Abstract
Introduction
Estimating the risk of disease progression is of utmost importance for planning appropriate setting of care and treatment for patients with coronavirus disease 2019 (COVID-19). This study aimed to develop and validate a novel prediction model of COVID-19 progression.
Methods
In total, 814 patients in the training set were included to develop a novel scoring system; and 420 patients in the validation set were included to validate the model.
Results
A prediction score, called ACCCDL, was developed on the basis of six risk factors associated with COVID-19 progression: age, comorbidity, CD4+ T cell count, C-reactive protein (CRP), D-dimer, and lactate dehydrogenase (LDH). For predicting COVID-19 progression, the ACCCDL score yielded a significantly higher area under the receiver operating characteristic curve (AUROC) compared with the CALL score, CoLACD score, PH-COVID-19 score, neutrophil–lymphocyte ratio, and lymphocyte–monocyte ratio both in the training set (0.92, 0.84, 0.83, 0.83, 0.76, and 0.65, respectively) and in the validation set (0.97, 0.83, 0.83, 0.78, 0.74, and 0.60, respectively). Over 99% of patients with the ACCCDL score < 12 points will not progress to severe cases, and over 30% of patients with the ACCCDL score > 20 points will progress to severe cases.
Conclusion
The ACCCDL score could stratify patients with at risk of COVID-19 progression, and was useful in regulating the large flow of patients with COVID-19 between primary health care and tertiary centers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
We developed a novel prediction model of COVID-19 progression, called the ACCCDL score, based on six variables (age, comorbidity, CD4+ T cell count, CRP, D-dimer, and LDH). |
The ACCCDL score yielded a higher predictive performance compared with previous reported prediction models including the CALL score, CoLACD score, PH-COVID-19 score, neutrophil–lymphocyte ratio, and lymphocyte–monocyte ratio. |
Over 99% of patients with the ACCCDL score ≤ 12 points will not progress to severe cases, and can be managed at primary health care centers. Over 30% of patients with the ACCCDL score > 20 points will progress to severe cases, and can benefit from early transfer to tertiary centers. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.14602290.
Introduction
Since November 2019, the outbreak of the novel coronavirus disease (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has influenced almost all countries and regions. Evidence of human-to-human transmission has been reported among close contacts of patients with COVID-19 [1]. Although considerable efforts have been made to reduce transmission, the overall upward trend of COVID-19 is continuing around the world. As of 26 January 2021, the outbreak of COVID-19 brings the cumulative numbers to over 98 million reported cases and over 2.1 million deaths globally [2].
The COVID-19 pandemic not only affected the economic development throughout the world but also forced people to strongly modify their daily routines, putting a significant strain on the social aspects of daily life. Diminished volumes of habitual physical activity and increased sedentary levels have been observed as a result of COVID-19 home confinement [3]. A worldwide multicenter study elucidates the risk of psychosocial strain during the early COVID-19 home confinement period in 2020 [4]. The results of the ECLB-COVID19 international online survey also show that isolation alters physical activity and eating behaviors in a health-compromising direction [5]. Consequences of inactivity, including a higher mortality rate and poorer general health and fitness, have been reported. In order to mitigate the negative psychosocial effects of home confinement, implementation of national strategies focused on promoting social inclusion through a technology-based solution is strongly suggested [4]. The insight from the ECLB-COVID19 multicenter study provides a clear remit for the urgent implementation of technology-based intervention to foster an Active and Healthy Confinement Lifestyle [6]. Souissi et al. also suggest combining video feedback with pedagogical activity during the pandemic-induced online coaching or physical education to improve movement learning in school-aged children [7].
The prevalence of severe cases has been reported in patients with COVID-19 [8, 9]. Richardson et al. included 5700 patients hospitalized with COVID-19 in New York, and reported that 373 patients (14.2%) were severe cases that required treatment in the intensive care unit (ICU) [8]. In a report of 72,314 cases in China, 14% were severe cases that required ventilation in the ICU [9]. The risk factors of COVID-19 progression have been reported, and broadly include older age [10], comorbidity [11], C-reactive protein (CRP) [12], CD4+ T cell count [13], D-dimer, lactate dehydrogenase (LDH) [14], leukocyte count, lymphocyte count, procalcitonin, and so on [15]. Prediction models, which combine multiple risk factors to estimate the risk of COVID-19 progression, could help physicians to decide which patients can be treated at primary health care centers and who needs transfer to tertiary centers. Some prediction models for early identification of patients with risk of COVID-19 progression have been reported in previous studies [16,17,18,19,20,21]. However, most of the existing prediction models lack validation, are inadequately reported, or are at high risk of bias. Thus, it is not a surprise to see different results from different models. Few existing prediction models have the potential to be extensively used by healthcare providers.
Before performing this study, we proposed some hypotheses. First, besides previously reported predictors, there are some other novel predictors which are associated with COVID-19 progression. Second, including novel predictors might further improve the sensitivity and specificity of previously reported prediction models. Third, it is possible to develop a novel prediction model of COVID-19 progression, which is superior to previously reported prediction models. In this cohort of 1234 patients with COVID-19, we aimed to (1) develop and validate a novel prediction model of COVID-19 progression; (2) validate previously reported prediction models, including the CALL score [16], CoLACD score [17], PH-COVID-19 score [18], neutrophil–lymphocyte ratio [19], and lymphocyte–monocyte ratio [20, 21].
Methods
Study Population
In this retrospective study, 1332 consecutive patients with COVID-19 admitted to Shanghai Public Health Clinical Center between January 20, 2020 and November 30, 2020 were analyzed. Shanghai Public Health Clinical Center is a tertiary teaching hospital in Shanghai, China. Exclusion criteria: (1) patients requiring immediate ICU admission at hospital admission (n = 15); (2) patients who did not yet have a definite outcome, i.e., who were still being treated at the time of analysis (n = 83). Finally, 1234 non-severe patients with COVID-19 at hospital admission were enrolled. The 814 patients admitted to hospital between January 20, 2020 and August 31, 2020 constituted the training set, and 420 patients admitted to hospital between September 1, 2020 and November 30, 2020 constituted the validation set.
The study was approved by the Clinical Research Ethics Committee of Shanghai Public Health Clinical Center (No. 2021-S013-01). In our hospital, patients with COVID-19 were insulated in negative pressure isolation rooms. As researchers, we could not obtain the chance of physical contact with patients with COVID-19. Therefore, at hospital admission, patients provided verbal consent for their clinical data to be used for medical study using voice or video calls. The procedures were in accordance with the ethical standards of the Helsinki Declaration (1964, amended most recently in 2008) of the World Medical Association.
Diagnostic Criteria
Patients with COVID-19 were confirmed by the positive results of SARS-CoV-2 nucleotide tests in the nasopharyngeal or throat swab specimens using the real-time reverse transcription polymerase chain reaction (RT-PCR) method. Severe COVID-19 cases were diagnosed using at least one of the following standards: (1) respiratory frequency ≥ 30 breath/min; (2) resting oxygen saturation ≤ 93%; (3) oxygenation index ≤ 300 mmHg; (4) mechanical ventilation; (5) shock; (6) other organ failures and ICU admission.
Data Collection
Demographic and clinical data including age, sex, body mass index (BMI), comorbidity, epidemiological history, clinical manifestation, vital signs, laboratory parameters, and clinical outcomes were collected from the electronic medical records of Shanghai Public Health Clinical Center. In our hospital, the laboratory parameters of patients with COVID-19 were centralized in the intensive testing laboratory which is specialized for patients with COVID-19.
Calculation of Previously Reported Prediction Models of COVID-19 Progression
-
1.
The CALL score was calculated using four clinical factors [16]: comorbidity (without, 1 point; with, 4 points); age (≤ 60 years, 1 point; > 60 years, 3 points); lymphocyte count (> 1.0 × 109/L, 1 point; ≤ 1.0 × 109/L, 3 points); LDH (≤ 250 U/L, 1 point; 250–500 U/L, 2 points; > 500 U/L, 3 points).
-
2.
The CoLACD score was calculated using four clinical factors [17]: COVID-19 lymphocyte ratio (≥ 17.6%, 0 points; < 17.6%, 1 point); age (< 50, 0 points; 50–65, 1 point; ≥ 65, 2 points); CCI score (< 3, 0 points; ≥ 3, 1 point); dyspnea (without, 0 points; with, 1 point).
-
3.
The PH-COVID-19 score was calculated using eight predictors [18]: age (< 20, − 2 points; 20–29, 0 points; 30–39, 2 points; 40–49, 4 points; 50–59, 6 points; 60–69, 8 points; 70–79, 10 points; 80–89, 12 points; 90–99, 14 points; > 99, 15 points); sex (female, 0 points; male, 2 points); diabetes (without, 0 points; with, 2 points); chronic obstructive pulmonary disease (without, 0 points; with, 1 point); immunosuppression (without, 0 points; with, 1 point); hypertension (without, 0 points; with, 1 point); obesity (without, 0 points; with, 1 point); chronic kidney disease (without, 0 points; with, 2 points).
-
4.
The neutrophil–lymphocyte ratio (NLR) = neutrophil count/lymphocyte count [19].
-
5.
The lymphocyte–monocyte ratio (LMR) = lymphocyte count/monocyte count [20].
Statistical Analysis
Normally distributed data, non-normal distribution data, and categorical data are presented as mean ± standard deviation, median (interquartile range, IQR), and frequency, respectively. The statistical differences were compared using the Student’s t test for normally distributed data, the non-parametric Mann–Whitney test for non-normal distribution data, and the chi-square test for categorical data. The significance of each variable was assessed using univariate and multivariate Cox proportional hazards model for identifying the independent risk factors of COVID-19 progression. All the variables at a statistically significant level after multivariate Cox analysis were candidates for formulation of a novel scoring model, and their relevant points were determined by the hazard ratio (HR) values to reflect their weights of impact on COVID-19 progression. The predictive performances of the scoring models were assessed using receiver operating characteristic (ROC) curves and areas under the ROC curves (AUROCs). The Delong test was used to compare the areas under two or more correlated ROC curves [22]. Two sets of cutoffs were calculated: (1) maximizing the Youden index (sensitivity + specificity − 1); (2) obtaining a specificity of at least 95%. All significance tests were two-tailed, and p < 0.05 was considered statistically significant. The statistical analyses were performed using the SPSS software, version 15.0 (SPSS Inc. Chicago, Illinois, USA), the MedCalc software, version 16.1 (MedCalc Software bvba, Ostend, Belgium), and the R software, version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Clinical Characteristics of Patients on Hospital Admission in the Training Set
Clinical characteristics of patients on hospital admission in the training set are shown in Table 1. The median age was 36 years (IQR 25–51), 110 (13.5%) were older than 60 years, 468 (57.5%) were male, 225 (27.6%) had obesity, and 146 (17.9%) had at least one comorbidity. The median white blood count (WBC), lymphocyte count, CD4+ T cell count, LDH, CRP, D-dimer, procalcitonin, and erythrocyte sedimentation rate (ESR) levels were 5.5 × 109/L (IQR 4.3–6.8), 1.5 × 109/L (IQR 1.1–1.9), 577 cells/µL (IQR 408–771), 201 U/L (IQR 178–234), 0.5 mg/L (IQR 0.5–7.0), 0.3 ng/mL (IQR 0.2–0.5), 0.03 µg/L (IQR 0.02–0.10), and 30 mm/h (IQR 10–74), respectively. The 814 patients in the training set were divided into progressive group (n = 18, 2.2%) and stable group (n = 796, 97.8%) based on whether they progressed to severe cases during the hospitalization. Age, obesity, comorbidity, lymphocyte count, CD4+ T cell count, LDH, CRP, D-dimer, procalcitonin, and ESR were significantly different between progressive group and stable group (p < 0.05) (Table 1).
Independent Risk Factors Associated with COVID-19 Progression
The independent risk factors associated with COVID-19 progression are shown in Table 2. Multivariate Cox proportional hazards analysis showed that age > 60 years (HR 6.3, 95% CI 2.1–29.4, p < 0.001), comorbidity (1 comorbidity, HR 4.0, 95% CI 1.4–16.9, p = 0.002; ≥ 2 comorbidities, HR 6.2, 95% CI 1.9–26.8, p < 0.001), CD4+ T cell count ≤ 410 cells/µL (HR 3.2, 95% CI 1.5–11.8, p = 0.025), LDH > 250 U/L (HR 4.0, 95% CI 1.7–19.8, p = 0.007), CRP > 10 mg/L (HR 3.1, 95% CI 1.2–10.5, p = 0.034), and D-dimer (HR 2.9, 95% CI 1.0–9.7, p = 0.042) were the independent risk factors associated with COVID-19 progression.
Construction of a Novel Prediction Model of COVID-19 Progression
On the basis of the HR values of multivariate Cox analysis, we assign 6 points to age (≤ 60 years, 1 point; > 60 years, 6 points), 6 points to comorbidity (absence of comorbidity, 1 point; 1 comorbidity, 4 points; ≥ 2 comorbidities, 6 points), 4 points to LDH (≤ 250 U/L, 1 point; > 250 U/L, 4 points), and 3 points to CD4+ T cell (> 410 cells/µL, 1 point; ≤ 410 cells/µL, 3 points), CRP (≤ 10 mg/L, 1 point; > 10 mg/L, 3 points), and D-dimer (≤ 0.5 ng/mL, 1 point; > 0.5 ng/mL, 3 points). In order to facilitate clinical use and further assessment, a novel prediction model of COVID-19 prediction was established, called the ACCCDL score, which scores from 6 to 25 points. The calculation of the ACCCDL score is shown in Table 3.
Clinical Characteristics of Patients on Hospital Admission in the Validation Set
Clinical characteristics of patients on hospital admission in the validation set are shown in Table 4. The median age was 35 years (IQR 28–49), 20 (4.8%) were older than 60 years, 291 (69.3%) were male, and 68 (16.2%) had at least one comorbidity. The 420 patients in the validation set were divided into progressive group (n = 5, 1.2%) and stable group (n = 415, 98.8%) based on whether they progressed to severe cases during the hospitalization. Compared with stable group, progressive group had higher proportions of age > 60 years (40% vs. 4.3%, p < 0.001), comorbidity (80% vs. 15.4%, p < 0.001), CD4+ T cell count ≤ 410 cells/µL (60% vs. 13.0%, p = 0.002), CRP > 10 mg/L (40% vs. 3.9%, p < 0.001), D-dimer > 0.5 ng/mL (60% vs. 9.9%, p < 0.001), and LDH > 250 U/L (60% vs. 4.3%, p < 0.001) (Table 4).
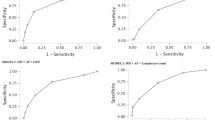
Comparison of AUROCs of Prediction Models
Pairwise comparison of AUROCs of prediction models is shown in Table 5 and Fig. 1. In the training set, the ACCCDL score yielded a significantly higher AUROC compared with the CALL score (0.92 vs 0.84, p = 0.047), the CoLACD score (0.92 vs 0.83, p = 0.043), the PH-COVID-19 score (0.92 vs 0.83, p = 0.029), the NLR model (0.92 vs 0.76, p < 0.001), and the LMR model (0.92 vs 0.65, p < 0.001). In the validation set, the ACCCDL score also yielded a significantly higher AUROC compared with the CALL score (0.97 vs 0.83, p = 0.018), the CoLACD score (0.97 vs 0.83, p = 0.014), the PH-COVID-19 score (0.97 vs 0.78, p = 0.012), the NLR model (0.97 vs 0.74, p < 0.001), and the LMR model (0.97 vs 0.60, p < 0.001).
Comparison of AUROCs of prediction models. For predicting COVID-19 progression, the ACCCDL score yielded a significantly higher AUROC compared with the CALL score, the CoLACD score, the PH-COVID-19 score, the NLR model, and the LMR model both in the training set (0.92, 0.84, 0.83, 0.83, 0.76, and 0.65, respectively) and in the validation set (0.97, 0.83, 0.83, 0.78, 0.74, and 0.60, respectively)
Cutoff Value and Accuracy of the ACCCDL Score
Cutoff value and accuracy of the ACCCDL score is shown in Table 6. The cutoff value is 12 points by maximizing the Youden index, and the corresponding sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) was 88.9%, 80.3%, 9.2%, and 99.7%, respectively, in the training set; and 80.0%, 94.7%, 15.4%, and 99.7%, respectively, in the validation set. The cutoff value is 20 points by using specificity ≥ 95%, and the corresponding sensitivity, specificity, PPV, and NPV was 55.6%, 97.6%, 34.5%, and 99%, respectively, in the training set; and 20.0%, 99.8%, 50%, and 99.0%, respectively, in the validation set.
Discussion
Defining the prognosis of patients with COVID-19 is of the utmost importance for planning the most appropriate setting of care and treatment. By using the clinical data of 1234 patients with COVID-19, we developed and validated a novel prediction score, called the ACCCDL score, based on six variables (age, comorbidity, CD4+ T cell count, CRP, D-dimer, and LDH), aimed at predicting progression toward severe COVID-19. The ACCCDL score ranges from 6 points (age ≤ 60 years, absence of comorbidity, CD4+ T cell > 410 cells/µL, CRP ≤ 10 mg/L, D-dimer ≤ 0.5 ng/mL, LDH ≤ 250 U/L) to 25 points (age > 60 years, ≥ 2 comorbidities, CD4+ T cell ≤ 410 cells/µL, CRP > 10 mg/L, D-dimer > 0.5 ng/mL, LDH > 250 U/L). The power of the ACCCDL score for predicting COVID-19 progression was excellent with AUROC of 0.92 (95% CI 0.90–0.94) in the training set and 0.97 (95% CI 0.95–0.99) in the validation set.
In this study, two cutoff points were reported for the ACCCDL score. A high cutoff (20 points) with high specificity and PPV is used to rule in patients who had risk of COVID-19 progression. A low cutoff (12 points) with high sensitivity and NPV is used to rule out the risk of COVID-19 progression. A total of 641 patients (78.7%) in the training set and 394 patients (93.8%) in the validation set had the ACCCDL score ≤ 12 points, and these patients could be managed at primary health care centers or district hospitals because over 99% of patients with the ACCCDL score ≤ 12 points will not progress to severe cases. About 34.5% (10/29) of patients with the ACCCDL score > 20 points in the training set, and 50% (1/2) of patients with the ACCCDL score > 20 points in the validation set will progress to severe COVID-19, and can benefit from early transfer to tertiary centers.
The ACCCDL score has several attractive features. First, it is inexpensive and very easily calculated, which makes it easier to use. Second, compared with previously reported prediction models, the ACCCDL score provides higher prediction performance and more accurate evaluation for the risk of COVID-19 progression. Third, the ACCCDL score provided a clinically available method for the large flow of patients between primary health care and tertiary centers.
Ji et al. enrolled 208 patients with COVID-19 and derived a scoring system (the CALL score) predicting progression to severe COVID-19 based on patients’ age, comorbidity, lymphocyte count, and LDH [16]. In the study by Ji et al., the CALL score could identify patients who had low risk of COVID-19 progression with an AUROC of 0.91 (95% CI 0.86–0.94) [16]. However, in another study of 210 patients with COVID-19, Grifoni et al. reported the opposite conclusion that the power of the CALL score for predicting progression to severe COVID-19 was low with an AUROC of 0.62 (95% CI 0.53–0.69) [23]. The two studies had relatively small samples and come to the opposite conclusion. Other external validations are needed to further validate the prediction performance of the CALL score. In this large sample study, we found that the power of the CALL score for predicting progression to severe COVID-19 was high with an AUROC of 0.84 (95% CI 0.81–0.87) in the training set and an AUROC of 0.83 (95% CI 0.79–0.87) in the validation set. There are several possible explanations for the differences. First, the statistic difference might be caused by the size of the sample. Second, there are some differences in the study populations regarding age, comorbidity, and the prevalence of severe cases, known as the spectrum bias [24, 25].
The probable reasons why the ACCCDL score is superior to previous ones is worthy of being discussed. First, compared with the CALL score, the ACCCDL score includes CD4+ T cell count, CRP, and D-dimer levels and this might improve the sensitivity and the specificity. Previous studies also had reported that CD4+ T cell count, CRP, and D-dimer levels could help clinicians to identify patients with COVID-19 progression [12,13,14]. Second, compared with the CALL score which just considers whether patients have comorbidity (without, 1 point; with, 4 point), the ACCCDL score includes the number of comorbidities (absence of comorbidity, 1 point; 1 comorbidity, 4 points; ≥ 2 comorbidities, 6 points) and this also might improve the sensitivity and the specificity. Guan et al. also reported that patients with any comorbidity yielded poorer clinical outcomes than those without, and the number of comorbidities was one of the risk factors of reaching the composite endpoints (admission to an ICU, invasive ventilation, or death). The hazard ratio (95% CI) was 1.79 (1.16–2.77) among patients with at least one comorbidity and 2.59 (1.61–4.17) among patients with two or more comorbidities [26].
This study has some limitations. First, this study is a single-center study. Second, the retrospective design might have caused selection bias [27]. Therefore, the ACCCDL score needs to be externally validated in a prospective study to confirm its prediction reliability. Third, in our cohort, the majority of patients with COVID-19 (more than 70%) were imported cases, which mainly included overseas students and business people. Generally, the overseas students and business people are young and had low risk of comorbidity. Therefore, in this study, both the training set and validation set included < 15% of 60 years old patients, < 20% had more than one comorbidity. The diagnostic performance of the ACCCDL score deserves to be validated in a cohort with more patients who have older age and more common comorbidity, which might strengthen the results of this study. Fourth, the ACCCDL score was not evaluated using patients with negative RT-PCR and a high clinical suspicion of COVID-19 because in Shanghai, China, our hospital is the only designated hospital for confirmed adult patients with COVID-19. All patients were confirmed by the positive results of SARS-CoV-2 nucleotide tests before they were transferred to our hospital.
Conclusions
The ACCCDL score is a simple and accurate model for the prediction of COVID-19 progression. Over 99% of patients with the ACCCDL score ≤ 12 points will not progress to severe cases, and over 30% of patients with the ACCCDL score > 20 points will progress to severe cases. On the basis of the results, we suggest that patients with the ACCCDL score ≤ 12 points can be managed at primary health care centers or district hospitals, and patients with the ACCCDL score > 20 points should be transferred early to tertiary centers for more intensive care and management. The ACCCDL score was useful in regulating the large flow of patients with COVID-19 between primary health care and tertiary centers.
References
Hoehl S, Rabenau H, Berger A, et al. Evidence of SARS-CoV-2 infection in returning travelers from Wuhan, China. N Engl J Med. 2020;382:1278–80.
WHO. Weekly operational update on COVID-19. https://www.who.int/publications/m/item/weekly-operational-update. Accessed 26 Jan 2021.
Bentlage E, Ammar A, How D, et al. Practical recommendations for maintaining active lifestyle during the COVID-19 pandemic: a systematic literature review. Int J Environ Res Public Health. 2020;17:62–5.
Ammar A, Chtourou H, Boukhris O, et al. COVID-19 home confinement negatively impacts social participation and life satisfaction: a worldwide multicenter study. Int J Environ Res Public Health. 2020;17:6237.
Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. 2020;12:1583.
Ammar A, Trabelsi K, Brach M, et al. Effects of home confinement on mental health and lifestyle behaviours during the COVID-19 outbreak: insights from the ECLB-COVID19 multicentre study. Biol Sport. 2021;38:9–21.
Souissi MA, Ammar A, Trabelsi O, et al. Distance motor learning during the COVID-19 induced confinement: video feedback with a pedagogical activity improves the snatch technique in young athletes. Int J Environ Res Public Health. 2021;18:3069.
Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–9.
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–42.
Gupta S, Hayek SS, Wang W, et al. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med. 2020;180:1436–47.
Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–6.
Ali N. Elevated level of C-reactive protein may be an early marker to predict risk for severity of COVID-19. J Med Virol. 2020;92:2409–11.
Li Q, Zhang J, Ling Y, et al. A simple algorithm helps early identification of SARS-CoV-2 infection patients with severe progression tendency. Infection. 2020;48:577–84.
Henry BM, Aggarwal G, Wong J, et al. Lactate dehydrogenase levels predict coronavirus disease 2019 (COVID-19) severity and mortality: a pooled analysis. Am J Emerg Med. 2020;38:1722–6.
Zhang J, Lee KS, Ang LW, Leo YS, Young BE. Risk factors for severe disease and efficacy of treatment in patients infected with COVID-19: a systematic review, meta-analysis, and meta-regression analysis. Clin Infect Dis. 2020;71:2199–206.
Ji D, Zhang D, Xu J, et al. Prediction for progression risk in patients with COVID-19 pneumonia: the CALL score. Clin Infect Dis. 2020;71:1393–9.
Varol Y, Hakoglu B, Kadri CA, et al. The impact of charlson comorbidity index on mortality from SARS-CoV-2 virus infection and A novel COVID-19 mortality index: CoLACD. Int J Clin Pract. 2020;75:e13858.
Mancilla-Galindo J, Vera-Zertuche JM, Navarro-Cruz AR, et al. Development and validation of the patient history COVID-19 (PH-Covid19) scoring system: a multivariable prediction model of death in Mexican patients with COVID-19. Epidemiol Infect. 2020;148:e286.
Imran MM, Ahmad U, Usman U, Ali M, Shaukat A, Gul N. Neutrophil/lymphocyte ratio—a marker of COVID-19 pneumonia severity. Int J Clin Pract. 2020;75:e13698.
Liu G, Zhang S, Hu H, Liu T, Huang J. The role of neutrophil–lymphocyte ratio and lymphocyte–monocyte ratio in the prognosis of type 2 diabetics with COVID-19. Scott Med J. 2020;65:154–60.
Ramos-Penafiel CO, Santos-Gonzalez B, Flores-Lopez EN, et al. Usefulness of the neutrophil-to-lymphocyte, monocyte-to-lymphocyte and lymphocyte-to-platelet ratios for the prognosis of COVID-19-associated complications. Gac Med Mex. 2020;156:405–11.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45.
Grifoni E, Valoriani A, Cei F, et al. The CALL score for predicting outcomes in patients with COVID-19. Clin Infect Dis. 2021;72:182–3.
Ransohoff DF, Feinstein AR. Problems of spectrum and bias in evaluating the efficacy of diagnostic tests. N Engl J Med. 1978;299:926–30.
Poynard T, Halfon P, Castera L, et al. Standardization of ROC curve areas for diagnostic evaluation of liver fibrosis markers based on prevalences of fibrosis stages. Clin Chem. 2007;53:1615–22.
Guan WJ, Liang WH, Zhao Y, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55:2000547.
Choi BC. Sensitivity and specificity of a single diagnostic test in the presence of work-up bias. J Clin Epidemiol. 1992;45:581–6.
Acknowledgements
We thank all doctors who worked in Shanghai Public Health Clinical Center for their efforts in the diagnosis and treatment of patients with COVID-19.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Study concept and design: QL and LC. Data collection: WX, CH, LF, WL, and XX. Analysis and interpretation of data: WX, CH, LF, and QL. Drafting of the manuscript: QL. Critical revision of the manuscript: LC.
Disclosures
Wei Xu, Chenlu Huang, Ling Fei, Weixia Li, Xudong Xie, Qiang Li, and Liang Chen have nothing to declare.
Compliance with Ethics Guidelines
The study was approved by the Clinical Research Ethics Committee of Shanghai Public Health Clinical Center (No. 2021-S013-01). In our hospital, patients with COVID-19 were insulated in negative pressure isolation rooms. As researchers, we could not obtain the chance of physical contact with patients with COVID-19. Therefore, at hospital admission, patients provided verbal consent for their clinical data to be used for medical study using voice or video calls. The procedures were in accordance with the ethical standards of the Helsinki Declaration (1964, amended most recently in 2008) of the World Medical Association.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Xu, W., Huang, C., Fei, L. et al. A Novel Prediction Model of COVID-19 Progression: A Retrospective Cohort Study. Infect Dis Ther 10, 1491–1504 (2021). https://doi.org/10.1007/s40121-021-00460-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-021-00460-4