Abstract
Introduction
The objective of the present study was to gain insight into patients’ experiences in a 4-week interdisciplinary chronic pain management program by determining major themes from patients’ written comments on exit questionnaires.
Methods
Upon completion of the program at the Chronic Pain Management Unit (CPMU), patients fill out program satisfaction (Pain Program Satisfaction Questionnaire) and evaluation of goal accomplishment (Self-Evaluation Scale) forms, sections of which are open-ended. Questionnaire data from 50 patients, admitted into the CPMU between May 2013 and December 2014, were randomly selected for this study. Written responses to open-ended sections were obtained. Comments were stratified by gender and coded using an inductive approach. Codes were grouped into categories which were further combined into several major themes.
Results
Six main themes extracted from comments were (1) impact of a strong interdisciplinary team, (2) learning to adapt in order to manage, (3) the Program as a stepping stone, (4) positive effects of a group effort, (5) improved mental health, and (6) benefits of the program.
Conclusion
The results of this analysis reinforce the effectiveness of the interdisciplinary CPMU program at improving patients’ quality of life. Findings may assist in the promotion of the program to stakeholders such as referral sources. The outcomes may also assist in the development of future programs that have similar goals. Concerns that arise within patients’ comments may assist clinicians in this program to make adjustments such that all unique needs are met.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic pain (CP) occurs when pain persists past the normal healing time of 3 months [1]. Approximately one-fifth of all Canadians over the age of 18 were living with CP in 2011 [2]. CP status is predictive of healthcare use, specifically primary care, emergency, and overnight hospital stays [3]. It is, therefore, evident that people living with CP spend a significant amount of time in the healthcare environment. Whether it is single physician visits or an outpatient program lasting several weeks, it is important that these patients’ experiences are evaluated to allow for evidence-based improvements [4].
Patient experience is defined as “the sum of all interactions, shaped by an organization’s culture, that influence patients’ perceptions across the continuum of care” [5]. Patient experience is increasingly recognized as an important contributing factor to the quality of care in all healthcare settings [6]. A focus on patient experience is easily justified on the basis of human ethics; however, literature also shows a positive relationship between patient experience and clinical outcomes [7]. For example, positive associations exist between the quality of patient experience and outcomes such as those assessed by objective health measures, self-reported health and well-being, adherence to recommended treatment and use of preventive care, outcomes related to healthcare resource use, and errors or adverse events and measures of the technical quality of care [7]. Additional research found positive changes in areas such as patient satisfaction, clinical outcomes, and improvements at an organizational level after implementing several patient-centered care initiatives [8].
Due to the complex nature of CP, outpatient programs that have an interdisciplinary focus typically lead to significant improvements in multiple clinical outcomes [9–13]. In fact, when compared to standard inpatient rehabilitation, interdisciplinary pain management programs are significantly more effective at improving pain, social functioning, catastrophizing, and ability to decrease disability [10]. It is for reasons like these that Hamilton Health Sciences (HHS) applies this tactic in their Chronic Pain Management Unit (CPMU) at Chedoke Hospital. The CPMU at Chedoke Hospital, Hamilton Health Sciences, Hamilton, Ontario, Canada is an interdisciplinary, multimodal 4-week program with a cognitive-behavioral therapy (CBT) orientation. Most of the activities in the CPMU are designed to teach and enable patients to adopt self-management approaches to their CP problems [14]. The primary focus is on learning self-help techniques and to encourage the use of coping strategies to challenge maladaptive thoughts and behaviors related to pain. One of the main goals of this approach is to enhance patients’ sense of control over their pain by providing them with a set of skills to better manage their physical symptoms. Goal setting, active exercises by quotas, stress management, relaxation, vocational counseling, family intervention are essential components of the CPMU [14, 15]. It should be noted that the CPMU has now been renamed as the Michael G. DeGroote Pain Clinic and has been relocated at McMaster University Medical Center as of June 2015.
In an effort to improve patient experience at HHS, Cunningham et al. [16] surveyed 508 patients at HHS. The patients’ opinions regarding what was most important when receiving care were used to design the model of care for HHS, “Family-Centred Care: Doing What Matters Most”. According to this model, HHS has committed itself to communicating, collaborating, and responding more effectively [16].
In addition to these innovative implementations, it is imperative to continually monitor patient experience to ensure consistent quality of patient experience. A previous study at the CPMU was conducted by Hapidou and Li [17]. Written comments from patients who had completed the 4-week pain management program were analyzed for major themes to understand the patients’ experiences [17]. The following themes were obtained: from limitation to function, focus on the self, taking the initiative, the importance of peer support, impact of team effort, and targeting the psychology.
Since that time, the CPMU has introduced several changes into the program: (a) Interdisciplinary initial assessment (previously, one staff member assessed patients prior to entry into the CPMU), (b) the length of the daily program changed from 9:00AM–4:00PM to 9:30AM–3:30PM, (c) changes in staff composition and the reduction of staff due to institutional budgetary changes and other administrative changes. (d) moving into a different part of the hospital, and (e) change of directors. It is for these reasons that the current study was undertaken at this time: to gain insight into patients’ experiences at the CPMU.
Methods
The study received ethics approval from the Hamilton Integrated Research Ethics Board. The CPMU program is an interdisciplinary pain management program attended by CP patients on the basis of third party referral. The CPMU program is 4 weeks long, with ongoing admission, and runs Monday–Friday. The CPMU staff includes two physicians, a psychologist, a psychometrist, a physiotherapist, a pharmacist, a social worker, and two occupational therapists. The program uses a group-based approach; however, patients establish individual goals. Some activities that take place in the program include relaxation classes, functional activity classes, exercise classes, and group therapy. Patients work with all members of the staff and receive care from a wide range of professionals. Patients were admitted to the 4-week program if they had goals for increased functionality and productivity/readiness for change, if they did not have active psychosis or untreated medical conditions such as hypertension and if they received financial authorization by their referring agency. Reason for admission was learning to manage CP/unlearn maladaptive responses to pain, and becoming more functional in spite of pain. Length of admission was 4 weeks.
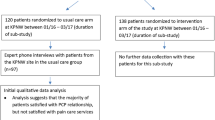
Data were collected retrospectively from 50 randomly selected patients, chosen from the 86 patients admitted to the CPMU between May 13th, 2013 and December 9th, 2014. The rationale for random sampling is that (a) a large number of patients would be used as participants without bias due to time of program attendance and (b) not all patients could be sampled due to time limitations (student project for one term).
Upon admission into the program, all patients provided written consent for their data to be used for research purposes. Data from two exit questionnaires were analyzed. The first was the Self-Evaluation Scale (SES) [18, 19]. On this form, the patient is asked to rate his/her own goal accomplishment on a 5-point Likert scale. This is followed by an open-end section titled “comments” where the patient may elaborate on their perceived goal accomplishment. The second questionnaire from which data were extracted was the Pain Program Satisfaction Questionnaire (PPSQ) [18]. The PPSQ consists of 11 questions regarding satisfaction with the program, each rated on a 4-point Likert scale, and two open-ended sections. The first open-ended section asks patients to list any problems that the program helped with, other than pain. The second open-ended section asks the patient to provide any comments they may have regarding their experience in the program.
Patients with responses to any of the three open-ended questions were included.
Two participants did not have comments on their questionnaires. For this reason, the next patient on the database was used instead. The randomization process was to ensure that this was a complete representation of anyone who participated in the program. All patients who were admitted to the program during the study period completed the 4 weeks.
Written responses were collected, typed into a database verbatim, arranged by patient and questionnaire section, and stratified by gender. The decision to assess themes based on gender was based on the literature of gender differences in pain. CP has been shown to be more common in women than men [20–24]. Gender may play a role in reports of pain and distress following interdisciplinary CP management [25].
To maintain anonymity, patients’ names were replaced with coded numbers. All data were read through comprehensively before any analysis was performed. Conventional content analysis was applied in an inductive manner to rigorously analyze text and extract major themes [26–30]. Codes, which are words or short phrases that summarize the essence of what is being said [30], were written in the margins of the text to which they applied. This process is known as open coding and was performed to develop the codes. Simultaneously, a codebook was created to record all codes [See Appendix A and B (Supplementary Material)] [29, 30]. Once all data were coded, the process was repeated two times using the existing codebook to verify or retract previously assigned codes and to develop and apply new codes where appropriate. Repeating the process several times ensured that all data were properly interpreted [29, 30]. When all data were thoroughly coded, code frequencies within male and female data as well as total code frequencies were calculated (see supplementary material). Codes were then grouped together based on the author’s understanding of a common focus between codes in the category [29]. Once categories were formed, a similar process was used to group categories together to form major themes [26–30].
There was only one coder, the student, E. Horst, alone. She was not part of the clinical team, nor did she know any of the patients. The assumption is that she could provide a completely objective perspective on the comments from a clinically naïve point of view. Her understanding of the program at the time of the study was only theoretical.
Results
Quantitative Results
Fifty patients’ comments were analyzed in this study. There was an equal representation of males and females (24 males, 26 females), reflecting the overall composition of the program patients. Their age ranged from 21 to 79 years with an average (SD) of 43.96 years (12.24) and a median of 46.5. The majority of patients had pain resulting from a motor vehicle accident (56%) followed by a work-related injury (28%), a military-related injury (14%), and pain of insidious onset (2%). Duration of pain was very variable, ranging from 16 to 348 months with an average (SD) of 74.83 (69.99) and a median of 50. At discharge from the 4-week program, patients felt they had accomplished their goals on average at 3.38 out of 5 (0.98) on the SES with a median of 3 (well). Their PPSQ score was an average of 35.96 out of 44 (4.15), with a median of 36. There were no gender differences on the SES (p = 0.54) or the PPSQ (p = 1).
Qualitative Results
The Impact of a Strong Interdisciplinary Team
The most frequently observed theme was the important role the CPMU staff had in the patients’ experience in the program. Almost all patients expressed some form of gratitude to the staff or had positive things to say about them. The patients wrote that the staff demonstrated a good balance of professionalism and compassion. While they understood the physiology of CP, they were also able to connect and empathize with the patient.
-
“Very informative with lots of good support from a team of people who understand our pain”.
-
“With the guidance and professionalism of this genuinely caring team…”
-
“Passionate, caring and dedicated staff make this course”.
Patients also commented on the benefits of learning about their own condition. Many patients entering the program have limited knowledge regarding the physiological mechanisms and psychosocial repercussions of CP. For this reason, many of the patients found it beneficial to simply learn more about CP. The interdisciplinary nature of the CPMU provided patients with a ranging perspective.
-
“It has covered a wide range of topics and each one plays on the other”.
-
“I have learned a lot about chronic pain. It helped me to understand more about it”.
Learning to Adapt in Order to Manage
The CPMU places a large emphasis on learning to manage pain as opposed to curing it. Fortunately, patients were in agreement with this approach. Patients reported learning new coping strategies to employ in order to live a better life with their CP.
-
“I’ve learned […] exercise for stretching and to take breaks […] methods to try and control [my pain]”.
-
“I learned different ways of handling the kitchen area”.
-
“I’ve learned […] to take breaks and pace myself […] I will try and stop just going and going with my daily activities and slow down so my pain won’t get worse”.
In addition, patients wrote that they had made modifications to their daily life and routine to more easily live with their pain. Patients demonstrated an understanding and acceptance that their pain was not likely to be cured and that they must, therefore, find ways to live with the pain, despite the fact that their life was no longer the same as it was before CP began.
-
“I can have a happy life even if it will be different”.
-
“More aware of what I have to do to accomplish a reasonable life”.
-
“Pain will always be a part of you but there’s ways to lower pain levels”.
The Program as a Stepping Stone
While it is important that patients make adaptations to their lives while enrolled in the program, it is perhaps even more important that patients continue these practices once discharged from the CPMU. Fortunately, patients displayed an optimistic outlook and planned to continue applying what they learned in the program.
-
“…Information that I will take with me and continue to practice”.
-
“When I go home, I will continue my exercises and mix it in with my daily life”.
Furthermore, patients expressed an understanding that they still had progress to make. Since the program is only 4 weeks long, patients generally have a long way to go once discharged. Fortunately, the patients understood this and were willing to put in effort to continue improving. In fact, there was often a tone of optimism when discussing future progress.
-
“Still a long way to go but now I see the light that I didn’t before”.
-
“Change does not happen overnight and with time I can implement my new coping skills”.
-
“I am going to keep moving forward with same passion and positive changes”.
The Positive Effects of a Group Effort
People living with CP are often the only one of their peers with the condition. For this reason, people with CP may become isolated as there is a lack of understanding from others. For many patients, coming to the CPMU is the first encounter they have with other CP patients. Not surprisingly, this can be very therapeutic. Patients expressed enjoyment in being able to share their own thoughts and concerns with others, as well as listen to other people’s stories. The feeling of belonging to a group, even if the common factor is a condition like CP, gave the patients a sense of togetherness.
-
“It was very helpful to hear other people’s stories”.
-
“Learned that there is a lot of people like me suffering from chronic pain”.
-
“Best part was knowing people with the same condition and getting to share with them”.
The theme of a group effort also carried over into the patients’ family lives. As they learned more about what was best for their own well-being, patients began to improve communication with family members. They were able to be more assertive regarding their need to pace. Several patients wrote about these improvements and how their families were involved in the process.
-
“Started to improve my family life through better communication”.
-
“[I have learned to] set limits with my family”.
-
“[before,] I never let them see my true pain […] I started telling them ‘ok guys I can’t do this anymore, I need help’”.
Improved Mental Health
CP has far reaching effects on mental health due to the limitations it places on people’s ability to participate fully in daily life. Although the program does not guarantee a reduction in pain, the learned ability to cope can improve mental health status. In the section of the SES where patients are asked to list problems that the program helped with other than pain, patients said the following:
-
“Depression”, “Anxiety”, “Stress”, “Emotional”, “Anger”, “Social”, “Mental health in general”.
Some patients also elaborated on how the program helped them to improve their mental well-being.
-
“I have learned a lot about myself”.
-
“Dealing with negative emotions related to pain”.
-
“The Self-Talk was a big one for me”.
-
“This program has opened my eyes to a more positive way to deal with my pain”.
-
“I do not feel as closed off as I had before”.
Benefits of the Program
As previously stated, the intention of the program is not to cure pain. However, this is not to say that patients do not experience benefits. Due to the interdisciplinary approach, patients reported benefits in a range of areas. Patients commented on improvements that they made in life outside the program as well as components of the program that they found especially helpful.
-
“Felt pain in my muscles that I haven’t in many years, good pain from exercising”.
-
“Sleeping in the bed not on the couch”.
-
“I am eating healthier foods and smaller portions”.
-
“Improved my overall general health”.
-
“Yoga has been very helpful, relaxation as preventative measures”.
-
“Relaxing (Oh my, this is so helpful)”.
Rare but Concerning Comments
Despite the overall program satisfaction being quite high, patients did report some concerns. Although these comments do not appear frequently enough to be considered a main theme, it is still important to report them. Some patients reported difficulty in applying what they had learned. This was brought to attention mostly by those who were staying in hotels for the durations of the program, making it difficult to implement coping strategies.
-
“Hard to implement things when I’m not in my ‘natural environment’”.
Other patients reported difficulty implementing coping strategies because of external factors:
-
“I can upkeep the basics but to add extra things will increase the pain”.
-
“Work limits ability to implement certain aspects”.
Lastly, a small number of patients reported some specific concerns:
-
“Too much paperwork for my liking”.
-
“The classes were a bit too long because my pain increases when I sit for long”.
Gender Differences
No statistically significant differences were found between males and females on the PPSQ or the SES scores. However, some differences did arise in written comments. Females, more often than males, reported an acceptance of limitation and the need to ask for help. Females were more comfortable admitting need for assistance from family or friends. Additionally, females reported an increased understanding of the need to pace their daily activities as opposed to fighting through the pain and subsequently worsening it. The following quotations are from female data:
-
“Ask for help, it’s okay if you cannot do something, it doesn’t mean you’re worthless”.
-
“That’s another thing you have helped me with is asking for HELP […] I was always the one who did for everyone. Hard to sit back and ask for help but I am doing it”.
-
“I learned to take time for me […] I need to pace myself and try relaxation”.
Discussion
Patients’ written comments on exit questionnaires demonstrate the importance of the interdisciplinary team as well as the group-based approach. Comments also indicate that patients take on the initiative of adapting their lives to manage pain and are willing to continue practicing learned coping strategies to maintain positive outcomes. As well, comments reflect the numerous benefits of the CPMU program regarding patients’ physical and mental well-being.
The most frequently observed theme was the important role of the CPMU staff in the patients’ experience of the program. Almost all patients expressed some form of gratitude to the staff or had positive things to say about them. According to Gatchel et al. [11], “the key ingredients for interdisciplinary care are a common philosophy of rehabilitation, constant daily communication among on-site health care professionals, and active patient involvement” (p. 121). The patients must have been able to perceive this cohesiveness and true integration of the team and thus made the comments they made so frequently.
More generally, patients’ comments reveal thoughts and feelings regarding their experiences in the CPMU. While quantitative data such as PPSQ and SES scores can provide limited insight regarding overall program satisfaction and self-evaluation, qualitative written text offers a more robust account of both program and self-satisfaction. Quantitative research often provides answers to questions about “when”, “how many” or “how much” and is, therefore, not helpful when asking questions about “how” or “what”. In the case of the current study, questions such as how patients experience the CPMU and what benefits they gain from it are best answered using qualitative methods [30].
Comparisons to Previous CPMU Research
Results are generally consistent with those of previous research conducted at the CPMU. Hapidou and Li [17], using a similar approach, found comparable themes in patients’ written comments. Six main themes were extracted: from limitation to function, focus on the self, taking the initiative, the importance of peer support, impact of team effort, and targeting the psychology. Several of these themes overlap with the current findings. For example, the importance of peer support and the impact of team effort remained salient themes in patients’ comments. The current study found that the important role of the interdisciplinary staff as well as the therapeutic effects of group therapy were important themes in patients’ comments. As well, the theme of targeting the psychology remains present in patients’ comments and was replicated in the current study as improved mental health. Last, the current study found the themes adapting to manage and the program as a stepping stone, implying that patients expressed an intention to continue applying what they had learned at the CPMU. This is quite similar to the previous authors’ finding of patients taking the initiative [17]. The theme of limitation to function was not replicated in the current study. However, it is important to note that within the current theme, benefits of the program, several patients wrote about improved fitness, function, sleep, and overall health, benefits which imply a transformation toward better functioning.
Implications of Themes
The results of the current study further strengthen the evidence for an interdisciplinary approach to CP management, which is supported by the current literature [9–13]. Patients’ appreciation of staff may speak to their being recognized and validated for their difficulties as well as for their efforts to mitigate the deleterious effects of CP on their lives. Regardless of the positive outcomes associated with interdisciplinary methodologies, it has also been found that little or even no professional input is helpful for CP patients to achieve improvements [31]. In the presence of peer support from others who have CP and without any professional consultation, CP patients have reported improvements in functional ability, and decreased use of healthcare [31]. However, it is not known how complex these patients’ conditions are and how similar they are to those who are referred to interdisciplinary programs. Therefore, caution needs to be applied in drawing conclusions about patients in an interdisciplinary program. Nevertheless, patients in the current study reported benefits from simply being around others with CP. Due to the fear of experiencing further pain, people living with CP often withdraw from family and social interactions, becoming severely isolated [32]. As well, limited understanding from friends and family can cause frustration and further promote social isolation [33]. The ability to share concerns, thoughts and emotions with others who are also living with CP can be both informative and therapeutic [31]. According to the patients’ comments, the experience of being met with a validating attitude by other patients and staff was of great importance. They felt listened to, understood, confirmed, accepted, and tolerated by other group members as well as staff. It is expected that this might increase their ability to understand and deal with other aspects of their lives as well. We are not aware of research findings that support groups alone bring about changes in terms of developing tools and strategies to handle pain and strengthen patients’ individual resources. The golden standard of CP management seems to be interdisciplinary treatment [10–13].
Additionally, patients frequently reported having made adjustments and modifications to their daily life by incorporating learned coping mechanisms. Said adjustments made living with CP easier, despite the disruptions made to daily routines. The patients’ acceptance that they must adapt their lives to be able to live with CP is a reflection of the effectiveness of the CPMU staff to convey the messages of management over cure. As well, this finding is especially important because it has been shown that acceptance of CP is negatively associated with frequency in reports of pain, pain-related anxiety and avoidance, depression and disability, and positively associated with work status [34]. Therefore, CP patients who learn to accept their pain and actively cope with it are more likely to derive benefits from programs like the CPMU [34].
Because the program is only 4 weeks long, making adaptations to daily life is necessary but not sufficient for a patient to achieve long-term benefits. As previously mentioned, the CPMU places emphasis on managing pain, not curing it, implying that CP is something these patients will likely live with for the rest of their lives. This means that for the CPMU program to be truly successful patients must take on initiative and maintain self-management of their condition. The transition toward self-management that occurs upon discharge from the CPMU requires increasing autonomy for the patients [35]. Tasks such as problem identification and goal setting, which were previously facilitated and/or led by professionals, become the responsibility of the patient [35]. Fortunately, at the CPMU, patients show willingness to take responsibility for their own pain management and optimism regarding future progress. It should be mentioned here that previous studies in our program over the years found sustainability of quantitative outcomes 6 weeks following discharge [14].
The strong, positive correlation between mental and physical health symptoms is well documented [36–39]. This correlation is strongest when disease state becomes chronic and is found most frequently in association with pain conditions [36]. Due to the enduring nature of CP and its strong association with mental health problems, the CPMU focusses on improving the psychological and emotional health of patients, regardless of a reduction in pain levels [14, 15]. Patients’ comments reflect success of this intention in that they report an improvement in many areas of mental health.
Analyzing code frequencies, it was found that females, more often than males, are willing to admit physical limitation and, therefore, ask for help. Females often wrote about an acquired acceptance that they must ask family and friends for help instead of trying to be unreasonably independent. This may be the result of females having higher pain sensitivity [40]; however, it is more likely due to social factors influencing patients’ decisions to express a need for help. These findings are consistent with previous research, which shows that males are typically less likely to engage in help-seeking behaviors due to their gender socialization [41].
Limitations
It is important to note that, while both the PPSQ and SES are well validated self-report tools [18, 19], there may be bias within patients’ written responses to open-ended questions. The open-ended questions are situated within and/or after several Likert scale items which may have influenced patients’ thoughts and ideas when responding to open-ended questions. As well, because the authors were not blind to the results of previous qualitative studies at the CPMU, this may have introduced bias. Despite thorough effort to maintain scientific rigor by employing supported methods of qualitative content analysis [26–29], the current findings are limited in that they represent the interpretations of one individual as there was only one coder (E. Horst), the student researcher. As stated above, she was not part of the clinical team, nor did she know any of the patients, and the assumption is that she could provide a completely objective perspective on the comments from a naïve point of view. Her understanding of the program at the time of the study was only theoretical. However, we are aware of previous qualitative studies in which a single author codes all data and co-authors corroborate findings [42, 43]. We do recognize the fact of the single coder in this study as a limitation and do point it out.
However, the findings of this study are replicable in that they are consistent with the results of previous studies at the CPMU [17].
Conclusion
Despite inherent limitations, the results of this study contribute to the existing literature regarding both patient experience and CP management. The qualitative nature of the research provides insight that may be overlooked when using quantitative measures [30]. These results may be used by clinicians at the CPMU to improve the quality of care and the patient experience. Results may also be used to promote the CPMU to stakeholders such as referral sources (family physicians, insurance companies, lawyers, etc.). Last, results may be used for the development of future programs that have similar goals of chronic disease management.
References
Mersek HE. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. Pain. 1986;(Suppl 3):S1–S225.
Schopflocher D, Taenzer P, Jovey R. The prevalence of chronic pain in Canada. Pain Res Manag. 2011;16(6):445–50.
Blyth FM, March LM, Brnabic AJ, Cousins MJ. (2004). Chronic pain and frequent use of health care. Pain. 2004; 111(1):51–8.
Rutledge N. The 411 on HCAHPS. J Nurs Manag. 2008;39(8):29–32.
Wolf JA, Niederhauser V, Marshburn D, LeVela L. Defining patient experience. Patient Exp J. 2014;1(1):7–19.
Bloom BS. Crossing the quality chasm: a new health system for the 21st century. JAMA. 2004;287(5):646–7.
Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. Brit Med J. 2013. doi:10.1136/bmjopen-2012-001570.
Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. 2012. doi:10.1177/1077558712465774.
Singh G, Willen SN, Boswell MV, Janata JW, Chelimsky TC. The value of interdisciplinary pain management in complex regional pain syndrome type I: a prospective outcome study. Pain Physician. 2004;7(2):203–10.
Angst F, Verra ML, Lehmann S, Brioschi R, Aeschlimann A. Clinical effectiveness of an interdisciplinary pain management programme compared with standard inpatient rehabilitation in chronic pain: a naturalistic, prospective controlled cohort study. J Rehabil Med. 2009;41(7):569–75.
Gatchel RJ, McGeary DD, McGeary CA, Lippe B. Interdisciplinary chronic pain management: past, present, and future. Am Psychol. 2014;69(2):119.
Artner J, Kurz S, Cakir B, Reichel H, Lattig F. Intensive interdisciplinary outpatient pain management program for chronic back pain: a pilot study. J pain res. 2012;5:209.
Noe C, Williams CF. The benefits of interdisciplinary pain management. Chronic Pain Perspect. 2012;61(4):12–6.
Hapidou EG, Safdar S, MacKay KD. Evaluation of an Inpatient chronic pain management program. Poster abstract # 54. Pain Res Manag. 1997;2(1):63.
Williams R, Hapidou EG, Cullen KL. Self-efficacy and resumption of activities of daily living scales in chronic pain. Physiother Can. 2003;55(2):87–95 (Winner of the Silver Quill Award, 2003).
Cunningham CE, Deal K, Rimas H, Campbell H, Russell A, Henderson J, Melnick B. Using conjoint analysis to model the preferences of different patient segments for attributes of patient-centered care. Patient Patient Centered Outcomes Res. 2008;1(4):317–30.
Hapidou EG, Li K. Confronting the challenges of chronic pain: patient experiences in an interdisciplinary pain management program. Poster presented at the 28th Annual Conference of the Canadian Pain Society, Victoria, British Columbia, May 27–30, 2008.
Hapidou EG. Program evaluation of pain management programs. Paper presented at the 9th Inter-Urban Conference, Kitchener, Ontario, October 30, 1994.
Hapidou EG, O’Brien MA, Pierrynowski MR, de las Heras E, Patel M, Patla T. Fear and avoidance of movement in people with chronic pain: psychometric properties of the 11-Item Tampa Scale for Kinesiophobia (TSK-11). Physiother Can. 2012;64(3):235–41.
Berkely KJ, Holdcroft A. Sex and gender differences in pain. In: Wall P, Melzack R, editors. Textbook of pain. 4th ed. London: Churchill Livingstone; 1999. p. 951–65.
Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287.
Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. J Pain. 2010;11(11):1230–9.
Tsang A, Von Korff M, Lee S, Alonso J, Karam E, Angermeyer MC, et al. Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain. 2008;9(10):883–91.
Verhaak PF, Kerssens JJ, Dekker J, Sorbi MJ, Bensing JM. Prevalence of chronic benign pain disorder among adults: a review of the literature. Pain. 1998;77(3):231–9.
Keogh E, McCracken LM, Eccleston C. Do men and women differ in their response to interdisciplinary chronic pain management? Pain. 2005;114:37–46.
Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15.
Saldaña J. The coding manual for qualitative researchers. London: Sage; 2012.
MacQueen KM, McLellan E, Kay K, Milstein B. Codebook development for team-based qualitative analysis. Cult Anthropol. 1998;10(2):31–6.
Neergaard MA, Olesen F, Andersen RS, Sondergaard J. Qualitative description—the poor cousin of health research. BMC Med Res Methodol. 2009;. doi:10.1186/1471-2288-9-52.
Subramaniam V, Stewart MS, Smith JF. Development and Impact of a Chronic Pain Support Group: a qualitative and quantitative study. J Pain Symptom Manag. 1999;17(5):376–83.
Falvo D. Medical and psychosocial aspects of chronic illness and disability. Burlington: Jones & Bartlett Publishers; 2013.
Kleinman A. The illness narratives: suffering, healing and the human condition. USA: Basic Books; 1988.
McCracken LM, Carson JW, Eccleston C, Keefe FJ. Acceptance and change in the context of chronic pain. Pain. 2004;109(1):4–7.
Richardson J, Loyola-Sanchez A, Sinclair S, Harris J, Letts L, MacIntyre NJ, Ginis KM. Self-management interventions for chronic disease: a systematic scoping review. Clin Rehabil. 2014;28(11):1067–77.
Gatchel RJ. Comorbidity of chronic pain and mental health disorders: the biopsychosocial perspective. Am Psychol. 2004;59(8):795.
Demyttenaere K, Bruffaerts R, Lee S, Posada-Villa J, Kovess V, Angermeyer MC, Levinson D, de Girolamo G, Nakane H, Mneimneh Z, Lara C, de Graaf R, Scott KM, Gureje O, Stein DJ, Haro JM, Bromet EJ, Kessler RC, Alonso J, Von Korff M. Mental disorders among persons with chronic back or neck pain: results from the World Mental Health Surveys. Pain. 2007;129(3):332–42.
Blyth FM, March LM, Brnabic AJ, Jorm LR, Williamson M, Cousins MJ. (2001). Chronic pain in Australia: a prevalence study. Pain. 2001;89(2):127–34.
Gilmour H. Chronic pain, activity restriction and flourishing mental health. Health Rep. 2015;26(1):15–22.
Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Brit J Anaesth. 2013;111(1):52–8.
Addis ME, Mahalik JR. Men, masculinity, and the contexts of help seeking. Am Psychol. 2003;58(1):5.
Darlow, B., Dowell A., Baxter, G., Mathieson, F., Perry, M. Dean S. The enduring impact of what clinicians say to people with low back pain. Ann Fam Med. 2013;11(6):527–34 (online first).
Snelgrove S, Edwards S, Liossi CA. A longitudinal study of patients’ experiences of chronic low back pain using interpretative phenomenological analysis: changes and consistencies. Psychol Health. 2013;28(2):121–138 (online first).
Acknowledgments
No funding or sponsorship was received for this study or publication of this article. This was conducted as an independent study project for the term of January to April 2015. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
E. G. Hapidou and E. Horst have nothing to disclose.
Compliance with Ethics Guidelines
The study received ethics approval from the Hamilton Integrated Research Ethics Board. All patients provided written consent for their data to be used for research purposes.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hapidou, E.G., Horst, E. Learning to Manage Chronic Pain: The Patients’ Perspective. Pain Ther 5, 93–105 (2016). https://doi.org/10.1007/s40122-016-0047-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-016-0047-0