Abstract
Introduction
Herpes zoster (HZ) and its complications still represent a significant burden for patients and health care systems. In Spain, vaccination is progressively being introduced and recommended for patients between 65 and 80 years old and patients > 18 years of age suffering from certain immunosuppression conditions. The aim of this study is to estimate the number of hospital admissions related to HZ from 2016 to 2019 in Spain.
Methods
Data were collected from the Minimum Basic DataSet (MBDS) and codified according to the Spanish version of the 10th International Classification of Disease (ICD-10-CM codes B02—B02.9). Among others, variables such as sex, age and presence of complications were included.
Results
A total of 27,642 hospitalizations were identified (90% in patients > 50 and 45.8% in patients > 80). Women represented 51.2% of the patients, and 59.9% of patients presented complications related to HZ. The hospitalization rate was 17.74, the mortality rate was 1.2, and the case fatality rate was 6.75%. All rates were significantly higher with age, among men and in complicated HZ. Immunosuppression status for which vaccination had been recommended represented 22.7% of the total cases, affecting mostly individuals > 65 and causing more deaths in those > 80 years. The estimated annual cost of hospitalization for herpes zoster was €35,738,285, and the mean cost per patient was €5172.
Conclusion
The hospitalization burden for HZ is still important in Spain. Data on the current epidemiology are important to evaluate future vaccination strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hospitalization burden due to herpes zoster (resulting after reactivation on varicella zoster virus from its latent state) can have a great impact on healthcare systems |
Sex, age, immunosuppression, and other underlying chronic conditions are risk factors for hospitalization due to herpes zoster-associated complications |
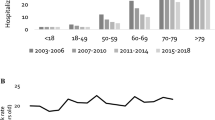
We observed an increasing trend in Spain, which demonstrates that the hospitalization rate related to herpes zoster has doubled over the last 20 years |
In Spain, vaccination is recommended for the elderly and for immunosuppressed patients, regardless their age |
Despite the low rate of mortality, a good understanding of the epidemiology of hospitalizations due to herpes zoster can tackle the burden on healthcare and evaluate future prevention strategies |
Introduction
Herpes zoster (HZ) results from reactivation of varicella zoster virus (VZV), which stays latent in the sensory ganglia of individuals previously infected during childhood,e.g., with chickenpox. HZ causes rash and severe pain followed by a vesicular eruption in the corresponding dermatome [1]. In 20–50% of the cases, it leads to complications, especially post-herpetic neuralgia (PHN), defined as persisting pain 1 month from the beginning of the skin lesions. Other complications may include otic, ocular and central nervous system (CNS) involvement [1].
Several risk factors have been identified, including female sex and age, with 68.8% of the cases and 80.2% of the hospitalizations registered in individuals aged ≥ 50 and 97.2% of the deaths of individuals > 65 [2]. Other risk factors for hospitalization may include immunosuppression, certain chronic conditions, genetics, depression, psychologic stress and mechanical trauma [3].
Currently, treatments for HZ and PHN are mainly symptomatic, with limited efficacy [4]. In terms of prevention of HZ, two vaccines were approved by the European Medicines Agency (EMA): Zostavax ® (ZVL), a single-dose live attenuated vaccine, and Shingrix ® (RZV), a two-dose recombinant vaccine [5]. In 2018, the Advisory Committee on Immunization Practices (ACIP) recommended the use of Shingrix over Zostavax, as it may be administered to immunocompetent adults aged > 50 years, adults with chronic medical conditions and immunocompromised individuals in certain situations [6]. In Spain, the Ministry of Health intends to progressively incorporate vaccination with Shingrix and has recently recommended its prioritization among: (1) the general population aged 65–80 years, starting with the 80-year-old cohort, and (2) patients aged > 18 years with hematopoietic stem cell transplantation (HSCT), solid organ transplantation (SOT), hematologic tumors and solid tumors undergoing chemotherapy as well as individuals infected with human immunodeficiency virus (HIV) and patients with rheumatoid arthritis (RA) receiving anti-JAK therapy [7].
In Europe, the annual incidence of HZ is 2–4.6 cases per 1000 population. In Spain, 3–5 cases per 1000 were estimated from 1998 to 2018, with an annual average number of hospitalizations of 3022 per 100,000 and an average number of deaths of 19 per year [2]. Despite low mortality rates, HZ and PHN result in a significant burden for patients and health care systems, which is expected to increase [3]. A good understanding of the epidemiology of HZ is essential to evaluate ongoing and future prevention strategies.
We aim to estimate the burden of herpes zoster-related hospitalizations from 2016 to 2019 in Spain. Given that HZ vaccines are already available, our study may have considerable value for public health policy decision-making.
Methods
Study Design
We performed a retrospective epidemiologic study of all hospital admissions related to HZ during the period 2016–2019 in Spain. Data were collected from the Minimum Basic Data Set (MBDS) from the Spanish Ministry of Health and codified according to the Spanish version of the 10th International Classification of Disease (ICD-10-CM). We included all hospital discharges with HZ codified in any diagnostic position (primary or secondary). For each case, information about age, sex, region of Spain, length of stay, outcome and comorbidities was collected. We classified HZ cases as uncomplicated (code B02.9) or complicated (the remaining B02 codes). Complicated HZ included encephalitis, meningitis or other nervous system complications, ophthalmic affection, disseminated HZ and other unspecified complications (please see Supplementary Table 1). For comorbidities, we selected and codified those in which vaccination has been specifically recommended by the Spanish Ministry of Health: hematopoietic stem cell transplantation, solid organ transplantation, anti-JAK therapy in patients with rheumatoid arthritis, HIV, hematologic tumors and solid tumors undergoing chemotherapy (please see Supplementary Table 2).
Statistical Analysis
The total hospitalization rate (number of admissions diagnosed with HZ per 100,000 population), median length of stay (total length of stay/total number of hospitalizations), mortality rate (number of deaths at hospital per 100,000 population) and case-fatality rate (number of deaths at hospital/number of hospitalizations, expressed in percentage) were calculated from the overall period 2016–2019 in Spain for each (autonomous) region and for all the comorbidities mentioned before. The annual hospitalization rate in Spain was also calculated per year. The total Spanish population stratified by sex and age was used as the denominator in each case; the rates were adjusted by age. Finally, the total and average costs per HZ hospitalization (total annual cost/total number of hospitalizations per year, in euros) were estimated.
All analyses were performed by sex and age for complicated and uncomplicated HZ cases (according to the ICD-10-CM codes). The following age groups were created: < 50, 50–59, 60–69, 70–79 and ≥ 80 years. For the analysis performed by comorbidities, we decided to state three groups (< 65, 65–79 and ≥ 80) based on the recommendations for vaccination made by the Spanish Ministry of Health.
The Statistical Package for Social Sciences (SPSS/PASW, version 27) was used to perform statistical analyses. For statistical comparison, a p value of 0.05 was considered significant. Poisson regression was used to compare hospitalization rates. Logistic regression was used to analyze case fatality rates. Mean hospital stay lengths were compared using ANOVA. The patient information was anonymized and de-identified prior to the analysis in compliance with ethics guidelines. The study was performed in accordance with the Helsinki Declaration 1964 and its later amendments. The Rey Juan Carlos University Ethics Committee Board ruled that no formal ethics approval was required for this study.
Results
A total of 27,642 cases of HZ were registered during the period 2016–2019, of which 90% were patients > 50 years old and 45.8% were individuals > 80. Almost 52% of the cases were found in women, and 59.9% were related to complicated HZ (Table 1).
The hospitalization rate during the study period was 17.74 hospitalizations per 100,000 inhabitants (CI 95% 17.53–17.95). This rate increased significantly with age, reaching a maximum in the population ≥ 80 years (104.58 per 100,000 inhabitants). Significantly higher rates were also observed among men in both uncomplicated and complicated HZ. This can be found in all age groups except for the total group, which becomes significant when comparing age-adjusted rates The median length of stay was 7 days (IQR 13–4), with no differences by age or sex (Table 1).
During the study period, we observed a significant increase in the hospitalization rates over time in both complicated and uncomplicated HZ (Fig. 1).
The mortality rate was 1.2 deaths per 100,000 inhabitants (CI 95% 1.15–1.25), and the case fatality rate was 6.75% (CI 95% 6.45–7.05). When compared by age and sex, both rates were significantly higher with age (reaching a maximum of 10.65 per 100,000 and a 9.6% among patients ≥ 80) and among men when analyzing age-adjusted rates (Table 1).
Complicated HZ caused more hospitalizations than uncomplicated HZ. Complicated HZ caused higher mortality and case fatality rates in women ≥ 80 and men of all ages, excluding the group of 60–69 years (Table 1).
Figure 2 shows the hospitalization rate for HZ in each autonomous region of Spain. La Rioja has the highest hospitalization rate (30.81 per 100,000 inhabitants), followed by País Vasco (26.55 per 100,000 population), Castilla y León (25.86 per 100,000) and Madrid (25.24 per 100,000). Ceuta, Melilla and the Canary Islands show the lowest hospitalization rates (5.65, 5.3 and 7.94 per 100,000 population, respectively).
Among the studied comorbidities, the most common was solid tumors. We found a total of 3078 cases (11.14% of the total hospitalizations), of which 51.2% corresponded to complicated HZ. The second most common one was hematologic tumors, with 1237 cases identified (4.48% of the hospitalizations), of which 56.1% were related to complicated HZ. All comorbidities were more frequent in men, except for RA. Most of the cases of HSCT and HIV occurred in patients < 65. RA was more frequent in those aged > 65. Both solid and hematologic tumors were more common in the 65- to 79-year-old group. The total average length of hospital stay was 7 days, and total in-hospital mortality was 1867 cases (6.75%), of which 58% were related to complicated HZ. A significantly higher number of deaths was observed in individuals ≥ 80 years in all the groups, with no differences observed by sex (Table 2).
Hospitalizations for HZ were estimated to generate a total cost of €142.953.128 and an annual expenditure of €35,738,285 for the healthcare system. The mean cost per patient was €5172 (Table 3).
Discussion
The main objective of our study was to describe and analyze the burden of hospitalizations related to HZ in Spain in a given period. We identified > 27,000 hospitalizations related to HZ infection between 2016 and 2019. We also found that the hospitalization rate was 17.74 per 100,000 population, which was slightly higher than the rates previously reported in Spain from 1998 to 2018 [8,9,10,11]. This increasing trend is consistent with the results found by the last review performed by the Ministry of Spain, which states that the hospitalization rate related to HZ has doubled within the past 20 years. In Europe, the results varied from 18.16 hospitalizations per 100,000 in Italy [12] to 24.8 hospitalizations per 100,000 population in Norway [13]. Studies conducted in the USA and Japan reported hospitalization rates of 9.92 and 17.8, respectively [14, 15]. This variation could be explained by inter-individual differences between populations, different National Health Systems, national databases and criteria for hospitalization [16, 17].
When analyzing these results, it is important to consider that several factors may have contributed to this increase. On one hand, as has been previously described, it can be attributed to an increase in the mean age of the > 85 year group related to an increase in life expectancy. As HZ incidence increases with age, a higher hospitalization rate in this group can be expected [11, 18]. Furthermore, this could also be associated with an increase in the number of hospitalizations for any cause in those aged > 75 years during the study period and with an increase in the incidence of some immunosuppressive and chronic conditions, such as diabetes, chronic obstructive pulmonary disease (COPD) and depression, which are described as risk factors for HZ [3, 10, 11]. On the other hand, as we considered hospitalizations related to HZ in any diagnostic position, we could not know whether the patient was hospitalized for HZ or developed it during the hospital stay [11], which could be a major limitation of our study.
Some differences have been observed regarding the rate of hospitalization among regions of Spain. They follow the same pattern shown in previous studies. Thus, higher rates were found in the north, whereas the Canary Islands had the lowest rates. This has been attributed to a lower seroprevalence of VZV related to geographic characteristics [9]. Additionally, a younger population is found in the Canary Islands in contrast to an older population located in northern Spain [19]. We also found an increase in hospitalizations over time in almost all regions, which is consistent with our total results [9, 19, 20].
As in similar studies, age was identified as the main risk factor for HZ, with 90% of the hospitalizations found in patients older than 50 years and 45.8% of them estimated in patients over 80 years [2, 10]. This is thought to be mainly related to the decrease in cell immunity associated with age but also to the higher incidence of comorbidities, polypharmacy and social-environmental changes associated with elderly individuals, such as institutionalization or lack of family or social support [3, 21, 22].
Although female sex is described as an independent risk factor for HZ [23], we found that both hospitalization and mortality rates were higher among men. This can be attributed to a higher incidence of associated comorbidities (especially immunosuppression conditions such as HIV or tumors) and a lower average life expectancy in men [3]. When reviewing the current literature, the same discordant results were found [3, 10, 24]. Similar results were shown in the last study done in Spain by the Ministry of Health [10], while a study conducted by Esteban Vasallo et al. identified higher rates in men except for extreme ages [3], and other European studies found higher rates of hospitalization and mortality for females [24, 25].
Immunosuppression has been proven to be highly associated with HZ, as it is identified in almost one-third of patients [3, 9, 16]. When analyzing those comorbidities in which vaccination is recommended by the Ministry of Health, they represented 22.7% of total hospitalizations, 6.75% of hospital mortality and 20% of the complicated total cases. As in other studies, tumors were the most frequent comorbidity, and all comorbid illnesses were higher among men [3, 9, 26]. Although immunosuppression conditions were found in patients of all ages, most of the cases affected the 65–79-year-old group, and higher mortality rates were found in patients over 80 years for all conditions.
MBDS is a feasible and sensitive way to study the epidemiology of a disease, as it provides a large representative sample size that gives great statistical power to the study. However, it can have some limitations due to its nature. First, as we considered hospitalization related to HZ in any diagnostic position, we could not identify whether HZ was the main cause of the hospitalization. Second, as our aim was to focus on the burden of hospitalizations, we chose to analyze the number of hospitalizations and not the number of patients so several hospitalizations could occur for the same patient. Potential biases associated with the codification process should also be considered, although a positive predictive value of 89%–96% over an ICD9 diagnostic code of HZ [10] has been reported. Furthermore, ICD10 has no code for either “hematologic tumors and solid tumors undergoing chemotherapy” or “rheumatoid arthritis receiving anti JAK therapy,” so we included all solid and hematologic tumors and AR cases. Finally, the MBDS does not include useful data on disease severity, microbiologic confirmation, medication and other procedures or patients’ functional level and social situation. However, HZ is an easily recognizable disease that can be clearly diagnosed clinically, not resulting in an overdiagnosis or infradiagnosis.
Therefore, we consider that immunocompromised patients of all ages would benefit from vaccination with the new recombinant vaccine, especially those older than 80 years. Other common chronic conditions, such as diabetes mellitus or chronic obstructive pulmonary disease (COPD), have also been described as risk factors for HZ. Although we did not include them in our study, they have been identified as priority groups for immunization in the future [3, 5]. On the other hand, immunocompromised adults should never receive the live HZ vaccine (Zostavax) because the vaccine virus itself can cause disseminated viral infection and even death [27].
Although HZ is not in general a life-threatening disease, this condition primarily affects individuals > 80 years of age and is more prevalent among men. This population has underlying comorbitidies that may increase the risk of mortality. However, even if the mortality rate is low, HZ in a high-risk population may reduce the patient's health-related quality of life [9, 10, 19, 26].
Regarding HZ vaccination, the positive impact on epidemiologic indicators has been seen in the reduction of HZ incidence in children vaccinated against varicella [28]. Some studies propose that this impact may be greater among the elderly with high coverage (currently between 58 and 72% of the population) [29, 30]. In Spain, it is estimated that 97% of the child population is vaccinated against varicella, but in the elderly this coverage decreases to 57%. We should be aware of preventive measures to improve later outcomes among the elderly population.
Furthermore, we have shown that our hospitalization rates are higher than those previously reported in Spain, with almost 60% of hospitalizations attributed to complicated HZ, as already reported elsewhere (48.7–53%), estimated at a cost of €35.7 million per year, which would be higher if indirect costs were also considered [3, 8]. Finally, regarding mortality, a systematic review of HZ-associated mortality in Europe reported that available data on HZ mortality are too heterogeneous to for cross-country comparisons [31].
As discussed above, the main limitation of our study is that it was based on administrative data (MBDS). Electronic health records allow for greater availability of data collection, but as long as databases such as the MBDS focus on economic management, clinical relevance may be limited. One of the aims of MBDS is to facilitate clinical research, but the validity of the dataset depends on the accuracy of clinical discharge reports. If primary or secondary diagnoses are incorrect, or incomplete, or some clinical conditions are excluded, the reliability of our dataset is not be guaranteed. We are aware that there is some discrepancy between correct and incorrect diagnoses recorded in the MBDS, and this is an important limitation of our study. Although a certain amount of misclassification errors is expected, the MBDS can provide valid information and can be a useful tool in epidemiologic studies [32, 33].
Conclusions
The burden of hospitalization related to herpes zoster is still important in Spain, as it is higher with age, among men and in immunocompromised patients. We can conclude that the main risk factors are aging and immunosuppression. The results obtained regarding the epidemiology of HZ in Spain are similar to those previously found in national and international literature. However, data on the epidemiology of HZ are needed to evaluate the potential impact of future vaccination. Finally, an interesting future research line is more detailed studies to assess its cost-effectiveness and its impact on quality of life once the HZ vaccine is introduced in a given national program.
References
Hope-Simpson RE. The nature of herpes zoster: a long-term study and a new hypothesis. Proc R Soc Med. 1965;58(1):9–20.
Yawn BP, Saddier P, Wollan PC, St Sauver JL, Kurland MJ, Sy LS. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc. 2007;82(11):1341–9.
Esteban-Vasallo MD, Domínguez-Berjón MF, de Miguel GÁ, Astray-Mochales J, Blanco-Ancos LM, Gil-Prieto R. Characteristics of herpes zoster-associated hospitalizations in Madrid (SPAIN) before vaccine availability. J Infect. 2016;72(1):70–9.
Lopez-Belmonte JL, Cisterna R, de Miguel GA, Guilmet C, Bianic F, Uhart M. The use of Zostavax in Spain: the economic case for vaccination of individuals aged 50 years and older. J Med Econ. 2016;19(6):576–86.
Siedler A, Koch J, Garbe E, Hengel H, von Kries R, Ledig T, et al. Background paper to the decision to recommend the vaccination with the inactivated herpes zoster subunit vaccine: Statement of the German Standing Committee on Vaccination (STIKO) at the Robert Koch Institute. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2019;62(3):352–76.
Dooling KL, Guo A, Patel M, Lee GM, Moore K, Belongia EA, et al. Recommendations of the Advisory Committee on immunization practices for use of Herpes Zoster vaccines. MMWR Morb Mortal Wkly Rep. 2018;67(3):103–8.
Anderson TC, Masters NB, Guo A, Shepersky L, Leidner AJ, Lee GM, et al. Use of recombinant zoster vaccine in immunocompromised adults aged ≥19 years: recommendations of the Advisory Committee on Immunization Practices—United States, 2022. MMWR Morb Mortal Wkly Rep. 2022;71(3):80–4.
Esteban-Vasallo MD, Domínguez-Berjón MF, Gil-Prieto R, Astray-Mochales J, de Miguel GÁ. Temporal trends in herpes zoster-related hospitalizations in Madrid (Spain), 2003–2013. J Infect. 2015;71(1):85–92.
Gil A, Gil R, Alvaro A, San Martín M, González A. Burden of herpes zoster requiring hospitalization in Spain during a seven-year period (1998–2004). BMC Infect Dis. 2009;7(9):55.
Masa-Calles J, López-Perea N, Vila Cordero B, Carmona R. Surveillance and epidemiology of Herpes Zoster in Spain. Rev Esp Salud Publica. 2021;95:e202106088.
Gil-Prieto R, Walter S, Gonzalez-Escalada A, Garcia-Garcia L, Marín-García P, Gil-de-Miguel A. Different vaccination strategies in Spain and its impact on severe varicella and zoster. Vaccine. 2014;32(2):277–83.
Piazza MF, Paganino C, Amicizia D, Trucchi C, Orsi A, Astengo M, et al. The unknown health burden of herpes zoster hospitalizations: the effect on chronic disease course in adult patients ≥50 years. Vaccines (Basel). 2020;8(1):E20.
Mirinaviciute G, Quist-Paulsen E, Brantsæter AB, Flem E. The burden of herpes zoster disease in Norway. Vaccine. 2020;38(18):3501–7.
Tseng HF, Bruxvoort K, Ackerson B, Luo Y, Tanenbaum H, Tian Y, et al. The epidemiology of herpes zoster in immunocompetent, unvaccinated adults ≥50 years old: incidence, complications, hospitalization, mortality, and recurrence. J Infect Dis. 2020;222(5):798–806.
Kuniyoshi Y, Tokutake H, Takahashi N, Kamura A, Yasuda S, Tashiro M. Routine varicella vaccination program and hospitalization for herpes zoster in Japan. Hum Vaccin Immunother. 2021;17(11):4171–6.
Esteban-Vasallo MD, Domínguez-Berjón MF, Gil-Prieto R, Astray-Mochales J, de Miguel GA. Sociodemographic characteristics and chronic medical conditions as risk factors for herpes zoster: a population-based study from primary care in Madrid (Spain). Hum Vaccin Immunother. 2014;10(6):1650–60.
Kawai K, Gebremeskel BG, Acosta CJ. Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open. 2014;4(6): e004833.
Pérez Díaz J, Abellán García A, Aceituno Nieto P, Ramiro Fariñas D. Un perfil de las personas mayores en España, 2020. Indicadores estadísticos básicos. 2020 []; Available from: https://digital.csic.es/handle/10261/241145. Cited 9 Oct 2022.
García-Rojas A, Gil-Prieto R, Núñez-Gallo DÁ, Matute-Cruz P, Gil-de-Miguel A. Hospitalizations realted to herpes zoster infection in the Canary Islands, Spain (2005–2014). BMC Infect Dis. 2017;17(1):586.
Morant-Talamante N, Diez-Domingo J, Martínez-Úbeda S, Puig-Barberá J, Alemán-Sánchez S, Pérez-Breva L. Herpes zoster surveillance using electronic databases in the Valencian Community (Spain). BMC Infect Dis. 2013;5(13):463.
Johnson RW, Alvarez-Pasquin MJ, Bijl M, Franco E, Gaillat J, Clara JG, et al. Herpes zoster epidemiology, management, and disease and economic burden in Europe: a multidisciplinary perspective. Ther Adv Vaccines. 2015;3(4):109–20.
Jackson LA, Reynolds MA, Harpaz R. Hospitalizations to treat herpes zoster in older adults: causes and validated rates. Clin Infect Dis. 2008;47(6):754–9.
Opstelten W, Van Essen GA, Schellevis F, Verheij TJM, Moons KGM. Gender as an independent risk factor for herpes zoster: a population-based prospective study. Ann Epidemiol. 2006;16(9):692–5.
Studahl M, Petzold M, Cassel T. Disease burden of herpes zoster in Sweden–predominance in the elderly and in women - a register based study. BMC Infect Dis. 2013;12(13):586.
Gonzalez Chiappe S, Sarazin M, Turbelin C, Lasserre A, Pelat C, Bonmarin I, et al. Herpes zoster: burden of disease in France. Vaccine. 2010;28(50):7933–8.
Muñoz-Quiles C, López-Lacort M, Díez-Domingo J, Orrico-Sánchez A. Herpes zoster risk and burden of disease in immunocompromised populations: a population-based study using health system integrated databases, 2009–2014. BMC Infect Dis. 2020;20(1):905.
Price NB, Grose C. Corticosteroids contribute to serious adverse events following live attenuated varicella vaccination and live attenuated zoster vaccination. Vaccines (Basel). 2021;9(1):23.
Weinmann S, Naleway AL, Koppolu P, Baxter R, Belongia EA, Hambidge SJ, et al. Incidence of herpes zoster among children: 2003–2014. Pediatrics. 2019;144(1): e20182917.
Matthews I, Duong M, Parsons VL, Nozad B, Qizilbash N, Patel Y, et al. Burden of disease from shingles and post-herpetic neuralgia in the over 80 year olds in the UK. PLoS ONE. 2020;15(2): e0229224.
Amirthalingam G, Andrews N, Keel P, Mullett D, Correa A, de Lusignan S, et al. Evaluation of the effect of the herpes zoster vaccination programme 3 years after its introduction in England: a population-based study. Lancet Public Health. 2018;3(2):e82-90.
Bricout H, Haugh M, Olatunde O, Prieto RG. Herpes zoster-associated mortality in Europe: a systematic review. BMC Public Health. 2015;5(15):466.
Sánchez-Trujillo L, Sanz-Anquela JM, Ortega MA. Use of the minimum basic data set as a tool for the epidemiological surveillance of mesothelioma. An Sist Sanit Navar. 2021;44(3):405–15.
Fernandez-Navarro P, Lopez-Abente G, Salido-Campos C, Sanz-Anquela JM. The minimum basic data set (MBDS) as a tool for cancer epidemiological surveillance. Eur J Intern Med. 2016;34:94–7.
Acknowledgements
The authors thank the Subdirección General del Instituto de Información Sanitaria for providing the information on which this study is based.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Medical Writing/Editorial Assistance
American Journal Experts edited this manuscript for proper use of English language. This assistance was funded by the authors.
Author Contributions
Marta Corcuera-Munguia, Ruth Gil-Prieto and Ángel Gil de Miguel conceived and designed the study; Marta Corcuera-Munguia wrote the first draft of the manuscript. Rafael García-Carretero preprocessed and analyzed the data. All the authors made substantial contributions to the interpretation of the results, critically reviewed the first draft of the manuscript, made valuable suggestions, supervised the project, and critically reviewed and edited the final draft of the manuscript. All authors read and approved the final manuscript.
Disclosures
Marta Corcuera-Munguia, Ruth Gil-Prieto, Rafael García-Carretero and Ángel Gil de Miguel have no conflicts of interest to declare.
Compliance with Ethics Guidelines
The patient information was anonymized and de-identified prior to the analysis in compliance with ethics guidelines. The study was performed in accordance with the Helsinki Declaration 1964 and its later amendments. The Rey Juan Carlos University Ethics Committee Board ruled that no formal ethics approval was required for this study.
Data Availability
The datasets analyzed during the current study are available from the corresponding author, Ruth Gil-Prieto, on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Corcuera-Munguia, M., Gil-Prieto, R., Garcia-Carretero, R. et al. Hospitalization Burden Related to Herpes Zoster Infection in Spain (2016–2019). Infect Dis Ther 12, 143–156 (2023). https://doi.org/10.1007/s40121-022-00717-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-022-00717-6