Abstract
Limited data are available for ceftazidime–avibactam (CZA) dosing in patients receiving renal replacement therapy, especially the data on the dosing in patients receiving intermittent hemodialysis (IHD). In this report, we firstly described a case in which CZA was administered as 2.5 g after each time of IHD, and a dose of 1.25 g was added on the 48th-hour for the 72-h interdialytic interval. Plasma concentrations of CZA measured at different time indicated that > 50% of administered ceftazidime and avibactam were removed during the 4-h hemodialysis. In addition, we described another case on continuous venovenous hemodialysis (CVVHD), in which CZA was administered as 2.5 g q12h in 2-h infusions. The dose regimen for these two cases could achieve trough concentration of ceftazidime higher than fourfold of the MIC and trough concentration of avibactam higher than the threshold of 1 μg/mL during the treatment, and exert efficient antimicrobial effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The dose recommendation and validation of ceftazidime–avibactam (CZA) is limited in patients receiving renal replacement therapy, especially there is no data in intermittent hemodialysis (IHD) patients. |
This is the first case report on exposure of CZA in IHD patient, in which CZA was administered as 2.5 g (2 g ceftazidime and 0.5 g avibactam) after each time of IHD, and a dose of 1.25 g was added on the 48th-hour for 72-h interdialytic interval. The dose regimen in this case could achieve the joint pharmacokinetic/pharmacodynamic (PK/PD) targets for CZA and alleviate the peritoneal dialysis-associated peritonitis caused by Klebsiella pneumoniae. |
We reported another case that CZA administered as 2.5 g q12h in 2-h infusions could adequately achieve the joint PK/PD targets in the patient on continuous venovenous hemodialysis (CVVHD), and alleviated the pneumonia caused by carbapenem-resistant Klebsiella pneumoniae. |
Introduction
Ceftazidime–avibactam (CZA) is a novel β-lactam/β-lactamase inhibitor combination (ceftazidime: avibactam = 4:1) for the treatment of serious infections caused by resistant Gram-negative pathogens [1, 2]. In patients with renal insufficiency, dosage adjustments based on renal function are needed according to the label approved by FDA [2]. However, the dose regimen for patients with renal replacement therapy is absent in the label inserts.
Research data for CZA dosing in patients undergoing renal replacement therapy are limited to two cases, and both are focused on continuous renal replacement therapy (CRRT) [3, 4]. One of the cases reported by Wenzler et al. [3] who used the dose regimen of 1.25 g q8h for a patient with continuous venovenous hemofiltration (CVVHF), while another case reported by Soukup et al. [4] who used a more aggressive dose regimen of 2.5 g q8h for a patient with continuous venovenous hemodiafiltration (CVVHDF). Both two cases could achieve the joint pharmacokinetic/pharmacodynamic (PK/PD) target of CZA throughout the treatment. However, the case reported by Wenzler et al. [3] had persistent bacteremia 5 days after CZA initiation and was eventually succumbed to the infection. Another case reported by Soukup et al. [4] had the trough concentration of ceftazidime as high as 70 μg/mL. In addition, although the label of CZA recommend the dose of 940 mg (ceftazidime 750 mg and avibactam 190 mg) every 48 h given post-hemodialysis for patients with end-stage renal disease (ESRD) on intermittent hemodialysis (IHD) [2], the validation of the recommended dosage by the label inserts has not been reported.
Despite the growing use of RRT in critically ill patient, the lack of PK/PD data during RRT nowadays limits evidence-based dosing recommendations for novel antibiotics. It has been reported that CRRT was an independent risk factor for ceftazidime–avibactam treatment failures and development of resistance with carbapenem-resistance Enterobacteriaceae infections [5]. In general, real-world data are needed to guide appropriate dosing in patients with renal replacement therapy. Here, we reported two clinical cases receiving CZA treatment, (1) a patient with peritoneal dialysis-associated peritonitis on IHD and (2) a patient with pulmonary infection on continuous venovenous hemodialysis (CVVHD).
Methods
Serial blood samples were collected from peripheral vein into a red-top collection tube which containing no preservatives or anticoagulants, and were immediately sent for analysis after sampling. In case one, trough concentration was collected 30 min before the initiation of CZA dosing, while peak concentration was collected 30 min after finishing CZA infusion. Meanwhile, the concentrations 30 min before and after IHD were collected. In case two, serial blood samples were collected before the CZA infusion and 3, 5, 12 h after starting 2-h CZA infusion. The quantification of concentration of ceftazidime and avibactam was performed using a validated high performance liquid chromatography–tandem mass spectrometry (LC–MS/MS) assay [6]. The calibration ranges for ceftazidime and avibactam were 0.1–200 μg/mL and 0.1–100 μg/mL respectively. The method validations including calibration curve, selectivity, accuracy, precision, matrix effect, recovery, and stability met the requirement of FDA principles. The pharmacokinetics parameters for both ceftazidime and avibactam were estimated using a noncompartmental analysis (WinNonlin Version 7.0). This study was conducted following the legal requirements and the Declaration of Helsinki and its subsequent amendments. The informed consent for publication of the clinical data were obtained. The basic characteristics of cases were listed in Table 1.
Case One
A 75-year-old female patient was diagnosed with ESRD and started on continuous ambulatory peritoneal dialysis (CAPD, 2 L dialysate × 4 cycles with 10–12 h dwell time at night) since 6 years ago. She was presented with 2 days of intermittent abdominal pain accompanied by fever and diarrhea, while the peritoneal dialysis (PD) fluid was cloudy when performing CAPD at home. Peritoneal dialysis-associated peritonitis was then diagnosed. The patient was initially treated with cefazoline (0.5 g added into 2 L dialysate i.p. qid) contaminant with amikacin (0.02 g added into 2 L dialysate i.p. qid).
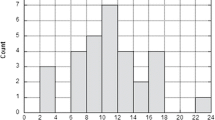
On day 3, the PD fluid culture reported Klebsiella pneumoniae with positive extended-spectrum β-lactamase (Table 2), the antimicrobial treatment was then changed to imipenem and cilastatin sodium (0.5 g added into 2 L dialysate i.p. qid) and levofloxacin (0.5 g po qod). Although the fever and diarrhea were alleviated, the patient was still suffering abdominal pain. On day 7, the blood culture collected at onset of infections reported negative inbacteria growth. On day 14, considering the infection might be derived from the PD catheter, the PD catheter was then removed, and the patient was started on IHD therapy. The schedule of the patient receiving 4-h IHD was on Monday, Wednesday, and Friday per week. Imipenem and cilastatin sodium was administered intravenously of 1 g every 12 h. On day 16, the patient developed a high fever with a temperature higher than 39 °C, and the abdominal pain was not alleviated. Laboratory tests showed a serum procalcitonin (PCT) of 1.26 ng/mL and a C-reactive protein (CRP) of > 90 mg/L. In addition, the culture of PD fluid collected before removing the catheter still reported the Klebsiella pneumoniae, and the reported results were same as before. While the cultures of blood samples collected on day 10 reported no bacteria growth. On day 18 (Friday), the antimicrobial treatment was changed to CZA contaminant with metronidazole. The dose regimen of CZA was 2.5 g administered after each time of IHD (Gambro AK 96, blood flow of 260 mL/min, and dialysate flow of 500 mL/min), while a second dose of 1.25 g was added on Sunday per week. The concentration of ceftazidime and avibactam was monitored between day 27 (Sunday) and day 30 (Wednesday) (Fig. 1). After being treated with CZA for 5 days, the patient’s abdominal pain and fever were gradually alleviated. No adverse events of CZA were observed during the CZA treatment.
Ceftazidime–avibactam plasma concentrations after the first dose. The dose regimen of CZA was 2.5 g administered after each time of IHD, while a second dose of 1.25 g was added on the 48th-hour for the 72-h interdialytic interval. Solid line: Ceftazidime serum levels (μg/mL). Dashed line: Avibactam serum levels (μg/mL)
Case Two
An 82-year-old male patient with a history of resection of malignant thyroid tumor was diagnosed with neck metastasis and laryngeal stenosis. The total laryngectomy was performed, and the patient was then discharged with normal body temperature. However, a few weeks later, the patient developed a high fever with temperature higher than 39 °C, accompanied with cough and dyspnea and readmitted to the local hospital. The chest computed tomography (CT) suggested pulmonary infection. Imipenem and cilastatin sodium, and vancomycin were given for initially antimicrobial therapy, but the patient was still presented with a repeated low fever. After treating for 16 days in the local hospital, he was then transferred to our hospital for further treatment.
After admission, the chest CT showed scattered inflammatory lesions and pleural effusion on both sides of the lungs. The laboratory test showed white blood cell counts (WBC) of 63.34 × 109/L, CRP of 67.10 mg/L, PCT of 9.750 ng/mL. Thus, intrathoracic drainage catheter insertion was performed, imipenem and cilastatin sodium (1 g ivgtt q8h) was initially used. On the third day since his admission to our hospital, the patient developed irritability, which was considered to be caused by imipenem and cilastatin sodium, as it was the only drug in use which meets the probable grade of the Naranjo criteria for adverse drug reactions. Meanwhile, the oxygen saturation and blood pressure were decreased, the drainage of pleural fluid was cloudy, and the WBC, CRP, PCT levels were further increased. On day 4, the pleural fluid cultures and sputum cultures reported the same carbapenem-resistant Klebsiella pneumoniae (CRKP) (Table 2), the blood sample culture reported negative in bacteria growth. In the meantime, the patient developed anuric renal failure, necessitating the initiation of CRRT. The patient was started on CZA 2.5 g every 12 h in 2-h infusions while on CRRT via a Gambro AK 200 hemodialysis machine (Baxter Healthcare) with a 1.5 m2 polyethersulfone membrane filter. After three doses of CZA, the plasma concentration of CZA during CVVHD throughout the entire 12-h dosing interval was continuously detected (Fig. 2), which indicated the current dose of CZA could achieve the joint PK/PD target of CZA. The pharmacokinetics parameters of ceftazidime and avibactam were presented in Table 3. On the day when plasma samples were collected, the CVVHD parameters were set as following that the blood flow was 200 mL/min, the dialysate flow was 2000 mL/h. Besides, his daily urine volume was 30 mL, indicating that the patient had little residual renal function to remove CZA. There were no interruptions in CVVHD during the 4th dose of CZA. After being treated with CZA for 5 days, the body temperature decreased to around 37 °C, and the WBC, CRP and PCT levels were also decreased, indicating the infection was alleviated. The blood cultures collected at different timepoints during the therapy reported negative in bacteria growth. However, the patient developed coagulation disorder due to the advanced thyroid tumor, leading to disseminated intravascular coagulation and eventually died.
Discussion
A recent report described that RRT was independently associated with CZA clinical failure [5]. However, there are no data on CZA dosing in patients on IHD, and only two recent studies reported CZA concentrations in patients on CRRT [3, 4]. To our knowledge, this was the first report on efficacy and pharmacodynamic target attainment of CZA in patients on IHD or CRRT.
A joint PK/PD target for CZA is defined as simultaneous achievement of 50% time during each dosing interval that free plasma concentrations exceed CZA minimal inhibitory concentration for ceftazidime (50% fT > MIC), and 50% fT above a threshold concentration (CT) of 1 μg/mL for avibactam (50% fT > 1 μg/mL) [7]. 50% fT > MIC is an established PK/PD target for ceftazidime and other cephalosporins, and a target of 8 μg/mL was chosen based on global surveillance studies where a CZA MIC of < 8 μg/mL was observed to include ≥ 90% of clinical isolates of Enterobacteriaceae and P. aeruginosa [8,9,10,11,12]. Moreover, some experts supported a target of 100% fT > fourfold MIC for ceftazidime to maximize efficacy and minimize the potential of drug resistance in critically ill patients [13].
In case one, considering the severity of illness of the patient, the dose of CZA used was extrapolated from the dosing recommendations by label inserts. CZA was administered as 2.5 g after each time of IHD, and a dose of 1.25 g was added on the day with 72-h interdialytic interval. As shown in Fig. 1, > 50% of administered ceftazidime and avibactam were removed during the 4-h hemodialysis, which was in accordance with the study reported by Merdjan et al., who found that > 50% of the administered avibactam was removed during a 4-h hemodialysis session [14]. As shown in Fig. 1, the 48-h interval without hemodialysis decreased nearly 50% of plasma concentration of CZA. Besides, the estimated glomerular filtration rate (eGFR) was 12.1 mL/min on the day before hemodialysis, demonstrating that her intrinsic renal function could remove part of CZA. What’s more, except for the short session at the end of 4-h IHD, the current dose regimen could achieve the trough concentration of ceftazidime higher than fourfold of the MIC threshold (8 μg/mL) of CZA and the trough concentration of avibactam higher than the 1 μg/mL threshold during the treatment. Taken together, the dose regimen used in case one could achieve the joint PK/PD target for CZA. It was noted that the peak concentration of CZA at third dose was much lower than that of the fourth dose. As the blood samples collected for case one were not continuous, the peak concentration was defined as the concentration of blood sample collected 30 min after finishing CZA infusion. However, the timepoint of collecting peak concentration might not reach to the timepoint of the max concentration because of the incomplete drug distribution, which led to lower value of peak concentration at third dose. Thus, the possible reason for these two different peak concentrations might be the inter-individual difference in the time needed for completing drug distribution. Another limitation caused by the discontinuous sample collection scheme is that it leads to incapable to calculate PK parameters.
Limited data are available for CZA dosing during CRRT. To our knowledge, clearance of CZA in patients receiving CRRT has not been evaluated in a large, prospective fashion, and CRRT may impact antibiotic dosing through a range of variables including volume of distribution dynamics, flow of dialysis fluid, replacement fluid infusion site, and type and surface of the used membrane. Only two cases reported the pharmacokinetics of CZA during CRRT [3, 4]. Wenzler et al. [3] found that the CVVHF accounted for 57.1% of total clearance of ceftazidime and 54.3% of the total clearance of avibactam. Both cases could achieve concentrations with 100% T > fourfold MIC over the dosing interval for ceftazidime and 100% fT > 1 μg/mL for avibactam in the patients on CRRT. In our case two patient, using a noncompartmental analysis, the pharmacokinetic parameters of ceftazidime and avibactam were shown in Table 3. In addition, the concentration data showed that dose regimen of 2.5 g q12h could achieve the same PK/PD target throughout the 12-h dosing interval. Given that antibiotic therapy cannot be guided by a clinical endpoint (measurable marker of effectiveness) in a timely manner, achievement of PK/PD target provides the clinician with an appropriate target to guide antibiotic dosing.
Despite achieving target plasma PK/PD endpoint with current dose regimens in these two cases, the concentrations of CZA in dialysate and post-filtration were not collected in these two cases. Thereby, the estimations of removal of ceftazidime and avibactam by RRT, such as extraction ratio, clearance by RRT were not calculated. Based on these two case reports and the available evidence, the off-label dose regimens for patient on IHD received CZA of 2.5 g administered after each time of IHD, while a second dose of 1.25 g was added on the 48th-hour for the 72-h interdialytic interval, while patient on CVVHD received CZA of 2.5 g q12h could achieve the PK/PD target and exert efficient antimicrobial effect. Additional studies are still required to evaluate CZA PK alteration in distinct dialysis modalities in multiple patients to verify the optimal dosing strategy of CZA.
Change history
05 November 2022
A Correction to this paper has been published: https://doi.org/10.1007/s40121-022-00675-z
References
Das S, Li J, Riccobene T, Carrothers TJ, Newell P, Melnick D, et al. Dose selection and validation for ceftazidime–avibactam in adults with complicated intra-abdominal infections, complicated urinary tract infections, and nosocomial pneumonia. Antimicrob Agents Chemother. 2019;63(4):e02187-e2218. https://doi.org/10.1128/AAC.02187-18.
Anonymous. 5 December 2014. Food and Drug Administration AntiInfective Drugs Advisory Committee Meeting. Ceftazidime–avibactam for injection for treatment of complicated intra-abdominal infection (used in combination with metronidazole), complicated urinary tract infection including acute pyelonephritis, and limited use indication: aerobic Gram-negative infections with limited treatment options. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/Anti-InfectiveDrugsAdvisoryCommittee/UCM425459.pdf. Accessed 25 Nov 2021.
Wenzler E, Bunnell KL, Bleasdale SC, Benken S, Danziger LH, Rodvold KA. Pharmacokinetics and dialytic clearance of ceftazidime–avibactam in a critically ill patient on continuous venovenous hemofiltration. Antimicrob Agents Chemother. 2017;1:e00464-e517. https://doi.org/10.1128/AAC.00464-17.
Soukup P, Faust AC, Edpuganti V, Putnam WC, McKinnell JA. Steady-state ceftazidime–avibactam serum concentrations and dosing recommendations in a critically ill patient being treated for pseudomonas aeruginosa pneumonia and undergoing continuous venovenous hemodiafiltration. Pharmacotherapy. 2019;39:1216–22. https://doi.org/10.1002/phar.2338.
Shields RK, Nguyen MH, Chen L, Press EG, Kreiswirth BN, Clancy CJ. Pneumonia and renal replacement therapy are risk factors for ceftazidime–avibactam treatment failures and resistance among patients with carbapenem-resistant enterobacteriaceae infections. Antimicrob Agents Chemother. 2018;62:e02497-e2517. https://doi.org/10.1128/AAC.02497-17.
Sillén H, Mitchell R, Sleigh R, et al. Determination of avibactam and ceftazidime in human plasma samples by LC–MS. Bioanalysis. 2015;7(12):1423–34. https://doi.org/10.4155/bio.15.76.
Li J, Lovern M, Green ML, Chiu J, Zhou D, Comisar C, et al. Ceftazidime–avibactam population pharmacokinetic modeling and pharmacodynamic target attainment across adult indications and patient subgroups. Clin Transl Sci. 2019;12:151–63. https://doi.org/10.1111/cts.12585.
Castanheira M, Farrell SE, Krause KM, Jones RN, Sader HS. Contemporary diversity of β-lactamases among Enterobacteriaceae in the nine US census regions and ceftazidime–avibactam activity tested against isolates producing the most prevalent β-lactamase groups. Antimicrob Agents Chemother. 2014;58:833–8. https://doi.org/10.1128/AAC.01896-13.
Flamm RK, Stone GG, Sader HS, Jones RN, Nichols WW. Avibactam reverts the ceftazidime MIC90 of European Gram-negative bacterial clinical isolates to the epidemiological cut-off value. J Chemother. 2014;26:333–8. https://doi.org/10.1179/1973947813Y.0000000145.
Levasseur P, Girard AM, Claudon M, Goossens H, Black MT, Coleman K, et al. In vitro antibacterial activity of the ceftazidime-avibactam (NXL104) combination against Pseudomonas aeruginosa clinical isolates. Antimicrob Agents Chemother. 2012;56:1606–8. https://doi.org/10.1128/AAC.06064-11.
Nichols WW, de Jonge BL, Kazmierczak KM, Karlowsky JA, Sahm DF. In vitro susceptibility of global surveillance isolates of pseudomonas aeruginosa to ceftazidime–avibactam (INFORM 2012 to 2014). Antimicrob Agents Chemother. 2016;60:4743–9. https://doi.org/10.1128/AAC.00220-16.
Sader HS, Castanheira M, Flamm RK, Farrell DJ, Jones RN. Antimicrobial activity of ceftazidime–avibactam against Gram-negative organisms collected from US medical centers in 2012. Antimicrob Agents Chemother. 2014;58:1684–92. https://doi.org/10.1128/AAC.02429-13.
Delattre IK, Taccone FS, Jacobs F, Hites M, Dugernier T, Spapen H, et al. Optimizing β-lactams treatment in critically-ill patients using pharmacokinetics/pharmacodynamics targets: are first conventional doses effective? Expert Rev Anti Infect Ther. 2017;15:677–88. https://doi.org/10.1080/14787210.2017.1338139.
Merdjan H, Tarral A, Das S, Li J. Phase 1 study assessing the pharmacokinetic profile and safety of avibactam in patients with renal impairment. J Clin Pharmacol. 2017;57(2):211–8. https://doi.org/10.1002/jcph.793.
Acknowledgements
We would like to express our sincere gratitude towards the participants of the study.
Funding
This work was supported by grants from the Natural Science Foundation of Wenzhou (Y20211019 to C.R.T.). The journal's Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author contributions
X.B.Y., and C.H.Z. conceptualized and planned the work that led to the manuscript. Y.Z.W., F.M.X., J.H.Y. and J.C. collected and analyzed the data, X.S.Z., D.W.S. and G.Y.L. drafted the manuscript. C.R.T, drafted the revised manuscript and replenished the data. The final submitted version of manuscript was reviewed and approved by all the authors.
Disclosures
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Xiao-Shan Zhang, Yu-Zhen Wang, Da-Wei Shi, Fang-Min Xu, Jun-Hui Yu, Jie Chen, Guan-Yang Lin, Chun-Hong Zhang, Cong-Rong Tang and Xuben Yu all have nothing to disclose.
Compliance with ethics guidelines
This study was conducted following the legal requirements and the Declaration of Helsinki and its subsequent amendments. The informed consent for publication of the clinical data was obtained.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original article was revised due to an addition of an corresponding author to the article.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhang, XS., Wang, YZ., Shi, DW. et al. Efficacy and Pharmacodynamic Target Attainment for Ceftazidime–Avibactam Off-Label Dose Regimens in Patients with Continuous or Intermittent Venovenous Hemodialysis: Two Case Reports. Infect Dis Ther 11, 2311–2319 (2022). https://doi.org/10.1007/s40121-022-00621-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-022-00621-z