Abstract
Introduction
Carbapenem-resistant organisms (CRO) have emerged as a significant worldwide issue. However, the availability of efficacious antibiotics for treating CRO infections remains limited. Polymyxins, including colistin sulfate, represent the last-line therapeutic option against CRO infections. This study aims to retrospectively evaluate the clinical effectiveness and safety of colistin sulfate in managing CRO infections among patients with hematological diseases.
Methods
Between April 2022 and January 2023, a total of 118 hematological patients diagnosed with CRO infection were treated with colistin sulfate at Suzhou Hongci Hospital of Hematology. The assessment encompassed the clinical efficacy, bacterial clearance rate, adverse reactions, and 30-day all-cause mortality.
Results
The study found that the total effective rate of colistin sulfate in the treatment of CRO infection was 74.6%, with a bacterial clearance rate of 72.6%. Throughout the treatment, nephrotoxicity occurred in 7.6% of cases, neurotoxicity in 2.5% of cases, and the 30-day all-cause mortality rate was 22.9%. Multivariate logistic analysis revealed that the treatment course and combination medication with other antimicrobials were independent factors affecting the clinical efficacy of colistin sulfate.
Conclusion
Our study demonstrates that the treatment of colistin sulfate can achieve high clinical efficacy and microbial responses, with a low risk of nephrotoxicity. This study provides evidence of the positive clinical efficacy and safety of colistin sulfate treatment in these patients. High-quality randomized controlled trials are still needed to further confirm the beneficial role of colistin sulfate.
Similar content being viewed by others
Why carry out this study? |
Colistin sulfate has been only clinically available in China, and there is an unmet need to clarify the efficacy and safety of colistin sulfate in hematological patients with carbapenem-resistant organisms (CRO) infections. |
We retrospectively evaluated the efficacy, microbial response, 30-day all-cause mortality, and incidence of adverse events at discontinuation. |
What was learned from the study |
Colistin sulfate can achieve high clinical efficacy and microbial responses, with a low risk of nephrotoxicity in CRO infections. The treatment course and combination medication with other antimicrobials were independent factors affecting the clinical efficacy of colistin sulfate. |
Prospective, multicenter, randomized controlled, and well-designed trials are needed to better evaluate the efficacy and safety of colistin sulfate in the future. |
Introduction
In recent years, with the widespread clinical use of broad-spectrum antibiotics, drug-resistant bacteria have increased remarkably, which may delay targeted therapies and affect public health. Among these, carbapenem-resistant organisms (CRO), especially carbapenem-resistant Enterobacteriaceae (CRE), carbapenem-resistant Acinetobacter baumannii (CRAB), and carbapenem-resistant Pseudomonas aeruginosa (CRPA), are critical well-known contributors to infection-associated morbidity and mortality worldwide and have been identified by the World Health Organization (WHO) as the priority pathogens that critically threaten public health [1, 2].
Patients with hematological malignancies are at high risk for CRO infections [3, 4]. These patients have a higher incidence of CRO infections and mortality than patients in other clinical departments due to primary immunodeficiencies and therapeutic interventions such as chemotherapy, radiotherapy, and hematopoietic stem cell transplantation (HSCT) resulting in neutropenia [1, 5, 6]. Studies revealed that the mortality caused by CRE infections in patients with hematological malignancies ranges from 45.6% to 100% [7,8,9]. Unfortunately, the current availability of antimicrobials for CRO infections is very limited. Polymyxins, the “old” antibiotics that are effective against almost all CRO infections, have returned to clinical practice as the last line of defense [10, 11].
Currently, only three forms of polymyxins are available clinically, i.e., polymyxin B sulfate (PMB), colistin sulfate, and colistimethate sodium (CMS) [12]. Numerous published studies have shown very positive evidence for CMS and PMB in the treatment of CRO infections [13,14,15,16,17]. However, the most common side effects of polymyxins, especially nephrotoxicity, must be considered regarding clinical use [18]. Nephrotoxicity has been reported to occur in up to 50% to 60% of patients treated with CMS or PMB [19]. Moreover, PMB-induced skin hyperpigmentation remains a major quality-of-life concern for patients [20]. These adverse events have somewhat limited the clinical use of PMB and CMS.
As one of the polymyxins, colistin sulfate has been shown in recent studies to have a high clinical and microbiological response but a low nephrotoxicity incidence during the treatment of CRO infections [21,22,23]. However, limited studies have been reported on its efficacy and safety in infections in patients with hematological diseases. Therefore, we conducted this real-world retrospective study of the efficacy and safety of colistin sulfate in these patients, with the aim of providing a reference for the clinical use of this drug.
Methods
Study Design
This observational, retrospective, single-center clinical study was performed at the Hospital of Suzhou Hongci Hematology, Suzhou, Jiangsu Province, China. Data concerning patients treated with colistin sulfate in our hospital between April 2022 and January 2023 were reviewed. This study was approved by the Ethics Committee of the Hospital of Suzhou Hongci Hematology and was exempt from informed consent because of its observational nature. Furthermore, the study was implemented in accordance with the Declaration of Helsinki (as revised in 2013).
The primary outcomes of the study were clinical efficacy, microbial response, 30-day all-cause mortality, and the incidence of adverse events at discontinuation. Secondary outcomes were factors associated with the therapeutic efficacy of colistin sulfate.
Patients
Adult patients were considered eligible if they: (1) were diagnosed with a hematological disease (including malignant hematology and aplastic anemia); (2) had a positive culture for CRO or high suspicion of CRO infection. The diagnosis of CRO infection was made by two clinicians based on culture of CRO from sterile or eligible specimens and high suspicion of CRO infection based on the patient’s clinical symptoms, signs, and laboratory findings, such as fever pattern and inflammatory indicators, despite the absence of positive pathogenic bacterial culture results; (3) had completed clinical data; (4) had received colistin sulfate treatment for ≥ 72 h, either alone or in combination with other antimicrobials. Patients were excluded if they were: (1) under 18 years of age; (2) allergic to the study drug; (3) co-infected with any gram-positive bacteria; (4) died within 48 h after treatment; (5) had incomplete clinical data; (6) had severe organ damage (renal and/or hepatic dysfunction grade > 2 according to the Common Terminology Criteria for Adverse Events [version 5.0]).
Data Collection and Definitions
Patient data collection was based on the electronic medical record system of our hospital. It mainly includes basic demographic characteristics: age, gender, type of hematological disease, hematopoietic stem cell transplantation status, site of infection, distribution of pathogens, infection index, exposure to antimicrobial therapy, clinical and microbiological responses, adverse reactions, and survival status, etc.
All patients in this study were treated with intravenous colistin sulfate (colistin sulfate for injection, Shanghai SPH New Asia Pharmaceutical Co. Ltd., Shanghai, China) for ≥ 72 h at a dose of 1.0–1.5 million IU per day, divided into 2–3 intravenous doses. Clinicians administered colistin sulfate in accordance with the drug package insert, the national consensus on the optimal clinical use of the polymyxins in China [24], as well as adverse reactions and in the context of the patient’s disease progression.
The clinical effectiveness of colistin sulfate treatment was evaluated by clinical and microbiological criteria at the time of drug discontinuation. Patients received multiple courses of colistin sulfate treatment, whereas only the first course of therapy was evaluated. Clinical efficacy was defined as the recovery from symptoms and signs at the end of colistin sulfate treatment, while clinical failure was defined as the aggravation or persistence of symptoms and signs during treatment.
CRO strains were isolated from body fluid specimens of enrolled patients, including sputum, alveolar lavage fluid, and blood. The pathogenic bacteria were extracted and identified through matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. In addition, when there was clinical suspicion of infection in a critically or seriously ill patient, or when empirical treatment had not been effective for 3 days, pathogen metagenomic next-generation sequencing (mNGS) was used for bacterial identification and detection of drug resistance genes in pathogens [25]. In vitro antimicrobial susceptibility testing was performed according to the Clinical and Laboratory Standards Institute (CLSI) guidelines (M100), using the micro-broth dilution method. The results for carbapenems, aminoglycosides, quinolones, fosfomycin, tigecycline, and aztreonam were interpreted according to CLSI breakpoints. Clinical breakpoint reference for colistin susceptibility testing was according to the United States Committee on Antimicrobial Susceptibility Testing (USCAST) (S ≤ 2 mg/l, R ≥ 4 mg/l) [26, 27]. Bacterial clearance was considered a clinically favorable outcome. However, the absence of the above microbiological responses or persistent detection of the same causative pathogens was defined as invalid.
Adverse events associated with colistin sulfate were closely monitored, including nephrotoxicity, hepatotoxicity, and neurotoxicity. The renal and liver functions were evaluated on the day before and after treatment with colistin sulfate. Increased creatinine (Cr) was calculated by subtracting the creatinine level prior to the commencement of colistin sulfate treatment from the post-treatment creatinine level. Renal impairment was assessed according to the Kidney Disease: Improving Global Outcomes (KDIGO) criteria [28]. Neurotoxicity was evaluated according to CTCAE (version 5.0).
Statistical Analysis
SPSS22.0 software was used for statistical analyses (IBM Corp. in Armonk, NY, USA). Data are presented as n (%), mean ± SD, or median (range). Student’s t-tests were performed for continuous variables between groups. The χ2 or Fisher’s exact tests were performed for categorical variables. Variables with a p-value < 0.05 in the univariate analysis were enrolled in the multivariate logistic regression model for further analysis. The Kaplan-Meier curve was used to demonstrate the survival probability. A two-tailed p-value < 0.05 indicates a significant difference.
Results
Patient Demographic and Clinical Characteristics
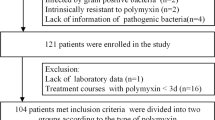
Patients who received colistin sulfate treatment between April 2022 and January 2023 were enrolled. Of 193 patients screened for eligibility, 118 were included in the final analysis based on the inclusion and exclusion criteria (Fig. 1). We summarized the patient demographic and clinical characteristics to describe the overall population. The mean age of these patients was 43.92 ± 15.82 years, including 52 (44.1%) females and 66 (55.9%) males. The most common hematological disease was acute myeloid leukemia (49.2%), followed by acute lymphoblastic leukemia (22.0%), myelodysplastic syndrome (18.6%), and aplastic anemia (10.2%). Among them, 81 (68.6%) patients received allogeneic hematopoietic stem cell transplantation, and 37 (31.4%) received chemotherapy.
All patients were diagnosed with CRO infections, and the most common site of infection was the lung (58.5%), followed by bloodstream (39.8%) and intestinal tract (15.3%). Among them, multiple sites of infection were seen in 21 (17.8%) of the patients. CRKP (28%) was the most commonly monitored CRO in sterile specimens, followed by CRAB (25.4%) and CRPA (20.3%). In addition, there were other CRE (33.1%) infections such as Enterobacter cloacae and Escherichia coli. Of the 118 patients, 33.1% were infected with more than one CRO pathogens.
Colistin Sulfate Administration
Overall, 118 patients received colistin sulfate at doses of 1.0–1.5 million IU/day for a mean treatment duration of 12.75 ± 5.91 (range 4–30) days. The total mean cumulative dose was 17.58 ± 8.70 million IU. Only nine (7.6%) patients were treated with a loading dosage of colistin sulfate at 1.5 million IU. Twenty-one (17.8%) patients received colistin sulfate treatment for no more than 7 days, 61 (51.7%) for 8–14 days, and 36 (30.5%) for > 14 days. Only nine (7.6%) patients received colistin sulfate monotherapy. Forty (33.9%) patients received colistin sulfate combined with one other antibacterial agent, 55 patients (46.6%) with 2, and 14 patients (11.9%) with 3 or more other antibacterial agents. Antibacterial agents used in combination with colistin sulfate included carbapenems, aminoglycosides, quinolones, fosfomycin, tigecycline, aztreonam, etc. (Table 1).
Clinical and Microbiological Outcomes
Based on the clinical response outcomes after colistin sulfate treatment, all patients and relevant variables were categorized into clinically effective and ineffective groups. The key demographic and clinical characteristics and clinical outcomes of these patients are presented below in Table 1. Overall, clinical response was achieved by 88 (74.6%) patients, and 30 (25.4%) patients were considered treatment failure. There were no significant differences between the clinically effective and ineffective groups (all p > 0.05) in terms of age, weight, gender, hematopoietic disease type, hematopoietic stem cell transplantation status, infection sites, and CRO types. Compared to the ineffective group, patients in the clinically effective group had a significantly longer course of treatment (13.73 vs. 9.90 days; p = 0.005) and received a higher cumulative dose of colistin sulfate (18.58 ± 7.89 vs. 14.67 ± 10.35 million IU, p = 0.033). A daily dose of 1.5 million IU/day was significantly more likely with favorable efficacy than that of 1.0 million IU/day (60.2% vs. 39.8%, p = 0.029). Compared to those treated for ≤ 7 days, a longer duration of > 7 days had a significantly higher efficacy rate (88.4% vs. 11.4, p = 0.002). Multiple comparisons of subgroups with different treatment durations showed that a treatment duration of 8–14 days or > 14 days was more advantageous in efficacy than that of a treatment duration of > 7 days (all p < 0.05). However, there was no significant difference in efficacy between treatments with a duration of 8–14 days and > 14 days (Fig. 2A). Compared with the clinically ineffective group, patients in the clinically effective group who were treated with colistin sulfate in combination with other antibiotics had a significantly higher clinical response rate than that of monotherapy (p = 0.016). Multiple comparisons of subgroups with different medications showed that the efficacy of colistin sulfate in combination with one or two antibacterial agents was superior to that of colistin sulfate monotherapy, but it was not when combined with three antibacterial agents (Fig. 2B).
A Compared with the efficacy of colistin sulfate at different treatment durations. B Compared with the efficacy of colistin sulfate at different antimicrobial combinations. Antibacterial agents used in combination with colistin sulfate included carbapenems, aminoglycosides, quinolones, fosfomycin, tigecycline, aztreonam, etc. *p < 0.05; **p < 0.001; NS not statistically significant
Of the 106 patients with bacterial culture results, 77 (72.6%) achieved eradication of the causative microorganism, including 72 (88.9%) in the effective group and 5 (20.0%) in the ineffective group. Compared to the ineffective group, patients in the clinically effective group had a significantly higher microbial response rate (p < 0.001).
Analysis of Infection Indicators
The changes in clinical parameters were evaluated before and after colistin sulfate treatment. Overall, all monitored clinical infection-associated indicators were improved after colistin sulfate treatment, with neutrophil counts and platelet levels significantly increased (p < 0.05), and C-reaction protein (CRP) and procalcitonin (PCT) levels significantly decreased (p < 0.05). Compared to baseline, an increase in creatinine (Cr) was observed after colistin sulfate administration, suggesting that colistin sulfate treatment might impair renal function. However, the level of alanine aminotransferase (ALT), aspartate aminotransferase (AST), and total bilirubin (TBIL) did not change significantly, suggesting that colistin sulfate did not affect liver function (p > 0.1) (Fig. 3).
Comparison of patient clinical parameters at baseline and after therapy. Pre: indicates the baseline level before colistin sulfate treatment; post: indicates the level after colistin sulfate treatment; SD standard deviation; ALT alanine aminotransferase; AST aspartate aminotransferase; Cr creatinine; CRP C-reaction protein; PLT platelet; PCT procalcitonin; TBIL total bilirubin. Data were expressed as mean ± SD. *p < 0.05; **p < 0.001; NS not statistically significant
Factors Associated with Clinical Efficacy
Multivariate logistic regression was used to analyze all above variables that showed significant differences and potentially affected the colistin treatment efficacy. The treatment course (p = 0.031; OR = 2.980; 95% CI 1.107–8.019) and combination with other antibacterial agents (p = 0.012; OR = 3.009; 95% CI 1.276–7.095) were identified factors that were significantly associated with the treatment effectiveness of colistin sulfate. These suggest that the treatment duration of colistin sulfate and co-medication with other antibacterial agents, rather than the daily dose of colistin sulfate and transplant status, might affect the curative effect (Fig. 4).
Mortality Analysis
Twenty-seven patients died within 30 days, with an overall 30-day all-cause mortality of 22.9%. Compared to the ineffective group, patients in the clinically effective group had significantly lower 30-day mortality (8.0% vs. 66.7%, χ2 = 43.71, p < 0.001) (Fig. 5).
Safety Evaluation
Overall, nephrotoxicity was observed in nine (7.6%) cases and neurotoxicity in three cases (2.5%). The incidence of these adverse events was comparable between the clinically effective and ineffective groups, with incidences of nephrotoxicity of 5.7% and 13.3% (p = 0.221) and neurotoxicity of 5.7% and 13.3% (p = 0.159), respectively (Table 1). These nine patients developed renal impairment within 4–7 days after drug administration, of which seven patients experienced a gradual decrease in creatinine after discontinuation of colistin sulfate and two died the next day of acute renal failure caused by septic shock. Three patients with neurotoxicity were relieved 2 days after discontinuation of colistin sulfate (not shown in Table 1). Treatment with colistin sulfate was safe and well tolerated.
Discussion
In this study, the clinical data of 118 patients with CRO infections treated with colistin sulfate were retrospectively analyzed. Based on the product sheet’s recommended dose of 1.0–1.5 million IU per day, clinical response and bacterial clearance was achieved in 74.6% and 65.3%, respectively, showing superior effectiveness over that previously published retrospective studies by Jin et al. (58% and 40%, respectively) and Lu et al. (53.8% and 49.1%, respectively) [29]. Notably, in the current study population, approximately six in ten patients had pulmonary infections, while none of these patients received nebulized antibiotic therapy. Effective antibiotic therapy for pulmonary infections requires the drug concentration at the infection site to be sufficient to meet or exceed the minimal inhibitory concentration (MIC) to inhibit or kill a particular bacterial strain. Although lung tissue penetration of colistin sulfate after intravenous infusion is unknown, and how this may affect the clinical efficacy in our studied population remains unclear, it is reasonable to assume a higher efficacy when using nebulized along with intravenous infusion of colistin sulfate considering that polymyxins do not efficiently diffuse into tissues and generally have poor penetration into the lung tissue [30].
In addition, a study of polymyxin B in patients with CRO infections showed that treatment with a duration of 8–14 days or > 14 days had significantly greater efficacy than those with a duration of 3–7 days (all p < 0.05); however, extending the treatment duration to > 14 days did not show a significant increase in efficacy compared to that treatment for 8–14 days (p > 0.05) [15]. The results of our study are consistent with those of polymyxin B. Extending the treatment duration of colistin sulfate to 8–14 days can result in better clinical efficacy than that not exceeding 7 days. Although a treatment duration of > 14 days also showed better efficacy, it seems this treatment duration confers no additional significant benefit compared with that of 8–14 days. However, prior studies examining the impact of the polymyxin treatment duration on hematological patients with CRO infection remain limited. Therefore, the optimal treatment course for colistin sulfate for patients with hematological diseases remains uncertain and needs to be further investigated.
Heterogeneous resistance against polymyxins has been often observed during the treatment of CRE, CRPA, and CRAB infections [31]. However, the risk of heterogeneous resistance can be improved or decreased by using a combination of polymyxins and other antimicrobials [32,33,34]. In our study, 80.5% of patients were treated with colistin sulfate combined with one or two other antimicrobials, and clinical response was achieved by 80.0% of these patients. This is considered comparable to the results of other studies on polymyxin combination therapy versus polymyxin monotherapy [35,36,37]. Notably, in our current study, only a small fraction of patients (9/118) received colistin sulfate monotherapy, and the corresponding results are based on a small sample size, which may cause statistical errors.
In the univariate study, increasing the daily dose of colistin sulfate could improve the efficacy, but further multivariate logistic analysis showed that the daily dose was not a factor affecting the efficacy, which might be disturbed by the interaction of combination drugs.
High post-treatment CRP and PCT levels indicated poor therapeutic effects of antibiotics. CRP and PCT are reliable biomarkers for differentiating bacterial infections in monitoring inflammation and infection courses [38,39,40]. The present study demonstrated a significant decrease in the levels of CRP and PCT after treatment with colistin sulfate. Due to the lack of therapeutic drug monitoring (TDM), post-treatment CRP and PCT levels were used to assess the response of patients to colistin sulfate therapy and to determine whether to continue therapy. In addition, the neutrophil and platelet counts were significantly increased in patients with hematological diseases. In turn, the increase of neutrophils after colistin sulfate treatment contributes to anti-infective therapy.
In terms of adverse events, the overall incidence of adverse events to colistin sulfate is low. In this study, only 7.6% of the patients had mild nephrotoxicity, 2.5% had neurotoxicity, and no patients had hepatic dysfunction. Studies have shown that nephrotoxicity is dose limiting for polymyxins [19, 41, 42]. Two recent meta-analyses showed that the overall incidences of CMS- and PMB-induced nephrotoxicity were 34.8% and 45%, respectively [43, 44]. Compared with those of CMS and polymyxin B, the event of renal impairment associated with colistin sulfate was considerably lower (up to 9.2%) [21, 45]. Furthermore, unlike polymyxin B, we did not find any skin hyperpigmentation in the current study [15]. Considering these findings, we suggest that the rational use of colistin sulfate in the clinic is effective and safe.
However, this study has several limitations. First, this is a single-center retrospective study with limited sample size. Second, the drug concentrations of colistin sulfate were not monitored during the treatment, and PK/PD analysis was lacking. Clinicians made clinical decisions about dosage, administration, and duration based on guidelines and personal clinical experience, which made it difficult to identify the optimal therapeutic concentrations. Third, the majority of patients were treated with colistin sulfate in conjunction with other drugs, and colistin sulfate might be not solely responsible for the ultimate effectiveness. Moreover, in the current study, a significant fraction of patients (58.5%) had lung infections but did not receive any nebulized antibiotic therapy, which may affect the possible antimicrobial treatment and outcomes. Therefore, prospective, multicenter, randomized controlled, and well-designed trials are needed to better evaluate the efficacy and safety of colistin sulfate in the future.
Conclusions
As one of the polymyxins, colistin sulfate has been marketed in China in 2018 and has played an increasingly important role in the treatment of CRO infections. There is an unmet need to clarify the efficacy and safety of colistin sulfate in hematological patients with CRO infections, and such a real-world study fills the gap in the current literature and provides a valuable reference for the clinical use of colistin sulfate. As the study had shown, colistin sulfate is an effective antimicrobial drug against CRO infections. Furthermore, the study found that the treatment course of colistin sulfate and its combination with other antimicrobial agents were the factors affecting the clinical efficacy of colistin sulfate. Colistin sulfate has a low incidence of nephrotoxicity and neurotoxicity, which provides a reference value for the rational use of colistin sulfate in clinical practice.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Averbuch D, Tridello G, Hoek J, et al. Antimicrobial resistance in Gram-negative rods causing bacteremia in hematopoietic stem cell transplant recipients: intercontinental prospective study of the infectious diseases working party of the european bone marrow transplantation group. Clin Infect Dis. 2017;65(11):1819–28.
Zeng M, Xia J, Zong Z, et al. Guidelines for the diagnosis, treatment, prevention and control of infections caused by carbapenem-resistant gram-negative bacilli. J Microbiol Immunol Infect. 2023;S1684–1182(23):00036–41.
Loon KV, Voor in ‘T Holt AF, Vos MC. A systematic review and meta-analyses of the clinical epidemiology of carbapenem-resistant Enterobacteriaceae. Antimicrob Agents Chemother. 2018;62(1):e01730-e11717.
Micozzi A, Gentile G, Minotti C, et al. Carbapenem-resistant Klebsiella pneumoniae in high-risk haematological patients: factors favouring spread, risk factors and outcome of carbapenem-resistant Klebsiella pneumoniae bacteremias. BMC Infect Dis. 2017;17(1):203.
Satlin MJ, Jenkins SG, Walsh TJ. The global challenge of carbapenem-resistant Enterobacteriaceae in transplant recipients and patients with hematologic malignancies. Clin Infect Dis. 2014;58(9):1274–83.
Satlin MJ, Cohen N, Ma KC, et al. Bacteremia due to carbapenem-resistant Enterobacteriaceae in neutropenic patients with hematologic malignancies. J Infect. 2016;73(4):336–45.
Andria N, Henig O, Kotler O, et al. Mortality burden related to infection with carbapenem-resistant Gram-negative bacteria among haematological cancer patients: a retrospective cohort study. J Antimicrob Chemother. 2015;70(11):3146–53.
Lalaoui R, Javelle E, Bakour S, et al. Infections due to carbapenem-resistant bacteria in patients with hematologic malignancies. Front Microbiol. 2020;11:1422.
Jaiswal SR, Gupta S, Kumar RS, et al. Gut colonization with carbapenem-resistant enterobacteriaceae adversely impacts the outcome in patients with hematological malignancies: results of a prospective surveillance study. Mediterr J Hematol Infect Dis. 2018;10(1): e2018025.
Adukauskiene D, Ciginskiene A, Adukauskaite A, et al. Clinical features and outcomes of monobacterial and polybacterial episodes of ventilator-associated pneumonia due to multidrug-resistant Acinetobacter baumannii. Antibiotics (Basel). 2022;11(7):892.
Tsuji BT, Pogue JM, Zavascki AP, et al. International consensus guidelines for the optimal use of the polymyxins: endorsed by the American college of clinical pharmacy (ACCP), European society of clinical microbiology and infectious diseases (ESCMID), infectious diseases society of America (IDSA), international society for anti-infective pharmacology (ISAP), society of critical care medicine (SCCM), and society of infectious diseases pharmacists (SIDP). Pharmacotherapy. 2019;39(1):10–39.
El-Sayed Ahmed MAE, Zhong LL, Shen C, et al. Colistin and its role in the Era of antibiotic resistance: an extended review (2000–2019). Emerg Microbes Infect. 2020;9(1):868–85.
Sirijatuphat R, Thawornkaew S, Ruangkriengsin D, et al. Colistin monotherapy versus colistin plus sitafloxacin for therapy of carbapenem-resistant acinetobacter baumannii infections: a preliminary study. Antibiotics (Basel). 2022;11(12):1707.
Zheng G, Cai J, Zhang L, et al. Ceftazidime/avibactam-based versus polymyxin B-based therapeutic regimens for the treatment of carbapenem-resistant klebsiella pneumoniae infection in critically ill patients: a retrospective cohort study. Infect Dis Ther. 2022;11(5):1917–34.
Xia GL, Jiang RL. Efficacy and safety of polymyxin B in carbapenem-resistant gram-negative organisms infections. BMC Infect Dis. 2021;21(1):1034.
Zhang X, Qi S, Duan X, et al. Clinical outcomes and safety of polymyxin B in the treatment of carbapenem-resistant Gram-negative bacterial infections: a real-world multicenter study. J Transl Med. 2021;19:431.
Yu Z, Liu X, Du X, et al. Pharmacokinetics/pharmacodynamics of polymyxin B in patients with bloodstream infection caused by carbapenem-resistant Klebsiella pneumoniae. Front Pharmacol. 2022;13: 975066.
Wagenlehner F, Lucenteforte E, Pea F, et al. Systematic review on estimated rates of nephrotoxicity and neurotoxicity in patients treated with polymyxins. Clin Microbiol Infect. 2021;S1198–743X(20):30764–73.
Zavascki AP, Nation RL. Nephrotoxicity of polymyxins: is there any difference between colistimethate and polymyxin B? Antimicrob Agents Chemother. 2017;61(3):e02319-e2416.
Mattos KPH, Cintra ML, Gouvêa IR, et al. Skin hyperpigmentation following intravenous polymyxin B treatment associated with melanocyte activation and inflammatory process. J Clin Pharm Ther. 2017;42(5):573–8.
Xie YL, Jin X, Yan SS, et al. Population pharmacokinetics of intravenous colistin sulfate and dosage optimization in critically ill patients. Front Pharmacol. 2022;13: 967412.
Peng D, Zhang F, Chen Y, et al. Efficacy and safety of colistin sulfate in the treatment of infections caused by carbapenem-resistant organisms: a multicenter retrospective cohort study. J Thorac Dis. 2023;15(4):1794–804.
Jin J, Zhu J, Zhu Z, et al. Clinical efficacy and nephrotoxicity of intravenous colistin sulfate in the treatment of carbapenem-resistant gram-negative bacterial infections: a retrospective cohort study. Ann Transl Med. 2022;10(20):1137.
Infectious Diseases Society of China, Chinese Thoracic Society, Chinese Society of Critical Care Medicine, et al. [Multi-disciplinary expert consensus on the optimal clinical use of the polymyxins in China]. Zhonghua Jie He He Hu Xi Za Zhi. 2021, 44(4):292–310
Editorial Board of Chinese Journal of Infectious Diseases. Clinical practice expert consensus for the application of metagenomic next generation sequencing (In Chinese). Chin J Infect Dis. 2020;38(11):681–9.
Yang QW, Ma XL, Hu FP, et al. Expert consensus on polymyxin antimicrobial susceptibility testing and clinical interpretation. Chin Med Sci J. 2021;36(1):1–16.
Pogue JM, Jones RN, Bradley JS, et al. Polymyxin susceptibility testing and interpretive breakpoints: recommendations from the United States committee on antimicrobial susceptibility testing (USCAST). Antimicrob Agents Chemother. 2020;64(2):e01495-e1519.
Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179-184.
Lu X, Zhong C, Liu Y, Ye H, Qu J, Zong Z, Lv X. Efficacy and safety of polymyxin E sulfate in the treatment of critically ill patients with carbapenem-resistant organism infections. Front Med (Lausanne). 2022;9:1067548.
Ayoub MC. Polymyxins and bacterial membranes: a review of antibacterial activity and mechanisms of resistance. Membranes (Basel). 2020;10(8):181.
Stefaniuk EM, Tyski S. Colistin resistance in enterobacterales strains - a current view. Pol J Microbiol. 2019;68(4):417–27.
Rodriguez CH, De Ambrosio A, Bajuk M, et al. In vitro antimicrobials activity against endemic Acinetobacter baumannii multiresistant clones. J Infect Dev Ctries. 2010;4(3):164–7.
Pankuch GA, Lin G, Seifert H, et al. Activity of meropenem with and without ciprofloxacin and colistin against Pseudomonas aeruginosa and Acinetobacter baumannii. Antimicrob Agents Chemother. 2008;52(1):333–6.
Gordon NC, Png K, Wareham DW. Potent synergy and sustained bactericidal activity of a vancomycin-colistin combination versus multidrug-resistant strains of Acinetobacter baumannii. Antimicrob Agents Chemother. 2010;54(12):5316–22.
Zusman O, Altunin S, Koppel F, et al. Polymyxin monotherapy or in combination against carbapenem-resistant bacteria: systematic review and meta-analysis. J Antimicrob Chemother. 2017;72(1):29–39.
Nutman A, Lellouche J, Temkin E, et al. Colistin plus meropenem for carbapenem-resistant Gram-negative infections: in vitro synergism is not associated with better clinical outcomes. Clin Microbiol Infect. 2020;26(9):1185–91.
Saelim W, Changpradub D, Thunyaharn S, et al. Colistin plus sulbactam or fosfomycin against carbapenem-resistant acinetobacter baumannii: improved efficacy or decreased risk of nephrotoxicity? Infect Chemother. 2021;53(1):128–40.
Covington EW, Roberts MZ, Dong J. Procalcitonin monitoring as a guide for antimicrobial therapy: a review of current literature. Pharmacotherapy. 2018;38(5):569–81.
Dias RF, de Paula ACRB, Hasparyk UG, et al. Use of C-reactive protein to guide the antibiotic therapy in hospitalized patients: a systematic review and meta-analysis. BMC Infect Dis. 2023;23(1):276.
Henriquez-Camacho C, Losa J. Biomarkers for sepsis. Biomed Res Int. 2014;2014: 547818.
Pogue JM, Ortwine JK, Kaye KS. Are there any ways around the exposure-limiting nephrotoxicity of the polymyxins? Int J Antimicrob Agents. 2016;48(6):622–6.
Azad MAK, Nation RL, Velkov T, et al. Mechanisms of polymyxin-induced nephrotoxicity. Adv Exp Med Biol. 2019;1145:305–19.
Wang JL, Xiang BX, Song XL, et al. Prevalence of polymyxin-induced nephrotoxicity and its predictors in critically ill adult patients: a meta-analysis. World J Clin Cases. 2022;10(31):11466–85.
Sisay M, Hagos B, Edessa D, et al. Polymyxin-induced nephrotoxicity and its predictors: a systematic review and meta-analysis of studies conducted using RIFLE criteria of acute kidney injury. Pharmacol Res. 2021;163: 105328.
Hao M, Yang Y, Guo Y, et al. Combination regimens with colistin sulfate versus colistin sulfate monotherapy in the treatment of infections caused by carbapenem-resistant gram-negative bacilli. Antibiotics (Basel). 2022;11(10):1440.
Funding
The work was supported by grants from the Su Zhou Industrial Park He He Yuan Da Blood Innovation Research Institute (H221084); Innovative and Applied Scientific Research Project of Professional Ability of Clinical Specialists (RCLX2315016). The journal’s Rapid Service Fee was sponsored by The Hospital of Suzhou Hongci Hematology.
Author information
Authors and Affiliations
Contributions
Yuanbing Wu and Xiaohui Hu designed the study; Depei Wu provided administrative support; Xiaohui Hu provided the study materials and patients; Shanshan Jiang, Dongyang Li, Yaxue Wu, Qian Li, Xing Wang, Bin Liu, Haiyan Bao collected the data; Shanshan Jiang and Dongyang Li performed the data analyses and interpretation; Yuanbing Wu wrote the manuscript. All authors reviewed the manuscript and approved the final version.
Corresponding authors
Ethics declarations
Conflict of Interest
Yuanbing Wu, Shanshan Jiang, Dongyang Li, Yaxue Wu, Qian Li, Xing Wang, Bin Liu, Haiyan Bao, Depei Wu, and Xiaohui Hu declared no competing interests.
Ethical Approval
This retrospective study was performed at the Hospital of Suzhou Hongci Hematology, Suzhou, Jiangsu Province, China. This study was approved by the Ethics Committee of the Hospital of Suzhou Hongci Hematology and was exempt from informed consent because of its observational nature. Furthermore, the study was implemented in accordance with the Declaration of Helsinki (as revised in 2013).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wu, Y., Jiang, S., Li, D. et al. Clinical Efficacy and Safety of Colistin Sulfate in the Treatment of Carbapenem-Resistant Organism Infections in Patients with Hematological Diseases. Infect Dis Ther 13, 141–154 (2024). https://doi.org/10.1007/s40121-023-00909-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-023-00909-8