Abstract
Introduction
Hepatitis C virus (HCV) is a global public health crisis. Egypt presents the highest HCV global prevalence. Recently, three different HCV screening/testing/therapy programs were implemented: In 2014 (wave 1), major decisions on HCV therapy were enacted, accompanied by a 99% discount for the HCV therapy sofosbuvir. In 2016 (wave 2), a first testing program was launched to identify patients for free treatment. In 2018 (wave 3), population-wide screening was conducted using a WHO-prequalified finger prick rapid diagnostic test (RDT) to identify/treat all Egyptians with HCV. The financial advantages of HCV screening programs (wave 1–3 results) were estimated vs a baseline period of limited Egyptian HCV testing/therapeutic intervention (2008–2014).
Methods
Using published evidence and model-based estimates from real-world data, we evaluated the direct costs of the different HCV programs, accompanied by a conservative simulation of major HCV health consequences (i.e., liver-related deaths/life years lost) and related indirect costs. Total economic consequences of each HCV program were compared to each other and baseline from a societal perspective. Future costs and health effects were discounted by 3.5% per year.
Results
Discounted total costs (in US dollars) were $1,057 billion (baseline), $913 million (wave 1), $457 million (wave 2), and $396 million (wave 3). Discounted HCV-related life years lost were 418,000 (baseline), 377,000 (wave 1), 142,000 (wave 2), and 62,000 (wave 3). With each successive Egyptian HCV screening/testing/therapy wave, total costs and HCV-related mortality were reduced.
Conclusion
Use of the community-applied, WHO-prequalified RDT was the most dominant approach to cost-effectiveness. These results provide rationale for worldwide scalability of similar HCV elimination programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Hepatitis C virus (HCV) infection effects an estimated 71 million people worldwide, with 400,000 deaths annually. The prevalence of HCV in Egypt is the highest in the world. The cumulative cost burden of HCV in Egypt is estimated at US $89 billion for the years 2015–2030 |
As a result of this high prevalence and cost burden, treatment of HCV in Egypt since 2008 has become one of the top national priorities and the country launched various national programs intending to identify and cure Egyptian HCV-infected patients |
The goal of the present analysis—based on published epidemiological HCV data, cost and health economic modeling analyses, and findings from three different screening/testing/treatment programs—was to estimate the impact of Egypt’s national HCV screening and treatment efforts on direct, indirect, and total healthcare costs |
What was learned from the study? |
The application of a WHO-prequalified HCV diagnostic test to mass screening, together with delivery of therapy to identified patients with HCV, suggests a likely cost-effective intervention from a societal perspective, representing the dominant option compared with other HCV screening, testing, and therapy approaches in Egypt between 2008 and 2019. However, as a result of the use of real-world data, model-based analyses, and the inherent uncertainty such methodologies can result in, other advanced health economic assessments to confirm the presented conclusions are appropriate |
Introduction
Hepatitis C is a liver disease caused by the hepatitis C virus (HCV) leading to both acute and chronic hepatitis, with severity ranging from a mild illness lasting a few weeks to a serious, lifelong condition that develops into a major cause of liver cancer [1]. HCV is estimated to effect 71 million people worldwide, with 400,000 deaths annually, mostly from cirrhosis and hepatocellular carcinoma (i.e., primary liver cancer) [1]. Mortality from viral hepatitis has increased by 22% between 2000 and 2015 despite the fact that HCV can now be effectively diagnosed and treated, with direct-acting antivirals (DAA) cure rates of higher than 95% in 8–12 weeks, representing one of the most remarkable medical breakthroughs in recent time [1]. Nevertheless, many of those infected remain undiagnosed and unaware that there is a cure for this disease, with an estimated 85% of HCV-infected individuals unaware of their infection [2]. Seventy-five percent of these individuals live in low- and middle-income countries [3].
The prevalence of HCV infection in Egypt is the highest in the world [4], mostly attributed to wide community-based campaigns against schistosomiasis performed by the Egyptian Ministry of Health (MOH) from 1950 to 1980 aimed at eradicating this endemic parasitic infection [5]. However, injections with poorly sterilized non-disposable needles caused the largest ever iatrogenic spread of blood-borne infection [6]. Additionally, approximately 150,000 individuals acquire HCV infection in Egypt each year primarily through healthcare-related transmission, which is considered the primary mode of HCV transmission in Egypt [7].
In 2017, the economic burden of chronic HCV infection was characterized as tremendous [8]. Focusing on Egypt specifically, the cumulative cost burden of HCV has been estimated at US $89 billion for the years 2015–2030 [9]. As a result of this high prevalence and cost burden, since 2008, treatment of HCV in Egypt has become one of the top national priorities, for which the country launched various national programs to identify and cure Egyptian HCV-infected patients [5]. These initiatives are described in detail in the “Methods” section.
Given the highly significant clinical and economic burden of HCV, it is of major interest for healthcare decision makers to identify cost-effective programs and interventions for HCV detection and therapy. Economic evaluations are typically defined as the comparative analysis of alternative interventions in terms of both their costs and consequences [10]. The results of such evaluations serve public health policy makers and central Health Technology Assessment bodies to make better informed decisions, ensuring that limited resources are allocated as efficiently as possible to improve overall population health.
Methods
The goal of this health economic evaluation is to estimate the absolute and incremental impact of Egypt’s national HCV screening and treatment efforts on direct, indirect, and total healthcare costs. All amounts are presented in US dollars (USD). This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
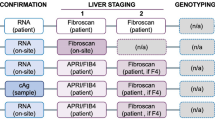
There have been several focused attempts to screen and treat HCV in Egypt: the largest, defined herein as wave 1, started in 2014; the second, defined as wave 2, was coordinated in 2016; and the third, defined as wave 3, was coordinated in 2018.
Prior to wave 1, during the period between 2008 and 2014 (defined as baseline), chronic HCV-infected patients from Egypt were served through 26 well-equipped, specialized centers all over the country for the treatment of viral hepatitis [11]. The previous standard of care therapy—combined pegylated interferon and ribavirin—were supplied for free or at reduced prices through these centers which succeeded in treating more than 350,000 patients with this therapy [11].
During wave 1 in 2014, three decisions were applied by the Egypt National Committee for Control of Viral Hepatitis (NCCVH): (1) to discontinue the use of sofosbuvir–ribavirin therapy because of its suboptimal responses; (2) that all degrees of fibrosis (F0–F4) were included in therapy without discrimination; and (3) that new guidelines for therapy include sofosbuvir/simeprevir treatment for 12 weeks (for which a 99% discount was negotiated by the Egypt Ministry of Health) [12].
In 2016, during wave 2, the Egyptian Ministry of Health began a screening program to identify patients for free treatment: 6.5 million individuals were tested for HCV antibodies, and those who tested positive were evaluated further, with 365,000 found to be viremic and treated for free [5]. Moreover, 1,635,000 Egyptian patients with known HCV were treated, supported by the simultaneous introduction of generic sofosbuvir [5].
Finally, in 2018, the Ministry of Health announced a massive screening effort, defined as wave 3, which began on October 1, 2018 [5, 13]. Its objective was to identify all individuals with HCV to be treated at the expense of the state. The screening was performed by a WHO-prequalified finger-prick-based rapid test (SD Bioline HCV, Abbott, Abbott Park, IL, USA) for individuals in outreach and rural areas (which included most of the target population), and blood-based immunoassay for screening done in hospitals and central facilities. Seropositive individuals were referred for HCV-RNA testing in 350 hospital facilities; those found to be positive were referred for evaluation and treatment in 180 specialized HCV treatment centers. By September 2019, the Ministry, through the NCCVH, expected to screen all adults aged 18 years and older in Egypt, which includes 52 million individuals after exclusion of those who have been treated or screened previously [5, 13].
Population Estimates and HCV Testing and Therapy Rates
Population estimates, and HCV testing and therapy rates, were determined on the basis of published literature [5, 11,12,13] and via local expert opinion. For each therapy wave, the total population size, HCV prevalence, population tested for HCV, population with HCV, population treated for HCV, and the treated/untreated HCV population were determined and/or calculated on the basis of given values. These epidemiologic data, presented in detail in Table 1, form the basis of the health economic assessment that is described and presented in the following section.
Health Economic Assessment
The current health economic assessment was performed to compare the cost and consequences of the different HCV programs applied in Egypt between 2008 and 2019. Published evidence was used to evaluate the direct costs of the different HCV programs (waves 1–3), accompanied by a conservative simulation of major HCV health consequences (i.e., liver-related deaths/life years lost) and the related indirect costs. The presented assessment is a model-based study that uses real-world estimates on HCV prevalence to simulate the related health economic impact using the methodological approach described below.
Direct Costs
Direct costs refer to the resource consumption in the provision of healthcare interventions. In the presented study, direct costs consist of HCV testing and therapy costs and are calculated by multiplying the population tested and the population treated (both presented in Table 1, according to therapy wave) by the related unit costs. These unit costs are presented in Table 2 by therapy wave. The testing costs are based on expert opinion and manufacturer information. The therapy costs from 2014 and later are based on published evidence [14], whereas the therapy costs before 2014 are conservatively assumed to be comparable to those from 2014.
HCV Health Consequences
As noted, a large proportion of HCV-infected individuals develop chronic HCV infection and are at risk for advanced liver fibrosis, HCV-related extrahepatic complications, cirrhosis and hepatocellular carcinoma, and liver-related death [15]. In the present health economic assessment, liver-related death—representing the most severe clinical consequence with the greatest loss of life years—was estimated on the basis of published evidence.
The liver-related death rate was estimated on the basis of data from Razavi et al. [16] that provided the number of liver-related deaths (33,000) and the total HCV-infected population (6,000,000) for the year 2013 in Egypt. On the basis of this data, a liver-related death rate of 0.55% was calculated and applied in the presented analysis for each investigated period.
The life-years lost by those liver-related deaths were estimated on the basis of data from Stanaway et al. [17], which reported 22.6 deaths per 100,000 and 609.5 life years lost per 100,000 due to HCV. This translates into an average 26.97 life years lost for each liver-related HCV death. On the basis of this data, the total liver-related deaths and liver-related life years lost were simulated for each testing/therapy wave.
Indirect Costs
Indirect costs usually refer to productivity loss resulting from increased morbidity or early mortality. In the presented health economic assessment, productivity losses due to liver-related life years lost were used to estimate the indirect costs related to each testing/therapy wave. Those costs were determined by multiplying the total liver-related life years lost by the period-specific gross domestic product (GDP) per capita in Egypt, with the following GDP per capita values applied: baseline, $2632 (2013); wave 1 (2015), $2704; wave 2 (2017), $2817; and wave 3 (2018), $2907 [18].
Analyses Settings and Perspective
For each therapy/testing wave, the total economic consequences, consisting of combined direct and indirect costs, were simulated and compared to each other from a societal perspective. In order to make the different time periods comparable, all costs and health outcomes are calculated and presented for a 1-year time-horizon. Future costs and health effects were discounted by 3.5% per year according to Egyptian health economic guidelines [19].
Results
The direct costs, consisting of HCV testing and therapy costs, range from $187 million (wave 2) to $316 million during the baseline period. Irrespective of the scenario investigated, the therapy costs were higher than the testing costs, even in wave 3, where a population-wide HCV screening of 56 million Egyptians was performed. The details for each HCV screening, testing, and therapy wave are presented in Fig. 1 in conjunction with the numbers of patients tested and treated.
Total direct costs, indirect costs, and total costs are presented in Fig. 2 for each HCV screening, testing and therapy wave. The total costs are based on combining the assessed direct and indirect costs related to HCV. Discounted total costs (in USD) were $1.057 billion (baseline), $913 million (wave 1), $457 million (wave 2), and $396 million (wave 3). These total costs were driven largely by the indirect costs, which were based on the decrease in liver-related deaths: 25,000 (baseline), 22,000 (wave 1), 8000 (wave 2), and 4000 (wave 3); and the related life years lost: 418,000 (baseline), 377,000 (wave 1), 142,000 (wave 2), and 62,000 (wave 3).
The decrease of liver-related deaths and the related life years lost is based on the increasing efforts made over time to eliminate HCV in Egypt. These are expressed by the decreasing number of untreated viremic patients with HCV: 4,480,000 (baseline), 4,037,000 (wave 1), 1,522,000 (wave 2), and 660,000 (wave 3), as presented in Table 1 and in Fig. 2.
Discussion
Overall, with each successive HCV screening, testing, and therapy wave, total costs were reduced while concurrently achieving decreasing HCV-related mortality. This methodology demonstrated increasing cost effectiveness (dominance: cost savings accompanied by positive health consequences) while also confirming progress aimed at eliminating HCV in Egypt. Notably, wave 3 was the most cost-effective of the three waves because of its reliance on the WHO-prequalified HCV diagnostic test.
Screening and treatment for HCV prevents the spread of infection and results in significant public health benefits when HCV is cured in identified patients. However, mass screening and its associated therapy is often seen as an approach that can also quickly deplete a national healthcare system’s resources.
The current assessment illustrates that the application of a WHO-prequalified HCV diagnostic mass screening test, together with subsequent therapy of identified HCV-infected patients, presents a cost-effective approach. When considering a societal perspective, this approach is more effective and less costly, and is thus the dominant option compared with other HCV screening, testing, and therapy approaches used in Egypt between 2008 and 2019. These results were achieved by avoiding negative HCV health consequences through the use of efficacious generic, direct-acting antivirals. Although the price of HCV therapy was generally quite low in Egypt (12 weeks’ sofosbuvir cost $900)—made possible by a rebate negotiated by the Egyptian Ministry of Health in 2014—the cost of therapy dropped further through the availability of generic medication alternatives in 2016 (the cost of 12-week therapy fell to $90) [14]. From a societal perspective, these reduced therapy prices made mass screening far more feasible and cost-effective; the avoided cumulative health consequences of HCV represented greater prospective cost savings than the aggregated costs of screening, testing, and therapy efforts.
Limitations
A limitation of the present health economic assessment is that it does not simulate a detailed HCV disease/transition process and related health consequences other than liver-related deaths and life years lost. This would require a more complete, sophisticated Markov modeling approach to simulate different states of HCV disease progression together with their respective health-related impact, which would further include the simulation of HCV reinfections not considered in the current model.
By doing so, additional positive effect of increased HCV screening, testing, and treatment activities could be investigated and thereby translated into further potential direct costs savings which could include therapy cost for different grades of liver fibrosis, liver cirrhosis, and/or hepatocellular carcinoma as well as indirect cost savings such as productivity associated with acute liver diseases. Potential reinfections, on the other hand, would result in a situation in which these positive influences on costs and health outcomes could not be sustained.
Consequently, the present approach is regarded as a preliminary assessment designed within a conservative framework to likely underestimate the positive health effects and reduced cost consequences of the different HCV screening, testing, and therapy waves, examining only the most severe health consequences such as liver-related death and the related life years lost. It is anticipated that the health economic consequences of the different screening, testing, and therapy waves described herein would likely be more pronounced if investigated using a more sophisticated modeling approach.
The presented analyses are also performed from a societal perspective. Consequently, it may be expected that direct non-medical costs would be included; however, as suitable non-medical cost estimates for HCV in Egypt were not available, such costs are not included. For context, however, in an HCV study from Iran, it was shown that non-medical costs reflected only about 1.3% of the direct costs [20] and hence the expected impact of the inclusion of these costs on the results would ultimately be limited.
Additionally, because the presented analysis is based on published epidemiological HCV data from Egypt, the length of the three different HCV screening/testing/therapy programs is not comparable with each other. To control the health economic results for this potential confounder, the results for each wave are presented by year, instead of for the whole time period, as stated in the “Methods” section.
As a result of this application of published and reliable epidemiologic data as the basis of the health economic assessment, potential uncertainty might be triggered because of the underlying costs and health effects applied in the modeling analyses. Since neither the underlying distributions nor the standard deviations of the underlying costs and health effects were identified, sensitivity analyses of this parameters were not performed. The rationale for this is based on the fact that any uncertainty assessment/simulation would have been based on pure assumption of the underlying data deviation, which would not add additional value to the findings. This lack of sensitivity analyses should therefore be rated as a limitation of the presented research. Therefore, other advanced health economic assessments should be performed, ideally using real-world data samples, which allow one to simulate the actual distributions of underlying input data and their influence on the health economic outcomes.
The present evaluation is based on a country-specific population, disease prevalence, and cost data which make it difficult to transfer the results to other healthcare settings geographically. The investigated HCV screening, testing, and therapy approaches also reflect the public health intervention in order to address the HCV epidemic in Egypt in particular. To transfer this approach and the related health economics findings to other country settings, an in-depth adaptation of the presented research will be necessary. Further research is therefore required to investigate the detailed health economic consequences of HCV elimination in Egypt via a more sophisticated modeling approach, in order to investigate the health economic impact of comparable public health measures in other healthcare settings around the world.
Conclusions
Hepatitis C virus remains a very serious and costly global public health crisis. With the highest country-wide prevalence of HCV in the world, Egypt presents an opportunity to estimate the absolute and incremental impact of national HCV screening efforts on direct, indirect, and total healthcare costs. The societal findings described herein illustrate a path to decreasing HCV prevalence while increasing overall program/intervention cost-effectiveness. Such results support the positive effect of HCV testing, screening, and associated treatment. This assessment further supports the application of a WHO-prequalified HCV diagnostic mass screening test with delivery of therapy to identified patients with HCV, thus representing a cost-effective/dominant option (i.e., more effective and less costly) compared with other HCV screening, testing, and therapy approaches. These findings suggest that other country-specific HCV screening and elimination/treatment interventions should likely be explored to determine to what degree the outcomes seen in Egypt serve as a model to improve societal health outcomes while reducing the economic burden of HCV in other countries around the world.
References
World Health Organization. Global hepatitis report 2017. Geneva: World Health Organization; 2017.
Thomas DL. Curing hepatitis C with pills: a step toward global control. Lancet. 2010;376(9751):1441–2.
Gower E, Estes C, Blach S, et al. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol. 2014;61(1 Suppl):S45-57.
Blach S, Zeuzem S, Manns M. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterol Hepatol. 2017;2(3):161–76.
Esmat G, El-Sayed MH, Hassany M, et al. One step closer to elimination of hepatitis C in Egypt. Lancet Gastroenterol Hepatol. 2018;3(10):665.
Frank C, Mohamed MK, Strickland GT, et al. The role of parenteral antischistosomal therapy in the spread of hepatitis C virus in Egypt. Lancet. 2000;355(9207):887–91.
Hajarizadeh B, Grebely J, Dore GJ. Epidemiology and natural history of HCV infection. Nat Rev Gastroenterol Hepatol. 2013;10(9):553–62.
Stepanova M, Younossi ZM. Economic burden of hepatitis C infection. Clin Liver Dis. 2017;21(3):579–94.
Estes C, Abdel-Kareem M, Abdel-Razek W, et al. Economic burden of hepatitis C in Egypt: the future impact of highly effective therapies. Aliment Pharmacol Ther. 2015;42(6):696–706.
Drummond MF, Sculpher MJ, Claxton K, et al. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2015.
El Kassas M, Elbaz T, Elsharkawy A, et al. HCV in Egypt, prevention, treatment and key barriers to elimination. Expert Rev Anti Infect Ther. 2018;16(4):345–50.
Gomaa A, Allam N, Elsharkawy A, et al. Hepatitis C infection in Egypt: prevalence, impact and management strategies. Hepat Med. 2017;9:17–25.
Omran D, Alboraie M, Zayed RA, et al. Towards hepatitis C virus elimination: Egyptian experience, achievements and limitations. World J Gastroenterol. 2018;24(38):4330–40.
Abozeid M, Alsebaey A, Abdelsameea E, et al. High efficacy of generic and brand direct acting antivirals in treatment of chronic hepatitis C. Int J Infect Dis. 2018;75:109–14.
Chen SL, Morgan TR. The natural history of hepatitis C virus (HCV) infection. Int J Med Sci. 2006;3(2):47–52.
Razavi H, Waked I, Sarrazin C, et al. The present and future disease burden of hepatitis C virus (HCV) infection with today’s treatment paradigm. J Viral Hepat. 2014;21(Suppl 1):34–59.
Stanaway JD, Flaxman AD, Naghavi M, et al. The global burden of viral hepatitis from 1990 to 2013: findings from the Global Burden of Disease Study 2013. Lancet. 2016;388(10049):1081–8.
Trading Economics/World Bank. Egypt GDP per capita. https://tradingeconomics.com/egypt/gdp-per-capita. Accessed 16 June 2020.
Elsisi GH, Kalo Z, Eldessouki R, et al. Recommendations for reporting pharmacoeconomic evaluations in Egypt. Value Health Reg Issues. 2013;2(2):319–27.
Mohammadzadeh M, Derafshi H, Ghari T. The estimation of economic burden of hepatitis C virus infection in Iran. Iran J Public Health. 2018;47(10):1575–82.
Acknowledgements
Funding
Funding for this health economic assessment, manuscript and publication fees were provided by Abbott Laboratories, USA.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Suela Sulo and Bjoern Schwander. The first draft of the manuscript was written by Bjoern Schwander, Josh Feldstein and Suela Sulo. All authors commented on ongoing versions of the manuscript. All authors read and approved the final manuscript.
Prior Presentation
Preliminary results from this study were presented at the ISPOR Europe 2019 Conference in Copenhagen, Denmark, 6–9 November 2019.
Disclosures
Bjoern Schwander and Josh Feldstein report grants from Abbott, USA, during the conduct of the study. Suela Sulo and Luis Gonzalez are employees and stockholders of Abbott, USA. Mohamed Hassany and Galal ElShishiney have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Schwander, B., Feldstein, J., Sulo, S. et al. Pursuing Elimination of Hepatitis C in Egypt: Cost-Effectiveness and Economic Evaluation of a Country-Wide Program. Infect Dis Ther 11, 1193–1203 (2022). https://doi.org/10.1007/s40121-022-00631-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-022-00631-x