Abstract
Appropriately selected neutralising monoclonal antibodies (nmAbs) are an effective treatment for patients with mild or moderate coronavirus disease 2019 (COVID-19) who are at high risk of progression to severe disease. In contrast, the efficacy of nmAbs in patients hospitalised with COVID-19 has been mixed, and clinical benefit has largely been restricted to seronegative patients [i.e. those lacking endogenous severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antibodies] in the trials with positive outcomes. This review summarises the major clinical trial data investigating nmAb treatment for hospitalised patients with COVID-19, and explores current definitions of seropositivity, what they mean in a late-pandemic context and discusses the current late-pandemic challenges associated with defining ‘seroprotection’ in a clinically meaningful way. We conclude that following widespread vaccination, increasing numbers of prior infections and emerging viral variants, seropositivity now reflects a range of immune coverage rather than a binary tool with which to aid decision-making on a clinically actionable timescale. Treatment decisions with nmAbs in a late-pandemic context would therefore likely best rely on information regarding clinical status, time since symptom onset, underlying patient condition(s) and the dominant circulating variant, should they be approved for future use in hospitalised patients with COVID-19.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Neutralising monoclonal antibodies (nmAbs) are clearly effective as early treatment for ambulatory patients with mild or moderate COVID-19 who are at high risk of progression to severe disease when circulating variants are susceptible, but their success in patients hospitalised with COVID-19 has been mixed. |
Existing clinical trial data showed that efficacy of nmAbs in hospitalised COVID-19 patients was limited to seronegative patients. |
In the current post-pandemic context of widespread vaccination, increasing numbers of prior infections and emerging viral variants, stratifying patients by serostatus is even more complex than it was in immunologically naïve populations. |
We propose that information regarding clinical status, time since symptom onset, underlying patient condition(s) and the dominant circulating variant may be more relevant than serostatus to inform treatment decisions with nmAbs in a late-pandemic context. |
Introduction
Neutralising monoclonal antibodies (nmAbs; alternatively named nAbs or mAbs) against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have emerged as effective prophylaxis and early treatment for outpatients with coronavirus disease 2019 (COVID-19) with risk factors for progression to severe disease [1,2,3]. However, the success of nmAb-based treatments in patients hospitalised for severe COVID-19 has been mixed [4,5,6,7,8,9]. Some trials failed to find evidence of nmAb efficacy and were halted for futility, while others reported efficacy in seronegative patients (lacking endogenous anti-SARS-CoV-2 antibodies), but failed to establish efficacy in seropositive patients [4,5,6,7,8,9]. This has led to the widespread perception that nmAbs are ineffective against SARS-CoV-2–seropositive patients, a view that is reflected in current treatment guidelines for hospitalised COVID-19 patients [10,11,12].
The definition of ‘seropositive’ is context- and trial-dependent, and the associated nuances must be considered before interpreting existing clinical trial results in a late-pandemic context of widespread vaccination and increasing numbers of citizens who have been infected once or more with SARS-CoV-2. A patient’s endogenous neutralising seropositivity to a prior variant or vaccine does not necessarily imply neutralisation against incrementally divergent variants, and a wider appreciation of this is needed. This is exemplified by the current SARS-CoV-2 Omicron subvariants BQ.1, BQ1.1, and XBB.1.5, which evade humoral immunity even in multiply-vaccinated seropositive patients, and illustrates the gap between a simple binary definition of seropositivity and the diagnostic limitations that emerge after vaccine- or recovery-related seroconversion [13]. At the current juncture of the pandemic, the virus has escaped our diagnostic ability to ascertain these distinctions in a widely deployable point-of-care fashion.
In this review, we explore the role of SARS-CoV-2 serostatus and nmAbs for patients hospitalised with COVID-19. We discuss considerations for defining seropositivity in the late-pandemic era, including the role of waning immunity, considerations for nmAb variant matching and the potential need to take patient comorbidity and immunocompetence into account when making treatment decisions. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Defining SARS-CoV-2 Seropositivity
Stratifying patients by serostatus was a useful distinction during the early phase of the pandemic when populations were immunologically naïve to SARS-CoV-2. However, in a late-pandemic era, it is incrementally more challenging to determine the importance of seropositivity given the rapid accumulation of variants. Saliently, while anti-nucleocapsid seropositivity may be helpful in distinguishing prior recovered wild-type infection from vaccine-induced humoral immunity, it is not likely to be a correlate of protection. This is because the viral nucleocapsid within the enveloped virus is not an accessible neutralising epitope. Moreover, immunoglobulins (IgG) against the nucleocapsid protein are reported to wane rapidly within a timescale of a few months; [14] as such, anti-nucleocapsid seronegativity does not imply a lifetime of immune naïveté regarding exposure to SARS-CoV-2, as recovered individuals can wane from seropositive to seronegative over the course of the first year post-infection. In contrast to the nucleocapsid protein, the envelope-embedded SARS-CoV-2 viral spike protein is critical for viral entry into the target host cell, rendering it available as a neutralising viral epitope (this is also the key epitope for most vaccines). Neutralising IgGs predominantly (>90%) target the receptor-binding domain (RBD) of the viral spike protein [15, 16] and thus prevent virus binding to the human angiotensin-converting enzyme 2 receptor [17]. As neutralising IgGs track reasonably well with an acute immune response, and because of their ability to restrict viral growth in vitro, their presence is believed to be the best potential accessible correlate for predicting protection against SARS-CoV-2 reinfection [18]. Unfortunately, mutations within the spike sequence are rapidly acquired, resulting in viral evolution that contributes to SARS-CoV-2 variant immune evasion. Although variant-susceptible neutralising anti-spike humoral immunity appears to be a correlate of protection, the technology to distinguish variant-specific neutralising antibodies is restricted to specialist laboratories only, and thus is impractical for day-to-day clinical decisions.
Various tests and definitions for seropositivity have been used across different clinical studies. The phase 3, multi-centre, adaptive platform study ACTIV-3 (NCT04501978) defined seropositive patients both by presence of neutralising IgG anti-spike antibodies and by quantitative measurements of anti-nucleocapsid antibodies [4, 5, 8]. Anti-spike (RBD) neutralising antibodies were measured using a surrogate viral neutralisation test (sVNT), whereby trends for improved efficacy in seronegative versus seropositive patients were observed using ≥ 30% binding inhibition to define seropositivity, albeit with a relatively low sample size. Theoretically, a pseudovirus neutralisation assay would benefit clinical decision-making; however, the assay time and resource intensity required renders it impractical at the clinical care level.
The RECOVERY platform trial (NCT04381936) primarily used an indirect enzyme-linked immunosorbent assay for anti-spike IgG to define baseline seropositive patients, with post-hoc sensitivity analyses using immunoassays to detect total anti-spike RBD and anti-nucleocapsid antibodies [6]. However, neutralising antibody tests were not used in RECOVERY. The COV-2066 (NCT04426695) study of casirivimab together with imdevimab used anti-spike (IgA or IgG) or anti-nucleocapsid (IgG) qualitative assays for the main analyses, whereby a positive test in any one of the three assays resulted in a seropositive classification [9]. In addition, in a post-hoc analysis, patients from the COV-2066 study who were seropositive at baseline were further characterised by the presence or absence of neutralising antibodies using an sVNT, which revealed a subpopulation of neutralising antibody-negative seropositive patients who may also benefit from nmAb treatment [19].
It is important to stress that these trials were conducted in the early-to-middle phase of the pandemic when population serostatus levels were low and vaccines were not yet widely available. Therefore, the utility of previously accepted definitions for seropositivity need to be revisited in the context of widespread vaccination and prior infection. Correlates between antibody levels and neutralisation, in the context of new circulating variants, are ultimately needed to better define which subsets of hospitalised COVID-19 patients are most likely to benefit from nmAb treatment. This is particularly relevant as most authorised nmAbs for outpatients have reduced activity to Omicron subvariants (such as BQ.1/BQ1.1 and XBB.1.5) [20], which, as of January 2023, are exponentially increasing globally [21] and dominant in Europe and the USA. Notably, these variants also express a high capacity to evade neutralisation in multiply-vaccinated individuals [13, 22], further underlining the potential futility in relying on a simple seropositive laboratory test to predict response to treatment. However, it is entirely reasonable to assume the susceptibility of future SARS-CoV-2 variants to nmAbs could vary dynamically with antigenic drift.
nmAbs in the Hospitalised Setting: Clinical Trial Evidence to Date
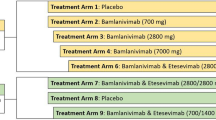
To date, the results of six phase 3 nmAb monotherapy or combination trials involving patients hospitalised for COVID-19 have been published (Table 1) [4,5,6,7,8,9]. Several of these have been investigated as part of the ACTIV-3 inpatient platform trial. ACTIV-3 showed that bamlanivimab (LY-CoV555) monotherapy resulted in no improvement in the primary endpoint of sustained recovery up to day 90 versus placebo [rate ratio (RR) 1.06; 95% CI 0.77–1.47] in the overall hospitalised COVID-19 patient population [4]. Interestingly, a subsequent post-hoc examination of the primary endpoint in patients by baseline serostatus suggested seronegative patients (RR 1.24; 95% CI 0.90–1.70) may derive greater benefit than seropositive patients (RR 0.74; 95% CI 0.54–1.00) [23]. A qualitative, statistically non-significant trend towards patient harm among those seropositive at baseline was noted following high-dose (7 g) bamlanivimab infusion, raising the query of whether humoral immune reconstitution might have a paradoxical adverse immunologic effect. However, no firm conclusions could be made as the trial was not sufficiently powered for subgroup analyses.
Additional nmAbs have been investigated as part of subsequent iterations of the ACTIV-3 study, whereby 536 patients were randomised to receive either sotrovimab monotherapy, the combination of BRII-196 together with BRII-198, or placebo [5]. Neither sotrovimab monotherapy nor BRII-196 together with BRII-198 demonstrated efficacy for improving sustained recovery by day 90 among patients hospitalised for COVID-19 (adjusted RR 1.08; 95% CI 0.88–1.32; p = 0.48). A pre-specified subgroup analysis showed that BRII-196 together with BRII-198 may potentially have clinical benefit in patients who were seronegative (adjusted RR 1.19; 95% CI 0.89–1.59) for endogenous neutralising antibodies to SARS-CoV-2, but not in those who were seropositive (adjusted RR 0.90; 95% CI 0.66–1.24). However, again the trial was under-powered for such subgroup analyses meaning firm conclusions could not be drawn. There was also a signal for potential harm from BRII-196 together with BRII-198 among patients who were seropositive at baseline (defined by presence of neutralising IgG anti-spike antibodies or total IgG anti-nucleocapsid antibodies), which the authors speculated may be due to antibody-dependent enhancement of inflammation and/or viral replication. No such efficacy or safety trends were observed with patients treated with sotrovimab, which had similar results regardless of serostatus, yet was also under-powered for subgroup analysis. There is an ongoing evaluation of sotrovimab in the RECOVERY platform trial (NCT04381936), which will be powered for a primary endpoint of 28-day all-cause mortality.
The ACTIV-3 study more recently investigated the combination of tixagevimab together with cilgavimab in 1455 patients with COVID-19 receiving remdesivir and other standard care [8]. The trial passed the early futility analysis, but there was no difference in the primary endpoint of cumulative incidence of sustained recovery between tixagevimab together with cilgavimab and placebo at day 90 in the full cohort (recovery RR 1.08; 95% CI 0.97–1.20; p = 0.21), with similar results reported for the seronegative population (recovery RR 1.14; 95% CI 0.97–1.34), even though the trial was sufficiently powered to detect a difference in this pre-specified population. Despite no effect of the ordinal scale outcomes for the primary endpoint, mortality was lower in the tixagevimab together with cilgavimab arm (hazard ratio 0.70; 95% CI 0.50–0.97) and there was no evidence of harm with the combination, either in the full cohort or by baseline serostatus.
A recent open-label, phase 3 study in hospitalised COVID-19 patients treated with the nmAb JS016 (also known as etesevimab or LY-CoV016) found that treatment led to no improvement in the primary endpoint of their inpatient six-point ordinal scale compared with patients receiving standard care only (odds ratio 0.31; 95% CI 0.03–3.19; p = 0.33); no examination of efficacy by patient serostatus was made [7].
The combination of casirivimab together with imdevimab was examined as part of the phase 3, open-label RECOVERY platform trial, and was compared with usual care in 9785 hospitalised patients with COVID-19 [6]. The nmAb combination reduced the primary endpoint of 28-day all-cause mortality versus placebo (24% versus 30%; RR 0.79; 95% CI 0.69–0.91; p = 0.0009) in patients who were seronegative at baseline (primarily defined as lacking anti-spike IgG); in seropositive patients, however, there was no difference in 28-day all-cause mortality between treatment groups (RR 1.09; 95% CI 0.94–1.25), and there was significant heterogeneity of the effect of the nmAb combination on mortality between seronegative and seropositive patients (p = 0.002). The pooled mortality rate ratio favoured the usual care arm, consistent with some smaller nmAb trials in hospitalised patients; however, a signal for harm cannot be firmly concluded given the 95% confidence interval crossed 1 (i.e. unity).
A second phase 2/3 trial compared casirivimab together with imdevimab versus placebo in 1336 hospitalised COVID-19 patients who were receiving low-flow or no supplemental oxygen (Study COV-2066; NCT04426695) [9]. The primary virological endpoint was met in seronegative patients, with viral loads significantly reduced with this nmAb combination versus placebo (–0.28 log10 copies/mL; 95% CI –0.51, –0.05; p = 0.017). The primary clinical endpoint of death or mechanical ventilation from day 6 to 29 in patients with high viral load had a positive trend towards a reduction in treated patients, that did not reach statistical significance [relative risk reduction (RRR) 25.5%; 95% CI –16.2, 52.2; p = 0.20]. In seronegative patients, the nmAb combination reduced the relative risk of mechanical ventilation or death from day 6 to 29 by 47% (RRR 47.1; 95% CI 10.2–68.8; nominal p = 0.02). In addition, casirivimab together with imdevimab numerically reduced the relative risk of all-cause mortality in seronegative patients by 56% through day 29 (RRR 55.6; 95% CI 24.2–74.0; nominal p = 0.003). In the overall seropositive population [defined as having a positive result in at least one of the anti-spike (IgG or IgA) or anti-nucleocapsid (IgG) tests], there was no clinical benefit of casirivimab together with imdevimab (risk of mechanical ventilation or death from day 1 to 29, RRR 19.5%; 95% CI –32.8, 51.2; nominal p = 0.30), while no harm signals were documented in this subgroup. Efficacy was further examined in a subset (~ 20%) of seropositive patients who were negative or borderline for functional endogenous neutralising antibodies to SARS-CoV-2 [19]. In these patients, casirivimab together with imdevimab treatment led to reduced viral load and a trend towards reduction of death or mechanical ventilation (RRR 42.9; 95% CI, –17.7, 72.3; nominal p = 0.11), and all-cause mortality (RRR 43.8; 95% CI –25.2, 74.8; nominal p = 0.12) versus placebo. These trends were not observed in seropositive patients who were also positive for endogenous neutralising antibodies.
Altogether, the available clinical trial data performed predominantly in non-vaccinated patients in the early-to-mid pandemic, before nearly universal prior recovery or vaccination, suggest that the clinical efficacy of nmAbs initially depended on baseline serostatus, with benefit primarily observed in seronegative patients. Most trials defined patient serostatus at least in part by qualitative testing for anti-spike or anti-nucleocapsid IgG binding antibodies, as well as neutralising antibodies (in the ACTIV-3 studies); however, definitions of seropositivity varied by trial, limiting the utility of this short-hand nomenclature. It is worth noting that, in addition to their direct antiviral neutralisation effect, potential immunological effector functions (e.g. via Fc-mediated effects) of some nmAbs may potentially act independently, and this is an avenue that warrants further investigation [24].
Guidelines for nmAbs in Hospitalised COVID-19 Patients
Due to their mixed success in clinical trials of patients hospitalised for COVID-19, nmAbs do not feature strongly in current treatment guidelines for inpatients [10,11,12], and no nmAbs are currently approved for treatment in this setting. The National Institutes of Health recommendations reflect the need to consider real-time SARS-CoV-2 epidemiology when considering any nmAb treatment decision. With rapid change in the circulation of new SARS-CoV-2 variants, particular attention should be paid to research on the impacts of these variants on activity of the various nmAbs. The Infectious Diseases Society of America acknowledges that nmAbs studied in clinical trials among hospitalised patients, as of the time of writing (January 2023), show no activity against predominant regional variants, but recognises the need to continue to accumulate clinical evidence with new and existing nmAbs in hospitalised patients [11].
Despite acknowledging the importance of serostatus in clinical decision-making with nmAbs, current guidelines do not consider the interplay of vaccination with serostatus. Nor do guidelines offer any recommendations on appropriate tests to define serostatus that may inform on nmAb treatment decisions, or on the potential importance of antibody levels that might drive clinical decision-making. A better discussion of the need for variant-specific serostatus is needed, as is a unified definition of serostatus. This will be especially important in the context of the evolving epidemiological situation and the circulation of new immune-escaped variants, and should take into account the fact that the majority of patients have received prior vaccination, previously recovered and/or are immunocompromised.
The Adaptive Immune Response to SARS-CoV-2 Infection: Overlapping Routes to Seroconversion via Vaccination and Recovery
Exposure to viral antigens primes naïve B and T cells to differentiate into functional immune effector cells, of which antibody-producing plasma cells and mature helper or cytotoxic T cells are the most important [25]. Helper T cells elicit several effector functions, including playing a critical role in neutralising antibody responses, while cytotoxic T cells kill virus-infected cells, particularly those presenting viral peptides on HLA class I molecules [25]. In contrast, B cells produce a range of different classes of antibodies following HLA class II-mediated antigen presentation, whereby the antibody response to SARS-CoV-2 infection involves the development of immunoglobulins, particularly IgA, IgM and IgG antibodies [25]. SARS-CoV-2 immunobiology may violate canonical dogma regarding IgM to IgG class switching, as both classes can arise simultaneously. Rechallenging with subsequent infection may also generate a new IgM response rather than solely affinity maturation of prior IgG response.
Seroconversion can occur via vaccination, previous infection or by current infection, meaning that, compared with the start of the COVID-19 pandemic, most individuals are currently likely to be seropositive by at least one measure. As new variants emerge through viral evolution and immune-escape mechanisms, seroconversion may not necessarily correlate with protective immunity against contemporaneously circulating variants, thus complicating clinical decision-making. In addition, the degree of protective immunity from memory T cells is not well understood; this may play a complex role due to the broad array of epitopes recognised.
As of January 2023, almost 70% of eligible individuals globally are thought to have had at least one dose of a COVID-19 vaccine [26], meaning that even though these individuals are likely to have positive serology by at least some measure, it is not clear what their protective immunity status is against a specific variant [27]. In addition, immunocompromised individuals, although having positive post-vaccine serology, may develop less robust immune responses resulting in a higher incidence of breakthrough infections and severe outcomes. Seroconversion during acute infection can occur as early as 8 days from symptom onset [28], but the timing of seroconversion can vary depending on several factors, including disease severity, patient characteristics (e.g. age or immunocompetence) and type of assay used. This has implications for the optimal timing of treatment with nmAbs, and notwithstanding the problems of meaningfully defining seroprotection, the ability to determine seroconversion status quickly during the infection process would be important for nmAb treatment decisions.
Current Perspectives and Future Directions on the Role of Serostatus in nmAb Treatment Decisions in Hospitalised Patients
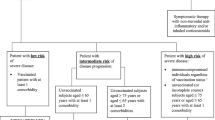
In our opinion, seropositivity alone is no longer a relevant predictor of treatment benefit because (1) its definition is malleable and context specific, and additional terms with greater specificity are needed; (2) it does not imply protection from disease caused by newer variants; (3) it does not distinguish between seroconversion acquired following vaccination, infection, or hybrid humoral response acquired following both vaccination and infection; and (4) it does not indicate whether it is sufficient to ‘control’ the current infection. While seronegativity after vaccination may reflect either an insufficient or an appropriate, physiologic, waning response to vaccination, seropositivity does not imply protection due to the inability to distinguish between historic vaccination/infection versus response to recent or active infection; even if the infection is known to be active, it is not possible to easily ascertain whether the antibodies detected are variant-matched and likely to provide protection against the current infection. As such, our opinion is that patient history (e.g. previous infection, vaccination status and date of last booster) and serostatus may have transitioned to be of limited benefit in clinical decision-making with nmAbs in the current phase of the pandemic. As we await further diagnostic advances, the most informative details regarding decision-making for treatment with nmAbs are likely to be current clinical status (e.g. severity of ongoing infection), time since symptom onset, underlying patient condition (e.g. elderly, multi-comorbid, immunocompromised) and knowledge of the dominant circulating variant and whether it evades pre-existing immunity. These factors all require investigation in clinical trials with nmAbs in hospitalised patients.
References
Dougan M, Nirula A, Azizad M, Mocherla B, Gottlieb RL, Chen P, et al. Bamlanivimab plus etesevimab in mild or moderate Covid-19. N Engl J Med. 2021;385(15):1382–92.
Weinreich DM, Sivapalasingam S, Norton T, Ali S, Gao H, Bhore R, et al. REGEN-COV antibody combination and outcomes in outpatients with Covid-19. N Engl J Med. 2021;385(23): e81.
Gupta A, Gonzalez-Rojas Y, Juarez E, Crespo Casal M, Moya J, Falci DR, et al. Early treatment for Covid-19 with SARS-CoV-2 neutralizing antibody sotrovimab. N Engl J Med. 2021;385(21):1941–50.
ACTIV-3 Therapeutics for Inpatients with COVID-19 Study Group. A neutralizing monoclonal antibody for hospitalized patients with Covid-19. N Engl J Med. 2021;384(10):905–14.
ACTIV-3 Therapeutics for Inpatients with COVID-19 Study Group. Efficacy and safety of two neutralising monoclonal antibody therapies, sotrovimab and BRII-196 plus BRII-198, for adults hospitalised with COVID-19 (TICO): a randomised controlled trial. Lancet Infect Dis. 2022;22(5):622–35.
RECOVERY Collaborative Group. Casirivimab and imdevimab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2022;399(10325):665–76.
Dong R, Jiang L, Yang T, Wang C, Zhang Y, Chen X, et al. Efficacy and safety of SARS-CoV-2 neutralizing antibody JS016 in hospitalized Chinese patients with COVID-19: a phase 2/3, multicenter, randomized, open-label, controlled trial. Antimicrob Agents Chemother. 2022;66(3): e0204521.
ACTIV-3 Therapeutics for Inpatients with COVID-19 (TICO) Study Group. Tixagevimab-cilgavimab for treatment of patients hospitalised with COVID-19: a randomised, double-blind, phase 3 trial. Lancet Respir Med. 2022;10(10):972–984. https://doi.org/10.1016/S2213-2600(22)00215-6
Somersan-Karakaya S, Mylonakis E, Menon VP, Wells JC, Ali S, Sivapalasingam S, et al. Casirivimab and imdevimab for the treatment of hospitalized patients with COVID-19. J Infect Dis. 2022;382:2372.
National Institutes of Health. Anti-SARS-CoV-2 Monoclonal Antibodies 2022. Available from https://www.covid19treatmentguidelines.nih.gov/therapies/anti-sars-cov-2-antibody-products/anti-sars-cov-2-monoclonal-antibodies/?utm_source=site&utm_medium=home&utm_campaign=highlights.
Infectious Diseases Society of America. Neutralizing Antibodies for Treatment 2022. Available from https://www.idsociety.org/globalassets/idsa/practice-guidelines/covid-19/treatment/idsa-covid-19-gl-tx-and-mgmt---na-tx-2022-05-24.pdf.
World Health Organization. Therapeutics and COVID-19: living guideline 2022. Available from https://www.who.int/publications/i/item/WHO-2019-nCoV-therapeutics-2022.5.
Hoffmann M, Behrens GMN, Arora P, Kempf A, Nehlmeier I, Cossmann A, et al. Effect of hybrid immunity and bivalent booster vaccination on omicron sublineage neutralisation. Lancet Infect Dis. 2022;23(1):25–8.
Lumley SF, Wei J, O’Donnell D, Stoesser NE, Matthews PC, Howarth A, et al. The duration, dynamics, and determinants of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antibody responses in individual healthcare workers. Clin Infect Dis. 2021;73(3):e699–709.
Suthar MS, Zimmerman MG, Kauffman RC, Mantus G, Linderman SL, Hudson WH, et al. Rapid generation of neutralizing antibody responses in COVID-19 patients. Cell Rep Med. 2020;1(3): 100040.
Piccoli L, Park YJ, Tortorici MA, Czudnochowski N, Walls AC, Beltramello M, et al. Mapping neutralizing and immunodominant sites on the SARS-CoV-2 spike receptor-binding domain by structure-guided high-resolution serology. Cell. 2020;183(4):1024-1042 e21.
Lee HJ, Jung J, Lee JH, Lee DG, Kim YB, Oh EJ. Comparison of six serological immunoassays for the detection of SARS-CoV-2 neutralizing antibody levels in the vaccinated population. Viruses. 2022;14(5):946.
European Centre for Disease Prevention and Control. Immune responses and immunity to SARS-CoV-2 2022. Available from https://www.ecdc.europa.eu/en/covid-19/latest-evidence/immune-responses.
Hooper AT, Somersan-Karakaya S, McCarthy SE, Mylonakis E, Ali S, Mei J, et al. Casirivimab and imdevimab treatment reduces viral load and improves clinical outcomes in seropositive hospitalized COVID-19 patients with nonneutralizing or borderline neutralizing antibodies. mBio. 2022;13(6): e0169922.
European Medicines Agency. ETF warns that monoclonal antibodies may not be effective against emerging strains of SARS-CoV-2 2022. Available from https://www.ema.europa.eu/en/news/etf-warns-monoclonal-antibodies-may-not-be-effective-against-emerging-strains-sars-cov-2.
REGENERON. COVID-19 Dashboard 2023. Available from https://covid19dashboard.regeneron.com/?tab=Home.
Kurhade C, Zou J, Xia H, Liu M, Chang HC, Ren P, et al. Low neutralization of SARS-CoV-2 Omicron BA.2.75.2, BQ.1.1 and XBB.1 by parental mRNA vaccine or a BA5 bivalent booster. Nat Med. 2022. https://doi.org/10.1038/s41591-022-02162-x.
ACTIV-3 Therapeutics for Inpatients with COVID-19 Study Group. Responses to a neutralizing monoclonal antibody for hospitalized patients with COVID-19 according to baseline antibody and antigen levels: a randomized controlled trial. Ann Intern Med. 2022;175(2):234–43.
Zhang A, Stacey HD, D’Agostino MR, Tugg Y, Marzok A, Miller MS. Beyond neutralization: Fc-dependent antibody effector functions in SARS-CoV-2 infection. Nat Rev Immunol. 2022. https://doi.org/10.1038/s41577-022-00813-1.
Sette A, Crotty S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell. 2021;184(4):861–80.
Our World In Data. Coronavirus (COVID-19) vaccinations 2022. Available from https://ourworldindata.org/covid-vaccinations.
World Health Organization. Interim statement on decision-making considerations for the use of variant updated COVID-19 vaccines 2022. Available from https://www.who.int/news/item/17-06-2022-interim-statement-on-decision-making-considerations-for-the-use-of-variant-updated-covid-19-vaccines.
Deeks JJ, Dinnes J, Takwoingi Y, Davenport C, Spijker R, Taylor-Phillips S, et al. Antibody tests for identification of current and past infection with SARS-CoV-2. Cochrane Database Syst Rev. 2020;6:CD013652.
Acknowledgements
Funding
F. Hoffmann-La Roche Ltd funded medical writing assistance and the journal’s Rapid Service Fee.
Medical Writing and/or Editorial Assistance
Third-party medical writing assistance, under the direction of the authors, was provided by John Bett, PhD, of Ashfield MedComms, an Inizio company, and funded by F. Hoffmann-La Roche Ltd.
Author Contributions
Robbert L Gottlieb and Francois Raffi: conceptualisation, writing, reviewing and editing of the manuscript. Both authors approved the submitted version.
Disclosures
Dr Francois Raffi received research funding or honoraria from or consulted for AbbVie, AstraZeneca, Gilead Sciences, GSK, Janssen, MSD, Roche, Synairgen, Theratechnologies, ViiV Healthcare. Dr Robert L Gottlieb has served on scientific advisory boards for AbbVie, Eli Lilly, Gilead Sciences, GSK, Roche, and served as a consultant for Gilead Sciences, Johnson & Johnson, Kinevant Sciences (indirectly, through his institution), and has served on a speaker bureau for Pfizer unrelated to COVID-19. His institution received a gift-in-kind to facilitate a multi-centre clinical trial outside the scope of COVID-19 (NCT03383419). He discloses a de minimis investment in AbCellera.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Raffi, F., Gottlieb, R.L. Monoclonal Antibodies in Hospitalised Patients with COVID-19: The Role of SARS-COV-2 Serostatus in an Evolving Pandemic. Infect Dis Ther 12, 735–747 (2023). https://doi.org/10.1007/s40121-023-00769-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-023-00769-2