Abstract
Introduction
In Japan, conservative therapy for patients with lumbar spinal stenosis (LSS) includes non-steroidal anti-inflammatory drugs (NSAIDs), prostaglandin E1, tramadol, physical/exercise therapy, and nerve blocks. Mirogabalin, a selective oral α2δ ligand, is approved for treating peripheral neuropathic pain, though data regarding visual analog scores (VAS) for pain in patients with LSS are limited. We investigated the efficacy and safety of mirogabalin as an add-on treatment in patients with LSS taking NSAIDs compared with patients taking NSAIDs only.
Methods
This multicenter, randomized, open-label study (MiroTAS) was conducted at 32 centers in Japan between June 2020 and October 2021. Patients were randomly assigned to mirogabalin and NSAIDs or NSAIDs alone in a 1:1 ratio. NSAIDs were administered according to their Japanese package inserts; mirogabalin was administered based on renal function [creatinine clearance (CrCL) ≥ 60 mL/min, 5 mg twice daily (BID) in Weeks 1–2, 10 mg BID in Weeks 3–4, and 15 or 10 mg BID after Week 5; CrCL 30 to < 60 mL/min, 2.5 mg BID Weeks 1–2, 5 mg BID Weeks 3–4, and 7.5 or 5 mg BID after Week 5]. The primary endpoint was the change in VAS score for leg pain from baseline to Week 12. Secondary endpoints were quality of life, evaluated using the EuroQol five-dimensional descriptive system (EQ-5D-5L) (at baseline and Week 12) and Patient Global Impression of Change (PGIC) (at Week 12), and safety. Change in VAS score at Week 12 was calculated using a linear mixed model for repeated measures. The safety endpoints were treatment-emergent adverse events (TEAEs) and adverse drug reactions.
Results
In total, 220 patients who met the eligibility criteria were enrolled. In the mirogabalin and NSAIDs and NSAIDs groups, mean ages (67.8 vs. 70.9 years), proportions of female patients (54.5% vs. 49.0%), mean body weights (63.9 vs. 62.0 kg), mean CrCL values (81.5 vs. 70.7 mL/min), proportions of patients with CrCL 30 to < 60 mL/min (27.3% vs. 33.7%), mean VAS scores (63.8 vs. 62.8 mm), and proportions of patients with VAS score ≥ 60 (53.6% vs. 52.9%) at enrollment were similar. The median durations of LSS were 9.0 and 11.0 months and the spine pain DETECT questionnaire (SPDQ) scores were 6.8 and 7.8, respectively. The least square (LS) mean change in VAS score from baseline to Week 12 was − 24.1 mm in the mirogabalin and NSAIDs group and − 14.2 mm in the NSAIDs group (both P < 0.0001 vs. baseline). The difference in LS mean was − 9.9 [95% confidence interval (CI), − 18.0, − 1.8] (P = 0.0174). The improvement in EQ-5D-5L score at Week 12 was significantly greater in the mirogabalin and NSAIDs group versus the NSAIDs group [mean difference, 0.0529 (95% CI, 0.0036, 0.1022), P = 0.0357]. At Week 12, the proportions of patients with PGIC scores ≤ 3 and ≤ 2 were higher in the mirogabalin and NSAIDs group vs. the NSAIDs group (76.2% vs. 50.0%, P = 0.0006, and 47.6% vs. 32.4%, P = 0.0523). In the mirogabalin and NSAIDs group, the incidences of TEAEs and adverse drug reactions were 60.9% and 57.3%, respectively, and the most common TEAEs were somnolence (30.0%) and dizziness (25.5%).
Conclusions
The addition of mirogabalin to NSAIDs improved VAS, EQ-5D-5L, and PGIC. The main TEAEs were somnolence and dizziness. The addition of mirogabalin to NSAIDs improved peripheral neuropathic pain associated with LSS and raised no new safety concerns.
Trial Registration
Japan Registry of Clinical Trials (jRCTs021200007).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Mirogabalin, a potent selective ligand of the α2δ subunit of voltage-gated Ca2+ channels, has been approved for use in Japan, Korea, and Taiwan. |
The efficacy of mirogabalin in improving peripheral neuropathic pain in patients with lumbar spinal stenosis (LSS) has been previously reported, but the number of studied cases is limited, and its efficacy and safety have not been fully investigated. |
We conducted a multicenter, randomized, open-label, parallel group, interventional study to assess the efficacy and safety of mirogabalin as an add-on in LSS patients taking non-steroidal anti-inflammatory drugs (NSAIDs) compared with those taking NSAIDs alone. |
What was learned from the study? |
Mirogabalin as an add-on to NSAIDs led to clinically meaningful improvement in pain intensity (visual analog scale score) and quality of life (EuroQol five-dimensional descriptive system and Patient Global Impression of Change questionnaire) with greater improvements than with NSAIDs alone in LSS patients. |
Mirogabalin as an add-on in LSS patients treated with NSAIDs was generally well tolerated. |
Mirogabalin as an add-on to NSAIDs may be an option for LSS patients who cannot achieve adequate pain control with NSAIDs only. |
Introduction
Lumbar spinal stenosis (LSS) describes patients who present symptoms associated with an anatomical reduction in the size of the spinal canal, and is one of the most commonly encountered spinal disorders [1]. The prevalence of LSS in Japan has been reported as approximately 5–20% [2,3,4,5,6], and the prevalence and economic burden associated with LSS are both expected to increase substantially given the aging population [4, 7, 8]. Although the mechanism of LSS is not fully understood, the Japanese Orthopaedic Association (JOA) Clinical Practice Guidelines on the Management of Lumbar Spinal Stenosis 2021 defines LSS as a syndrome in which the spinal canal and intervertebral foramen, which are nerve pathways, are narrowed owing to degeneration of the lumbar discs and intervertebral joints [9]. LSS often presents with neuropathic pain [10], which is implicated in causing leg pain in patients with LSS through compressed nerve roots, oedema, fibrosis, demyelination, and axonal degeneration of the involved neural elements [11,12,13].
According to the JOA guidelines, there is no clear standard for choosing between conservative therapy and surgery in Japan [9]. Accordingly, physicians make their own decisions based on the symptoms of each individual patient. Conservative therapy is the first choice for Japanese LSS patients and includes non-steroidal anti-inflammatory drugs (NSAIDs), prostaglandin E1, tramadol, physical/exercise therapy, and nerve blocks [9]. When conservative therapy fails to provide a satisfactory response, surgical therapy is undertaken. Treatment with NSAIDs is suggested for short-term use in LSS patients with nerve root or low back pain according to the JOA guidelines, and NSAIDs are often prescribed in daily practice [9]. In addition, neuropathic pain medications may be used to treat LSS patients experiencing neuropathic pain [14]. Several studies have reported that gabapentinoids, such as gabapentin and pregabalin, are effective in improving pain, walking distance, and quality of life (QOL) scores for LSS patients [11, 12, 15,16,17,18,19,20]. However, the JOA guidelines state that no clear recommendation can be made for administering these drugs to LSS patients because of insufficient evidence for efficacy and safety [9]. According to the guideline recently published by the US Association for the Study of Pain, evidence of efficacy with pregabalin and gabapentin is consensus-based and of very low quality, respectively [21].
Mirogabalin is a selective oral α2δ ligand, like pregabalin, and was first approved for treatment of peripheral neuropathic pain in 2019 in Japan [22]. Mirogabalin has been shown to be effective and well tolerated in the management of postherpetic neuralgia [23] and diabetic peripheral neuropathic pain in Asian patients [24]. Recently, a randomized, double-blind, placebo-controlled, phase 3 study was conducted to investigate the efficacy and safety of mirogabalin for central neuropathic pain in patients with spinal cord injury due to trauma (ClinicalTrials.gov Identifier: NCT03901352). Although the results of this study have not yet been published, they are the basis of the recent expanded indication of miroglabalin to include central neuropathic pain. Results from the previously conducted MIROP study suggested that mirogabalin reduces visual analog scale (VAS) pain scores in patients with LSS [25]. However, this study assessed a small number of cases, and further investigations into the efficacy and safety of mirogabalin for LSS, a common spinal disorder associated with peripheral neuropathic pain, are warranted. Additionally, previous studies did not evaluate the effect of mirogabalin on quality-of-life measures such as the EuroQol five-dimensional descriptive system (EQ-5D-5L).
This study evaluated the efficacy and safety of mirogabalin as an add-on treatment in LSS patients taking NSAIDs, a conventional therapy, compared with LSS patients taking only NSAIDs to determine whether, in a large study, mirogabalin could reduce VAS pain scores in patients with LSS.
Methods
Trial Design
The MiroTAS study was a multicenter, randomized, open-label, parallel group, interventional study, which took place in 32 centers in Japan between June 2020 and October 2021 (Fig. 1). The study received approval from the Clinical Research Review Committee, Fukushima Medical University Certified Review Board (CRB No. CRB2200002), which notified all participating centers of the approval. This was done in accordance with the Clinical Research Act in Japan; the CRB conducted a central review, and after the study was approved by the CRB, each site obtained permission from their administrator to start the research. Note that there is no need to hold an Ethical Review Committee for each facility according to the Clinical Research Act. The study was conducted in accordance with the ethical principles, clinical research laws, and relevant notifications stipulated in the Declaration of Helsinki (as revised in 2013). This study was registered in the Japan Registry of Clinical Trials under the identifier jRCTs021200007.
After obtaining informed consent, if patients used concomitantly contraindicated drugs (gabapentin, pregabalin, duloxetine, probenecid, cimetidine, or lorazepam) prior to study participation, a washout period of ≥ 7 days was set prior to study enrollment. NSAIDs were administered according to their Japanese package insert and a dose change was not permitted during the study period. Patients taking mirogabalin and NSAIDs were given NSAIDs as described above, and mirogabalin was administered based on the renal function of the patients as follows: for patients with creatinine clearance (CrCL) ≥ 60 mL/min, mirogabalin was administered at 5 mg twice daily (BID) for the first 2 weeks, 10 mg BID for the next 2 weeks, and 15 mg BID or 10 mg BID after Week 5; and for patients with CrCL 30 to < 60 mL/min, mirogabalin was administered at 2.5 mg BID for 2 weeks, 5 mg BID for 2 weeks, and 7.5 mg BID or 5 mg BID after Week 5. From the time of informed consent to the end of the study (or discontinuation), changes to, or additions of, new drugs/therapies for pain treatment were avoided as much as possible. No placebo was administered during this study to either treatment group.
At the time of enrollment, patient background factors were evaluated, including age, sex, weight, VAS score, spine pain DETECT questionnaire (SPDQ) score [26], short form SPDQ (SF-SPDQ) score, EQ-5D-5L score, Brief Scale for Psychiatric Problems in Orthopedic Patients (BS-POP) score, and compliance with the package insert, among others. Regarding the SPDQ and SF-SPDQ, we investigated the number and percentage of patients with SPDQ and SF-SPDQ scores of < 0 and ≥ 0.
Patients
The investigators explained what participation in this clinical study entailed to patients who were considered suitable for enrollment. Patients who agreed to participate in the study needed to be able to understand the study procedures and answer questions appropriately. After confirmation of eligibility, patients were randomly assigned to the mirogabalin and NSAIDs group or the NSAIDs only group in a 1:1 ratio using the permuted block method based on the VAS score (< 60 mm or ≥ 60 mm) at study enrollment (baseline) as an allocation adjustment factor.
The inclusion criteria were as follows: patients diagnosed with leg pain due to radicular type of LSS, who met the following four criteria according to the judgment of a physician ≥ 3 months before enrollment: (1) pain or numbness from the buttocks to the lower extremities (patients with only bilateral numbness from the buttocks to the lower extremities were excluded), (2) pain or numbness from the buttocks to the lower extremities that was aggravated by standing or walking and relieved by bending forward or sitting up, (3) if isolated, low back pain that was aggravated by walking was ruled out, and (4) magnetic resonance imaging and other imaging studies confirmed degenerative stenosis of the spinal canal and foramen intervertebralis, and the clinical findings could be explained (LSS International Classification of Diseases [ICD] 10 code, M4806); who had been taking NSAIDs for ≥ 4 weeks without a change in dose; had a VAS score of ≥ 40 mm both at the time of informed consent and at enrollment; and were aged ≥ 20 years. Patients were excluded if they used prohibited drugs concomitantly within 7 days prior to study enrollment; changed the usage and dosage of concomitantly restricted drugs within 4 weeks prior to study enrollment; had severe pain other than LSS at the time of study enrollment, which was considered difficult to evaluate; had cauda equina or mixed-type LSS; had a history of lumbar spine surgery; had cancer, infection, or bone fracture at the time of study enrollment; had a history of hypersensitivity to the components of mirogabalin; had serious hepatic, renal, or cardiac diseases that made participation in this study difficult; had CrCL < 30 mL/min (Cockcroft–Gault formula) at the time of study enrollment; had a score of (a) ≥ 11 for physicians on the BS-POP or (b) both ≥ 10 for physicians and ≥ 15 for patients on the BS-POP at the time of study enrollment [27]; were considered unsuitable for study participation as judged by the treating physician or study investigator; or had taken mirogabalin in the past. In addition, pregnant women, patients who may have been pregnant, and lactating patients were also excluded. All patients provided written informed consent.
Endpoints
The primary efficacy endpoint was the change in VAS score for leg pain from the study enrollment (baseline) to Week 12 (on a 100-mm scale; 0 mm for no pain and 100 mm for the worst pain imaginable). The secondary efficacy endpoints were QOL evaluated using the EQ-5D-5L (at baseline and Week 12) and Patient Global Impression of Change (PGIC) (at Week 12) [28]. PGIC was scored by patients rating their improvement on a scale from 1 = “very much improved” to 7 = “very much worse” at the end of treatment. The other efficacy endpoint was the VAS score for leg pain at each evaluation timepoint (baseline, Weeks 2, 4, 8, and 12) and changes from baseline at each evaluation timepoint.
The safety endpoint was the occurrence of treatment-emergent adverse events (TEAEs) and adverse drug reactions (ADRs). A TEAE was defined as an adverse event (AE) that occurred after randomization and initiation of the assigned study drug, or that worsened relative to the pre-treatment status. An ADR was defined as a TEAE judged by the physician to have a causal relationship with the study drug. The worsening of the primary disease and symptoms related to increased pain as judged by the principal investigator (submitting physician) were not treated as AEs.
Subgroup Analysis
According to the patients’ compliance with the package insert, patients were divided into two subgroups (compliant and non-compliant groups). Baseline patient demographic and clinical characteristics, as well as changes in VAS scores and EQ-5D-5L scores from baseline to Week 12, proportions of patients with PGIC scores ≤ 3 and ≤ 2, and the incidence of TEAEs and ADRs were evaluated in subgroups according to compliance with the package insert. In addition, changes in VAS scores from baseline to Week 12 were also evaluated in subgroups according to baseline VAS, renal function, type of LSS symptoms, SPDQ score, and SF-SPDQ score.
Statistical Analysis
The primary efficacy analysis was performed using the modified intention-to-treat (mITT) population, which was defined as all patients from the randomized analysis population who received at least one dose of the study drug. A sensitivity analysis for efficacy endpoints was performed using the per protocol set (PPS), which was defined as all patients in the mITT population who complied with the study protocol.
For the change in VAS score at Week 12 in the mITT population, a linear mixed model for repeated measures (MMRM) was used to calculate the estimated difference in the adjusted means between treatment groups and its 95% confidence interval (CI) and P value. The MMRM included treatment group, treatment duration (week), and treatment group–week interactions as fixed effects, VAS at study enrollment (baseline) as a covariate, and patients as a variable effect. The same statistical analysis method was used to assess changes in VAS scores from baseline to Week 12 in subgroups according to baseline VAS, renal function, types of LSS symptoms, SPDQ scores, SF-SPDQ scores, and compliance with the package insert.
For sensitivity analysis, the last observation carried forward (LOCF) and baseline observation carried forward (BOCF) methods were used to supplement the VAS scores at Week 12 in the mITT population. After LOCF and BOCF, analysis of covariance (ANCOVA) was used to compare the change in VAS score between the treatment groups at Week 12.
Analysis of EQ-5D-5L scores was performed using the mITT population. Summary statistics for EQ-5D-5L score conversions were calculated for each treatment group at each measurement timepoint and for the change from baseline. In addition, for the five domains of mobility, personal care, daily activities, pain/discomfort, and anxiety, frequency tables were prepared for each measurement timepoint, and cross frequency tables were prepared for each timepoint relative to the time of study enrollment (baseline). To handle missing data, complete case analyses were conducted to delete data for each patient if even one visit was missing. PGIC scoring was performed on the mITT population. A frequency table for PGIC scores at the end of treatment was created for each treatment group. The same statistical method was used to assess EQ-5D-5L and PGIC scores in the subgroups in compliance with the package insert.
The safety analysis set was defined as the population consisting of patients who were enrolled in the study and had received at least one dose of the study drug. AEs were coded using the Medical Dictionary for Regulatory Activities (MedDRA/J ver. 24.1). The number and percentage of patients in each treatment group who reported a TEAE was calculated. The number and percentage of patients with TEAEs and ADRs were summarized by System Organ Class and Preferred Term.
The significance level for hypothesis testing was set at 5%, and the CI for both sides was 95%. The statistical analysis was performed using SAS v.9.4 (SAS Institute, Cary, NC, USA).
Sample Size
Based on previous clinical studies of mirogabalin [23], assuming that the mean difference of the VAS score change between treatment groups at Week 12 was set as 8 mm and the standard deviation (SD) was set as 20 mm, a sample size of 266 (133 per arm) patients was needed to achieve a 90% power with a 5% two-sided significance level. Considering dropouts, the target number of patients was set at 300 (150 patients/group).
Results
Patients
As it was difficult to recruit patients who met the eligibility criteria during the enrollment period owing to the COVID-19 pandemic, only 220 patients were registered, and enrollment was completed without reaching the target sample size (n = 300) despite extending the registration period.
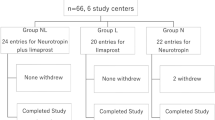
Informed consent was obtained from 233 patients; of these, 220 patients who met the eligibility criteria were enrolled in the study (Fig. 2). The mITT population included 110 patients in the mirogabalin and NSAIDs group and 104 patients in the NSAIDs group. The safety analysis set comprised 110 patients in the mirogabalin and NSAIDs group and 106 patients in the NSAIDs group. In the mirogabalin and NSAIDs group and the NSAIDs group, 87 and 75 patients, respectively, completed the study; the most common reasons for study withdrawal were TEAEs and patient’s request to discontinue the study.
Patient demographic and clinical characteristics for the mITT population are shown in Table 1. In the mirogabalin and NSAIDs group and the NSAIDs group, the respective mean ages (67.8 vs. 70.9 years), proportions of female patients (54.5% vs. 49.0%), mean body weights (63.9 vs. 62.0 kg), mean CrCL values (81.5 vs. 70.7 mL/min), proportions of patients with CrCL 30 to < 60 mL/min (27.3% vs. 33.7%), mean VAS scores (63.8 vs. 62.8 mm), and proportions of patients with VAS score ≥ 60 (53.6% vs. 52.9%) at enrollment were similar. The median duration of LSS was 9.0 months in the mirogabalin and NSAIDs group and 11.0 months in the NSAIDs group. The distribution of the pain and LSS symptoms, in the buttocks and bilateral legs, did not differ between the groups. The most common complications were hypertension, hyperlipidemia, and complications of orthopedic diseases. The most common types of NSAIDs used were celecoxib and loxoprofen sodium hydrate. Compliance with the package insert (compliant group) was reported in 74.5% of patients in the mirogabalin and NSAIDs group and 96.2% of patients in the NSAIDs group. The rescue medication (acetaminophen) was less prescribed in the mirogabalin and NSAIDs group than in the NSAIDs group (60.0% vs. 78.8%). Similar results were obtained when patient demographic and clinical characteristics were evaluated in patients who were compliant with the package insert (Supplementary Material Table S1).
The daily dose of mirogabalin at baseline and Weeks 2, 4, 8, and 12 according to renal function in the mITT population is shown in Supplementary Material Table S2. Among patients with normal/mild renal function (CrCL ≥ 60 mL/min), 9 (14.5%) and 44 (71.0%) patients received effective doses of 10 mg BID and 15 mg BID, respectively. Among patients with moderate renal impairment (CrCL 30 to < 60 mL/min), 5 (21.7%) and 15 (65.2%) patients received effective doses of 5 mg BID and 7.5 mg BID, respectively. Most patients (95% to 100%) reported that they were “mostly compliant (> 75%)” at all timepoints and for both CrCL subgroups (data not shown).
Efficacy
The least square (LS) mean change ± standard error (SE) in VAS score for leg pain from baseline to Week 12 (primary endpoint) was − 24.1 ± 2.8 mm (95% CI − 29.6, − 18.6; P < 0.0001 vs. baseline) in the mirogabalin and NSAIDs group and − 14.2 ± 3.0 mm (95% CI − 20.2, − 8.3; P < 0.0001 vs. baseline) in the NSAIDs group. Using MMRM analysis, the difference in LS mean was − 9.9 (95% CI − 18.0, − 1.8; P = 0.0174) (Table 2). Similar significant results were obtained in the PPS [difference in LS mean (95% CI), − 12.2 (– 20.5, − 3.9), P = 0.0040; by MMRM analysis], LOCF [difference in LS mean (95% CI), − 10.2 (– 17.3, − 3.2), P = 0.0047; by ANCOVA] and BOCF [difference in LS mean (95% CI), − 8.1 (− 14.8, − 1.4), P = 0.0176; by ANCOVA] as a sensitivity analysis (data not shown in Tables and Figures). The VAS score for leg pain gradually decreased from baseline to Week 12 in both groups (Fig. 3a). The change in VAS score from baseline to Week 12 was significantly higher in the mirogabalin and NSAIDs group versus the NSAIDs group [difference in mean (95% CI), − 9.9 (− 18.4, − 1.4), P = 0.0229; by t test] (Fig. 3b). Similar significant results were obtained in LOCF and BOCF. Additionally, a significant decrease in the VAS score was shown in the mirogabalin and NSAIDs group compared with the NSAIDs group starting at Week 8 [difference in mean (95% CI), − 13.7 (− 21.7, − 5.7), P = 0.0009; by t test] (Fig. 3b).
a VAS score for leg pain and b its change from baseline (mITT population). Data are mean ± SD. No statistical tests were conducted for the results shown in a; analysis by t test was conducted to obtain the P values in b. *P < 0.05 for between-group differences. **P < 0.01 for between-group differences. BOCF baseline observation carried forward, CI confidence interval, LOCF last observation carried forward, mITT modified intention-to-treat, NSAIDs non-steroidal anti-inflammatory drugs, SD standard deviation, VAS visual analog scale
In the subgroups according to compliance with the package insert, similar significant improvements in VAS scores from baseline to Week 12 were observed (Supplementary Material Figure S1 and Table S3). In the compliant subgroup, a significant decrease in VAS score was shown in the mirogabalin and NSAIDs group versus the NSAIDs group (LS mean − 10.2; 95% CI − 18.8, − 1.5; P = 0.0212) (Supplementary Material Table S3).
The changes in VAS scores from baseline to Week 12 in subgroups according to baseline VAS score, renal function, type of LSS symptoms, SPDQ score, and SF-SPDQ score are shown in Supplementary Material Table S3. In subgroups with VAS score < 60 mm, CrCL ≥ 60 mL/min, both pain and numbness, and SPDQ and SF-SPDQ total score ≥ 0, the mirogabalin and NSAIDs group had a significant tendency for a decreased VAS score compared with the NSAIDs group, although there was bias in the number of patients. In the other subgroups, there was a numerical decrease in VAS score in the mirogabalin and NSAIDs group versus the NSAIDs group.
Regarding the secondary endpoints, the EQ-5D-5L score improved from baseline to Week 12 in both treatment groups (Table 3). The improvement in EQ-5D-5L score at Week 12 was significantly greater in the mirogabalin and NSAIDs group compared with the NSAIDs group [mean difference (95% CI), 0.0529 (0.0036, 0.1022), P = 0.0357]. When evaluating each item of the EQ-5D-5L, the proportion of patients with no problems increased from baseline to Week 12 for all items in the mirogabalin and NSAIDs group (Supplementary Material Table S4). A similar tendency in EQ-5D-5L score changes in the mITT population was observed among patients who were compliant with the package insert (Supplementary Material Table S5).
At Week 12, the proportion of patients with a PGIC score ≤ 3 (the sum of minimally, much, and very much improved) was significantly higher in the mirogabalin and NSAIDs group versus the NSAIDs group (76.2% vs. 50.0%, respectively, P = 0.0006) (Table 4). The proportion of patients with PGIC score ≤ 2 (the sum of much and very much improved) at Week 12 was 47.6% in the mirogabalin and NSAIDs group, and 32.4% in the NSAIDs group (P = 0.0523). A similar tendency in PGIC score results was observed among patients in the mITT population who were compliant with the package insert (Supplementary Material Table S6).
Safety
TEAEs and ADRs occurring in ≥ 2% patients are shown in Table 5. The incidence of TEAEs was 60.9% and 14.2% in the mirogabalin and NSAIDs group and NSAIDs group, respectively, and that of ADRs was 57.3% and 3.8%, in each group, respectively. The proportion of patients who discontinued treatment due to a TEAE or ADR was 8.2% vs. 0.0%, in each group, respectively. The most common TEAEs in the mirogabalin and NSAIDs group were somnolence (30.0%), dizziness (25.5%), oedema peripheral (5.5%), and constipation (5.5%). Most TEAEs were mild or moderate in severity, and no serious TEAEs or deaths were reported in the mirogabalin and NSAIDs group. Weight gain, which is a known side-effect of gabapentinoids, occurred in 1.8% (n = 2) of patients in the mirogabalin group and 0% (n = 0) in the NSAIDs group as TEAEs, and as ADRs in 1.8% (n = 2) and 0% (n = 0) of patients in the mirogabalin and NSAIDs groups, respectively. In the NSAIDs group, there was one serious TEAE of breast cancer, which was determined to have no causal relationship to NSAID use; the outcomes were mild, and no deaths were reported during the study period. The most common TEAEs leading to treatment discontinuation were somnolence (1.8%), dizziness (1.8%), and diarrhea (1.8%). A similar tendency in the incidence of TEAEs and ADRs in the safety analysis set was observed in the subgroups according to compliance with the package insert (Supplementary Material Table S7).
Discussion
The MiroTAS study was a multicenter, randomized, open-label, parallel group, interventional study that aimed to assess the efficacy and safety of mirogabalin as an add-on in LSS patients taking NSAIDs compared with those taking NSAIDs alone. A total of 220 patients met the eligibility criteria and were enrolled in the study. Baseline patient demographic and clinical characteristics were generally well balanced between the two treatment groups.
Improvement in VAS Score
The VAS score for leg pain decreased significantly from baseline to Week 12 in both the mirogabalin and NSAIDs group (LS mean change, − 24.1 ± 2.8 mm) and the NSAIDs group (− 14.2 ± 3.0 mm) (both P < 0.0001 vs. baseline). This improvement in VAS score was significantly greater in the group taking mirogabalin as an add-on to NSAIDs compared with the group taking NSAIDs alone (P = 0.0174). These results are similar to previous phase 3 studies of mirogabalin vs. placebo for the treatment of Asian patients with diabetic peripheral neuropathic pain (mean change in VAS score at Week 14, − 22.5 mm) and postherpetic neuralgia (mean change in VAS score at Week 14, − 21.4 mm) [23, 24], and a subgroup analysis of the MIROP study (mean change in VAS score at Week 4, − 15.7 mm) [25]. In clinical practice, the fact that the VAS improved by > 20 mm in the group taking mirogabalin as an add-on to NSAIDs in this study is a clinically meaningful difference [29]. As noted by Ostelo et al., a 30% improvement from baseline is considered clinically meaningful for general pain related to back disorders [30]. Other studies have reported minimal clinically important differences of 1.6 points (VAS 16 mm) for leg pain and 2 points (VAS 20 mm) for leg pain and numbness [31, 32]. In the present study, improvements for patients in the mirogabalin and NSAIDs group exceeded the minimum clinically important differences described above, but those in the NSAIDS group did not.
One previous study reported that the combination of pregabalin and NSAIDs improved VAS score for leg pain at Week 6 (95% CI − 2.3, − 0.9) [17], and another study reported that a combination of pregabalin plus limaprost as a prostaglandin E2 analog decreased the VAS score (baseline, 6.7 cm; Week 8, 4.2 cm) [20]. These results were generally consistent with those of the present study. However, some previous studies of gabapentin reported different results in VAS score from our study [12, 15]. In 28 patients receiving combination therapy with gabapentin, NSAIDs, physical therapy exercises, and a lumbosacral corset, the mean VAS score decreased from baseline (7.0 ± 1.5 cm) to Week 16 (2.9 ± 2.6 cm) [12]. In that study, the control group consisting of patients receiving NSAIDs, physical therapy exercises, and a lumbosacral corset also had a decreased mean VAS score (baseline, 6.7 ± 1.2 cm; Week 16, 4.7 ± 2.2 cm). In a previous study of patients with chronic low back pain, exercise therapy was shown to have equivalent efficacy to that of NSAIDs use [33]. Thus, the difference in the presence or absence of physical therapy exercises may explain the difference of VAS reduction between the previous and present studies. It is also noted that the differences from the control group in VAS reduction is similar between the previous and present studies. Another study reported better improvement of VAS score in LSS patients taking gabapentin for 12 weeks compared with our study (baseline, 7.0 ± 0.9 cm; Week 12, 2.1 ± 1.5 cm) [15]. However, that study did not report detailed data such as patient background, had a relatively small number of cases (n = 45), bias of female patients (89%), inclusion of patients in acute pain due to LSS, and inclusion of patients who had received no prior treatment for LSS, which makes it difficult to compare the findings with our study. Notably, the current study shows that mirogabalin as an add-on to NSAIDs exhibits good efficacy for LSS patients, which is equivalent to pregabalin and gabapentin.
In this study, the change in VAS of leg pain at Week 8 in the mirogabalin and NSAIDs group was significantly different from that in the NSAIDs group. These results suggested that the effective dose of mirogabalin was reached at Week 8 and that it was important to increase the dose of mirogabalin to the effective dose. In contrast, in the 14-week Asian phase 3 study, a significant difference in the change of pain intensity in the mirogabalin group versus the placebo group was observed from the early phase (Week 1) after administration of mirogabalin, which was administered at low doses [24]. The reason for the difference in the time of onset of efficacy between the present study and the previous study is not clear. However, elements of the study design such as target disease, placebo control, single use or combination use, add-on to NSAIDs, and open-label use were different. Particularly, the NSAIDs group had a stronger effect of VAS reduction than initially expected, which may be explained as a placebo effect. However, as the statistical analysis used in our study was based on the difference from NSAIDs, we considered there to be no possibility of overestimating the efficacy of mirogabalin due to a placebo effect.
Mirogabalin as an add-on to NSAIDs showed a certain improvement in VAS regardless of renal function, although there was no statistically significant difference between the mirogabalin and NSAIDs group and the NSAIDs group in the subgroup with CrCL 30 to < 60 mL/min, which may be due to the small number of cases. It is possible that the percentage of patients who reached the effective dose of mirogabalin at the end of the study was relatively high regardless of renal function (both CrCL subgroups, > 85%).
In terms of the type of LSS symptoms, mirogabalin significantly reduced VAS scores in patients with pain, and both pain and numbness. When comparing the mirogabalin and NSAIDs group and the NSAIDs group, there was no statistically significant difference in the improvement in VAS score in the subgroup with pain alone, which may be due to the relatively small number of cases. To the best of our knowledge, there are no reports of gabapentinoids, such as pregabalin and gabapentin, analyzed in terms of their effect by type of LSS symptoms. Our results suggest that mirogabalin treatment may improve numbness in patients, which is not expected with gabapentinoids. While this study showed mirogabalin improved pain and numbness symptoms in LSS patients, we evaluated the pain intensity for affected legs using VAS scores and did not evaluate index scale of numbness. Further studies are required to evaluate the efficacy of mirogabalin for the treatment of numbness.
The SPDQ, recently developed by Nikaido et al., is a simple screening tool for the diagnosis of neuropathic pain due to spinal disorders, and although its specificity is relatively low, its sensitivity is good and it is highly convenient [26]. In this study, the majority of patients were diagnosed using the SPDQ and SF-SPDQ as having possible neuropathic pain, and for these patients, mirogabalin as an add-on to NSAIDs significantly reduced VAS more than NSAIDs alone. However, a similar trend was not observed in a small number of patients who were not diagnosed with possible neuropathic pain by the SPDQ and SF-SPDQ. These results suggest that mirogabalin may be particularly effective for neuropathic pain among patients with LSS.
Improvement in QOL (EQ-5D-5L and PGIC)
The goal of treating neuropathic pain is to reduce pain and improve daily living and QOL, rather than to eliminate the pain [34]. Our study showed that mirogabalin as an add-on to NSAIDs improves QOL indices such as EQ-5D-5L and PGIC with statistically and clinically meaningful differences compared with NSAIDs alone.
Improvement of EQ-5D-5L scores from baseline when mirogabalin was added on to NSAIDs was 0.0787 at Week 12, which exceeds the minimal important difference of 0.061 [35]. Additionally, mirogabalin improved EQ-5D-5L scores within a similar range to a previous study of pregabalin for patients with neuropathic pain and spine disease mostly taking NSAIDs (95%) (EQ-5D-5L LS mean change from baseline, 0.08 at Week 8) [36].
Mirogabalin as an add-on to NSAIDs also improved PGIC, and patient ratios of “minimally improved or better” and “much improved or better” were similar to those in previous phase 3 studies for patients with diabetic peripheral neuropathic pain and postherpetic neuralgia (30 mg/day mirogabalin, PGIC score ≤ 3, 76.2% vs. 70%, 69%; PGIC score ≤ 2, 47.6% vs. 40%, 34%) [23, 24]. Our result is also consistent with a previous study of pregabalin for patients with chronic low back pain with lower limb pain (including 31% LSS, of whom 97% were taking NSAIDs) (PGIC score ≤ 3, 76.2% vs. 74%) [37]. These results suggest that mirogabalin can not only reduce pain, but also improve QOL in patients with LSS taking NSAIDs.
Safety
There was no significant difference between the proportion of patients in the two groups who dropped out. Although there was an increase in AEs in the mirogabalin and NSAIDs group compared with the NSAIDs group, it was comparable to previous trials of mirogabalin [23, 24]. The major types of AEs were not new and were similar to those observed in previous trials [23, 24]. Safety findings were also consistent with those of previous studies of pregabalin [17, 20, 36] or gabapentin [38]. The incidences of oedema peripheral as a TEAE of mirogabalin treatment have previously been reported to be 4.6% [23] and 11.2% [24], which are similar to that seen in this study (5.5%). Previous phase III trials of mirogabalin have also observed the TEAE incidences of weight gain to be 7.9% [24] and 9.3% [23]. In this study, we observed far fewer incidences of weight gain (1.8%), although the reasons for this are unclear. Mirogabalin can be used for continued treatment with the risk of fewer AEs as it is possible to fine-tune dose adjustments after the titration period. When using mirogabalin for treatment, careful attention should be paid to the possibility of patients developing somnolence and dizziness.
Limitations
The present study is limited and biased by its open-label study design. The target sample size was not reached due to the impact of the COVID-19 pandemic. The present study only included patients with the radicular type of LSS with VAS scores of ≥ 40 mm. Additionally, muscle strength, functional disability, and sensory status, which are considered important outcome measures, were not evaluated.
Conclusion
The addition of mirogabalin to NSAIDs improved peripheral neuropathic pain associated with LSS and raised no new safety concerns, although caution is recommended due to the possibility of somnolence and dizziness. The results of this study suggest that mirogabalin may be a new treatment option for pain in patients with LSS patients, potentially broadening treatment options and improving quality of life for patients with LSS who experience pain.
Change history
06 October 2022
A Correction to this paper has been published: https://doi.org/10.1007/s40122-022-00441-6
References
Deer T, Sayed D, Michels J, Josephson Y, Li S, Calodney AK. A review of lumbar spinal stenosis with intermittent neurogenic claudication: disease and diagnosis. Pain Med. 2019;20:S32–44.
Miyakoshi N, Hongo M, Kasukawa Y, Ishikawa Y, Shimada Y. Prevalence, spinal alignment, and mobility of lumbar spinal stenosis with or without chronic low back pain: a community-dwelling study. Pain Res Treat. 2011;2001:340629.
Nagata K, Yoshimura N, Muraki S, et al. Prevalence of cervical cord compression and its association with physical performance in a population-based cohort in Japan: the Wakayama Spine Study. Spine (Phila Pa 1976). 2012;37:1892–8.
Yabuki S, Fukumori N, Konno S, et al. Prevalence of lumbar spinal stenosis, using the diagnostic support tool, and correlated factors in Japan: a population-based study. J Orthop Sci. 2013;18:893–900.
Ishimoto Y, Yoshimura N, Muraki S, et al. Prevalence of symptomatic lumbar spinal stenosis and its association with physical performance in a population-based cohort in Japan: the Wakayama Spine Study. Osteoarthrit Cartil. 2012;20:1103–8.
Ishimoto Y, Yoshimura N, Yoshida M, et al. Associations between radiographic lumbar spinal stenosis and clinical symptoms in the general population: the Wakayama Spine Study. Osteoarthrit Cartil. 2013;21:783–8.
Tomkins-Lane C, Melloh M, Lurie J, et al. Consensus on the clinical diagnosis of lumbar spinal stenosis: results of an International Delphi Study. Spine (Phila Pa 1976). 2016;41:1239–46.
Otani K, Kikuchi S, Yabuki S, et al. Lumbar spinal stenosis has a negative impact on quality of life compared with other comorbidities: an epidemiological cross-sectional study of 1862 community-dwelling individuals. Sci World J. 2013;2013:590652.
The Japanese Orthopaedic Association. Japanese Orthopaedic Association (JOA) Clinical Practice Guidelines on the Management of Lumbar Spinal Stenosis. 2nd ed. Tokyo: Nankodo Co., Ltd.; 2021.
Park SY, An HS, Moon SH, et al. Neuropathic pain components in patients with lumbar spinal stenosis. Yonsei Med J. 2015;56:1044–50.
Takahashi N, Arai I, Kayama S, et al. Therapeutic efficacy of pregabalin in patients with leg symptoms due to lumbar spinal stenosis. Fukushima J Med Sci. 2014;60:35–42.
Yaksi A, Ozgonenel L, Ozgonenel B. The efficiency of gabapentin therapy in patients with lumbar spinal stenosis. Spine. 2007;32:939–42.
Sekiguchi M, Kikuchi S, Myers RR. Experimental spinal stenosis: relationship between degree of cauda equina compression, neuropathology, and pain. Spine. 2004;29:1105–11.
Japan Society of Pain Clinicians. Guidelines for the Pharmacologic Management of Neuropathic Pain. Second Edition. 2016. https://minds.jcqhc.or.jp/docs/minds/Pharmacologic-management-of-neuropathic-pain/Pharmacologic-management-of-neuropathic-pain.pdf. Accessed 7 July 2022.
Kasimcan O, Kaptan H. Efficacy of gabapentin for radiculopathy caused by lumbar spinal stenosis and lumbar disk hernia. Neurol Med Chir (Tokyo). 2010;50:1070–3.
Bansal S, Lubelski D, Thompson NR, et al. Membrane-stabilizing agents improve quality-of-life outcomes for patients with lumbar stenosis. Global Spine J. 2016;6:139146.
Orita S, Yamashita M, Eguchi Y, et al. Pregabalin for refractory radicular leg pain due to lumbar spinal stenosis: a preliminary prospective study. Pain Res Manag. 2016;2016:5079675.
Markman JD, Frazer ME, Rast SA, et al. Double-blind, randomized, controlled, crossover trial of pregabalin for neurogenic claudication. Neurology. 2015;84:265–72.
Haddadi K, Asadian L, Isazade A. Effects of nasal calcitonin vs. oral gabapentin on pain and symptoms of lumbar spinal stenosis: a clinical trial study. Clin Med Insights Arthritis Musculoskelet Disord. 2016;9:133–8.
Kim HJ, Kim JH, Park YS, et al. Comparative study of the efficacy of limaprost and pregabalin as single agents and in combination for the treatment of lumbar spinal stenosis: a prospective, double-blind, randomized controlled non-inferiority trial. Spine J. 2016;16:756–63.
Bussières A, Cancelliere C, Ammendolia C, et al. Non-surgical interventions for lumbar spinal stenosis leading to neurogenic claudication: a clinical practice guideline. J Pain. 2021;22:1015–39.
Deeks ED. Mirogabalin: first global approval. Drugs. 2019;79:463–8.
Kato J, Matsui N, Kakehi Y, Murayama E, Ohwada S, Sugihara M. Mirogabalin for the management of postherpetic neuralgia: a randomized, double-blind, placebo-controlled phase 3 study in Asian patients. Pain. 2019;160:1175–85.
Baba M, Matsui N, Kuroha M, et al. Mirogabalin for the treatment of diabetic peripheral neuropathic pain: a randomized, double-blind, placebo-controlled phase III study in Asian patients. J Diabetes Investig. 2019;10:1299–306.
Kimura Y, Yamaguchi S, Suzuki T, et al. Switching from pregabalin to mirogabalin in patients with peripheral neuropathic pain: a multi-center, prospective, single-arm, open-label study (MIROP Study). Pain Ther. 2021;10:711–27.
Nikaido T, Sumitani M, Sekiguchi M, Konno S. The Spine painDETECT questionnaire: Development and validation of a screening tool for neuropathic pain caused by spinal disorders. PLoS ONE. 2018;13: e0193987.
Watanabe K, Kikuchi S, Konno S, Niwa S, Mashiko H. Validation study of brief scale for psychiatric problems in orthopaedic patients (BS-POP). Rinsho Seikei Geka. 2005;40:745–51.
Herdman M, Gudex C, Lloyd A. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20:1727–36.
Wessberg P, Frennered K. Central lumbar spinal stenosis: natural history of non-surgical patients. Eur Spine J. 2017;26:2536–42.
Ostelo RWJG, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976). 2008;33:90–4.
Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY. Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J. 2008;8:968–74.
Ogura Y, Ogura K, Kobayashi Y, et al. Minimum clinically important difference of major patient-reported outcome measures in patients undergoing decompression surgery for lumbar spinal stenosis. Clin Neruol Neurosurg. 2020;196:105966.
Takahashi N, Omata JI, Iwabuchi M, Fukuda H, Shirado O. Therapeutic efficacy of nonsteroidal anti-inflammatory drug therapy versus exercise therapy in patients with chronic nonspecific low back pain: a prospective study. Fukushima J Med Sci. 2017;63:8–15.
Sumitani M, Sakai T, Matsuda Y, et al. Executive summary of the Clinical Guidelines of Pharmacotherapy for Neuropathic Pain: second edition by the Japanese Society of Pain Clinicians. J Anesth. 2018;32:463–78.
Shiroiwa T, Fukuda T, Ikeda S, et al. Japanese population norms for preference-based measures: EQ-5D-3L, EQ-5D-5L, and SF-6D. Qual Life Res. 2016;25:707–19.
Taguchi T, Nakano S, Nozawa K. Effectiveness of pregabalin treatment for neuropathic pain in patients with spine diseases: a pooled analysis of two multicenter observational studies in Japan. J Pain Res. 2021;14:757–71.
Taguchi T, Igarashi A, Watt S, et al. Effectiveness of pregabalin for the treatment of chronic low back pain with accompanying lower limb pain (neuropathic component): a non-interventional study in Japan. J Pain Res. 2015;8:487–97.
Atkinson JH, Slater MA, Capparelli EV, et al. A randomized controlled trial of gabapentin for chronic low back pain with and without a radiating component. Pain. 2016;157:1499–507.
Acknowledgements
The authors wish to thank the participants of this study.
Funding
This study was supported by Daiichi Sankyo, Co., Ltd., Tokyo, Japan, which also provided funding for fees associated with medical writing support and the journal’s Rapid Service Fee. Daiichi Sankyo Co., Ltd. was involved in the study design, planning of the data analysis, data interpretation, and development of the manuscript, but was not involved in data management and statistical analysis. EPS Co., Ltd. was directly involved in data management and statistical analysis. The study results were not influenced by the commercial sponsor of this study (Daiichi Sankyo Co., Ltd.).
Medical Writing, Editorial, and Other Assistance
The authors wish to thank all of the institutions and investigators that participated in this study (Supplementary Material Table S8). The authors thank Michelle Belanger, MD, of Edanz (http://www.edanz.com) for providing medical writing support, which was funded by Daiichi Sankyo Co., Ltd.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Conceptualization, Methodology, and Writing – Review & Editing: All authors; Investigation: Takuya Nikaido and Shin-ichi Konno; Formal Analysis: Takuya Nikaido and Taichi Nakatani; Validation: Takuya Nikaido and Taichi Nakatani; and Writing – Original Draft: Takuya Nikaido.
List of Investigators
A complete list of investigators can be found in Supplementary Material Table S8.
Prior Presentation
This research will be presented at The 35th Annual Meeting of the Japanese Clinical Orthopaedic Association (17–18 July 2022, Tokushima, Japan).
Disclosures
Takuya Nikaido received lecture fees from Daiichi Sankyo Co., Ltd. Hiroshi Takatsuna, Shunsuke Tabata, and Kazuhito Shiosakai are employees of Daiichi Sankyo Co., Ltd. Taichi Nakatani is an employee of EP-CRSU Co., Ltd., and has the current affiliation: CR Data Science Department, Clinical Research Center, Real World Evidence Business Headquarters, EPS Co., Ltd. 6–29, Shin-ogawamachi, Shinjuku-ku, Tokyo 162–0814, Japan. Shin-ichi Konno received lecture fees from Daiichi Sankyo Co., Ltd., Pfizer Japan Inc., and Eisai Co., Ltd.; and scholarship donations from Stryker Japan K.K.
Compliance with Ethics Guidelines
The trial was conducted in accordance with the ethical principles, clinical research laws, and relevant notifications stipulated in the Declaration of Helsinki (as revised in 2013). The study received approval from the Clinical Research Review Committee, Fukushima Medical University Certified Review Board (CRB No. CRB2200002), which notified all participating centers of the approval. This study was registered at the Japan Registry of Clinical Trials under the identifier jRCTs021200007. All patients provided written informed consent.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original online version of this article was revised to correct Endpoint (LS mean) and Endpoint (mean) in the text, Figure 3 and supplementary material.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Nikaido, T., Takatsuna, H., Tabata, S. et al. Efficacy and Safety of Add-on Mirogabalin to NSAIDs in Lumbar Spinal Stenosis with Peripheral Neuropathic Pain: A Randomized, Open-Label Study. Pain Ther 11, 1195–1214 (2022). https://doi.org/10.1007/s40122-022-00410-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-022-00410-z