Abstract
Introduction
Complete postoperative analgesia is very important for puerperae after cesarean section. The objective of this study was to explore the optimal postoperative analgesia after cesarean section.
Methods
A total of 180 full-term puerperae who underwent cesarean section in Hanzhong People's Hospital from March 2019 to March 2020 were enrolled and were randomly divided into three groups. Group A was given 0.9% normal saline, group B and C were given 0.4% ropivacaine for transversus abdominis plane block (TAPB). Postoperative patient-controlled intravenous analgesia (PCIA) pumps were 2 μg/kg sufentanil + 2.5 mg droperidol, 1.5 μg/kg and 1.3 μg/kg sufentanil, respectively. All puerperae were given different but effective analgesia programs. The primary outcome indicators were visual analog scores (VAS), the first compression time of postoperative analgesia pump and the total number of compressions in 48 h. The secondary outcome indicators were vital signs, Ramsay sedation scores, comfort scores (BCS), the frequency of analgesic rescue, postoperative side effects and satisfaction.
Results
The dynamic and static VAS scores of the puerperae in group B at T2 and T6 were significantly lower than group A and at T12, T24 and T48 were significantly lower than group C. Compared with group A, the dynamic and static VAS scores of puerperae in group C were lower at T2 and T6 and higher at T12, T24 and T48. The Ramsay score and BCS score of the puerperae in group C at T12, T24 and T48 were significantly lower than those in groups A and B.
Conclusions
PCIA with sufentanil alone or combined with TAPB can be safely and effectively used for postoperative analgesia after cesarean section. PCIA combined with TAPB had better analgesic effect and lower incidence of side effects while reducing the dose of opioids. The results of this study provide new ideas and insights for the choice of analgesia after cesarean section.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Pain is the most common complication after cesarean section; however, the conventional analgesia methods in clinical practice have different limitations. |
Therefore, guided by the concepts of enhanced recovery after surgery (ERAS) and multimodal analgesia (MMA), we designed this study to try to explore more suitable modes of analgesia after cesarean section. |
What was learned from the study? |
Ultrasound-guided transversus abdominis plane block (TAPB) combined with patient-controlled intravenous analgesia (PCIA) can be safely and effectively used for postoperative analgesia after cesarean section. |
When the dose of sufentanil in PCIA is 1.5 μg/kg, the analgesic effect was good and the side effects were few. |
Ultrasound-guided TAPB cannot completely replace the application of opioids in analgesia after cesarean section, and its clinical application is limited. |
Introduction
Pain, which has been recognized as the fifth vital sign [1], is a very unpleasant physical experience and emotion caused by potential or substantial tissue damage [2]. Cesarean section is currently an important and the only effective means to solve high-risk pregnancy and dystocia in clinical practice. However, parturients will experience severe pain after cesarean section, which is mainly caused by lower abdominal incision pain and uterine contraction pain induced by repeated uterine contraction [3, 4]. The harm and influence of post-cesarean section pain on parturients are huge and will delay the time of active turning and ambulation of parturients, cause then to experience mental problems such as anxiety and depression, lead to depressed mood and sleep disorders, decreasing the ability of parturients to care for infants [5, 6]. Therefore, it is essential to provide perfect postoperative analgesia after cesarean section.
Multimodal analgesia (MMA) is a relatively new concept, mainly suing the synergistic effect of different analgesic drugs and methods under the premise of achieving a satisfactory analgesic effect reducing the dose of analgesic drugs and the incidence of side effects [7]. As one of the important components of MMA, regional nerve block technology has attracted the attention of anesthesiologists, in addition to its satisfactory analgesic effect, it also has little impact on various systems of the body, which can lead to an earlier time for patients to perform functional exercise and promote postoperative recovery [8]. Moreover, with the wide application of visualized ultrasound technology in the field of anesthesia, regional block technology has been greatly improved in terms of safety and accuracy.
Transversus abdominis plane block (TAPB) mainly relieves the pain of abdominal incision by blocking the anterior branch of the T8-L1 nerve in the abdominal wall. TAPB is increasingly widely used in laparotomy because of its good analgesic effect on the abdominal wall, simple operation and high safety [9]. At present, patient-controlled intravenous analgesia (PCIA) is widely used for postoperative analgesia after cesarean section [10], and sufentanil has become the first choice for PCIA because of its strong analgesic effect, good hemodynamic stability and wide safety threshold. However, some puerperae may experience side effects such as nausea, vomiting and skin itching [11]. Therefore, actively exploring better analgesic strategies or methods to make up for the deficiencies of traditional analgesic methods is an important issue to be solved urgently.
In this study, to explore the optimal analgesic scheme of puerperae after cesarean section, the traditional drug formula (opioids) commonly used in clinical post-cesarean section analgesia was set as the positive control group, and the effects of analgesia, sedation and side effects were evaluated.
Methods
Participants
This study was approved by the Ethics Committee of Hanzhong People’s Hospital (YDXY-KY-2019-004). The clinical research was conducted in accordance with the Declaration of Helsinki, and all patients and their families provided informed consent. According to the inclusion and exclusion criteria, this study finally included 180 full-term parturients who underwent cesarean section under spinal anesthesia in Hanzhong City People's Hospital from March 2019 to March 2020.
Inclusion criteria were: (1) Classified as I–II according to the American Society of Anesthesiologists (ASA); (2) aged between 18 and 38 years old; (3) body mass index (BMI) between 20 and 30 kg/m2; (4) gestational age between 37 and 41 weeks; (5) patients with clear consciousness and normal communication skills, who voluntarily accepted PCIA after surgery and who could correctly use PCIA and accurately describe VAS scores through learning; (6) no serious heart, lung, liver or kidney disease; (7) no history of alcohol or drug abuse; (8) coagulation function test indicators are normal; (9) no skin damage or infection at the abdominal wall puncture site.
Exclusion criteria were: (1) patients allergic to local anesthetics; (2) patients with impaired consciousness, severe neurosis, and so on, who could not cooperate and communicate; (3) patients with hypertension, diabetes, cardiopulmonary dysfunction or poor liver and kidney function; (4) patients with abnormal coagulation function; (5) a history of opioid dependence.
Research Procedure
In this study, according to the random number table method, the enrolled parturients were randomly divided into three groups with 60 cases in each group. All parturients underwent standard subarachnoid block anesthesia with 0.5% ropivacaine 3 ml. The puerperae were given TAPB after operation in groups A, B and C, who were respectively given 20 ml 0.9% normal saline, 20 ml 0.4% ropivacaine and 20 ml 0.4% ropivacaine, all of which were injected bilaterally at one time. The postoperative PCIA pumps in the three groups contained 16 mg ondansetron and 10 mg dexamethasone; in addition, the other drugs in groups A, B and C were 2 μg/kg sufentanil + 2.5 mg droperidol, 1.5 μg/kg sufentanil and 1.3 μg/kg sufentanil, respectively. If the analgesia is poor and the VAS ≥ 4 points, tramadol 50 mg can be added for relief, and the times of relief should be recorded. The design of sufentanil dose in PCIA is based on our pre-experiment in the early stage of the study.
The analgesic pumps of the three groups were all made up of 100 ml solution with normal saline. The parameters of the analgesic pump were set as: the background infusion rate was 0.03 ml/kg/h, additional dose was 1.0 ml, and lock-in time was 30 min. To maximize standardization and blinding, participants in this study were blinded to differences in analgesia methods. TAPB was administered by the same experienced clinician who performed only the procedure and was blinded to the drugs used. Postoperative assessments of relevant indicators were performed by the same assessor, and the assessor were blinded to the grouping of participants.
Observation Indicator
Primary outcome indicators: (1) the visual analog score (VAS score) for static and dynamic score (turn over 90°) at 2 h (T2), 6 h (T6), 12 h (T12), 24 h (T24) and 48 h (T48) after surgery; (2) the first compression time of PCIA pump and the total number of compressions in 48 h.
Secondary outcome indicators are: (1) vital signs: systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR) and pulse oxygen saturation (SpO2); (2) the Ramsay sedation score (Ramsay score) at T2, T6, T12, T24 and T48 after surgery: 1 = irritability; 2 = quiet cooperation; 3 = drowsiness; 4 = arousable sleep state; 5 = unresponsive calling; 6 = unarousable deep sleep state; (3) the comfort score (BCS score) at T2, T6, T12, T24 and T48 after surgery: 0 = persistent pain; 1 = no pain at rest and severe pain during deep breathing and cough; 2 = no pain at rest in the supine position and mild pain during deep breathing and cough; 3 = no pain during deep breathing; 4 = no pain during cough; (4) postoperative side effects and satisfaction; (5) the frequency of postoperative analgesic rescue (if VAS ≥ 4, tramadol 50 mg can be given for additional analgesia).
Statistical Method
Before the start of this study, we conducted a pre-experiment selecting 15 patients in each group, which found that the VAS scores of the three groups at 12 h after surgery respectively were (2.75 ± 0.35), (2.73 ± 0.31) and (2.80 ± 0.36). According to the sample size calculation online tool https://www.biostats.cn/statbox/ and some excellent research cases of researchers on post-cesarean analgesia [11,12,13,14,15,16], we decided to recruit 60 patients to each group, allowing for a 20% drop-out rate (the inspection efficiency is 80%, and the inspection level is 0.05).
Statistical analysis was performed using SPSS 25.0 statistical software. Categorical data were expressed as numbers and percentages, quantitative variables were expressed as the median and IQR or the mean and standard deviation (SD), and one-way ANOVA and Bonferroni corrections used among the groups and chi-squared test used on counting data. The difference was considered statistically significant when P < 0.05.
Results
Comparison of General Conditions of Three Groups
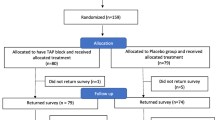
After strict inclusion, exclusion and elimination criteria, a total of 180 full-term pregnant women were included and randomly divided into three groups (Fig. 1). The basic characteristics of the three groups appear in Table 1. After statistical analysis, it was found that there was no significant difference in maternal age, height, weight, BMI and ASA classification among the three groups (P > 0.05).
Safety Evaluation
The analysis results of SBP, DBP, HR and SpO2 of the three groups of puerperae after operation are shown in Table 2. Interestingly, we found that the SBP at T2, T6, DBP at T6, T24 and HR at T24, T48 were statistically different among the three groups. Although these indicators were statistically different, they were all within the clinically reasonable range, which were not considered clinically meaningful.
Primary Outcome: Evaluation of Postoperative Analgesic Effect
First, we analyzed the static and dynamic scores at five different time points after the operations on the three groups of puerperae.
The static VAS scores of T2, T6 and T12 in group B and T2 and T6 in group C were significantly lower than those in group A (P < 0.05). The static VAS score of group C at T12, T24 and T48 was dramatically higher than that of group A and group B (P < 0.05). There was no significant difference in group B and group C at T2 and T6 (P > 0.05). Group A and group B at T24 and T48 had no significant difference (P > 0.05) (Fig. 2).
For the results of dynamic VAS scores, we found that the scores of puerperae in group B and group C at T2 and T6 were significantly lower than those in group A (P < 0.05). The dynamic VAS scores in group C at T12, T24 and T48 were significantly higher than those in group A and group B (P < 0.05). The dynamic VAS scores of group B and group C were not significantly different at T2 and T6 (P > 0.05). There was no significant difference in group A and group B at T24 and T48 (P > 0.05) (Fig. 3).
By comparing the use of postoperative PCIA in the three groups, we found that there were significant differences in the first compression time and the total number of compressions within 48 h among the three groups (P < 0.05). Among them, the first compression time in group A was significantly earlier than that in groups B and C, but the total number of compressions within 48 h in group C was significantly more than that in group A and B (P < 0.05) (Table 3).
Secondary Outcome: Postoperative Comfort, Satisfaction and Side Effects
By analyzing the Ramsay score of the three groups of puerperae after surgery, we found that the Ramsay scores of the puerperae in group C at T12, T24 and T48 were lower than those in groups A and B (P < 0.05). There was no significant difference in the Ramsay score at T6 among the three groups (P > 0.05). The Ramsay score of the puerperae in group A at T2 was higher than in group B and C(P < 0.05). There was no significant difference in the Ramsay score at T12, T24 and T48 between groups A and B (P > 0.05) (Fig. 4).
Figure 5 shows the postoperative BCS comfort score at T2, T6, T12, T24 and T48 for the three groups of puerperae, respectively. The scores of puerperae in group C at T12, T24 and T48 were significantly lower than those in groups A and B (P < 0.05). The scores in group A at T2 and T6 were significantly lower than those in group B and C (P < 0.05). There was no significant difference in the BCS score at T2 and T6 between group B and C (P > 0.05). There was no significant difference in the BCS score at T12, T24 and T48 between group A and B (P > 0.05) (Fig. 5).
Nausea and vomiting, analgesic satisfaction and frequency of postoperative analgesic rescue showed significant difference among the three groups of puerperae (P < 0.05). Skin itching and respiratory depression after surgery showed no significant difference (P > 0.05). (Table 4).
Discussion
Currently, cesarean section is an important and the only effective method to solve high-risk pregnancies and dystocia; it is crucial to provide perfect analgesia after operation. At present, the clinical analgesic methods after cesarean section are mainly patient-controlled epidural analgesia (PCEA) and PCIA, supplemented by oral or intramuscular injection of analgesics, which have their own analgesic advantages, but each one still has different limitations [17]. Studies have shown that PCEA has a good analgesic effect [12], which can not only increase the enthusiasm for breastfeeding, but also accelerate the recovery of gastrointestinal function [18]; however, there are some related complications such as lower limb weakness, numbness and urinary retention [19]. Hence, there is currently a clear downward trend in the amount of post-cesarean analgesia clinically used by PCEA. At the same time, PCIA also attracted the attention of anesthesiologists. In this study, for humanitarian reasons, we set postoperative analgesia using PCIA alone to a positive control group.
Satisfaction with the analgesic effects of PCIA is generally directly related to the type and concentration of analgesics. Currently, the preferred analgesic in the PCIA after cesarean section is sufentanil [20]. When the concentration of sufentanil is not enough, the analgesic effect is unsatisfactory, but when the concentration of drug is too high, side effects such as nausea, vomiting, skin itching and so on are likely to occur. In addition, the routine drugs such as oxytocin after cesarean section make the incidence of maternal nausea and vomiting higher [21], so the anesthesiologist will always hear complaints about the side effects of the analgesic drug affecting the puerperae during postoperative follow-up. The dose of sufentanil used in this study was set based on rich clinical experience and research data from multiple investigators, and its safety and efficacy have also been validated in clinical practice. However, the gastrointestinal side effects of group A with the highest dose of sufentanil in this study were significantly higher than those of the other two groups [22,23,24,25,26,27], so its clinical application needs to be further improved. Although PCIA has an acceptable analgesic effect on pain at rest, it has poor analgesic effect on wound pain caused by turning over, pressing the uterus and abdominal wall tension during breastfeeding [28].
With the development of the concept of enhanced recovery after surgery (ERAS), MMA has also emerged [29]. As a regional block technique and an important part of MMV, TAPB is simple and safe to operate and has a satisfactory analgesic effect on the abdominal wall and has few side effects. Therefore, in our study we combined PCIA with TAPB to try to explore the most suitable analgesia regimen for puerperae after cesarean section.
As a cornerstone of the study, we first evaluated the safety of three methods. This study applied TAPB and PCIA analgesia alone or in combination to 180 puerperae after cesarean section, and it was observed that the SBP, DBP, HR and SpO2 of the three groups at five time points were within the scope of clinical normality, demonstrating that the methods used in the three groups were all safe. At the same time, it was found that the patient satisfaction of groups A and B was high, which proved that both regimens could be effectively applied to post-cesarean analgesia. In the post-cesarean analgesic group with PCIA alone, we routinely added haloperidol 2.5 mg to PCIA to prevent side effects such as nausea and vomiting caused by sufentanil. So, it was also found that the number of gastrointestinal side effects of the puerperae was still higher than those of the other two groups. The US Food and Drug Administration (FDA) reported that nine patients had a Q-T interval prolonged after intravenous injection of low-dose haloperidol and led to cardiac accident-related events [30]. Therefore, although the postoperative analgesia group with PCIA alone after cesarean section is convenient to operate, it carries a greater risk to women with cardiac insufficiency and more obvious side effects.
By comparing the static and dynamic VAS score of three groups of puerperae at five different time points after surgery, it was found that TAPB by using ropivacaine could significantly reduce maternal pain within 12 h after surgery, but had little effect on the score after 12 h. Consequently, the puerperae in group A pressed the analgesic pump earlier. These results demonstrate that PCIA combined with TAPB can be more effective in preventing pain in the short term after surgery, but cannot completely replace the application of opioids in post-cesarean analgesia. On the other hand, it is worth noting that the VAS score of group C increased significantly after 12 h postoperatively, which was higher than in groups A and B, and remedial measures were needed. In addition, the Ramsay score and BCS score of puerperae in group C after 12 h were lower than those in groups A and B, indicating that the regimen of group C was insufficient for continuous analgesia. One potential explanation for this may be the underdose of sufentanil in PCIA. These findings are in line with the research results of scholars such as P. Fusco [31] and Mishriky [32], so the implementation of TAPB after cesarean section can significantly improve the analgesic effect and reduce the dosage of opioids. However, their study did not address the optimal dose of sufentanil. In this study, through the analysis of various indicators of three groups of puerperae, it was found that PCIA combined with TAPB can reduce the dosage of sufentanil in PCIA, and when the dosage is reduced to 1.5 μg/kg, the analgesic satisfaction is the best.
Nonetheless, the successful and effective implementation of TAPB nowadays in clinical practice still requires ultrasonic testing equipment and professional technical support. Non-visual TAPB procedures have a high risk of puncture and low success rates and may even damage the liver and intestines in the abdominal cavity [9, 33]. With the wide application of visual ultrasound technology in the field of clinical anesthesia, we can clearly distinguish the direction of tissues and the scope of drug diffusion, with high puncture success and few complications [34]. In this study, the implementation of TAPB was performed by the same fully qualified clinical anesthesiologist, who was proficient in TAPB puncture technology, coupled with the application of ultrasound visualization technology, which strongly guaranteed the accuracy and safety of the operation.
The local anesthetic selected for TAPB in our study is ropivacaine hydrochloride injection [35], which is a long-acting amide local anesthetic; it mainly exerts a local anesthetic effect by inhibiting the pain conduction fibers of nerves. The concentration of ropivacaine used was 0.4%, no patients had neurotoxicity-related. Effects and the duration of analgesia was about 6–12 h, so it can be seen that the concentration of ropivacaine designed in this study is safe and effective. Previous studies have performed TAPB in post-cesarean section patients by setting different concentration gradients of ropivacaine. The results showed [36] that when the concentration of ropivacaine was > 0.2%, and the toxic dose was not exceeded; the combination of TAPB and PCIA for postoperative analgesia after cesarean section was safe and effective. The use of 0.375% ropivacaine for TAPB is preferred in clinical work [37], which also supports the setting of ropivacaine concentration in this study. In addition, this study has demonstrated that by combining TAPB, it is feasible to reduce the dose of sufentanil, thereby avoiding the use of droperidol. This is undoubtedly that the best choice for postoperative analgesia for puerperae with cardiac insufficiency.
This study is a single-center study with a small sample size, and there are limitations in terms of regions and races. The grouping on the dose of the drug is still not detailed enough. In the follow-up study, we will use better methods such as the PASS to calculate the sample size, further expand the sample size to include multi-center clinical cases and establish more detailed drug dose groupings, further explore the model of TAPB combined with PCIA for postoperative analgesia and try to explore more analgesic methods combined with MMA to seek the best effect of post-cesarean analgesia.
Conclusion
In this study, we found that PCIA with sufentanil alone or ultrasound-guided TAPB combined with PCIA can both be safely and effectively used for postoperative analgesia after cesarean section. In addition, PCIA combined with ultrasound-guided TAPB has better analgesic effect and lower incidence of side effects while reducing the dose of opioids. Although ultrasound-guided TAPB requires professional equipment and technical support, the results of this study still provide new ideas and insights related to the choice of analgesia after cesarean section.
References
Pozza DH, Azevedo LF, Castro Lopes JM. Pain as the fifth vital sign: a comparison between public and private healthcare systems. PLoS ONE. 2021;16(11): e0259535.
Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131–57.
Weibel S, Neubert K, Jelting Y, Meissner W, Wöckel A, Roewer N, et al. Incidence and severity of chronic pain after caesarean section: a systematic review with meta-analysis. Obstet Anesth Dig. 2017;37(3):117–8.
Daly B, Young S, Marla R, Riddell L, Junkin R, Weidenhammer N, et al. Persistent pain after caesarean section and its association with maternal anxiety and socioeconomic background. Int J Obstet Anesth. 2017;29:57–63.
Niklasson B, Georgsson Ohman S, Segerdahl M, Blanck A. Risk factors for persistent pain and its influence on maternal wellbeing after cesarean section. Acta Obstet Gynecol Scand. 2015;94(6):622–8.
Komatsu R, Ando K, Flood PD. Factors associated with persistent pain after childbirth: a narrative review. Br J Anaesth. 2020;124(3):e117–30.
Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg. 2017;152(7):691–7.
Urits I, Ostling PS, Novitch MB, Burns JC, Charipova K, Gress KL, et al. Truncal regional nerve blocks in clinical anesthesia practice. Best Pract Res Clin Anaesthesiol. 2019;33(4):559–71.
Tran DQ, Bravo D, Leurcharusmee P, Neal JM. Transversus abdominis plane block: a narrative review. Anesthesiology. 2019;131(5):1166–90.
Wu Z, Zhao P, Peng J, Fang L, Ding J, Yan G, et al. A patient-controlled intravenous analgesia with tramadol ameliorates postpartum depression in high-risk woman after cesarean section: a randomized controlled trial. Front Med (Lausanne). 2021;8: 679159.
Sun S, Guo Y, Wang T, Huang S. Analgesic effect comparison between nalbuphine and sufentanil for patient-controlled intravenous analgesia after cesarean section. Front Pharmacol. 2020;11: 574493.
Kacmaz O, Gulhas N, Erdogan Kayhan G, Durmus M. Effects of different epidural initiation volumes on postoperative analgesia in cesarean section. Turk J Med Sci. 2020;50(8):1955–62.
Sharpe EE, Molitor RJ, Arendt KW, Torbenson VE, Olsen DA, Johnson RL, et al. Intrathecal morphine versus intrathecal hydromorphone for analgesia after cesarean delivery: a randomized clinical trial. Anesthesiology. 2020;132(6):1382–91.
Nedeljkovic SS, Kett A, Vallejo MC, Horn JL, Carvalho B, Bao X, et al. Transversus abdominis plane block with liposomal bupivacaine for pain after cesarean delivery in a multicenter, randomized, double-blind, controlled trial. Anesth Analg. 2020;131(6):1830–9.
Irwin R, Stanescu S, Buzaianu C, Rademan M, Roddy J, Gormley C, et al. Quadratus lumborum block for analgesia after caesarean section: a randomised controlled trial. Anaesthesia. 2020;75(1):89–95.
Blanco R, Ansari T, Riad W, Shetty N. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg Anesth Pain Med. 2016;41(6):757–62.
Sen Tan H, Diomede O, Habib AS. Postoperative analgesia after cesarean delivery. Int Anesthesiol Clin. 2021;59(3):90–7.
Murata Y, Yamada K, Hamaguchi Y, Yamashita S, Tanaka M. An optimal epidural catheter placement site for post-cesarean section analgesia with double-space technique combined spinal-epidural anesthesia: a retrospective study. JA Clin Rep. 2021;7(1):3.
Koh JC, Song Y, Kim SY, Park S, Ko SH, Han DW. Postoperative pain and patient-controlled epidural analgesia-related adverse effects in young and elderly patients: a retrospective analysis of 2,435 patients. J Pain Res. 2017;10:897–904.
Lee W, Gao X, Tang J, Li A, Zhu Y, Ling X, et al. Postoperative sufentanil intravenous patient-controlled analgesia within the first 24 hours: a retrospective study. Ann Palliat Med. 2020;9(6):3932–7.
Heesen M, Carvalho B, Carvalho JCA, Duvekot JJ, Dyer RA, Lucas DN, et al. International consensus statement on the use of uterotonic agents during caesarean section. Anaesthesia. 2019;74(10):1305–19.
Qin M, Chen K, Liu T, Shen X. Dexmedetomidine in combination with sufentanil for postoperative analgesia after partial laryngectomy. BMC Anesthesiol. 2017;17(1):66.
Liu F, Li TT, Yin L, Huang J, Chen YJ, Xiong LL, et al. Analgesic effects of sufentanil in combination with flurbiprofen axetil and dexmedetomidine after open gastrointestinal tumor surgery: a retrospective study. BMC Anesthesiol. 2022;22(1):130.
Zhen L, Li X, Gao X, Wei H, Lei X. Dose determination of sufentanil for intravenous patient-controlled analgesia with background infusion in abdominal surgeries: a random study. PLoS ONE. 2018;13(10): e0205959.
Yang C, Geng WL, Hu J, Huang S. The effect of gestational diabetes mellitus on sufentanil consumption after cesarean section: a prospective cohort study. BMC Anesthesiol. 2020;20(1):14.
Cao X, Zhang X. Comparison of different sufentanil-tramadol combinations for pain relief within the first 24 hours after cesarean section: a retrospective study. J Pain Res. 2018;11:2445–51.
Nie ZB, Li ZH, Lu B, Guo YY, Zhang R. Hydromorphone vs sufentanil in patient-controlled analgesia for postoperative pain management: a meta-analysis. Medicine (Baltimore). 2022;101(3): e28615.
Motamed C. Clinical update on patient-controlled analgesia for acute postoperative pain. Pharmacy (Basel). 2022;10(1):22.
Mitra S, Carlyle D, Kodumudi G, Kodumudi V, Vadivelu N. New advances in acute postoperative pain management. Curr Pain Headache Rep. 2018;22(5):35.
Smyla N, Koch T, Eberhart LH, Gehling M. An overview of intravenous amisulpride as a new therapeutic option for the prophylaxis and treatment of postoperative nausea and vomiting. Expert Opin Pharmacother. 2020;21(5):517–22.
Fusco P, Scimia P, Paladini G, Fiorenzi M, Petrucci E, Pozone T. Transversus abdominis plane block for analgesia after cesarean delivery: a systematic review. Minerva Anestesiol. 2015;81(2):195–204.
Mishriky BM, George RB, Habib AS. Transversus abdominis plane block for analgesia after Cesarean delivery: a systematic review and meta-analysis. Can J Anaesth. 2012;59(8):766–78.
Finnerty O, McDonnell JG. Transversus abdominis plane block. Curr Opin Anaesthesiol. 2012;25(5):610–4.
Tsai HC, Yoshida T, Chuang TY, Yang SF, Chang CC, Yao HY, et al. Transversus abdominis plane block: an updated review of anatomy and techniques. Biomed Res Int. 2017;2017:8284363.
Ropivacaine. Drugs and lactation database (LactMed). Bethesda: National Library of Medicine (US); 2021.
Eng HC, Ghosh SM, Chin KJ. Practical use of local anesthetics in regional anesthesia. Curr Opin Anaesthesiol. 2014;27(4):382–7.
Sun N, Wang S, Ma P, Liu S, Shao A, Xiong L. Postoperative analgesia by a transversus abdominis plane block using different concentrations of ropivacaine for abdominal surgery: a meta-analysis. Clin J Pain. 2017;33(9):853–63.
Acknowledgements
We thank our colleagues for their help in this study, the support of their families and the participants in this study.
Funding
This study was supported by the National Natural Science Foundation of China (81972241). The journal's Rapid Service Fee was funded by the researchers.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the whole article and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception, design, material preparation, data collection and analysis. The first draft of the manuscript was written by Mengwen Xue and Cong Guo; all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Mengwen Xue, Cong Guo, Kunyu Han, Ruiping Bai, Rui An and Xin Shen declare that they have no conflict of interest.
Compliance with Ethics Guidelines
This study was approved by the Ethics Committee of Hanzhong People's Hospital (YDXY-KY-2019-004). The clinical research was conducted in accordance with the Declaration of Helsinki, and all patients and their families provided informed consent.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Xue, M., Guo, C., Han, K. et al. Analgesia Effect of Ultrasound-Guided Transversus Abdominis Plane Block Combined with Intravenous Analgesia After Cesarean Section: A Double-Blind Controlled Trial. Pain Ther 11, 1287–1298 (2022). https://doi.org/10.1007/s40122-022-00425-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-022-00425-6