outcome Taskforce [17], the presence of postoperative pulmonary complications was defined as the presence of 1 or more of the following criteria: respiratory infection, atelectasis, respiratory failure, pleural effusion, pneumothorax, bronchospasm, or aspiration pneumonitis.
Data Collection
Every patient’s data were prospectively collected in real time. Collected variables included patient demographics, pain scores, perioperative clinical information, and complications. Patient-reported pain assessment began in the PACU by the nursing staff, once a day after the operation, who were unaware of the experimental group .
Statistical Analysis
Based on a review of the literature, we expected a difference in mean VAS score between the intervention groups (the noninferiority limit) of < 1 on a scale from 0 to 10. Previous studies [18,19,20] have suggested that, for a VAS, a difference of 0.9–1.6 cm is clinically significant. Using a power of 80% for the noninferiority test, a significance level of < 5%, and a mean margin in VAS score of 1 (SD 2) [21], we calculated that a sample of 153 patients would be needed. With a supposed dropout rate of 10%, we planned to include 168 patients, 56 in each group. The distribution of each continuous variable was summarized by its mean standard deviation and/or median with range/interquartile range. The distribution of each categorical variable was summarized in terms of its frequency and percentage. Continuous variables which satisfied normal distribution and homogeneity of variance were compared for three treatment groups using Analysis of Variance, and further pairwise comparison was conducted by a least-squares difference test. Shapiro–Wilk tests and Levene tests were used to test for normal distribution and homogeneity of variance, respectively. For variables which do not satisfy normal distribution and homogeneity of variance, Kruskal–Wallis tests were conducted for comparison of the three treatment groups and the further pairwise comparison with Bonferroni correction, and the 95% confidence interval for difference of the median was calculated by the Hodges–Lehman method. For categorical variables, Chi-square test was utilized for comparison of the three treatment groups and Fisher's exact test was used for further pairwise comparison with Bonferroni correction, with the Wilson method used to calculate the difference of rate between the treatment groups. A linear mixed model was used to analyze the effects of different treatment groups, times, and their interactions, and, in the meanwhile, control the effects from confounding factors. We used the Bonferroni method for correcting p values. Statistical analyses were performed using SPSS Statistics 21 (IBM, Armonk, NY, USA). All the tests were two-sided, and the confidence interval was 95%. A bilateral p value of < 0.05 was considered statistically significant.
Results
A total of 177 patients were randomly assigned to McKeown esophagectomy, with a PCIA group (n = 59), PVB group (n = 59), and PCEA group (n = 59,) between February 2020 and December 2021. Two patients accidentally detached epidural catheters in the PCEA group. One patient was converted to thoracotomy in each of the PCEA and PCIA groups, and two patients were converted to laparotomy in the PVB group. In addition, two patients in PCIA and one patient in PVB declined to participate. Thus, 168 patients were finally included in the study with a PCIA group (n = 56), PVB group (n = 56), and PCEA group (n = 56). A consort flow diagram is shown in Fig. 1.
Patient Characteristics
Baseline characteristics are presented in Table 1. A total of 168 patients underwent McKeown esophagectomy. No differences were observed in the perioperative clinical characteristics except for a history of diabetes. The PCIA group had ten patients with diabetes, more than the other two groups.
Postoperative Pain Experience
The pain score on movement in the PVB group was similar to that of the PCEA group in the PACU (p = 0.737) and at 24 h postoperatively (p = 0.074). However, the PVB group pain scores at 48 h, 72 h, 96 h, and 120 h postoperatively were significantly higher than that in the PCEA group (p < 0.05). The PCIA group had significantly higher pain scores on the first 4 days after surgery than the PCEA and PVB groups (in the PACU: 4 vs. 0 vs. 1, p < 0.001; 24 h postoperatively: 3 vs. 0 vs. 2, p < 0.001; 48 h postoperatively: 4 vs 1 vs 2, p < 0.001; 72 h postoperatively: 4 vs. 1 vs. 3, p < 0.001; 96 h postoperatively: 4 vs. 2 vs. 4, p < 0.001). The pain score at 120 h postoperatively was significantly higher in the PCIA group than in the PCEA group (4 vs. 2, p < 0.001), but there were no differences between the PCIA and PVB groups (4 vs. 4, p = 0.307) (Fig. 2).
There were no significant differences in pain scores at rest between the PVB group and the PCEA group in the PACU, 24 h and 48 h postoperatively. The pain score was significantly higher in the PVB group than in the PCEA group at 72 h, 96 h, and 120 h postoperatively (p < 0.005). Pain scores at rest on the first 3 days were significantly higher in the PCIA group than in the PCEA and PVB groups (in the PACU: 2 vs. 0 vs. 0, p < 0.001; 24 h postoperatively: 2 vs. 0 vs. 0, p < 0.001; 48 h postoperatively: 2 vs. 0 vs. 0, p < 0.001; 72 h postoperatively: 2 vs. 0 vs. 1, p < 0.001). The pain scores at 96 h and 120 h postoperatively in the PVB group and the PCIA group were similar (Fig. 3).
We used linear mixed model analysis to analyze the effects of treatment group, time, and their interaction, and, in the meanwhile, control the effects from confounding factors. Gender, age, BMI, diabetes, preoperative chemotherapy, preoperative radiotherapy, chronic smoking, duration of surgery, duration of anesthesia, and remifentanil were selected as confounding factors in our research. In the linear mixed model analysis, auto-regression of order one was selected as the repeated covariance type as it generated the smallest Akaike information criterion.
Our results showed that the difference in the main effect between the PVB group and the PCIA group was significant, with the VAS score on movement of the PCIA group increasing on average by 1.205 compared with the PVB group. In addition, the difference of the main effect between the PVB group and the PCIA group was significant, and the VAS at rest of the PCIA group increased on average by 0.96 compared with that of the PVB group. See Tables S1–S4 in the electronic supplementary material for details.
Additional Postoperative Utilization of Narcotics and Vasopressors
The median utilization of oxycodone over the first 5 days after surgery was markedly less in the PCEA group (0 mg, range: 0–11 mg) than in the PCIA (10 mg, range: 0–35 mg) and PVB groups (4 mg, range: 0–36 mg, p < 0.001), and was significantly less in the PVB group than in the PCIA group (p = 0.002; Table 4). The mean norepinephrine usage in the PCEA group was more than the usage in the PVB and PCIA groups (p = 0.001; Table 2), and there was no difference between the PVB and PCIA groups during the operation (p = 0.962; Table 4). There was no significant difference in intraoperative blood loss and perioperative total infusion volume among the three groups (p > 0.05; Table 2). For those who required vasopressor support after the operation, we found no significant difference in the number of patients receiving infused vasopressor (5.4% vs. 3.6% vs. 0%, p = 0.206; Table 3).
Postoperative Surgical and Analgesic-Related Complications
Among 168 patients, 54 (32.1%) experienced a surgical complication. Collectively, there were 2 hemorrhages, 1 stress ulcer, 19 anastomotic fistula, 1 wound infection, 2 recurrent nerve injuries, and 29 pulmonary complications. For pulmonary complication, there were 13 atelectasis, 4 respiratory failure, 6 pneumothorax, and 22 respiratory infection. The pulmonary complication rate in the PCIA group was significantly higher than the rate in the PCEA and PVB groups (30.4% vs. 8.9% vs. 12.5%, p = 0.006). The one-lung ventilation time during McKeown esophagectomy in the PCIA group was shorter than that in the PCEA and PVB groups (p = 0.007; Table 2). Other surgical complication rates were similar among three groups (p > 0.05; Table 3). There was no significant difference in duration of anesthesia and surgery among the three groups (p > 0.05; Table 2).
The mean remifentanil usage was lower in the PCEA group than the PCIA and PVB groups (p < 0.001; Table 2), but there was no statistically significant difference between the PVB and PCIA groups (p > 0.05; Table 4). Sixteen patients experienced an analgesic-related complication. For the incidence of postoperative nausea, there was no difference between the three groups (p = 0.330). However, the postoperative dizziness rate was significantly higher in the PCIA group than the PCEA and PVB groups (19.6% vs. 3.6% vs. 1.8%, p = 0.002; Table 3). The extubation time in the PVB group was significantly shorter than that in the other two groups (p = 0.009, Table 3).
Length of ICU and Hospital Stay
Postoperative recovery was not significantly different between the three groups (Table 3). Median length of ICU stay was similar (p = 0.051). In addition, total hospital stay after esophagectomy did not differ (p = 0.106).
Discussion
Most of the available studies on analgesia efficacy of thoracic paravertebral block analgesia are retrospective, and the surgical methods of selected patients are uneven, which means that there is a great risk of bias in the results, and that these results cannot be generalized to minimally invasive esophagectomy. In this randomized controlled trial, we aimed to compare analgesic efficacy of combined PVB with TAP, TEA, and intravenous analgesia following thoraco-laparoscopic McKeown esophagectomy. PVB produces analgesia by directly depositing local anesthetics into the paravertebral space to block the ventral ramus and dorsal ramus of the spinal nerve root [22]. We found that TPVB and TAP combined with PCIA could provide similar analgesic effects compared with PCEA for a Mckeown esophagectomy in the PACU and at 24 h postoperatively. This result may related to the effective duration of single-injection PVBs having been shown to be well above 12 h [23]. However, PCEA was the best approach with regard to overall postoperative pain during the first 120 h postoperatively. The PVB group was better than the PCIA group.
During surgery, the PCEA group needed a minimum dose of remifentanil. In addition, the PCEA and PVB groups had lower rates of postoperative dizziness than the PCIA group. PVB will provide unilateral somatic and sympathetic block to meet the requirements of unilateral thoracoabdominal surgery. A four-quadrant TAP block has been used to cover supraumbilical skin and infraumbilical pain [24]. Therefore, TPVB combined with a TAP block can reduce opioid consumption and provide excellent analgesia. Previous studies have shown that mu opioid receptors have a direct impact on tumor progression, diffusion, or recurrence [25, 26]. In addition, preclinical studies suggest that opioids may promote tumor growth [27]. With more and more understanding of the interaction between these receptors and perioperative anesthetics, anesthesiologists may find it imperative to seek alternative methods to reduce perioperative opioid release. Therefore, this study supports TPVB combined with a TAP block as a safe and effective tool to limit the dosage of opioid anesthetics.
In the present study, combined TPVB and TAP has provided superior analgesia compared with PCIA. Not only that, TPVB and TAP has also been associated with fewer complications and reliably provides an equivalent pain relief to epidural analgesia. There were fewer patients in the PVB group who required vasopressor support after surgery compared to the PCEA group. Significantly fewer patients in the PVB group experienced one or more hypotensive episodes during the operation, but there were no differences in fluid administration or intraoperative blood transfusion between the two groups.
These results are similar to a previous study that compared different analgesic modalities after thoracotomy [15, 28,29,30], except for pulmonary complications. The previous meta-analysis and systematic review showed that thoracic epidural analgesia, especially paravertebral analgesia, has a certain effect, which can lead to a decrease in postoperative pain scores. In particular, paravertebral analgesia can provide similar pain relief, and there are fewer pulmonary complications [4]. Adequate postoperative analgesia is conducive to recovery [31]. This pain can lead to shortness of breath and severe coughing, leading to respiratory complications, such as hypoxia (insufficient oxygen), atelectasis (collapsed lungs), and lung infection. If it is serious enough, postoperative pain will lead to terrible respiratory disorders, including respiratory failure and other complications [28]. Good pain control with adequate medication facilitates thoracic wall mobility and expansion [3], which allows good pulmonary function and early mobilization after surgery. In addition to this, prior studies of thoracic surgical procedures have demonstrated that longer exposure to OLV is associated with a higher incidence of postoperative pulmonary complications [32]. In addition, a retrospective analysis found that a duration of OLV more than 150 min would increase the risk of postoperative pulmonary complications [33]. In our study, the one-lung ventilation time in the PCIA group was shorter than that in the PCEA and PVB groups, but they were all shorter than 150 min. However, the PCIA group still had a higher rate of pulmonary complications than the PCEA group, and there were no differences between the PCEA and PVB groups in pulmonary complications. The result was possibly due to a higher VAS score and a high rate of diabetes, but the higher VAS score was the most important reason.
Compared to the PCEA group, there did not appear to be any definite clinical benefit with regard to length of ICU stay or overall hospital admission and complication rates in the PVB group.
This study has a number of limitations. First, there may be concerns that results from a single center may not be transferable. However, pain scores were recorded contemporaneously and are likely to reflect the fact that the three modalities do provide good analgesia. Second, we performed single-shot PVB and single-shot subcostal TAP block instead of continuous infusion. The marginal benefits shown in this study were possibly due to the limited duration of the single local anesthetic dose. Finally, our analysis of hypotension only involved patients who had hypotension that required intervention. We did not take into account patients who were hypotensive but fluid-responsive.
Conclusions
This study illustrates that the use of a multimodal analgesia program based on thoracic paravertebral block combined with subcostal transverse abdominis plane block is a viable alternative to thoracic epidural analgesia for total minimally invasive McKeown esophagectomy. In future, anesthesiologists could consider using this multimodal analgesia to help patients with esophageal cancer relieve pain after surgery.
References
Wang C, Pan C, Mao W, Chen Q, Liu J, Hu J. Thoracolaparoscopic McKeown esophagectomy. J Thorac Dis. 2019;11(6):2564–6.
Gupta R, Van de Ven T, Pyati S. Post-thoracotomy pain: current strategies for prevention and treatment. Drugs. 2020;80(16):1677–84.
Tukanova K, Papi E, Jamel S, Hanna GB, McGregor AH, Markar SR. Assessment of chest wall movement following thoracotomy: a systematic review. J Thorac Dis. 2020;12(3):1031–40.
Steinthorsdottir KJ, Wildgaard L, Hansen HJ, Petersen RH, Wildgaard K. Regional analgesia for video-assisted thoracic surgery: a systematic review. Eur J Cardiothorac Surg. 2014;45(6):959–66.
Carli F, Kehlet H, Baldini G, et al. Evidence basis for regional anesthesia in multidisciplinary fast-track surgical care pathways. Reg Anesth Pain Med. 2011;36(1):63–72.
Pires Sousa I, da Silva L, Peixoto CI, Fernandes Coimbra LA, da Costa Rodrigues FM. Comparison of pericapsular nerve group (PENG) block and epidural analgesia following total hip arthroplasty: a retrospective analysis. Rev Esp Anestesiol Reanim (Engl Ed). 2022;69(10):632–9.
Hermanides J, Hollmann MW, Stevens MF, Lirk P. Failed epidural: causes and management. Br J Anaesth. 2012;109(2):144–54.
Jeong YH, Jung JY, Cho H, et al. Transverse abdominis plane block compared with patient-controlled epidural analgesia following abdominal surgery: a meta-analysis and trial sequential analysis. Sci Rep. 2022;12(1):20606.
Cook TM, Counsell D, Wildsmith JA, Royal College of Anaesthetists Third National Audit Project. Major complications of central neuraxial block: report on the Third National Audit Project of the Royal College of Anaesthetists. Br J Anaesth. 2009;102(2):179–90.
Gisbertz SS, Hagens ERC, Ruurda JP, et al. The evolution of surgical approach for esophageal cancer. Ann N Y Acad Sci. 2018;1434(1):149–55.
Guo W, Ma X, Yang S, et al. Combined thoracoscopic-laparoscopic esophagectomy versus open esophagectomy: a meta-analysis of outcomes. Surg Endosc. 2016;30(9):3873–81.
Blackshaw WJ, Bhawnani A, Pennefather SH, Al-Rawi O, Agarwal S, Shaw M. Propensity score-matched outcomes after thoracic epidural or paravertebral analgesia for thoracotomy. Anaesthesia. 2018;73(4):444–9.
Levy G, Cordes MA, Farivar AS, Aye RW, Louie BE. Transversus abdominis plane block improves perioperative outcome after esophagectomy versus epidural. Ann Thorac Surg. 2018;105(2):406–12.
Re M, Blanco J, Gómez de Segura IA. Ultrasound-guided nerve block anesthesia. Vet Clin N Am Food Anim Pract. 2016;32(1):133–47.
Li NL, Liu CC, Cheng SH, et al. Feasibility of combined paravertebral block and subcostal transversus abdominis plane block in postoperative pain control after minimally invasive esophagectomy. Acta Anaesthesiol Taiwan. 2013;51(3):103–7.
New York School of Regional Anesthesia. Truncal and Cutaneous Blocks. www.nysora.com/techniques/ultrasound-guided-techniques/3253-truncal-and-cutaneousblocks.html.
Jammer I, Wickboldt N, Sander M, et al. Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European Perioperative Clinical Outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol. 2015;32:88–105.
Kelly AM. Does the clinically significant difference in visual analog scale pain scores vary with gender, age, or cause of pain? Acad Emerg Med. 1998;5(11):1086–90.
Myles PS, Myles DB, Galagher W, et al. Measuring acute postoperative pain using the visual analog scale: the minimal clinically important difference and patient acceptable symptom state. Br J Anaesth. 2017;118(3):424–9.
Gallagher EJ, Bijur PE, Latimer C, Silver W. Reliability and validity of a visual analog scale for acute abdominal pain in the ED. Am J Emerg Med. 2002;20(4):287–90.
Hausken J, Fretland ÅA, Edwin B, et al. Intravenous patient-controlled analgesia versus thoracic epidural analgesia after open liver surgery: a prospective, randomized, controlled. Noninferiority Trial Ann Surg. 2019;270(2):193–9.
Seidel R, Wree A, Schulze M. Thoracic-paravertebral blocks: comparative anatomical study with different injection techniques and volumes. Reg Anesth Pain Med. 2020;45(2):102–6.
Klein SM, Bergh A, Steele SM, Georgiade GS, Greengrass RA. Thoracic paravertebral block for breast surgery. Anesth Analg. 2000;90(6):1402–5.
Niraj G, Kelkar A, Hart E, Kaushik V, Fleet D, Jameson J. Four quadrant transversus abdominis plane block and continuous transversus abdominis plane analgesia: a 3-year prospective audit in 124 patients. J Clin Anesth. 2015;27(7):579–84.
Lennon FE, Mirzapoiazova T, Mambetsariev B, et al. The Mu opioid receptor promotes opioid and growth factor-induced proliferation, migration and Epithelial Mesenchymal Transition (EMT) in human lung cancer. PLoS ONE. 2014;9(3): e91577.
Lennon FE, Mirzapoiazova T, Mambetsariev B, Salgia R, Moss J, Singleton PA. Overexpression of the μ-Opioid receptor in human non-small cell lung cancer promotes Akt and mTOR activation, tumor growth, and metastasis. Anesthesiology. 2012;116(4):857–67.
Bortsov AV, Millikan RC, Belfer I, Boortz-Marx RL, Arora H, McLean SA. μ-Opioid receptor gene A118G polymorphism predicts survival in patients with breast cancer. Anesthesiology. 2012;116(4):896–902.
Sabanathan S, Eng J, Mearns AJ. Alterations in respiratory mechanics following thoracotomy. J R Coll Surg Edinb. 1990;35(3):144–50.
Davies RG, Myles PS, Graham JM. A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural blockade for thoracotomy—a systematic review and meta-analysis of randomized trials [published correction appears in Br J Anaesth. 2007 Nov;99(5):768]. Br J Anaesth. 2006;96(4):418–26.
Zhang W, Fang C, Li J, et al. Single-dose, bilateral paravertebral block plus intravenous sufentanil analgesia in patients with esophageal cancer undergoing combined thoracoscopic-laparoscopic esophagectomy: a safe and effective alternative. J Cardiothorac Vasc Anesth. 2014;28(4):966–72.
Joshi GP, Bonnet F, Shah R, et al. A systematic review of randomized trials evaluating regional techniques for postthoracotomy analgesia. Anesth Analg. 2008;107(3):1026–40.
Lohser J, Slinger P. Lung injury after one-lung ventilation: a review of the pathophysiologic mechanisms affecting the ventilated and the collapsed lung. Anesth Analg. 2015;121(2):302–18.
Lai G, Guo N, Jiang Y, Lai J, Li Y, Lai R. Duration of one-lung ventilation as a risk factor for postoperative pulmonary complications after McKeown esophagectomy. Tumori. 2020;106(1):47–54.
Acknowledgements
We thank our colleagues Huang Wan, Wang Huanwei, Zhang Jianxing, and Tong Panpan for their help in this study, and these colleagues received no funding. We also thank the participants of the study.
Funding
This work and the article processing fees were funded by the Guangdong Esophageal Cancer Institute Science and Technology Program (No. M201812), the Natural Science Foundation of Guangdong Province (2022A1515012543), the Guangzhou Basic and Applied Basic Research Project (202201010792), the Medical Scientific Research Foundation of Guangdong Province, China (Grant numbers: C2020058) and the Research of Traditional Chinese Medicine Bureau of Guangdong Province (20211099). The Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection were performed by Fu Shuwen, Lu Xiaofan and Lai Jielan. Analysis was performed by Lu Yali, Wang Xudong and Song Xiong. The first draft of the manuscript was written by Lai Renchun, Xumei and Feng Yuerou and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Xu Mei, Feng Yuerou, Song Xiong, Fu Shuwen, Lu Xiaofan, Lai Jielan, Lu Yali, Wang Xudong and Lai Renchun declare that they have no conflicts of interest.
Compliance with Ethics Guidelines
Ethical approval for this study (B2019-163) was provided by the Ethics Committee of Cancer Center of Sun Yat-Sen University, Guangzhou City, Guangdong Province, China. The trial was registered in the Chinese Clinical Trial Registry (ChiCTR2000029588, Principal investigator: Renchun Lai, Date of registration: 2020-02-16). The study was in accordance with the Declaration of Helsinki and its later amendments. Informed consent was obtained from all individual participants included in the study.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Xu, M., Feng, Y., Song, X. et al. Combined Ultrasound-Guided Thoracic Paravertebral Nerve Block with Subcostal Transversus Abdominis Plane Block for Analgesia After Total Minimally Invasive Mckeown Esophagectomy: A Randomized, Controlled, and Prospective Study. Pain Ther 12, 475–489 (2023). https://doi.org/10.1007/s40122-023-00474-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-023-00474-5