Abstract
Introduction
Much of the current literature on treatment patterns and disability progression in multiple sclerosis (MS) does not distinguish between the relapsing–remitting and progressive subtypes (including primary [PPMS] and secondary progressive MS [SPMS]), or between active/nonactive disease. Current treatment options for progressive MS are limited, with only one approved product for PPMS and none specifically for nonactive SPMS. Here we report treatment patterns, disability progression, and unmet needs among patients with active and nonactive PPMS and SPMS.
Methods
The annual, cross-sectional survey from the Adelphi Disease Specific Program was used to collect physician-reported data on US adult patients with PPMS and SPMS, including active and nonactive disease. Treatment patterns (including the proportion of patients who were untreated with a disease-modifying therapy [DMT]), disability progression, and unmet need are described from 2016 to 2021.
Results
Data were collected for 2067 patients with progressive MS (PPMS, 1583; SPMS, 484). A substantial proportion of patients were untreated across all groups, and this was highest for nonactive PPMS (~ 43%). The proportion of untreated patients generally declined over time but remained high in 2018–2021 (~ 10–38%). Among treated patients, the proportion receiving infusions increased over time to ~ 34–46%, largely driven by ocrelizumab use after approval. Disability progression was reported for most patients (> 50%), including many who were receiving a DMT. Across all disease subtypes, when physicians were asked about the greatest unmet need with current DMTs, they most frequently cited effectiveness (~ 63–87%), and specifically slowing disease progression (~ 32–59%).
Conclusions
This analysis of physician-reported data reveals that patients with progressive MS, particularly those with nonactive disease, frequently remain untreated or continue to decline despite treatment with available DMTs. Thus there is an enduring need for safe and effective treatments for this underserved population.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Why carry out this study? |
Compared with relapsing–remitting multiple sclerosis (RRMS), progressive MS is associated with greater symptom severity and functional impairment, higher rates of unemployment and hospitalization, greater economic burden, and a more substantial impact on health-related quality of life. |
Much of the current literature on treatment patterns and disability in MS does not distinguish between RRMS and progressive MS, despite there only being one approved product for primary progressive MS (PPMS), and none specifically for nonactive secondary progressive MS (SPMS). |
This study describes treatment patterns, disability progression, and unmet needs specifically among patients with active or nonactive PPMS and SPMS. |
What were the study outcomes/conclusions? |
The data reveal that a substantial proportion of patients are untreated, particularly among those with nonactive disease; that most patients continue to have disability progression, even among those who are treated; and that there is a physician-reported need for disease-modifying therapies with greater effectiveness, followed by improved safety and tolerability. |
These findings suggest that there is an ongoing need for new effective and safe treatments for patients with progressive MS, particularly those with nonactive disease. |
Introduction
Multiple sclerosis (MS) is a chronic, autoimmune, inflammatory disease of the central nervous system, characterized by axonal demyelination and neurodegeneration. The prevalence in 2017 was between 337.9 and 362.6 patients per 100,000 people in the USA [1], affecting approximately one million people.
The clinical course of MS is broadly characterized as relapsing–remitting (RRMS), secondary progressive (SPMS), or primary progressive (PPMS). RRMS accounts for the majority of patients with MS [2,3,4,5,6,7,8], and is defined by symptomatic exacerbations (relapses) that either fully or partially resolve (remission). SPMS follows an initial relapsing–remitting disease course that transitions over time to a progressive worsening of symptoms [9]. SPMS may be further classified as active, which is typically defined by relapse and/or radiologic activity (e.g., gadolinium [Gd]-enhancing lesions) within the previous 2 years, or nonactive, which is defined by the absence of clinical relapse or radiological activity yet having progression independent of relapse activity (PIRA). PPMS is characterized by accruing disability in the absence of a prior relapsing phase and is further classified as active or nonactive depending on the presence or absence of Gd-enhancing lesions, respectively.
MS is associated with significant disability and morbidity [10,11,12], with all-cause mortality up to three times higher than in the general population [10]. There is no cure [13, 14], and the currently available treatments may slow disability progression but do not halt or reverse it [11, 12]. Shared decision-making between the patient and physician should be used to weigh the benefit–risk profile of available treatment options in order to provide optimum care and outcomes for patients [15].
Ocrelizumab, a B cell-depleting agent, is the only disease-modifying treatment (DMT) currently approved for PPMS in the USA [16]. It was approved in 2017 on the basis of results from the phase 3 ORATORIO trial, showing an ~ 6% absolute reduction in the number of patients experiencing disability progression compared with placebo (32.9% versus 39.3%) [17]. Moreover, the reduction in disability progression was higher in patients with active PPMS, with limited benefit for the nonactive population (~ 4% absolute reduction; 32.9% versus 37.2%) [17, 18]. In the EU, ocrelizumab is approved for only early active PPMS, as defined by disease duration, level of disability, and the presence of Gd-enhancing lesions; there are no approved treatments in the EU for nonactive PPMS [19]. The use of ocrelizumab has been associated with various safety concerns, including increased risk of infection and malignancy [16, 19, 20].
In the USA, mitoxantrone is the only approved therapy for SPMS with no distinction regarding activity status [21]. The approval of mitoxantrone was based on studies in patients with active SPMS, with efficacy in nonactive SPMS remaining undefined [22, 23]. The use of mitoxantrone is associated with risks of congestive heart failure and secondary acute myeloid leukemia [21, 24, 25]. Siponimod was studied across the active and nonactive SPMS subpopulations in the phase 3 EXPAND study [26]. It was approved for active SPMS in the USA and the EU in 2019 and 2020, respectively [27, 28]; however, it is not indicated for nonactive SPMS in either region because of limited efficacy in this subpopulation [26,27,28,29]. In the USA, approved therapies for RRMS are also indicated for patients with active SPMS. However, there are currently no approved treatments for nonactive SPMS specifically [29, 30]. As such, there remains a high unmet need for safe and effective DMTs for patients with progressive MS, particularly those with nonactive disease.
Much of the current literature on treatment patterns and disability in MS does not distinguish between subtypes (RRMS or progressive MS) or disease activity (active or nonactive), despite there only being one approved product for PPMS, and none specifically for nonactive SPMS [30,31,32,33,34,35]. A possible reason for this is that claims data for MS use only one ICD-10 code (G35), which limits the availability of subtype-specific data that could be analyzed.
PPMS and SPMS share similar pathophysiology and comparable rates of disease progression [9]; however, both populations are clinically distinct from RRMS. Compared with RRMS, progressive MS is clinically associated with greater symptom severity and functional impairment, higher rates of unemployment and hospitalization [3], greater economic burden, and a more substantial impact on health-related quality of life [36].
Given the limited treatment options for these patients, and the dearth of relevant literature, this study was conducted to gain insight into the current treatment landscape and unmet need across the spectrum of patients with progressive MS, including both active and nonactive disease. Data were examined both before and after the approvals of ocrelizumab and siponimod in order to assess the impact of these therapies, and to better understand the continuing unmet need.
Methods
Study Design
An annual, cross-sectional survey from the Adelphi Disease Specific Program (DSP), conducted independently by Adelphi Real World (Bollington, UK), was used to collect physician-reported data between 2016 and 2021. Detailed methodology has previously been published [37, 38].
Physicians were invited to participate in the survey if they were qualified to practice medicine, were responsible for treatment decisions for patients with MS, and made treatment decisions for ≥ 16 patients with MS in a typical month. All physicians were neurologists, consisting of a mixture of general neurologists and specialists. Participating physicians completed patient record forms (PRFs) every 1–2 years for the next 10–15 patients with MS who consulted them. Information was obtained on the basis of the current consultation and through a review of patients’ medical records; there was no time limit on how far back the physician could look. Physicians were incentivized with financial reimbursement upon survey completion according to fair market rates.
Patients
Physicians in the USA who treat patients with MS and participated in the Adelphi DSP collected data for their next 10–15 adult patients (aged ≥ 18 years) with MS. Data for patients with PPMS or SPMS (active or nonactive) were used for this study.
Active and nonactive PPMS were categories within the current diagnosis reported by the physician. SPMS was also defined by the current diagnosis; however, the active and nonactive categories did not always correspond to presence or absence of relapse. Therefore, disease activity for SPMS was recategorized by looking for clinical relapse in the preceding year, based on responses to a question in the survey (data were not gathered prior to the preceding year). Patients who had a relapse in the previous year were considered to have active SPMS, and those who did not were considered to have inactive SPMS. Patients with unknown relapse status in the previous year were excluded.
Patients could not have been participating in any clinical trials at the time of the survey.
Outcomes
Treatment patterns (including patients with or without a DMT) and physician-reported change in disability are reported for all patients. Treatment patterns are described by the route of DMT administration (infusions, orals, or injectables); time period (2016–2017 or 2018–2021); and for a subset of patients with Expanded Disability Status Scale (EDSS) score ≤ 6.5. Patient characteristics and change in disability are reported for those with and without DMT treatment.
Physicians were also asked to report their reasons for selecting the current DMT, issues experienced with current DMTs, and areas for improvement with DMT regimens. Reasons for selection of the current regimen and areas for improvement were categorized as related to effectiveness, administration, safety and tolerability, or other. Issues with the current regimen were categorized as related to effectiveness and compliance, safety and side effects, insurance, or other. These data are summarized by route of DMT administration (infusions, orals, or injectables) and focus on the most recent time period (2018–2021) in order to determine whether there is a continuing unmet need with the most recently approved treatment options. Data from 2016 to 2017 are reported in the electronic supplementary material.
Statistical Analyses
Data are summarized using descriptive statistics, including frequency (n, %), mean with standard deviation (SD), and median with range.
Study Oversight
This study was funded by Atara Biotherapeutics. Financial support for medical editorial assistance was provided by Atara Biotherapeutics. Data were collected through the Adelphi MS DSP and were analyzed by Adelphi and Atara Biotherapeutics. All authors contributed to data interpretation and the writing, reviewing, and amendment of the manuscript; the first draft was prepared by the authors and a medical writer funded by Atara Biotherapeutics. All authors made the decision to submit the manuscript for publication and vouch for the accuracy and completeness of the data and for the fidelity of the study to the protocol.
Ethics
The data provider (Adelphi Real World, Bollington, UK) and Western Institutional Review Board (Puyallup, WA, USA) confirmed that ethics committee approval was not required for this analysis, as it was based on previous studies, data were de-identified, and no new studies of human or animal subjects were performed by any of the authors. This research is compliant with the US Health Insurance Portability and Accountability Act 1996. This study was performed in accordance with Helsinki Declaration of 1964, and its later amendments. All subjects provided informed consent. Atara Biotherapeutics subscribed to the Adelphi MS DSP; this subscription granted access to analyze and publish from the dataset.
Results
Patients
A total of 2067 patients with progressive MS were included, comprising 1583 patients with PPMS (active, 536; nonactive, 1047) and 484 with SPMS (active, 160; nonactive, 324) (Table 1). A proportion of patients in all subgroups were not currently receiving a DMT, and this was highest for nonactive PPMS (~ 43%). However, the number of prior treatments was generally comparable between treated and untreated patients (Table 1).
Mean age across subgroups ranged from 47.5 to 56.7 years. Approximately half (~ 54%) of patients with PPMS were female, compared with about two-thirds (~ 67%) of those with SPMS. Across all subgroups, most patients were Caucasian (~ 72–84%), with ~ 11–22% African American and ~ 0–4% Hispanic/Latino patients (Table 1).
Treated patients were more likely to work full- or part-time (active PPMS, 37.1%; nonactive PPMS, 40.5%; active SPMS, 52.1%; nonactive SPMS, 26.1%) than untreated patients (26.4%, 29.8%, 27.8%, and 16.5%, respectively). These trends were largely driven by higher rates of full-time employment in the treated population (Table 1). However, rates of unemployment were substantial across all groups and ranged from ~ 17% (treated active SPMS) to ~ 28% (untreated nonactive PPMS; Table 1). There were no trends in the distribution of race/ethnicity between treated and untreated groups (Table 1).
Among currently untreated patients, most of those who were unemployed were aged < 65 years (active PPMS, 79.8%; nonactive PPMS, 81.1%; active SPMS, 91.7%; nonactive SPMS, 65.0%). Among these younger unemployed patients, between ~ 27% (active SPMS) and ~ 40% (active PPMS) were on Medicare.
Treatment Patterns
Treatment patterns for progressive MS, including use (or non-use) of DMTs, the route of administration, and time period (2016–2017 or 2018–2021) are described in Table 2.
PPMS
The proportion of patients with active PPMS who were untreated remained stable from 2016–2017 to 2018–2021 (~ 27%). Nonactive PPMS continued to have the highest proportion of untreated patients, even with the decrease over time from 50.6% to 37.7% (Table 2). In the subset of patients with EDSS score ≤ 6.5, the percentage who were untreated increased among those with active PPMS (17.2% to 22.1%) and declined among those with nonactive PPMS (41.6% to 25.4%).
Over time, the percentage of patients with active PPMS who received infusions more than doubled from 19.6% to 46.1%, causing a decrease in injectables (22.4% to 10.4%) and orals (28.3% to 15.1%) (Table 2). The trend was similar for nonactive PPMS, with increasing use of infusions (9.3% to 35.1%) and declining use of injectables (21.5% to 12.5%) and, to a lesser extent, orals (15.2% to 13.9%) (Table 2). The increasing numbers of patients with active or nonactive disease who received infusions was driven by the use of ocrelizumab (Table 2).
SPMS
The proportion of patients who were untreated decreased from 15.4% to 9.9% for active SPMS, and from 27.1% to 23.8% for nonactive SPMS (Table 2). In the subset of patients with EDSS score ≤ 6.5, the percentage who were untreated remained stable for active SPMS (9.4% to 9.8%) and decreased for nonactive SPMS (23.7% to 18.4%).
There was an increase in the percentage of patients with active SPMS who received infusions (28.2% to 39.7%), while the proportion of injectables and orals remained broadly stable (Table 2). In 2018–2021, only one patient with active SPMS received siponimod. For nonactive SPMS, there was an increase in the use of infusions (15.3% to 34.3%) and a decrease in injectables (25.4% to 14.7%) and orals (30.5% to 25.3%) (Table 2). The increased use of infusions in active and nonactive patients with SPMS was driven by the use of ocrelizumab (Table 2). In 2018–2021, siponimod was used in 3.5% (7/202) of the treated patients with nonactive SPMS.
Disability Progression
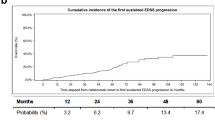
A deterioration/worsening in disability was reported in the majority of patients with active and nonactive PPMS and SPMS (Fig. 1a); this was broadly the case across all types of DMT and in the untreated population (Fig. 1b).
Physician-reported disability progression. a Percentage of patients with stabilization or improvement versus deterioration; percentages calculated from the total number of patients within the given disease category. b Percentage of patients with slow or rapid deterioration by type of DMT and in the untreated population; percentages calculated from the total number of patients within the given disease category who received DMTs via the given mode of administration. Chart excludes patients who received DMTs via “other” mode of administration. DMT disease-modifying treatment, PPMS primary progressive multiple sclerosis, SPMS secondary progressive multiple sclerosis
Reasons for Selecting Current DMT Regimen
In 2018–2021, across all disease subtypes and types of DMT, the most cited reason for selecting the current DMT regimen was effectiveness (~ 85–100%). More specifically, the primary consideration in all cases was to slow disease progression (Supplementary Table S1). Among administration-related factors, convenience was the primary reason for selecting infusions and orals, while the clear and simple dosing regimen was predominant for injectables (Supplementary Table S1).
Safety factors that influenced current DMT selection varied by disease subtype. For active PPMS, favorable risk–benefit balance was the main reason for selecting infusions (19.1%), better tolerability for orals (25.6%), and better tolerability and lack of serious side effects for injectables (28.0% each) (Supplementary Table S1). For nonactive PPMS, favorable risk–benefit balance was the main consideration for infusions (25.0%) and orals (24.0%), and better tolerability for injectables (35.4%) (Supplementary Table S1). For active SPMS, the main safety driver was favorable risk–benefit balance for infusions (25.0%) and orals (36.0%), whereas for injectables it was reduced flu-like symptoms (36.8%) (Supplementary Table S1). For nonactive SPMS, the primary safety factor was risk–benefit balance for infusions (21.0%), and better tolerability for orals (21.3%) and injectables (25.9%) (Supplementary Table S1).
Other reasons that influenced DMT selection included patient-driven demand, including patient’s quality of life and patient request (Supplementary Table S1).
Corresponding data for 2016–2017 are summarized in Supplementary Table S2.
Issues with Current DMT Regimen
In 2018–2021, issues or challenges associated with the current DMT regimen varied by disease subtype and type of DMT (Supplementary Table S3) and are described in detail below. Corresponding data for 2016–2017 are summarized in Supplementary Table S4.
Active PPMS
Issues or challenges with safety and side effects were most commonly reported for infusions (18.5%) and orals (31.3%), followed by efficacy and compliance issues (11.0% and 22.9%, respectively). For injectables, the opposite was true, with higher reports of efficacy and compliance issues (27.3%), followed by safety and side effects (15.2%) (Supplementary Table S3).
Nonactive PPMS
Safety and side effects were the most frequently reported issues for infusions (19.8%), followed by insurance challenges (9.2%) and efficacy and compliance issues (6.0%). For orals, the rates of safety and side effect issues (14.1%) and efficacy and compliance issues (17.4%) were comparable; the same was true of injectables (23.4% and 24.7%, respectively) (Supplementary Table S3).
Active SPMS
Safety and side effects were the most frequently reported issues or challenges for infusions (27.1%) and orals (29.0%), while efficacy and compliance issues were reported in 8.3% and 22.6% of patients, respectively (Supplementary Table S3). For injectables, rates of safety and side effect issues (17.9%) and efficacy and compliance challenges (14.3%) were comparable.
Nonactive SPMS
Safety and side effects were the most commonly reported issues or challenges for orals (19.4%), followed by efficacy and compliance issues (9.0%). For injectables, efficacy and compliance issues (28.2%) were more frequently reported than safety and side effects (18.0%) (Table S3). For infusions, the frequency of safety and side effect issues (15.4%) was comparable with efficacy and compliance (13.2%).
Areas for Improvement Related to Currently Available DMTs
In 2018–2021, across all four disease subtypes, the most cited area for improvement was effectiveness (~ 63–87%), regardless of the type of DMT. More specifically, slowing disease progression was identified as the biggest unmet need (Fig. 2, Supplementary Table S5). Insurance and cost-related issues were less frequently cited as needing improvement, at ~ 14–22%.
Areas for improvement related to current DMT regimen: a active PPMS; b nonactive PPMS; c active SPMS; and d nonactive SPMS. Answers are based on responses to the following question: “What are the main areas where improvement is needed in terms of drug treatment for this patient?” aTotal values include patients receiving DMTs via “other” mode of administration (active PPMS, n = 0; nonactive PPMS, n = 4; active SPMS, n = 1; nonactive SPMS, n = 4). DMT disease-modifying treatment, PPMS primary progressive multiple sclerosis, SPMS secondary progressive multiple sclerosis
The remainder of this section summarizes other areas for improvement, relating to safety and administration. Corresponding data for 2016–2017 are summarized in Supplementary Table S6.
Active PPMS
Safety and tolerability issues requiring improvement were reported in 36.6%, 39.5%, and 24.0% of patients who received infusions, orals, or injectables, respectively (Fig. 2a). A requirement for less monitoring was the most prominent safety and tolerability-related area for improvement across all modes of administration (19.9% infusions, 23.3% orals, 12.0% injectables) (Supplementary Table S5).
Administration issues requiring improvement were reported in 18.3%, 14.0%, and 40.0% of patients who received infusions, orals, or injectables, respectively (Fig. 2a). Convenience of administration was the most reported area needing improvement for infusions (10.7%), while the level of disruption to patients’ lives was most cited for orals (11.6%). Convenience of administration and injection frequency were equally identified as most needing improvement for injectables (20.0% each) (Supplementary Table S5).
Nonactive PPMS
Safety and tolerability issues requiring improvement were reported in 37.2%, 38.7%, and 41.7% of patients who received infusions, orals, or injectables, respectively (Fig. 2b). The most prominent area for improvement with infusions and orals was a requirement for less monitoring (18.9% and 20.0%, respectively), while for injectables a reduction in injection-site pain and reactions was most cited (25.0%) (Supplementary Table S5).
Administration issues requiring improvement were reported in 15.3%, 9.3%, and 37.5% of patients who received infusions, orals, or injectables, respectively (Fig. 2b). In particular, convenience of administration was reported as needing improvement for infusions (7.7%) and orals (5.3%), and the level of disruption to patients’ lives for injectables (18.8%) (Supplementary Table S5).
Active SPMS
Safety and tolerability issues requiring improvement were reported in 45.0%, 48.0%, and 31.6% of patients who received infusions, orals, or injectables, respectively (Fig. 2c). Specifically, the emergence of serious side effects was the main area identified as needing improvement for infusions (17.5%), while emergence of serious side effects, risk of liver damage, and a requirement for less monitoring were equally paramount for orals (12.0% each). For injectables, flu-like symptoms, cardiac risk, and drug interactions were all cited as areas most needing improvement (10.5% each) (Supplementary Table S5).
Administration issues requiring improvement were reported in 15.0%, 16.0%, and 10.5% of patients who received infusions, orals, or injectables, respectively (Fig. 2c). Specific areas requiring improvement varied and included convenience of administration for infusions (10.0%), clarity and simplicity of the dosing regimen for orals (12.0%), and injection frequency and level of disruption to patients’ lives for injectables (5.3% each) (Supplementary Table S5).
Nonactive SPMS
Safety and tolerability issues requiring improvement were reported in 29.6%, 44.3%, and 25.9% of patients who received infusions, orals, or injectables, respectively (Fig. 2d). A requirement for less monitoring was the most frequently cited area for improvement for infusions (23.5%) and orals (26.2%). For injectables, requirements for less monitoring and reduced flu-like symptoms were equally cited (11.1% each) (Supplementary Table S5).
Administration issues requiring improvement were reported in 17.3%, 9.8%, and 44.4% of patients who received infusions, orals, or injectables (Fig. 2d); convenience was the main administration factor needing improvement for infusions (9.9%) and injectables (29.6%), while clarity and simplicity of dosing regimen was most cited for orals (6.6%) (Supplementary Table S5).
Discussion
This study analyzed responses to an annual, cross-sectional, physician-reported survey conducted from 2016–2017 (prior to ocrelizumab and siponimod approval) to 2018–2021 (after ocrelizumab and siponimod approval), and provides unique insight into the evolving treatment landscape for patients with progressive MS. The survey highlights an unmet need by revealing that many patients either do not receive treatment or receive therapies that are not approved for progressive MS (particularly the nonactive subtypes), which may not be effective in these populations. Strikingly, the data reveal that a substantial proportion of patients were untreated across all groups, ranging from ~ 11% of those with active SPMS to ~ 43% with nonactive PPMS. Many untreated patients were unemployed (~ 24–28%) and on Medicare (~ 28–42%), despite the majority being under 65 years of age. Across disease subtypes, most of the currently untreated patients had received prior treatment (~ 57–85%), with the exception of nonactive PPMS (~ 41%). Importantly, the significant proportion of patients with an EDSS score ≤ 6.5 who remained untreated (~ 10–25%) indicates that the unmet need extends to those who are not wheelchair-bound.
Although several treatments have been approved for RRMS and active SPMS in recent years, patients with progressive (particularly nonactive) disease remain underserved by the current treatment options [39,40,41]. Potential reasons for not currently treating patients with SPMS might include having exhausted all treatment options with a positive benefit–risk profile, or stabilization of their condition due to immunosenescence. The limited availability of effective treatment options for patients with PPMS, particularly those with nonactive disease [41], may have contributed to the high proportion of untreated patients with nonactive PPMS who were also treatment-naïve (~ 59%). In addition, while patients with SPMS may have had stepwise therapy during the relapsing–remitting phase, those with PPMS have to decide at diagnosis whether to proceed with high-efficacy (but potentially high-risk) therapy or receive no treatment at all. Since evidence suggests that patients with MS generally have a low tolerance for risk, which is lower at diagnosis and increases with longer disease duration [42], this may explain the high proportion of patients with PPMS in particular who choose to remain treatment naïve.
Among patients with progressive MS who were currently treated, there was an increase over time in the proportion who received DMT via infusion, from ~ 9–28% in 2016–2017, to ~ 34–46% in 2018–2021. The increase was consistent between patients with active and nonactive disease, and was primarily driven by the use of ocrelizumab following its approval for PPMS and active SPMS in 2017 [16]. In contrast, only a small percentage of treated patients (~ 0–3%) received siponimod after its approval for active SPMS in 2019/2020 [27, 28]. In 2018–2021, there remained a substantial proportion of patients receiving off-label treatments, evidenced by the fact that ~ 14–15% of patients with PPMS and ~ 25% of patients with nonactive SPMS received oral treatments, while ~ 10–13% of patients with PPMS and ~ 15% of patients with nonactive SPMS received injectable treatments. Although there are currently no approved treatments for nonactive SPMS, there continued to be high off-label use of DMTs (~ 76% of patients). These treatments may not be effective for nonactive SPMS, and data on physician-reported disability progression suggest that this is the case, with deterioration reported in ~ 63% of patients with nonactive SPMS.
Responses to this survey also revealed that the majority of patients (~ 52–70%) across all disease types, and 46–75% of patients receiving a DMT, continued to have disability progression. The high proportion of patients with continued disability progression is a concern, since functional impairment is one of the main determiners of diminished quality of life among patients with MS [43]. Previous studies have shown that treatments for progressive MS lead to slowing—but not cessation—of disability progression [26, 44, 45], meaning that patients continue to deteriorate, albeit at a slower rate. There is therefore an enduring need for additional treatments for progressive MS that are safe and effective and could potentially halt or improve disability [40, 41, 46]. Underlining this unmet need is the fact that progressive patients experience greater disease burden and worse quality of life than those with relapsing–remitting disease [3, 36]. The unmet need is especially urgent for patients with nonactive disease, for whom approved treatment options are limited (PPMS) or non-existent (SPMS) [41].
This survey also explored physicians’ perceptions of current DMT regimens for their patients. Across all groups, the primary reason for prescribing the current regimen was effectiveness in slowing disease progression. Interestingly, however, most physicians also reported that their patients continued to have slow or rapid deterioration of their disability, including many who were being treated with DMTs. Concordantly, effectiveness was the area most frequently cited by physicians as needing improvement. Among issues related to safety and tolerability, a requirement for less monitoring was frequently cited by physicians as the main area for improvement. This reflects the burden imposed by many existing therapies, both for patients themselves and for healthcare professionals whose time and resources are needed for monitoring. When choosing DMT regimens for their patients, an often-cited reason for selecting injectables was the reduction of flu-like symptoms. This is perhaps surprising, given that injectable DMTs—particularly interferons—are associated with the emergence of flu-like symptoms [47, 48]. However, physicians likely consider this when selecting interferons and opt for the one that is associated with the least flu-like symptoms. Moreover, physicians may opt for glatiramer acetate, which has not been associated with flu-like symptoms [49]. Convenience, patient’s quality of life, and, to a lesser extent, patient’s direct request as reasons for the current DMT regimen suggest that shared decision-making between physicians and patients plays a role in treatment choice.
Although there is a wealth of literature on the management of patients with RRMS, this study is among the few focusing on treatment patterns and disability progression across the spectrum of progressive MS. However, the use of a physician-reported, cross-sectional survey is associated with various weaknesses and limitations. The first is a susceptibility to recall, nonresponse, and selection bias [50]. Since this is a cross-sectional survey with real-world data, timing between visits for patients may vary greatly, collected outcomes are limited (i.e., do not have data for outcomes in clinical trials that are not collected in clinical practice, including all MRI outcomes such as slowly expanding lesions), and documentation of outcomes may be unclear, which impacts physicians’ recall and available data. There may be selection bias for those physicians who agree to participate and those who did not respond. Patients who were not seeing a physician, were not properly diagnosed with progressive disease, or had a delay in receiving this diagnosis are not included in this study. Patients who are less likely to see a physician and may be underrepresented include African Americans, patients with lower socioeconomic status, no insurance, or those who live remote from providers. This will likely lead to an underestimation of the number of patients who go untreated so the estimates reported here should therefore be treated as conservative. Secondly, given that this is a descriptive study based on annual cross-sectional surveys, it is difficult to make causal inferences or comparisons, as this would require ongoing, longitudinal patient follow-up, with adjustment made for differences in key patient characteristics [50]. It is also likely that there will be some overlap in the patient samples from each year, though this may be small. Sex- or race/ethnicity-specific analyses were not conducted as part of this study; however, the predominance of female patients and those who are White/Caucasian in the study population (~ 57% and 76% overall, respectively) is to be expected, given that MS is known to have a higher prevalence among women and those who are White/Caucasian [51, 52]. We would therefore expect our findings to broadly reflect the progressive MS population as a whole. Nevertheless, further studies investigating sex- or race/ethnicity-specific differences in treatment patterns and unmet need may be of interest. Thirdly, as this study explores the current unmet need in a real-world setting with currently approved or available treatments, future studies may also be needed as new therapies are approved, particularly in progressive MS. A final consideration is that the population studied here does not reflect the true epidemiology of PPMS and SPMS, due to oversampling of PPMS in certain years. However, it is likely that the overall surveyed population is broadly representative of patients with progressive MS, including within the PPMS and SPMS subtypes. This is also limited to the USA and may not reflect other countries, especially those with different labels that may impact prescribing and treatment patterns.
Balancing these weaknesses and limitations, this study did present a number of strengths. Categorization of progressive MS type (PPMS or SPMS) and disease activity (active or nonactive) allowed for the analysis of subtype-specific data. Further, this study provided both objective data on treatment patterns and physicians’ reasoning for selecting the current DMT as well as areas for improvement with DMT regimens. Finally, the fact that data were collected for a large number of patients (PPMS, 1583; SPMS, 484), over a substantial period of time (2016–2021), provides a strong basis for future studies.
Conclusions
This study provides unique insight into treatment patterns and unmet needs among patients with progressive MS. The unmet need in this population is evidenced by the high proportion of patients who were untreated or had never started treatment (particularly among those with nonactive disease), evidence of continued deterioration in function despite treatment with DMTs, and the physician-reported need for DMTs with improved effectiveness and reduced monitoring. Thus, there is an ongoing need for new effective and safe treatments for patients with progressive MS—particularly those with nonactive disease.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States: a population-based estimate using health claims data. Neurology. 2019;92(10):e1029–40.
Damotte V, Lizee A, Tremblay M, et al. Harnessing electronic medical records to advance research on multiple sclerosis. Mult Scler. 2019;25(3):408–18.
Gross HJ, Watson C. Characteristics, burden of illness, and physical functioning of patients with relapsing-remitting and secondary progressive multiple sclerosis: a cross-sectional US survey. Neuropsychiatr Dis Treat. 2017;13:1349–57.
Kalincik T, Vivek V, Jokubaitis V, et al. Sex as a determinant of relapse incidence and progressive course of multiple sclerosis. Brain. 2013;136(Pt 12):3609–17.
Kister I, Chamot E, Cutter G, et al. Increasing age at disability milestones among MS patients in the MSBase Registry. J Neurol Sci. 2012;318(1–2):94–9.
Nazareth TA, Rava AR, Polyakov JL, et al. Relapse prevalence, symptoms, and health care engagement: patient insights from the Multiple Sclerosis in America 2017 survey. Mult Scler Relat Disord. 2018;26:219–34.
Tintore M, Alexander M, Costello K, et al. The state of multiple sclerosis: current insight into the patient/health care provider relationship, treatment challenges, and satisfaction. Patient Prefer Adherence. 2017;11:33–45.
Zhou Y, Claflin SB, Stankovich J, et al. Redefining the multiple sclerosis severity score (MSSS): the effect of sex and onset phenotype. Mult Scler. 2020;26(13):1765–74.
Lublin FD, Reingold SC, Cohen JA, et al. Defining the clinical course of multiple sclerosis: the 2013 revisions. Neurology. 2014;83(3):278–86.
Capkun G, Dahlke F, Lahoz R, et al. Mortality and comorbidities in patients with multiple sclerosis compared with a population without multiple sclerosis: an observational study using the US Department of Defense administrative claims database. Mult Scler Relat Disord. 2015;4(6):546–54.
Claflin SB, Broadley S, Taylor BV. The effect of disease modifying therapies on disability progression in multiple sclerosis: a systematic overview of meta-analyses. Front Neurol. 2018;9:1150.
Kister I, Bacon TE, Chamot E, et al. Natural history of multiple sclerosis symptoms. Int J MS Care. 2013;15(3):146–58.
Carrithers MD. Update on disease-modifying treatments for multiple sclerosis. Clin Ther. 2014;36(12):1938–45.
Cree BA, Hartung HP. Steering through complexity: management approaches in multiple sclerosis. Curr Opin Neurol. 2016;29(3):263–71.
Ubbink DT, Damman OC, de Jong BA. Shared decision-making in patients with multiple sclerosis. Front Neurol. 2022;13:1063904.
FDA. OCREVUS Prescribing Information. 2017. https://www.gene.com/download/pdf/ocrevus_prescribing.pdf. Accessed 18 Nov 2022.
Montalban X, Hauser SL, Kappos L, et al. Ocrelizumab versus placebo in primary progressive multiple sclerosis. N Engl J Med. 2016;376(3):209–20.
Mills EA, Begay JA, Fisher C, Mao-Draayer Y. Impact of trial design and patient heterogeneity on the identification of clinically effective therapies for progressive MS. Mult Scler. 2018;24(14):1795–807.
EMA. OCREVUS Summary of Product Characteristics. 2018. https://www.ema.europa.eu/en/documents/product-information/ocrevus-epar-product-information_en.pdf. Accessed 23 Nov 2022.
Wolinsky JS, Arnold DL, Brochet B, et al. Long-term follow-up from the ORATORIO trial of ocrelizumab for primary progressive multiple sclerosis: a post-hoc analysis from the ongoing open-label extension of the randomised, placebo-controlled, phase 3 trial. Lancet Neurol. 2020;19(12):998–1009.
FDA. NOVANTRONE®mitoXANTRONE for injection concentrate. 2008. https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/019297s030s031lbl.pdf. Accessed 9 Dec 2022.
Hartung H-P, Gonsette R, Konig N, et al. Mitoxantrone in progressive multiple sclerosis: a placebo-controlled, double-blind, randomised, multicentre trial. Lancet. 2002;360(9350):2018–25.
Krapf H, Morrissey SP, Zenker O, Zwingers T, Gonsette R, Hartung H-P. Effect of mitoxantrone on MRI in progressive MS: results of the MIMS trial. Neurology. 2005;65(5):690–5.
FDA. Mitoxantrone Hydrochloride (marketed as Novantrone and generics) - Healthcare Professional Sheet text version. 2008. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/mitoxantrone-hydrochloride-marketed-novantrone-and-generics-healthcare-professional-sheet-text. Accessed 9 Dec 2022.
Martinelli V, Radaelli M, Straffi L, Rodegher M, Comi G. Mitoxantrone: benefits and risks in multiple sclerosis patients. Neurol Sci. 2009;30(Suppl 2):S167–70.
Kappos L, Bar-Or A, Cree BAC, et al. Siponimod versus placebo in secondary progressive multiple sclerosis (EXPAND): a double-blind, randomised, phase 3 study. Lancet. 2018;391(10127):1263–73.
EMA. Mayzent. 2020. https://www.ema.europa.eu/en/medicines/human/EPAR/mayzent. Accessed 19 Dec 2022.
FDA. FDA approves new oral drug to treat multiple sclerosis. 2019. https://www.fda.gov/news-events/press-announcements/fda-approves-new-oral-drug-treat-multiple-sclerosis. Accessed 9 Dec 2022.
Gold R, Piani-Meier D, Kappos L, et al. Siponimod vs placebo in active secondary progressive multiple sclerosis: a post hoc analysis from the phase 3 EXPAND study. J Neurol. 2022;269(9):5093–104.
Tintore M, Vidal-Jordana A, Sastre-Garriga J. Treatment of multiple sclerosis - success from bench to bedside. Nat Rev Neurol. 2019;15(1):53–8.
Bogosian A, Morgan M, Moss-Morris R. Multiple challenges for people after transitioning to secondary progressive multiple sclerosis: a qualitative study. BMJ Open. 2019;9(3): e026421.
Bowen J, Mehta R, Pelletier C, et al. Treatment patterns among patients with multiple sclerosis initiating second-line disease-modifying therapy. Adv Ther. 2020;37(7):3163–77.
Fernandez-Diaz E, Perez-Vicente JA, Villaverde-Gonzalez R, et al. Real-world experience of ocrelizumab in multiple sclerosis in a Spanish population. Ann Clin Transl Neurol. 2021;8(2):385–94.
Lepore V, Bosetti C, Santucci C, Iaffaldano P, Trojano M, Mosconi P. Detection of disability worsening in relapsing-remitting multiple sclerosis patients: a real-world roving Expanded Disability Status Scale reference analysis from the Italian Multiple Sclerosis Register. Eur J Neurol. 2021;28(2):567–78.
Wiendl H, Spelman T, Butzkueven H, et al. Real-world disability improvement in patients with relapsing-remitting multiple sclerosis treated with natalizumab in the Tysabri Observational Program. Mult Scler. 2021;27(5):719–28.
Chataway J, Murphy N, Khurana V, Schofield H, Findlay J, Adlard N. Secondary progressive multiple sclerosis: a systematic review of costs and health state utilities. Curr Med Res Opin. 2021;37(6):995–1004.
Anderson P, Benford M, Harris N, Karavali M, Piercy J. Real-world physician and patient behaviour across countries: disease-specific programmes - a means to understand. Curr Med Res Opin. 2008;24(11):3063–72.
Neuberger EE, Abbass IM, Jones E, Engmann NJ. Work productivity outcomes associated with ocrelizumab compared with other disease-modifying therapies for multiple sclerosis. Neurol Ther. 2021;10(1):183–96.
Baldassari LE, Fox RJ. Therapeutic advances and challenges in the treatment of progressive multiple sclerosis. Drugs. 2018;78(15):1549–66.
Faissner S, Plemel JR, Gold R, Yong VW. Progressive multiple sclerosis: from pathophysiology to therapeutic strategies. Nature Rev Drug Discov. 2019;18(12):905–22.
Hauser SL, Cree BAC. Treatment of multiple sclerosis: a review. Am J Med. 2020;133(12):1380-90.e2.
Glanz BI, Greeke E, LaRussa A, et al. Risk attitudes and risk perceptions in individuals with multiple sclerosis. Mult Scler J Exp Transl Clin. 2016;2:2055217316665406.
Gil-González I, Martín-Rodríguez A, Conrad R, Pérez-San-Gregorio M. Quality of life in adults with multiple sclerosis: a systematic review. BMJ Open. 2020;10(11): e041249.
Naegelin Y, Naegelin P, von Felten S, et al. Association of rituximab treatment with disability progression among patients with secondary progressive multiple sclerosis. JAMA Neurol. 2019;76(3):274–81.
Vermersch P, Brieva-Ruiz L, Fox RJ, et al. Efficacy and safety of masitinib in progressive forms of multiple sclerosis: a randomized, phase 3, clinical trial. Neurol Neuroimmunol Neuroinflamm. 2022;9(3):e1148.
Hollen CW, Paz Soldán MM, Rinker JR 2nd, Spain RI. The future of progressive multiple sclerosis therapies. Fed Pract. 2020;37(Suppl 1):S43–9.
Filipi ML, Beavin J, Brillante RT, et al. Nurses’ perspective on approaches to limit flu-like symptoms during interferon therapy for multiple sclerosis. Int J MS Care. 2014;16(1):55–60.
Halper J, Centonze D, Newsome SD, et al. Management strategies for flu-like symptoms and injection-site reactions associated with peginterferon beta-1a: obtaining recommendations using the Delphi Technique. Int J MS Care. 2016;18(4):211–8.
Simpson D, Noble S, Perry C. Glatiramer acetate: a review of its use in relapsing-remitting multiple sclerosis. CNS Drugs. 2002;16(12):825–50.
Wang X, Cheng Z. Cross-sectional studies: strengths, weaknesses, and recommendations. Chest. 2020;158(1s):S65-71.
Harbo HF, Gold R, Tintoré M. Sex and gender issues in multiple sclerosis. Ther Adv Neurol Disord. 2013;6(4):237–48.
Amezcua L, McCauley JL. Race and ethnicity on MS presentation and disease course. Mult Scler J. 2020;26(5):561–7.
Acknowledgements
We thank the participants of the study.
Medical Writing/Editorial Assistance
Medical writing assistance was provided by Lee Blackburn, AMICULUM Ltd, funded by Atara Biotherapeutics. Analytical support was provided by Mia Unsworth and Emily Trenholm, Adelphi Real World.
Funding
This study was funded by Atara Biotherapeutics, Thousand Oaks, CA, USA. The Rapid Service Fee was also funded by Atara Biotherapeutics.
Author information
Authors and Affiliations
Contributions
Crystal Watson, Dhanalakshmi Thirumalai, Arie Barlev, Sasha Bogdanovich, and Kiren Kresa-Reahl were involved in the conception or design of the study. All authors performed data acquisition, analysis, or interpretation. All authors reviewed and approved the final manuscript. All authors are accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
Crystal Watson, Kiren Kresa-Reahl, Arie Barlev, and Sasha Bogdanovich are employees and shareholders of Atara Biotherapeutics. Dhanalakshmi Thirumalai was an employee and shareholder of Atara Biotherapeutics at the time of the study. Eddie Jones is an employee of Adelphi Real World.
Ethical Approval
The data provider (Adelphi Real World, Bollington, UK) and Western Institutional Review Board (Puyallup, WA, USA) confirmed that ethics committee approval was not required for this analysis, as it was based on previous studies, data were de-identified, and no new studies of human or animal subjects were performed by any of the authors. This research is compliant with the US Health Insurance Portability and Accountability Act 1996. This study was performed in accordance with Helsinki Declaration of 1964, and its later amendments. All subjects provided informed consent. Atara Biotherapeutics subscribed to the Adelphi MS DSP; this subscription granted access to analyze and publish from the dataset.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Watson, C., Thirumalai, D., Barlev, A. et al. Treatment Patterns and Unmet Need for Patients with Progressive Multiple Sclerosis in the United States: Survey Results from 2016 to 2021. Neurol Ther 12, 1961–1979 (2023). https://doi.org/10.1007/s40120-023-00532-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-023-00532-2