Abstract
Introduction
Mechanistic target of rapamycin (mTOR) inhibitors sirolimus and everolimus are an effective therapy for subependymal giant cell astrocytomas, cardiac rhabdomyomas, renal angiomyolipomas, and lymphangioleiomyomatosis associated with tuberous sclerosis complex (TSC). Everolimus was recently approved in the EU and the USA for the treatment of refractory focal-onset seizures. Despite frequent use of mTOR inhibitors, there are only a few studies on their effect on epilepsy control in children under 2 years of age. This study aims to assess the effect of adjunctive mTOR inhibitor treatment on seizure frequency in this age group.
Methods
We performed retrospective data analysis of medical records of patients with TSC who initiated sirolimus or everolimus under the age of 2 years. Participants’ antiseizure medication was adjusted according to their epilepsy control independently from mTOR inhibitor administration. The data was assessed separately for patients treated with mTOR inhibitors before and after the onset of seizures. We also compared the treatment group with a matched control group. The follow-up duration was up to 24 months.
Results
Twenty-one patients with TSC from two clinical centers were included in the study. Nine participants had no history of seizures before mTOR inhibitor initiation. Twelve reported active epilepsy in the month prior to treatment initiation. Most patients treated preventively with mTOR inhibitors did not report active epilepsy at the end of their follow-up. In the second group, the mean frequency of seizures decreased with time. According to the comparative analysis, seizure control was better in the groups treated with mTOR inhibitors.
Conclusion
Patients with TSC treated with mTOR inhibitors demonstrated better seizure control than individuals without this treatment. Adjunctive pharmacotherapy with mTOR inhibitors appears to have a beneficial effect on epilepsy outcome in young children. Further prospective clinical trials should be conducted to determine the efficacy of mTOR inhibitors on epilepsy in patients with TSC under the age of 2 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
mTOR inhibitors are a novel pharmacotherapy alternative for treating TSC-associated subependymal giant cell astrocytomas, renal angiomyolipomas, focal-onset epilepsy, cardiac rhabdomyomas, and lymphangioleiomyomatosis. However, there is limited research on their impact on seizure control in patients under the age of 2 years. |
In this study, we aimed to assess the effect of mTOR inhibitors on epilepsy control in young children when administered preventively and when added to the current antiseizure medication. |
Patients treated with mTOR inhibitors demonstrated better seizure control when compared with the patients in the control group. |
Introduction
Mechanistic target of rapamycin (mTOR) pathway plays a specific role in epileptogenesis in several neurological disorders, belonging to the group of “mTORopathies”, including focal cortical dysplasia, tuberous sclerosis complex (TSC), and hemimegalencephaly [1,2,3]. TSC is an autosomal dominant neurocutaneous disorder resulting from a mutation in TSC1 or TSC2 genes. Under normal conditions, their protein products, hamartin and tuberin, inhibit mTOR function. mTOR is a protein kinase that regulates cellular growth, metabolism, and differentiation [4, 5]. The mutation leads to disinhibition and overactivation of the mTOR pathway and, thus, multiple benign tumor formation in various organs.
Results of several clinical trials demonstrated that mTOR inhibitors (mTORi) sirolimus and everolimus are effective in the treatment of TSC-associated subependymal giant cell astrocytomas (SEGA), cardiac rhabdomyomas (CR), renal angiomyolipomas (AML), and lymphangioleiomyomatosis (LAM) [6, 7]. mTOR inhibitors were recently approved in the EU, USA, and Japan [8]. Besides focal-onset seizures, everolimus is currently approved for treating SEGA and LAM and used as an off-label treatment for CR reduction [9,10,11,12,13]. Sirolimus is approved only as LAM therapy in patients with TSC, while its impact on seizure frequency is not yet determined.
Up to 80–90% of patients with TSC report epilepsy, and almost 80% of them experience the onset of seizures under 2 years of age [14]. The direct mechanism of epileptogenesis in TSC is still unknown. mTOR mutations may impact synaptic plasticity mechanisms, while molecular changes in protein expression may increase neuronal excitability, leading to seizures [15,16,17,18].
Epilepsy control depends widely on the timing of the treatment introduction, with the best outcome when initiated prior to or within a week from clinical seizure onset [19,20,21,22]. Vigabatrin is recommended as the first-line treatment for infantile spasms in the USA and all seizures under the age of 1 year in the EU in patients with TSC [23]. It increases GABA (γ-aminobutyric acid) levels and, thus, has a different mechanism of action from mTOR inhibitors. Preclinical animal studies demonstrated the antiepileptogenic effect of mTOR inhibitor treatment [24, 25]. The synergistic action of those drugs may strengthen their preventive and disease-modifying function.
One-third of epileptic seizures in children with TSC become refractory to treatment, and it correlates with the early age at the first clinical seizure, a mutation in the TSC2 gene, and the number of cortical tubers [26].
Adjunctive treatment with sirolimus or everolimus in the youngest patients with drug-resistant seizures could improve their epilepsy control, as was reported by a few studies [9, 27]. However, analyses were conducted only on a small number of patients. Prospective clinical trials are ongoing in the EU and USA, but no results have been published yet. This is the largest study so far to assess the effect of adjunctive mTOR inhibitor treatment in seizure control in patients with TSC under the age of 2 years.
Methods
Study Design
We performed a retrospective analysis of medical records of patients with TSC born between 2008 and 2022. The data was derived from the medical history of individuals treated with mTOR inhibitors for SEGA, CR, renal AML, and epilepsy in the two clinical centers in Warsaw, Poland: the Department of Neurology and Epileptology, The Children’s Memorial Health Institute, and the Department of Pediatric Neurology, the Medical University of Warsaw in Warsaw, Poland. The ICD coding number for TSC, Q85.1, was applied for the database search. The data was extracted and transferred into a spreadsheet. The data collection process was performed until 30 June 2022.
The inclusion criteria were:
-
1.
Genetic or clinical diagnosis of TSC
-
2.
Oral pharmacotherapy with an mTORi, sirolimus or everolimus, initiated before the age of 2 years
-
3.
Active epilepsy in the month prior to mTORi introduction or no history of epilepsy
-
4.
At least 3 months of follow-up after mTORi pharmacotherapy commencement
Patients’ characteristics collected from the medical records included gene mutation and sex. We also retrieved information on the age at the first epileptic seizure and whether epilepsy was active the month before mTORi treatment introduction.
The details of mTORi and antiseizure medication (ASM) used during the follow-up were collected.
We identified patients with refractory epilepsy, also known as drug-resistant epilepsy. It was defined according to the International League Against Epilepsy (ILAE) definition, “the failure of adequate trials of two tolerated and appropriately chosen and used antepileptic drug schedules (whether as monotherapies or in combination) to achieve sustained seizure freedom” [28].
Regarding the patient’s medical history, the following information from the follow-up visits was collected: the number of seizures per week, sirolimus and everolimus dose, their blood concentration, and ASM used at the time. For each patient, the data was collected from the visit at the beginning of the treatment with mTOR inhibitor, 3 months later, 6 months after the initiation of the treatment, and 1 year and 2 years after starting pharmacotherapy (V0, V3, V6, V12, and V24, respectively).
After data collection, the patients were divided into two groups:
- G0:
-
individuals with no history of epileptic seizures prior to mTOR inhibitor initiation
- G1:
-
individuals with epileptic seizures prior to mTOR inhibitor initiation
Each patient was then matched 1:1 with the control group. The control group was recruited from a database of patients with TSC from the same two clinical centers but not treated with mTOR inhibitors.
The study was conducted according to the guidelines of the Declaration of Helsinki 1964, and the Bioethics Committee of the Medical University of Warsaw was informed of the study. Ethical approval was waived for this study as a result of the study characteristics. Patient consent was waived because of the retrospective nature of the study, minimal risk, and data anonymization.
Propensity Score Matching
The matching of treated patients with the control group used a propensity score matching (PSM) method based on propensity score (PS), defined as the probability of assigning an individual due to a set of specified variables, to minimize differences between the individuals being compared. Patients were matched on the basis of the covariates: gene mutation, sex, and age at the onset of pharmacotherapy, ASM, or mTOR inhibitor, depending on which was first.
Patients from the G0 group were matched with individuals treated preventively with vigabatrin. In the G0 group, the age at the onset of pharmacotherapy was set at the initiation of the mTORi treatment, while for their control group it was set as the age at the initiation of vigabatrin. The aim was to compare the effect of preventive treatment with an mTOR inhibitor and vigabatrin.
Participants from the G1 group were matched with patients treated conventionally with ASM after the initiation of seizures. In the G1 group and their control group, the age at the onset of pharmacotherapy was set at the first ASM administration.
Detailed information on the statistical analysis applied in the PSM is available in the supplementary materials.
The V0 visit in the control group for the G0 was set at the age of the first preventive ASM administration. The V0 date in the G1 control group was set at the age of the V0 visit of their matched pair from the G1 group. The data on the seizure frequency was recovered from the control group at the V0 visit and after 3, 6, 12, and 24 months (V3, V6, V12, V24).
Statistical Analysis
The statistical analysis is divided into two parts:
-
1.
Baseline analysis—characteristics of the treated patients; statistical analysis, and graphical analysis of the course of seizures in the group treated with mTOR inhibitors.
-
2.
Comparative analysis—statistical analysis comparing the epilepsy control between the treatment and control groups. It was performed separately for the G0 group and their control, the G1 group and their control, and all treated patients collectively compared with both control groups.
For quantitative variables, minimum and maximum values, mean, standard deviation, median, and interquartile range were assessed. For qualitative variables, the number and frequency of occurrence were described. For numerical variables on consecutive visits, visits were treated as dependent variables. Appropriate statistical tests were used to assess the significance of the impact of individual variables between groups or visits. More detailed information on the statistical tests applied in the analysis is available in the supplementary materials.
Differences were considered statistically significant if p ≤ 0.05.
The change in seizure frequency between visits was compared to the baseline (V0). The differences were also described in percentages: relative and absolute changes in the number of seizures between the visits.
Categories were assigned for relative change calculations and are described in Table 1. The formula to calculate the change was:
where y is the number of seizures at a consecutive visit; x is the number of seizures at the first visit (V0)
In the G0 group, the patients with stabilization were categorized as “No seizures”, while those who reported epileptic seizures as “Seizures”.
The analysis was conducted with R programming language, version 4.1.1 (2021-08-10).
Results
Study Population
Twenty-one patients born between 2008 and 2022 were included in this study. Nine patients (9/21, 42.86%) started treatment with an mTORi before the first epileptic seizures and were included in the G0 group. Twelve patients began the mTORi treatment after the onset of epilepsy and were included in the G1 group (12/21, 57.14%). Thirteen patients were female (13/21, 61.90%), and eight were male (8/21, 38.10%). All included individuals had a TSC2 mutation, and three had an additional mutation in the PKD1 gene.
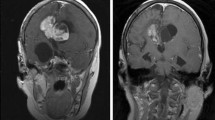
SEGA was the reason for treatment initiation in 13 patients (13/21, 61.90%), refractory epilepsy in seven (7/21, 33.33%), CR in seven (7/21, 33.33%), and renal AML in one (1/21, 4.76%). Eight patients received mTORi as a result of more than one cause (8/21, 38.10%). Ten children (10/12, 83.33%) had epilepsy refractory to treatment when the mTORi treatment was initiated. One patient from the G0 group (1/9, 11.10%) developed drug-resistant epilepsy during the follow-up.
The median age at the mTORi treatment initiation was 20 days in the G0 group, and the median age at the onset of seizures was 122 days. In the G1 group, the median age at the mTOR inhibitor introduction was 444 days, while epilepsy was first reported at 90 days.
Patients’ baseline characteristics are reported in Table 2.
Dosing
Eighteen patients received sirolimus (18/21, 85.71%) and three everolimus (3/21, 14.29%). All patients treated with everolimus were in the G1 group. Patients received mTOR inhibitors orally in the form of a solution.
The initial dosing of sirolimus was 0.5 mg/m2 per day, while that of everolimus was 5 mg/m2 per day. During the follow-up, doses were adjusted on the basis of the mTORi blood levels and the severity and frequency of reported adverse effects. During the follow-up, the median blood levels were 3.72 ng/mL (range 1.72–16.10) for sirolimus and 4.96 ng/mL (range 1.9–6.6) for everolimus.
Treatment Discontinuation
Three patients (3/9, 33.33%) in the G0 group completed the 2-year follow-up. The rest, six individuals (6/9, 66.67%), continued the mTORi treatment until the end of data collection, although their follow-up was shorter than 24 months. None of the patients withdrew from the treatment during the follow-up. The median follow-up duration in this group was 183 days.
Seven patients (7/12, 58.33%) in the G1 group completed the 2-year follow-up. Two individuals continued the mTORi treatment until the end of data collection (2/12, 16.67%), yet their follow-up was shorter than 2 years. Three patients with large dysplastic lesions in the brain discontinued pharmacotherapy because of unsatisfactory results (3/12, 25.00%), one after 6 months of treatment and two after 12 months. All qualified for neurosurgery. The median follow-up duration in the G1 group was 732 days.
ASM Modification During Follow-up
During the follow-up, 19 patients (19/21, 90.48%) received antiseizure treatment.
In the G0 group, two patients did not receive any ASM (2/9, 22.22%). Seven were administered vigabatrin during the follow-up because of the onset of seizures or EEG abnormalities; two required additional valproic acid and levetiracetam. The mean number of ASM was 1.
In the G1 group, all patients were treated with vigabatrin and had antiseizure pharmacotherapy modified during the follow-up. All received more than one ASM, including valproic acid, carbamazepine, levetiracetam, clobazam, and topiramate. Two children received adrenocorticotropic hormone (ACTH), and two patients were on the ketogenic diet. The mean number of ASMs was 2.5.
Adverse Effects of mTORi
All included patients (21/21, 100.00%) reported at least one adverse effect (AE). Adverse events were of mild and moderate severity, grade 1 and 2, according to Common Terminology Criteria for Adverse Events v5.0 [29]. None of the participants discontinued the mTOR inhibitor treatment because of an AE. The interpretation of the blood test results was based on the norms provided by the laboratories after adjusting for age.
The most common adverse effects in patients treated with sirolimus were hyperlipidemia in 16 (16/18, 88.89%), anemia in 11 (11/18, 61.11%), and elevated platelet count in 10 (10/18, 55.56%).
All patients treated with everolimus reported mouth ulcerations (3/3, 100%), hyperlipidemia was found in two (2/3, 66.67%), and anemia in two (2/3, 100%). Mouth ulcerations required temporary treatment discontinuation.
None of the patients reported hemoglobin levels below 8.0 g/dL, nor did they require transfusion. Most patients who reported thrombocytosis reported a platelet count between 450,000 and 700,000/µL, considered “mild”; one patient had a platelet count of 750,000/µL [29].
None of the participants had to be hospitalized because of hyperlipidemia, and it was managed with dietary modifications. Two patients with the highest hyperlipidemia levels were on a ketogenic diet, and the blood test results normalized after the adjustment of the lipid-to-nonlipid ratio.
Effect on Epilepsy Control
G0 Group: Patients with mTORi Introduced Before Onset of Seizures
Nine patients started pharmacotherapy with mTOR inhibitors with no prior history of epilepsy (9/21, 42.86%). Five individuals had their first seizure in the first 3 months after treatment initiation; in three, it was a one-time event, and no other seizures appeared until the end of the follow-up. Two patients had their first epileptic seizure between 3 and 6 months after the initiation of the mTORi, one of them as a one-time event. One patient had a follow-up of less than 6 months. At V3, they developed seizures yet did not discontinue the treatment.
The detailed estimated frequency of epileptic seizures per week during the follow-up in this group is presented in supplementary Table S1.
Five patients were seizure-free 6 months after starting the treatment (5/8, 62.50%). At 24 months, all patients who reached that observation time did not have seizures (3/3, 100.00%). No seizures were reported in seven patients in total at the end of their follow-up (7/9, 77.78%) (Table 3).
G1 Group: Patients with mTORi Introduced After Onset of Seizures
Twelve patients reported active epilepsy the month before the initiation of mTOR inhibitor treatment (12/21, 57.14%). The estimated frequency of epileptic seizures per week during the follow-up in this group is presented in Table 4. The statistical significance was calculated for differences between the seizure frequency at the particular visit and the baseline (V0).
The mean number of seizures per week reduced during the follow-up. Improvement in epilepsy control between the baseline visit (V0) and 24 months later (V24) was statistically significant. The number of patients remaining in the study and the standard deviation decreased. The data on seizure frequency at V24 were not available for one patient, although they did not discontinue the treatment for more than 24 months.
Relative increase was used to characterize the treatment outcome in this group (supplementary material Table S2). At 24 months, six patients were followed up; a significant improvement was achieved in five (5/6, 83.33%) and improvement in one (1/6, 16.67%), compared with V0. Four patients were seizure-free at the end of the follow-up. One patient with the shortest follow-up of less than 6 months presented a minimal initial response to the treatment and a decrease in seizure frequency by 25%.
Absolute changes in the number of seizures between each visit and the baseline are presented in supplementary materials Figs. S2–S5.
Propensity Score Matching
A total of 77 and 28 patients were included in the initial database before PSM for the control group for patients from G0 and G1 treatment groups, respectively.
Detailed results of PSM are available in the supplementary materials. A summary of patients’ characteristics after matching is presented in Table S3.
The groups were not completely balanced, yet the matching could be performed. After analysis, nine patients from the control group were matched with the G0 group, and 12 were matched with the G1 group. All patients from the G0 control group were treated preventively with vigabatrin, and their V0 visit was set at the age of the vigabatrin treatment initiation. All patients from the G1 control group had active epilepsy, and their V0 visit was set at the age of the V0 visit of their respective matched pair from the G1 mTORi treatment group.
All patients from the G0 control group received vigabatrin preventively, before the onset of seizures. During the follow-up, one patient required two additional ASMs, levetiracetam and topiramate, and four patients were administered valproic acid because of insufficient seizure control. The mean number of ASMs was 1.67.
Patients from the G1 control group received vigabatrin, valproic acid, levetiracetam, lamotrigine, carbamazepine, and clobazam. The mean number of ASMs was 2.42. One patient underwent surgical removal of cortical dysplasia after the follow-up period, and one was on a ketogenic diet.
Comparative Analysis
Three comparative analyses were performed: the G0 treatment group compared with their control group, the G1 treatment group compared with their control group, and all patients treated with mTOR inhibitors (G0 and G1) compared with the whole control group.
The mean number of seizures increased in both the G0 and their control groups compared to no active epilepsy at the baseline. The increment was more noticeable in the control group, especially 3 months after the initiation of the treatment. At 24 months, both groups reached stabilization (Fig. 1).
In the G1 mTORi treatment group, the reduction in the number of seizures was more noticeable than in the control group. The mTOR inhibitor in the treatment group was administered as an adjunctive treatment to the ASM, while the control group received only ASMs (Fig. 2).
The whole mTORi treatment group (G0 and G1) was compared with the control group. The seizure frequency reduction was greater in the treatment than in the control group. The difference was statistically significant at 24 months of follow-up (Fig. 3).
The detailed data on the changes in all three versions is presented in supplementary material Tables S4–S6.
Discussion
Randomized clinical trial EXIST-3 reported that everolimus reduced seizure frequency in patients with TSC and refractory epilepsy [30,31,32]. Adjunctive treatment with everolimus improved long-term epilepsy control in children under 3 years of age, both in low- and high-exposure groups.
Our study reports the results of the largest research so far, assessing the effect of two mTOR inhibitors, sirolimus and everolimus, in epilepsy treatment in children under 2 years of age.
Various animal models described an antiepileptogenic effect of preventive treatment with mTOR inhibitors on epilepsy development [25, 33, 34]. We collected data from nine patients with no history of seizures prior to sirolimus initiation, the G0 group. In most of them, seizures appeared during follow-up as one-time events, and the patients did not develop active epilepsy. The appearance of seizures could overlap with the typical age at the onset of epilepsy in patients with TSC, as more than 60% of them experience the first epileptic seizure in the first year of life [35]. The study by Domańska-Pakieła et al. reported that 70% of patients with normal EEG in the first 2 months of life develop EEG abnormalities in the next few months [36].
The G1 treatment group, to whom the mTOR inhibitors were administered after the onset of seizures, reported a decrease in seizure frequency in all visits compared with the baseline. The difference was statistically significant at 24 months from the mTORi initiation. The positive impact of everolimus on seizure reduction in similarly young patients with TSC under 2 years of age was reported in a smaller retrospective study by Saffari et al. [9]. Everolimus was effective as adjunctive therapy in two out of four patients with refractory epilepsy. Kotulska et al. reported improved seizure control in three out of five patients with drug-resistant epilepsy who received everolimus as a result of SEGA [27].
Most patients in this study received sirolimus, a more common and available pharmacotherapy than everolimus, although according to the literature, its efficacy in epilepsy control remains inconclusive [37,38,39]. Research studies on mTOR inhibitors often set the target blood levels of everolimus and sirolimus at 5–15 mg/mL and 4–20 ng/mL, respectively [10]. In our study, the median serum levels of both medications were at the lower threshold. The antiseizure effect could probably be more significant if the blood levels were greater. Similar observations were described in the EXIST-3 reports, where the group with lower exposure to everolimus (3–7 ng/mL) had less significant improvement in epilepsy control than the high-exposure group (9–15 ng/mL) [40].
Once seizures develop, vigabatrin is a treatment of choice in infantile spasms and refractory focal-onset seizures in Europe and the USA [23]. Other conventional ASMs are considered second-line therapy, and in our study, ASMs and their dosing were modified independently from the mTOR inhibitor treatment during the follow-up. The modifications, such as increasing the dose or changing to another ASM were decided on the basis of epilepsy control. It may have impacted the significance of the seizure frequency reduction and led to an overestimation of the role of mTOR inhibitors.
However, according to the comparative analysis, seizure control improved in the group treated additionally with mTOR inhibitors. This study aimed to determine the effect of mTORi added to currently recommended pharmacotherapy. The mean number of ASM and the type of ASMs used in the treatment and control groups were similar. All patients were treated in the two clinical centers, so we assume that the antiseizure pharmacotherapy approach was similar. Therefore we may assess the positive mTORi effect on seizure control as an added disease-modifying treatment.
In all patients included in our study, TSC2 gene mutation, most commonly associated with worse clinical outcomes and a higher prevalence of refractoriness, was found [26, 41]. Dabora et al., in a study on 224 patients, found that seizures are significantly more common in patients with TSC2 than TSC1 mutation (98% vs. 86%, p = 0.02) [42].
Early administration of mTORi could delay the onset of seizures and reduce their severity, as suggested by the results of our study. The risk of refractoriness correlates with the age at the first epileptic seizure [26]. Intellectual impairment, learning difficulties, and disturbances in social development also appear to be related to earlier epilepsy onset [43]. Therefore, it is possible that delaying the onset of epilepsy may contribute to overall better control in the future.
Those findings are important to patients with TSC2 mutation, as epilepsy is more likely to become refractory to treatment if seizures appear early, in the neonatal period, often in individuals with perinatal complications and SEGA [44]. Most patients in our study were administered mTOR inhibitors as a result of SEGA, CR, and epilepsy. According to Krueger et al. and Saffari et al., those are the most common reasons for mTORi treatment introduction [6, 9]. In the last few years, clinical trials have determined a positive effect of mTORi on SEGA size reduction, and currently everolimus is recommended for use in this indication. Therefore, owing to the established role of mTORi in SEGA size change, it was not included as an outcome parameter in this study. mTORi discontinuation may lead to SEGA recurrence, especially if the treatment duration is relatively short [45]. Therefore, most patients who begin the treatment continue it for many years. Epilepsy control after sirolimus and everolimus discontinuation has not been determined yet. Most patients in this study continued the treatment at the end of data collection, so seizure recurrence assessment in a long-term follow-up after mTORi cessation was impossible. The long-term effect of mTORi on epilepsy control after their discontinuation should be addressed in future studies.
Safety is one of the main concerns regarding mTOR inhibitor administration to young children and infants. All participants in our study reported adverse effects, yet of mild or moderate severity. Likewise, the results from EXIST-1 and EXIST-3 clinical trials demonstrated everolimus safety in children under 3 years of age [46, 47]. The adverse effects were more common and significant in the high-dose group, although they remained relatively safe and reversible. Various reports also described sirolimus safety, mostly in older children and adults with TSC [48,49,50]. According to the studies, sirolimus adverse effects are also frequent yet not severe [9, 51]. Both sirolimus and everolimus appear to be safe in young children as well as adults with TSC.
The main limitation of this study is its retrospective character, which may hinder the objectivity and availability of all data. The anamnesis technique and accuracy differed among the physicians. The seizure types and epileptiform discharge types could not be determined for some patients in the treatment and control groups because of missing data in the medical records. PSM aims to assemble two groups with similar characteristics with equal mean baseline data. As the groups are analyzed as a whole, not individually, the analysis was mainly balanced despite the lack of those parameters.
Secondly, the small cohort size, divided into smaller subgroups, could impede the statistical significance of the analysis. One participant from each group, G0, and G1, had a follow-up shorter than half a year, yet they did not withdraw from the treatment until the end of data collection. All information on the effect of mTORi in epilepsy control was considered relevant as few patients start mTORi treatment at such a young age. Therefore incomplete follow-up data were not excluded.
During the follow-up, the ASMs were adjusted according to the epilepsy control and thus could impact the significance of mTOR inhibitors in seizure reduction.
Despite these limitations, our study assesses the effect of mTOR inhibitor treatment on seizure control in infants and young children.
Conclusions
mTOR inhibitors are a novel promising treatment for TSC-related symptoms and conditions, including epilepsy. Young children and infants could benefit from sirolimus and everolimus use, which leads to a suppression of epileptic activity and a lower risk of refractoriness.
Adjunctive treatment with mTOR inhibitors appears to improve seizure control when administered preventively or after the onset of seizures. Further prospective clinical studies on the efficacy of mTOR inhibitors on epilepsy in young children with TSC should be performed.
References
Russo E, Citraro R, Constanti A, de Sarro G. The mTOR signaling pathway in the brain: focus on epilepsy and epileptogenesis. Mol Neurobiol. 2012;46:662–81.
Marsan E, Baulac S. Review: Mechanistic target of rapamycin (mTOR) pathway, focal cortical dysplasia and epilepsy. Neuropathol Appl Neurobiol. 2018;44:6–17.
Specchio N, Pepi C, de Palma L, Trivisano M, Vigevano F, Curatolo P. Neuroimaging and genetic characteristics of malformation of cortical development due to mTOR pathway dysregulation: clues for the epileptogenic lesions and indications for epilepsy surgery. Expert Rev Neurother. 2021;21(11):1333–45. .
Lipton JO, Sahin M. The neurology of mTOR. Neuron. 2014;84:275–91.
Saxton RA, Sabatini DM. mTOR signaling in growth, metabolism, and disease. Cell. 2017;168:960–76.
Krueger DA, Care MM, Holland K, et al. Everolimus for subependymal giant-cell astrocytomas in tuberous sclerosis. N Engl J Med. 2010;363:1801–11.
Franz DN. Everolimus: an mTOR inhibitor for the treatment of tuberous sclerosis. Expert Rev Anticancer Ther. 2011;11:1181–92.
Northrup H, Aronow ME, Bebin EM, et al. Updated international tuberous sclerosis complex diagnostic criteria and surveillance and management recommendations. Pediatr Neurol. 2021;123:50–66.
Saffari A, Brösse I, Wiemer-Kruel A, et al. Safety and efficacy of mTOR inhibitor treatment in patients with tuberous sclerosis complex under 2 years of age—a multicenter retrospective study. Orphanet J Rare Dis. 2019;14:1–13.
Sugalska M, Tomik A, Jóźwiak S, Werner B. Treatment of cardiac rhabdomyomas with mtor inhibitors in children with tuberous sclerosis complex—a systematic review. Int J Environ Res Public Health. 2021;18:4907.
Tomoto K, Fujimoto A, Inenaga C, et al. Experience using mTOR inhibitors for subependymal giant cell astrocytoma in tuberous sclerosis complex at a single facility. BMC Neurol. 2021. https://doi.org/10.1186/s12883-021-02160-5.
Hinton RB, Prakash A, Romp RL, Krueger DA, Knilans TK. Cardiovascular manifestations of tuberous sclerosis complex and summary of the revised diagnostic criteria and surveillance and management recommendations from the International Tuberous Sclerosis Consensus Group. J Am Heart Assoc. 2014;3:e001493.
Sagiv E, Chikkabyrappa S, Conwell J, Lewin M, Chun T. Use of everolimus to treat cardiac rhabdomyomas and incessant arrhythmias in a newborn: benefits and complications. Ann Pediatr Cardiol. 2022;15:58–60.
Nabbout R, Belousova E, Benedik MP, et al. Epilepsy in tuberous sclerosis complex: findings from the TOSCA Study. Epilepsia. 2019;4:73–84.
Mühlebner A, van Scheppingen J, Hulshof HM, et al. Novel histopathological patterns in cortical tubers of epilepsy surgery patients with tuberous sclerosis complex. PLoS ONE. 2016;11:e0157396.
Boer K, Crino PB, Gorter JA, et al. Gene expression analysis of tuberous sclerosis complex cortical tubers reveals increased expression of adhesion and inflammatory factors. Brain Pathol. 2010;20:704–19.
Ostendorf AP, Wong M. mTOR inhibition in epilepsy: rationale and clinical perspectives. CNS Drugs. 2015;29:91–9.
Hodges SL, Lugo JN. Therapeutic role of targeting mTOR signaling and neuroinflammation in epilepsy. Epilepsy Res. 2020;161:106282.
Canevini MP, Kotulska-Jozwiak K, Curatolo P, et al. Current concepts on epilepsy management in tuberous sclerosis complex. Am J Med Genet C Semin Med Genet. 2018;178:299–308.
Jóźwiak S, Kotulska K, Domańska-Pakieła D, et al. Antiepileptic treatment before the onset of seizures reduces epilepsy severity and risk of mental retardation in infants with tuberous sclerosis complex. Eur J Paediatr Neurol. 2011;15:424–31.
Cusmai R, Moavero R, Bombardieri R, Vigevano F, Curatolo P. Long-term neurological outcome in children with early-onset epilepsy associated with tuberous sclerosis. Epilepsy Behav. 2011;22:735–9.
Jozwiak S, Słowińska M, Borkowska J, et al. Preventive antiepileptic treatment in tuberous sclerosis complex: a long-term, prospective trial. Pediatr Neurol. 2019;101:18–25.
van der Poest CE, Jansen FE, Braun KPJ, Peters JM. Update on drug management of refractory epilepsy in tuberous sclerosis complex. Pediatr Drugs. 2020;22:73–84.
Wong M. mTOR as a potential treatment target for epilepsy. Future Neurol. 2012;7:537–45.
Zeng LH, Xu L, Gutmann DH, Wong M. Rapamycin prevents epilepsy in a mouse model of tuberous sclerosis complex. Ann Neurol. 2008;63:444–53.
Miszewska D, Sugalska M, Jóźwiak S. Risk factors associated with refractory epilepsy in patients with tuberous sclerosis complex: a systematic review. J Clin Med. 2021;10:5495.
Kotulska K, Chmielewski D, Borkowska J, et al. Long-term effect of everolimus on epilepsy and growth in children under 3 years of age treated for subependymal giant cell astrocytoma associated with tuberous sclerosis complex. Eur J Paediatr Neurol. 2013;17:479–85.
Kwan P, Arzimanoglou A, Berg AT, et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia. 2010. https://doi.org/10.1111/j.1528-1167.2009.02397.x.
National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) Common Terminology Criteria for Adverse Events (CTCAE) v5.0. 2017. https://www.meddra.org/. Accessed 29 Jan 2023.
Bissler JJ, Kingswood JC, Radzikowska E, et al. Everolimus long-term use in patients with tuberous sclerosis complex: four-year update of the EXIST-2 study. PLoS ONE. 2017;12:e0180939.
Mizuguchi M, Ikeda H, Kagitani-Shimono K, et al. Everolimus for epilepsy and autism spectrum disorder in tuberous sclerosis complex: EXIST-3 substudy in Japan. Brain Dev. 2019;41:1–10.
Franz D, Lawson J, Yapici Z, et al. Sustained seizure reduction with adjunctive everolimus for treatment-refractory seizures associated with tuberous sclerosis complex (TSC): long-term results from the phase 3 EXIST-3 study. Neurology. 2017;89:e100.
Meikle L, Pollizzi K, Egnor A, et al. Response of a neuronal model of tuberous sclerosis to mammalian target of rapamycin (mTOR) inhibitors: effects on mTORC1 and Akt signaling lead to improved survival and function. J Neurosci. 2008;28:5422–32.
Zeng L-H, Rensing NR, Zhang B, Gutmann DH, Gambello MJ, Wong M. Tsc2 gene inactivation causes a more severe epilepsy phenotype than Tsc1 inactivation in a mouse model of tuberous sclerosis complex. Hum Mol Genet. 2011;20(3):445–54.
Chu-Shore CJ, Major P, Camposano S, Muzykewicz D, Thiele EA. The natural history of epilepsy in tuberous sclerosis complex. Epilepsia. 2010;51:1236–41.
Domańska-Pakieła D, Kaczorowska M, Jurkiewicz E, Kotulska K, Dunin-Wasowicz D, Jóźwiak S. EEG abnormalities preceding the epilepsy onset in tuberous sclerosis complex patients—a prospective study of 5 patients. Eur J Paediatr Neurol. 2014;18:458–68.
Kato M, Kada A, Shiraishi H, et al. Sirolimus for epileptic seizures associated with focal cortical dysplasia type II. Ann Clin Transl Neurol. 2022;9:181–92.
He W, Chen J, Wang Y-Y, et al. Sirolimus improves seizure control in pediatric patients with tuberous sclerosis: a prospective cohort study. Seizure. 2020;79:20–6.
Overwater IE, Rietman AB, van Eeghen AM, de Wit MCY. Everolimus for the treatment of refractory seizures associated with tuberous sclerosis complex (TSC): current perspectives. Ther Clin Risk Manag. 2019;15:951–5.
French JA, Lawson JA, Yapici Z, et al. Adjunctive everolimus therapy for treatment-resistant focal-onset seizures associated with tuberous sclerosis (EXIST-3): a phase 3, randomised, double-blind, placebo-controlled study. Lancet. 2016;388:2153–63.
Jones AC, Shyamsundar MM, Thomas MW, et al. Comprehensive mutation analysis of TSC1 and TSC2—and phenotypic correlations in 150 families with tuberous sclerosis. Am J Hum Genet. 1999;64:1305–15.
Dabora SL, Jozwiak S, Franz DN, et al. Mutational analysis in a cohort of 224 tuberous sclerosis patients indicates increased severity of TSC2, compared with TSC1, disease in multiple organs. Am J Hum Genet. 2001;68:64–80.
Capal JK, Bernardino-Cuesta B, Horn PS, et al. Influence of seizures on early development in tuberous sclerosis complex. Epilepsy Behav. 2017;70:245–52.
Kotulska K, Jurkiewicz E, Domańska-Pakieła D, et al. Epilepsy in newborns with tuberous sclerosis complex. Eur J Paediatr Neurol. 2014;18:714–21.
Miller JM, Wachsman A, Haker K, Majlessipour F, Danielpour M, Puliyanda D. The effects of everolimus on tuberous sclerosis-associated lesions can be dramatic but may be impermanent. Pediatric Nephrol. 2015;30:173–7.
Hertzberg C, Belousova E, Fan P, et al. Long-term efficacy and safety of everolimus among pediatric patients with tuberous sclerosis complex (TSC) and treatment-refractory seizures: final analysis of the exist-3 study. Ann Neurol. 2018;84:S345.
Jóźwiak S, Kotulska K, Berkowitz N, Brechenmacher T, Franz DN. Safety of everolimus in patients younger than 3 years of age: results from EXIST-1, a randomized, controlled clinical trial. J Pediatrics. 2016;172:151–155.e1.
Bissler JJ, Mccormack FX, Young LR, et al. Sirolimus for angiomyolipoma in tuberous sclerosis complex or lymphangioleiomyomatosis. N Engl J Med. 2008;358(2):140–51.
Davies DM, de Vries PJ, Johnson SR, et al. Sirolimus therapy for angiomyolipoma in tuberous sclerosis and sporadic lymphangioleiomyomatosis: a phase 2 trial. Clin Cancer Res. 2011;17:4071–81.
Verhave J, Boucher A, Dandavino R, et al. The incidence, management, and evolution of rapamycin-related side effects in kidney transplant recipients. Clin Transplant. 2014;28:616–22.
Krueger DA, Capal JK, Curatolo P, et al. Short-term safety of mTOR inhibitors in infants and very young children with tuberous sclerosis complex (TSC): multicentre clinical experience. Eur J Paediatric Neurol. 2018;22:1066–73.
Acknowledgements
Funding
The study has been partly funded by grant EPIMARKER of the Polish National Center for Research and Development no. STRATEGMED3/306306/4/2016, grant VIRAP (Project number 2019/ABM/01/00034) and grant RaRE-TS (Project number 2020/ABM/01/00054) of the Medical Research Agency, Poland, and a statutory grant of the Children’s Memorial Health Institute financed by the Ministry of Science and Higher Education no. S196/2022. The publication was financed by the Medical University of Warsaw as part of the Time 2 MUW project (Agreement Number POWR.03.05.00-00-Z040/18-00).
Medical Writing and Editorial Assistance
The authors would like to thank Jagoda Głowacka-Walas, Weronika Mucha, Piotr Rycielski, and Kamil Sijko (Transition Technologies) for their assistance in the methodology design, and data analysis.
Author Contributions
Conceptualization: Dominika Śmiałek, Sergiusz Jóźwiak and Katarzyna Kotulska; Methodology: Dominika Śmiałek, Aleksandra Duda and Sergiusz Jóźwiak; Software: Aleksandra Duda and Dominika Śmiałek; Validation: Dominika Śmiałek, Sergiusz Jóźwiak and Katarzyna Kotulska; Formal analysis: Dominika Śmiałek, Aleksandra Duda and Sergiusz Jóźwiak; Investigation: Dominika Śmiałek; Resources: Sergiusz Jóźwiak and Katarzyna Kotulska; Data curation: Dominika Śmiałek, Aleksandra Duda; Writing - original draft preparation: Dominika Śmiałek; Writing - review and editing: Dominika Śmiałek, Aleksandra Duda, and Sergiusz Jóźwiak; Visualization: Dominika Śmiałek, Aleksandra Duda; Supervision: Sergiusz Jóźwiak and Katarzyna Kotulska; Project administration: Dominika Śmiałek and Sergiusz Jóźwiak; Funding acquisition: Sergiusz Jóźwiak, Katarzyna Kotulska and Dominika Śmiałek. All authors read and agreed to the published version of the manuscript.
Disclosures
The authors declare that they have no competing interests.
Compliance with Ethics Guidelines
The study was conducted according to the guidelines of the Declaration of Helsinki 1964, and the Bioethics Committee of the Medical University of Warsaw was informed of the study. Ethical approval was waived for this study as a result of the study characteristics. Patient consent was waived because of the retrospective nature of the study, minimal risk, and data anonymization.
Data Availability
The data sets generated during and/or analyzed during the current study are included as supplementary information files or are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Śmiałek, D., Kotulska, K., Duda, A. et al. Effect of mTOR Inhibitors in Epilepsy Treatment in Children with Tuberous Sclerosis Complex Under 2 Years of Age. Neurol Ther 12, 931–946 (2023). https://doi.org/10.1007/s40120-023-00476-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-023-00476-7