Abstract
Introduction
We recently reported that a majority of opioid-dependent Malay males on methadone therapy are cold pain sensitive. It is postulated that common OPRM1 polymorphisms may be responsible. This study investigated the association between 118A>G (dbSNP rs1799971) and IVS2+691G>C (dbSNP rs2075572) variants on cold pain responses among opioid-dependent Malay males on methadone maintenance therapy.
Methods
Cold pain responses including pain threshold, pain tolerance, and pain intensity were measured using the cold pressor test. DNA was extracted from the venous blood before polymerase chain reaction genotyping. Repeated measures analysis of variance was used to compare the cold pain responses and OPRM1 polymorphisms (118A>G and IVS2+691G>C) using models including genotype dominant and recessive models, allelic additive models, and analysis of haplotypes and diplotypes.
Results
A total of 148 participants were recruited. With the recessive model, those with IVS2+691 homozygous CC genotype had a shorter cold pain tolerance time than those without CC genotype (i.e., GG/GC genotype; 29.81 vs. 43.08 s, respectively, P = 0.048). On the other hand, with diplotype analysis, participants with combined homozygous 118 AA genotype and heterozygous IVS2+691 GC genotype (i.e., AC/AG diplotype) had a longer cold pain tolerance time than those without this diplotype (49.34 vs. 31.48 s, respectively, P = 0.043). Cold pain threshold was not associated with any of the 118A>G and IVS2+691G>C variations despite being analyzed using various models (all P > 0.05).
Conclusion
The IVS2+691 CC genotype and AC/AG diplotype of 118A>G and IVS2+691G>C seem to have opposing roles in pain tolerance among opioid-dependent Malay males on methadone therapy. Haplotypes of OPRM1 may be associated with altered binding affinity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The opioidergic neurotransmission system is an important processor of painful stimuli [1–4]. The μ-opioid receptor (OPRM1) is a primary target for clinically important opioid analgesics, including methadone. Studies among healthy subjects showed a possible role of the opioid receptor mu 1 gene (OPRM1) in altered pain sensitivity [5, 6]. Genetic factors that affect the density, function, and, consequently, the signaling efficacy of μ-opioid receptors may contribute to inter-individual variations in the pain response to opioids [7–9].
Southeast Asia is a highly populated and cultural-diverse region with ethnic Malays constituting the largest population group, mainly populating countries including Malaysia, Indonesia, and the southern part of the Philippines. Males who are ethnic Malays make up the majority of opioid-dependent patients on methadone treatment in Malaysia [10]. We have previously reported that a majority of opioid-dependent Malay males on methadone therapy are cold pain sensitive and that the pain is frequently associated with poor sleep quality [11]. One postulated mechanism for altered pain sensitivity in this susceptible population is polymorphisms in the OPRM1 gene.
Some of the most frequently studied polymorphisms of OPRM1 include 118A>G (dbSNP rs1799971), IVS2+691G>C (dbSNP rs2075572), and IVS2+31G>A (dbSNP rs9479757). The association between 118A>G polymorphism and pressure pain was first reported by Fillingim et al. [6] and Lotsch et al. [5], but subsequent studies failed to replicate these preliminary reports in different experimental pain models and in different populations [12–14]. Similarly, the roles of other polymorphisms on pain sensitivity, including IVS2+691G>C and IVS2+31G>A, have been mixed. For example, the IVS2+691G>C polymorphism did not increase morphine requirements in patients with pain caused by malignant disease [7] and did not have significant association with 24-h post-operative opioid requirement [15]. To summarize, available studies have raised a great deal of speculation over the role of OPRM1 polymorphisms in pain sensitivity and one postulation is that this phenomenon may be gender and ethnic dependent [16].
Recent studies indicate OPRM1 polymorphisms are associated with side effects including changes in libido and insomnia [17], and also methadone-related deaths [18, 19]. On the other hand, the role of OPRM1 polymorphisms on pain sensitivity among opioid-dependent patients on methadone is unclear because of limited evidence. Thus far, only one study has explored this [20] but unfortunately the low frequencies of variants in the study samples were a limitation. A better understanding of OPRM1 polymorphisms in pain and opioid response of a specific population has implications for the treatment of pain and addictive disease, and clinical management of each in the presence of the other. In the present study, we aimed to investigate the influence of common OPRM1 polymorphisms on pain responses among opioid-dependent Malay males on methadone maintenance therapy (MMT).
Methods
Participants
Characteristics of the sampling population have been previously described [11]. Briefly, study participants were opioid-dependent males undergoing methadone treatment at Hospital Universiti Sains Malaysia (USM) and other MMT clinics (Kota Bharu, Pasir Mas, Pasir Puteh, and Bachok) in the state of Kelantan, Malaysia. Opioid dependency was defined according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) criteria [21]. They were sequentially recruited after informed consent. Study participants were included if they were: (a) in the national MMT program with a duration of participation of more than 1 month; (b) more than 18 years of age; (c) free of regular use of alcohol; (d) free of intoxication; (e) able to understand study protocols and to follow simple study instructions; and (f) willing to sign written informed consent. Exclusion criteria included the following: (a) presence of acute medical, surgical, or psychiatric illnesses; (b) current intake of benzodiazepines, cannabinoids, and barbiturates; (c) on regular anticonvulsants, neuroleptics, or analgesics; (d) history of chronic or ongoing acute pain; (e) history of analgesics ingestion within 3 days before the cold pressor test (CPT); and (f) presence of severe cognitive impairment which might interfere with pain assessments and/or communication. Psychiatric illnesses were carefully evaluated during interview of participants, and the information verified with their medical records and also from their treating doctors. Participants also had to have two consecutive negative urine tests for morphine, tetrahydrocannabinol, amphetamines, and benzodiazepines before study inclusion.
This study was approved by the Human Research Ethics Committee (HREC), Universiti Sains Malaysia (USM) in Kelantan, Malaysia (Reference number: USMKK/PPP/JEPeM (253.3 (14))) and the Medical Research and Ethics Committee (MREC) at the Ministry of Health (MOH), Malaysia (Reference number: NMRR-13-524-16614).
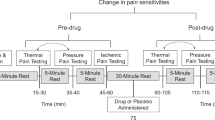
Assessment of Cold Pain Threshold, Pain Tolerance, and Pain Intensity Using the Cold Pressor Test
The CPT method utilized in the current study has been previously described [11]. Briefly, a 48-quart cool box was filled with a mixture of two-thirds crushed ice and one-third tap water. A constant temperature of 0–2 °C was maintained by adding ice intermittently. The non-dominant hand and forearm of participant would be placed in the ice bath with their palm flat at the bottom of the box, with ice water covering the hand and approximately 10 cm of the forearm. The test was truncated at 300 s because the numbness associated with cold would reduce the pain.
Pain threshold was defined as the first experience of pain that can be identified, pain tolerance as the time elapsed when the participant had to withdraw his hand (i.e., the most severe pain that a subject was willing to tolerate), and pain intensity as the maximal pain experienced during test on a visual analog scale (VAS; 0–100). We examined the cold pressor responses six times over a 24-h period [i.e., at 0 h (at about 8.00 am), and at 2, 4, 8, 12, and 24 h after the first test] to reduce the diurnal variation in the cold pressor pain response. The cold pressor pain measurements at these six different time points were used for subsequent data analysis.
PCR Genotyping for OPRM1 Polymorphisms
Venous blood samples (2.5 mL) were collected in tubes containing sodium citrate and were stored at −20 °C until further processing. Genomic DNA was extracted from the unclotted blood using QIAamp® DNA blood mini kit (Qiagen Gmbh, Hilden, Germany) according to the manufacturer’s instructions. The quantity and quality of the extracted genomic DNA was determined on the NanoDrop® ND-1000 spectrophotometer (NanoDrop Technologies, Inc. Wilmington, DE, USA) with measurements performed at 260 and 280 nm. A two-step polymerase chain reaction (PCR) method for simultaneous OPRM1 and CYP2B6 genotyping was developed and validated for reproducibility and specificity through direct sequencing [22]. All PCRs were performed in standard 0.2-mL Eppendorf PCR tubes and carried out in a volume of 25 μL comprising buffer [10 mM Tris–HCl (pH 8.0), 50 mM KCl, 1 mM EDTA, 0.1% Triton X-100, 50.0% glycerol (v/v)]. The reactions were performed on the Applied Biosystems® Veriti® 96-well thermal cycler (Applied Biosystems, Carlsbad, CA, USA).
Briefly, the first-step PCR (‘Set A’) was performed using specifically designed primers (see Table S1 in the supplementary material) to isolate regions of interest that contain the relevant OPRM1 polymorphisms (118A>G and IVS2+691G>C). These were later used for the second allele-specific PCR to avoid amplifications of similar sequences in the human genome that may be located outside the gene. PCR mixture for Set A contained 1.0 U of Biotool® DNA Taq polymerase (Biotools Biotechnological and Medical Laboratories, SA, Madrid, Spain), 2.0 mM MgCl2, 0.2 mM dNTPs (Biotools Biotechnological and Medical Laboratories SA), and 0.10–0.25 µM of the primers (Invitrogen, Waltham, MA, USA). The cycling conditions were optimized for Set A. Ten microlitres of the first PCR products of Set A was analyzed using 2.0% agarose gel (Promega Corporation, Madison, WI, USA) and 1 × TBE (Tris, Borate, EDTA) at 100 V for 60 min. Two microlitres of the diluted first-step PCR products of Set A was used as template for detection of wild-type or mutant-type alleles in the next-step PCR. Two secondary PCRs (Set 1 and 2) were then carried out using identical reaction mixtures described for the first-step PCR, with the exceptions of primer concentrations shown in Table S1 in the supplementary material. The cycling conditions were again optimized and 10 μl of the second PCR products were again analyzed using 2.0% agarose gel and 1 × TBE at 100 V for 60 min.
Statistical Analysis
Genotyping data were analyzed using the population genetic data analytical program, Golden Helix SNP and Variation Suite 7 (SVS 7, version 7.3.1; Golden Helix Inc., Bozeman, MT, USA) based on an expectation–maximization (EM) algorithm for the following procedures: (a) the calculation of OPRM1 alleles and genotype frequencies; (b) the estimation of heterozygosity in each polymorphism in Hardy–Weinberg proportion; and (c) the estimation of maximum-likelihood haplotype frequency. Repeated measures analysis of variance (RM-ANOVA) was used to compare mean differences of cold pain responses between OPRM1 polymorphisms (118A>G and IVS2+691G>C) according to their genotypes and allelic additive models, genotype dominant and recessive models, haplotypes and also diplotypes (frequency less than 10.0% were pooled). Statistical analysis was performed using SPSS/Win software (version 22; SPSS, Inc., Chicago, IL, USA). There was no correction for multiple testing since only one gene was tested [23]. All confidence intervals (CIs) were computed at the 95% level. A P value <0.05 was considered significant.
Results
Characteristics of Study Participants
From March to October 2013, 169 patients were screened: 148 completed the study and 21 failed the screening. Twelve patients were excluded for health reasons, 3 for scheduling conflicts, and 6 for miscellaneous reasons. The mean age of the study participants was 36.86 [standard deviation (SD) 6.13, range 25–55] years. The majority of the participants used more than one illicit drug in their lifetime with marijuana and amphetamines being the most widely used. Ten (6.8%) participants reported morphine and related substances as their past illicit drug use. The mean duration in the MMT program was 2.82 (SD 2.02, range 0.33–9.00) years. The mean daily methadone dose was 72.70 (SD 28.25, range 20–160) mg/day. There was no correlation between daily methadone dose and duration in the MMT program (r = 0.06, P = 0.485).
Genotyping Frequencies of OPRM1 Polymorphisms
The 118A/G and IVS2+691G/C alleles of the OPRM1 gene were successfully amplified from 148 subjects. Their genotype and allele frequencies are shown in Table S2 in the supplementary material. One participant carried the homozygous wild-type (IVS2+691 GG) genotype of the IVS2+691G>C polymorphism. The distributions of genotypes for the above polymorphisms followed the Hardy–Weinberg equilibrium (P > 0.078). Assuming a mutant allele was a high-risk allele, genotype frequencies under dominant and recessive model were determined for these polymorphisms (see Table S2 in the supplementary material). The most likely haplotype pair (i.e., diplotype) for each genotype in each individual was estimated and the haplotype frequency distributions were obtained with an expectation-maximum (EM) algorithm haplotypes. Their estimated haplotype and diplotype frequencies are as shown in Table S3 in the supplementary material. On the basis of the genotyping data of subjects included in the study, the standardized linkage disequilibrium value (Levontin’s D′) and correlation coefficient (r 2) between 118A>G and IVS2+691G>C polymorphisms were 0.473 and 0.031, respectively [x 2 (df) = 9.176 (1), P = 0.0026].
Association Between Cold Pain Parameters and Polymorphisms of OPRM1
Cold pain threshold was not associated with any of the 118A>G and IVS2+691G>C variations despite being analyzed using various models including dominant and recessive models, allelic additive models, as well as haplotype and diplotypes analyses (all P > 0.05; Table 1). Likewise, none of 118A>G and IVS2+691G>C variations were associated with cold pain intensity despite various models (all P > 0.05; Table 2). Table 3 shows the relationship between variants of 118A>G and IVS2+691G>C with cold pain tolerance time. With the recessive model, those with IVS2+691 homozygous CC genotype had a shorter cold pain tolerance time than those without CC genotype (GG/GC genotype; 29.81 s vs. 43.08 s, respectively, P = 0.048). Variations in the 118A>G polymorphism were not associated with cold pain tolerance time (all P > 0.05; Table 3). However, with diplotype analysis, participants with combined homozygous 118 AA genotype and heterozygous IVS2+691 GC genotype (AC/AG diplotype) had a longer cold pain tolerance time than those without this diplotype (49.34 s vs. 31.48 s, respectively, P = 0.043).
Discussion
The 118G allele frequency of 40.2% in our study is in good agreement with previous smaller scale studies of this polymorphism among Malay drug addicts in Malaysia [24] and heroin-dependent Malays in Singapore [25], although ours was much higher compared to intravenous drug users on MMT [26]. Likewise, frequency of variant IVS2+691C allele of 83.1% in our subjects is similar to those reports from heroin-dependent Malays in Singapore [25]. The reported frequency in our study seems to have contrasted with those of the Chinese (73.1%) and Indian (75%) Singaporeans [25], as well as the Chinese (69.3%) in Hong Kong [27]. The above reports indicate that variability in frequency of 118G and IVS2+691C allele in populations on methadone treatment may be an ethnic-dependent phenomena.
In the current study, there was no association seen between 118A>G variations with cold pain threshold and pain tolerance. Instead, IVS2+691G>C polymorphisms using different models were shown to affect cold pain tolerance, but not pain threshold and pain intensity. These include homozygous CC genotype (a significant shorter pain tolerance time in CC vs. GG/GC) and combined homozygous 118 AA genotype and heterozygous IVS2+691 GC genotype (AC/AG diplotype; a significant longer pain tolerance time with this diplotype vs. without this diplotype). We have previously reported that a majority of opioid-dependent Malay males on methadone therapy are cold pain sensitive [11] and OPRM1 polymorphisms might be responsible for this altered sensitivity based upon our study results. What are the implications of this? Any inter-individual variations in opioid-induced hyperalgesia among methadone users may weaken or strengthen their determination to abstain [28], and the knowledge of OPRM1 polymorphisms in such a circumstance may help to provide a prediction. In addition, this knowledge on OPRM1 polymorphisms may help to guide the methadone dosages and, therefore, avoid adverse drug reactions.
Studies by Wang et al. [17] indicated that IVS2+691G>C polymorphisms might affect the side effects of methadone including change in libido and insomnia. Our study suggests that variations in IVS2+691G>C might also affect pain tolerance. The actual functions of IVS2+691G>C are still under investigations but available data support its role in affinity of transcriptional regulatory factors for the intronic DNA sequence [29–31]. The DNA intronic sequence could involve in alternative DNA splicing and this results in creations of different isoforms of human OPRM1 gene [30, 32]. It may also directly alter mRNA levels and, therefore, affect expression of OPRM1 gene [29–31]. Based on our results, we hypothesized the increased expression of IVS2+691 CC variant resulted in a higher OPRM1 availability and because of chronic sensitization by prolonged opioid use, it may then facilitate opioid tolerance, hyperalgesia and subsequently lower the pain tolerance. However, tolerance normally indicates a rightward shift in a dose–response curve. Since participants have been treated with methadone anywhere from 0.3 to 9 years, sensitization may, therefore, also be quite variable or absent. It is possible that those participants in the program with a shorter stay were different than those with longer treatment times.
On the other hand, the AC/AG diplotype of 118 and IVS2+691 was associated with a longer cold pain tolerance time. Opioid-related adverse effects such as hyperalgesia were probably less likely to occur in patients with AC/AG diplotype at 118 and IVS2+691 given that the mechanisms of opioid-induced adverse events involve OPRM1. Thus, although 118A>G polymorphism alone does not influence cold pain tolerance, the 118 variant may play an indirect role in pain modulation. A strong linkage disequilibrium (LD) between studied polymorphisms and unstudied polymorphisms has been shown to exist [15, 33], and resulted in altered binding affinity between endogenous (and/or exogenous) opioids and OPRM1. As a consequence, there was less hyperalgesia and, therefore, an increase in cold pain tolerance.
There were associations, although not significant, where variants of 118G allele and GC haplotype of 118 and IVS2+691 caused a higher cold pain intensity, but 118 AA genotype resulted in a lower cold pain intensity. At this juncture, it is difficult to explain the differential effects on pain intensity with these polymorphisms and further studies with larger samples are needed. Besides individual polymorphisms, haplotype and diplotype analyses are also necessary to clarify the influence of OPRM1 on inter-individual variations in pain sensitivity among opioid-dependent patients on methadone therapy. There is also the possibility that heightened pain sensitivity is a result of the prolonged opioid use itself or opioid-induced hyperalgesia. The heightened pain sensitivity is a form of latent hyperalgesia to chronic opioid misuse, and subsequent methadone therapy does not exacerbate hyperalgesia but does not make it worse either [34, 35].
Some limitations to this study need to be highlighted. There are a number of OPRM1 polymorphisms (such as rs1074287, rs6912029, rs12209447, rs510769, rs3798676, rs7748401, rs495491, rs10457090, rs589046, rs3778152, and rs563649) but we only studied two common variants. Only Malay males were included but we aimed to reduce the confounding effects of gender and ethnicity on cold pain response [36–44]. Furthermore, Malay males are the majority of opioid-dependent patients on methadone treatment in Malaysia. There were other confounding factors such as induction of tolerance to methadone effects, methadone clearance and genetic variations of other pain-related genes and genes related to pharmacokinetics and pharmacodynamics of methadone, which may be important. Only a tonic pain model using cold pain was studied here and phasic pain may differ qualitatively, neurologically, and functionally from tonic pain stimuli [45]. However, CPT has been shown to be the better pain-induction technique for methadone studies [20, 46, 47]. Lastly, our analyses did not correct for multiple testing because of single gene being studied. There was a significant LD between loci and it was 47.3% of the theoretical maximum but there was a weak correlation between single nucleotide polymorphisms [D′ = 0.473, r 2 = 0.031, x 2 (df) = 9.176 (1), P = 0.0026]. In the view that correction was not performed for multiple tests, these two findings would be considered nominally significant. It is possible that our result might be a false-positive association partly because of limitation in sample size. Therefore, our study may be considered explorative in nature and it would require replication by other investigators. Nevertheless, our results can be considered as a basis for further larger scale study.
Conclusions
In summary, our study indicates that the IVS2+691 CC genotype was associated with a shorter cold pain tolerance time but AC/AG diplotype of 118A>G and IVS2+691G>C was associated with a longer cold pain tolerance time in opioid-dependent Malay males on methadone therapy. It can be postulated that haplotypes of OPRM1 may be associated with altered binding affinity. The OPRM1 polymorphisms may serve as an important variable for developing directed interventions and to guide management of pain among opioid-dependent patients on MMT with genetic risk for suffering pain. Personalized medicine based on pharmacogenetics may be able to maximize the benefits of methadone pharmacotherapy and minimize their harms.
References
Sprenger T, Valet M, Boecker H, Henriksen G, Spilker ME, Willoch F, et al. Opioidergic activation in the medial pain system after heat pain. Pain. 2006;122(1–2):63–7.
Eippert F, Bingel U, Schoell ED, Yacubian J, Klinger R, Lorenz J, et al. Activation of the opioidergic descending pain control system underlies placebo analgesia. Neuron. 2009;63(4):533–43.
Schoell ED, Bingel U, Eippert F, Yacubian J, Christiansen K, Andresen H, et al. The effect of opioid receptor blockade on the neural processing of thermal stimuli. PLoS One. 2010;5(8):e12344.
Holden JE, Jeong Y, Forrest JM. The endogenous opioid system and clinical pain management. AACN Clin Issues. 2005;16(3):291–301.
Lotsch J, Stuck B, Hummel T. The human mu-opioid receptor gene polymorphism 118A>G decreases cortical activation in response to specific nociceptive stimulation. Behav Neurosci. 2006;120(6):1218–24.
Fillingim RB, Kaplan L, Staud R, Ness TJ, Glover TL, Campbell CM, et al. The A118G single nucleotide polymorphism of the mu-opioid receptor gene (OPRM1) is associated with pressure pain sensitivity in humans. J Pain. 2005;6(3):159–67.
Klepstad P, Rakvag TT, Kaasa S, Holthe M, Dale O, Borchgrevink PC, et al. The 118 A>G polymorphism in the human mu-opioid receptor gene may increase morphine requirements in patients with pain caused by malignant disease. Acta Anaesthesiol Scand. 2004;48(10):1232–9.
Befort K, Filliol D, Decaillot FM, Gaveriaux-Ruff C, Hoehe MR, Kieffer BL. A single nucleotide polymorphic mutation in the human mu-opioid receptor severely impairs receptor signaling. J Biol Chem. 2001;276(5):3130–7.
Ravindranathan A, Joslyn G, Robertson M, Schuckit MA, Whistler JL, White RL. Functional characterization of human variants of the mu-opioid receptor gene. Proc Natl Acad Sci USA. 2009;106(26):10811–6.
Manan MM, Ali SM, Khan MA, Jafarian S, Hameed MA. Review on the demographic and social impact of methadone-medication therapy on Malaysian patients. Pak J Pharm Sci. 2013;26(4):841–6.
Zahari Z, Lee CS, Tan SC, Mohamad N, Lee YY, Ismail R. Relationship between cold pressor pain-sensitivity and sleep quality in opioid-dependent males on methadone treatment. Peer J. 2015;3:e839.
Fukuda K, Hayashida M, Ide S, Saita N, Kokita Y, Kasai S, et al. Association between OPRM1 gene polymorphisms and fentanyl sensitivity in patients undergoing painful cosmetic surgery. Pain. 2009;147(1–3):194–201.
Huang CJ, Liu HF, Su NY, Hsu YW, Yang CH, Chen CC, et al. Association between human opioid receptor genes polymorphisms and pressure pain sensitivity in females*. Anaesthesia. 2008;63(12):1288–95.
Zhang W, Chang YZ, Kan QC, Zhang LR, Lu H, Chu QJ, et al. Association of human μ-opioid receptor gene polymorphism A118G with fentanyl analgesia consumption in Chinese gynaecological patients. Anaesthesia. 2010;65(2):130–5.
Hayashida M, Nagashima M, Satoh Y, Katoh R, Tagami M, Ide S, et al. Analgesic requirements after major abdominal surgery are associated with OPRM1 gene polymorphism genotype and haplotype. Pharmacogenomics. 2008;9(11):1605–16.
Zahari Z, Ismail R. Impact of opioid receptor, mu 1 (OPRM1) polymorphisms on pain sensitivity and clinical response to opioid analgesic therapy. Curr Pharmacogenomics Pers Med. 2013;11(1):59–75.
Wang SC, Tsou HH, Chen CH, Chen YT, Ho IK, Hsiao CF, et al. Genetic polymorphisms in the opioid receptor mu1 gene are associated with changes in libido and insomnia in methadone maintenance patients. Eur Neuropsychopharmacol. 2012;22(10):695–703.
Bunten H, Liang WJ, Pounder DJ, Seneviratne C, Osselton D. OPRM1 and CYP2B6 gene variants as risk factors in methadone-related deaths. Clin Pharmacol Ther. 2010;88(3):383–9.
Bunten H, Liang WJ, Pounder DJ, Seneviratne C, Osselton D. Interindividual variability in the prevalence of OPRM1 and CYP2B6 gene variations may identify drug-susceptible populations. J Anal Toxicol. 2011;35(7):431–7.
Compton P, Geschwind DH, Alarcon M. Association between human mu-opioid receptor gene polymorphism, pain tolerance, and opioid addiction. Am J Med Genet B Neuropsychiatr Genet. 2003;121B(1):76–82.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994.
Mohamed Nazar NI. Therapeutic drug monitoring in methadone maintenance therapy (mmt): an evaluation of genetic factors influencing clinical outcomes and serum concentrations of methadone: Ph. D Thesis, Universiti Sains Malaysia; 2013.
Belfer I, Segall SK, Lariviere WR, Smith SB, Dai F, Slade GG, et al. Pain modality- and sex-specific effects of COMT genetic functional variants. Pain. 2013;154(8):1368–76.
Nagaya D, Ramanathan S, Ravichandran M, Navaratnam V. A118G mu opioid receptor polymorphism among drug addicts in Malaysia. J Integr Neurosci. 2012;11(1):117–22.
Tan EC, Tan CH, Karupathivan U, Yap EP. Mu opioid receptor gene polymorphisms and heroin dependence in Asian populations. NeuroReport. 2003;14(4):569–72.
Teh LK, Bannur Z, Zakaria ZA, Fazleen HMH, Salleh MZ. Single nucleotide polymorphism (SNPs) analysis of mu-opioid receptors (OPRM1) using denaturing high performance liquid chromatography (DHPLC) among the intravenous drug users Int. J Pharm Pharm Sci. 2014;6:281–7.
Szeto CY, Tang NL, Lee DT, Stadlin A. Association between mu opioid receptor gene polymorphisms and Chinese heroin addicts. NeuroReport. 2001;12(6):1103–6.
Eyler EC. Chronic and acute pain and pain management for patients in methadone maintenance treatment. Am J Addict. 2013;22(1):75–83.
Xin L, Wang ZJ. Bioinformatic analysis of the human mu opioid receptor (OPRM1) splice and polymorphic variants. AAPS Pharm Sci. 2002;4(4):E23.
Hoehe MR, Kopke K, Wendel B, Rohde K, Flachmeier C, Kidd KK, et al. Sequence variability and candidate gene analysis in complex disease: association of mu opioid receptor gene variation with substance dependence. Hum Mol Genet. 2000;9(19):2895–908.
Lotsch J, Geisslinger G. Relevance of frequent mu-opioid receptor polymorphisms for opioid activity in healthy volunteers. Pharmacogenomics J. 2006;6(3):200–10.
Wendel B, Hoehe MR. The human mu opioid receptor gene: 5′ regulatory and intronic sequences. J Mol Med (Berl). 1998;76(7):525–32.
Ding S, Chen B, Zheng Y, Lu Q, Liu L, Zhuge QC. Association study of OPRM1 polymorphisms with Schizophrenia in Han Chinese population. BMC Psychiatry. 2013;13:107.
White JM. Pleasure into pain: the consequences of long-term opioid use. Addict Behav. 2004;29(7):1311–24.
Compton P, Canamar CP, Hillhouse M, Ling W. Hyperalgesia in heroin dependent patients and the effects of opioid substitution therapy. J Pain. 2012;13(4):401–9.
Fillingim RB, Maixner W. Gender differences in the responses to noxious stimuli. Pain Forum. 1995;4(4):209–21.
Alabas OA, Tashani OA, Tabasam G, Johnson MI. Gender role affects experimental pain responses: a systematic review with meta-analysis. Eur J Pain. 2012;16(9):1211–23.
Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL 3rd. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 2009;10(5):447–85.
Racine M, Tousignant-Laflamme Y, Kloda LA, Dion D, Dupuis G, Choiniere M. A systematic literature review of 10 years of research on sex/gender and experimental pain perception—part 1: are there really differences between women and men? Pain. 2012;153(3):602–18.
Angst MS, Phillips NG, Drover DR, Tingle M, Ray A, Swan GE, et al. Pain sensitivity and opioid analgesia: a pharmacogenomic twin study. Pain. 2012;153(7):1397–409.
Shavers VL, Bakos A, Sheppard VB. Race, ethnicity, and pain among the US adult population. J Health Care Poor Underserved. 2010;21(1):177–220.
Edwards CL, Fillingim RB, Keefe F. Race, ethnicity and pain. Pain. 2001;94(2):133–7.
Rosseland LA, Stubhaug A. Gender is a confounding factor in pain trials: women report more pain than men after arthroscopic surgery. Pain. 2004;112(3):248–53.
Etherton J, Lawson M, Graham R. Individual and gender differences in subjective and objective indices of pain: gender, fear of pain, pain catastrophizing and cardiovascular reactivity. Appl Psychophysiol Biofeedback. 2014;39(2):89–97.
Chen AC, Dworkin SF, Haug J, Gehrig J. Human pain responsivity in a tonic pain model: psychological determinants. Pain. 1989;37(2):143–60.
Doverty M, White JM, Somogyi AA, Bochner F, Ali R, Ling W. Hyperalgesic responses in methadone maintenance patients. Pain. 2001;90(1–2):91–6.
Krishnan S, Salter A, Sullivan T, Gentgall M, White J, Rolan P. Comparison of pain models to detect opioid-induced hyperalgesia. J Pain Res. 2012;5:99–106.
Acknowledgments
We wish to thank Prof. Howard McNulty of the Institute of Pharmacy and Bio-medical Sciences University of Strathclyde for English language editing and proof reading of this article. We are grateful to Nur Amalina Che Rahim and Wan Izzati Mariah Binti Wan Hassan from Department of Pharmacy, Hospital Universiti Sains Malaysia, Kubang Kerian, Kelantan, Malaysia; Hazwan Bin Mat Din and Wan Nor Arifin Wan Harun, Biostatistics and Research Methodology Unit, School of Medical Sciences, Universiti Sains Malaysia; and all the members of Pharmacogenetics and Novel Therapeutics Cluster, Institute for Research in Molecular Medicine (INFORMM), Universiti Sains Malaysia (USM) for their support and valuable suggestions during the study. The study was supported by the Universiti Sains Malaysia (USM) grant under the ‘Research University Cluster (RUC)’ Grant No. 1001.PSK.8620014, under the project; Application of Personalised Methadone Therapy Methadone Maintenance Therapy (PMT for MMT). All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
Zalina Zahari, Chee Siong Lee, Muslih Abdulkarim Ibrahim, Nurfadhlina Musa, Mohd Azhar Mohd Yasin, Yeong Yeh Lee, Soo Choon Tan, Nasir Mohamad, and Rusli Ismail report no conflict of interest.
Compliance with ethics guidelines
The study procedures were approved by the Human Research Ethics Committee (HREC), Universiti Sains Malaysia (USM) in Kelantan, Malaysia (Reference number: USMKK/PPP/JEPeM (253.3 (14))) and the Medical Research and Ethics Committee (MREC) at the Ministry of Health (MOH), Malaysia (Reference number: NMRR-13-524-16614). Informed consent was obtained from all individual participants included in the study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Zahari, Z., Lee, C.S., Ibrahim, M.A. et al. The Opposing Roles of IVS2+691 CC Genotype and AC/AG Diplotype of 118A>G and IVS2+691G>C of OPRM1 Polymorphisms in Cold Pain Tolerance Among Opioid-Dependent Malay Males on Methadone Therapy. Pain Ther 4, 179–196 (2015). https://doi.org/10.1007/s40122-015-0041-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-015-0041-y