Abstract
Introduction
Ulotaront (SEP-363856), a dual trace animeassociated receptor 1 (TAAR1) and 5-HT1A receptor agonist, is in phase 3 clinical development for the treatment of schizophrenia. This study evaluated the comparative bioequivalence (BE) between tablet and capsule formulations of ulotaront and the food effect (FE) on pharmacokinetics (PK) of tablet form in healthy adult human subjects.
Methods
The BE study applied an open-label two-period crossover design in 24 healthy volunteers. Subjects were randomly assigned (1:1) to dosing sequence AB or BA (A, 25 mg ulotaront tablet; B, 25 mg ulotaront capsule). The FE study also used an open-label randomized two-period crossover design in 20 healthy volunteers. Subjects were fasted overnight then randomly assigned (1:1) to dosing sequence AB or BA (A, fasted condition; B, fed condition). Dosing periods were separated by 1 week for both studies. Serial plasma samples from each period were collected and analyzed by LC–MS/MS. PK parameters were calculated using Phoenix WinNonlin® software.
Results
For the BE study, geometric mean ulotaront Cmax values were 93.28 and 86.98 ng/mL for tablet and capsule, respectively. Cmax ratio was 107.25% (90% CI 101.84–112.94%). Geometric mean ulotaront area under the plasma concentration–time curve from time 0 to infinity (AUC0–∞) values were 868.8 and 829.3 ng·h/mL for tablet and capsule, respectively. AUC0–∞ ratio was 104.76% (90% CI 100.68109.01%).
For the FE study, geometric mean ulotaront Cmax was 157.89 and 157.95 ng/mL under fed and fasted conditions, respectively. Geometric mean ratio of Cmax was 99.96% (90% CI 94.48–105.77%). Geometric mean ulotaront AUC0–∞ was 1584.2 ng·h/mL fed and 1589.2 ng·h/mL fasted. Geometric mean ratio for AUC0–∞ was 99.69% (90% CI 95.02–104.58%). There was a delay in tmax (median difference 1.47 h) in the fed condition.
Conclusions
The results showed geometric mean ratios and 90% CIs for both Cmax and AUC0–∞ for ulotaront were well within typical bioequivalence criteria of 80–125% for both the BE and FE studies, thereby confirming the bioequivalence of the two dosage forms and no significant food effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Ulotaront is a novel small-molecule TAAR1 agonist with 5-HT1A receptor agonist activity currently in phase 3 clinical development under FDA-warranted Breakthrough Therapy Designation (BTD) status for the potential treatment of patients with schizophrenia |
It is important to clinically evaluate the comparative bioavailability and bioequivalence between tablet and capsule formulations of ulotaront and the effect of food co-administration on the pharmacokinetics (PK) of ulotaront in human subjects |
What was learned from the study? |
In the bioequivalence test of 25 mg tablet vs. 25 mg capsule, the geometric mean ratios and 90% CIs for both Cmax and AUC0–∞ for ulotaront were well within typical bioequivalence criteria of 80–125%, thereby confirming the bioequivalence of the two dosage forms |
The food effect study on the 50 mg tablet form of ulotaront showed no significant difference in ulotaront Cmax and AUC0–∞ under fed or fasting conditions, with a slight increase in tmax when administered with food |
There was no change in the ratio of N-desmethyl metabolite to parent drug, either between the two dosage forms or under fed versus fasted dosing conditions. The study also further confirmed that the N-desmethyl active metabolite is a minor one with 2–3% of the parent AUC |
Introduction
Ulotaront, or SEP-363856 [chemical name (7S)-4,7-dihydro-N-methyl-5H-thieno[2,3-c]pyran-7-methanamine; chemical structure is shown in Fig. 1], is a novel trace amine-associated receptor 1 (TAAR1) agonist with 5-hydroxytryptamine type 1A (5-HT1A) receptor agonist activity [1,2,3,4] discovered by Sunovion Pharmaceuticals in collaboration with PsychoGenics [1, 2]. Ulotaront is the first TAAR1 agonist to complete phase 2 clinical trials in patients with schizophrenia. Unlike the current class of antipsychotics, ulotaront does not confer its efficacy via dopamine D2 or 5-HT2a receptor blockade and may represent a new class for the treatment of schizophrenia. The safety and effectiveness of ulotaront has been demonstrated in an acute 4-week and 26-week open-label extension study in patients with schizophrenia [4,5,6,7]. Ulotaront has received Breakthrough Therapy Designation by the US Food and Drug Administration (FDA) for the potential treatment of patients with schizophrenia [9, 10] and it is currently in phase 3 clinical development [8].
Chemical structures of a ulotaront (SEP-363856; MW 183.27) and b N-desmethyl metabolite (SEP-363854; MW 169.25). Reproduced from ref. [12] with permission
Ulotaront is a highly soluble and highly permeable small-molecule compound with good brain penetration and low protein binding and has been designated as a Biopharmaceutics Classification System (BCS) Class I compound by the US FDA [11]. A single active metabolite, N-desmethyl, of ulotaront has been identified on the basis of in vitro and in vivo studies with ulotaront [11]. A fully validated high-performance liquid chromatography coupled with tandem mass spectrometry (LC–MS/MS) method with a lower limit of quantitation (LLOQ) of 0.0200 ng/mL has been established for both ulotaront and the active metabolite N-desmethyl (SEP-363854 or M11A, chemical structure shown in Fig. 1b) in human plasma [12]. Phase 1 clinical studies showed that ulotaront is rapidly absorbed with dose-proportional plasma exposure in the therapeutic dose range of 10–100 mg. The peak plasma concentration occurs approximately 3 h post-dose, and the median effective half-life is 7 h. A population pharmacokinetics (PK) analysis found no meaningful effects of race, age, sex, formulation, or clinical status (patient versus healthy) on ulotaront PK; body weight was the only meaningful covariate [13]. Phase 1 studies also determined that the N-desmethyl metabolite is a minor metabolite in humans with an approximate metabolite/parent area under the plasma concentration–time curve (AUC) ratio of 2–3% [12].
Early clinical trials of ulotaront used a capsule formulation. The absolute bioavailability of ulotaront was not clinically assessed in the past. To further support the clinical development of ulotaront, a comparative bioequivalence (BE) study between the capsule and a tablet formulation was conducted in healthy human volunteers. In addition, a food effect (FE) study was performed in healthy subjects using the ulotaront tablet formulation. Both studies were designed, conducted, and analyzed according to the corresponding FDA Guidance documents for BE and FE studies [14, 15]. The findings from the two studies are reported herein.
The main purposes of the current study are to clinically evaluate the comparative bioavailability and bioequivalence between tablet and capsule formulations of ulotaront and the effect of food co-administration on the pharmacokinetics (PK) of ulotaront in human subjects.
Methods
Clinical Trial Design
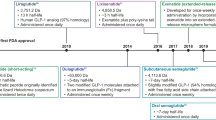
The BE (SEP361-111) study design is depicted in Fig. 2a. The study was an open-label and randomized two-period crossover in 24 healthy adult male and female subjects. Subjects were randomly assigned to one of two treatment sequences, AB or BA, where A was the 25 mg ulotaront tablet, and B was the 25 mg ulotaront capsule. Twelve adult subjects were planned to receive each treatment sequence. The randomization ensured that the two treatment sequences were balanced within gender. An attempt was made to enroll at least one-third of the subjects as male and one-third as female individuals. To minimize the possibility of carryover effects and to allow for complete elimination of ulotaront from the plasma, the second treatment was preceded by a 7-day washout period (postdose day 1 through the end of day 7). For each dosing period, blood samples for determination of plasma ulotaront and metabolite concentrations were collected at predose and at 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, 24, 48, 72, 96, 120, and 144 h postdose using K2-EDTA-coated tubes. For each time point, 6 mL of blood was collected, and then centrifuged to harvest plasma. Prior to analysis, plasma samples were stored at − 20 °C or lower temperature.
The FE (SEP361-117) study design is depicted in Fig. 2b. The study used an open-label randomized two-period crossover design to quantify the effect of food co-administration on the PK of a single oral dose of 50 mg ulotaront tablet in healthy adult male and female subjects. Twenty subjects were enrolled in the study and were dosed on day 1 and day 8 based on random assignment to one of two single-dose treatment sequences (fed followed by fasted, or vice versa). There was a 7-day washout period between the two treatments to mitigate the potential for carryover effects and to ensure complete elimination of ulotaront from plasma prior to the second treatment. For administration of study drug under fed condition, subjects received a high fat meal (800–1000 kcal with 500–600 kcal from fat) 30 min before dosing. For administration under fasted conditions, subjects were fasted overnight and through the first 4 h after the morning dose administration. For each dosing period, blood samples for plasma ulotaront and metabolite concentration measurement were collected at predose and at 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, 24, 48, 54,72, 78, and 96 h postdose using K2-EDTA-coated tubes. For each time point, 6 mL of blood was collected, and then centrifuged to harvest plasma. Prior to analysis, plasma samples were stored at − 20 °C or lower temperature.
The study drugs used in the BE study include the ulotaront capsules of 25 mg (size #0, Swedish Orange capsule), the ulotaront tablet of 25 mg (green, round, biconvex film-coated tablet, 9.5 mm). For the FE study, the ulotaront tablets of 50 mg (equivalent to 60 mg of its hydrochloride salt form) yellow oval shape film-coated tablets were used.
The washout period between the two treatments was determined on the basis of the elimination half-life (t1/2) information from previous single ascending dose (SAD) study, where at 25 mg and 50 mg dose the observed longest t1/2 is 25.6 h [12]. The washout duration was set for at least five times of the elimination half-life (5 × t1/2), thus a 7-day washout period was implemented to minimize the possibility of carryover effects.
The clinical protocol and the informed consent form (ICF) were reviewed and approved by an institutional review board (IRB) (for the BE study, Integerview IRB in Austin TX; for the FE study, Salus IRB in Austin TX). The clinical studies were designed and conducted in compliance with Good Clinical Practice (GCP) and in accordance with the Declaration of Helsinki.
Study Population and Inclusion/Exclusion Criteria
For the BE study, healthy adult male and female subjects, 18–55 years old (inclusive), with a body mass index (BMI) between 16 and 32 kg/m2 (inclusive) were enrolled in the study. Subjects had to be willing and able to comply with the study procedures and visit schedules and stay within the clinical study for the required period. The study actually enrolled 12 male subjects and 12 female subjects with age range of 21–49 (mean 32.3 and median 30.5) years old. The detailed demographic data is provided in the Supplementary Information Sect. 1.1. Detailed subject inclusion and exclusion criteria are provided in Supplementary Information Sect. 1.2 and 1.3, respectively.
For the FE study, healthy adult male or female subjects, 18–55 years old (inclusive), with a body mass index (BMI) between 18 and 32 kg/m2 (inclusive) were enrolled in the study. Subjects were to be in general good health based on screening physical examination, medical history, 12-lead ECG, and clinical laboratory evaluations (congenital nonhemolytic hyperbilirubinemia [e.g., Gilbert’s syndrome] was not acceptable) at screening as assessed by the investigator (or designee). Subjects were excluded if they had a disorder, history of a condition, or previous gastrointestinal surgery (e.g., cholecystectomy, vagotomy, bowel resection) that could have interfered with drug absorption, distribution, metabolism, excretion, gastrointestinal motility, or gastrointestinal pH; or a history of malabsorption (appendectomy and hernia repair were acceptable). This study actually enrolled 11 male subjects and 9 female subjects with age range of 20–53 (mean 38.7, median 37.5) years old. The detailed demographic data is provided in the Supplementary Information Sect. 2.1. Detailed subject inclusion and exclusion criteria are provided in Supplementary Information Sect. 2.2 and 2.3, respectively.
Bioanalytical LC–MS/MS Methods for Pharmacokinetic Sample Measurements
A fully validated LC–MS/MS method with the curve range of 0.0200–20.0 ng/mL using 0.200 mL plasma [12] was used for plasma PK sample analysis for both studies. To better cover the sample concentration range, the above method with extension to a higher curve range (0.250–250 ng/mL) by minimal modifications was also fully validated following FDA guidance [16]. Reference standards of ulotaront hydrochloride (MW 219.73) with chemical purity of 99.4% and N-desmethyl metabolite (also as its hydrochloride form, MW 205.71) with chemical purity of 98.0% (both were supplied by Sunovion, Marlborough, MA, USA) were used for preparation of calibration standards and quality control (QC) samples. Deuterated-materials ulotaront-d3 and M11A-d4 (also provided by Sunovion) were used as respective internal standards (IS). Blank human plasma with K2-EDTA anticoagulant was obtained from Bioreclamation (Westbury, NY, USA) and stored at − 20 °C. Waters Oasis MCX (30 µm, 10-mg) 96-well plates (Medford, MA, USA) were used for solid phase extraction (SPE) of plasma samples.
The detailed plasma extraction is described elsewhere [12]. In brief, an aliquot of 0.200 mL (or 0.100 mL for the high curve range) sample, after being mixed with 25 µL of the combined IS working solution, was diluted with 0.20 mL of 1% formic acid, then loaded onto the SPE plate that was pre-conditioned with 0.30 mL methanol followed by 0.30 mL water. After the sample passed through the cartridge it was then washed with 0.50 mL 1% formic acid followed by 0.50 mL methanol. Once the wash solvent went through the cartridge, the maximum positive pressure was applied to dry the cartridge (for at least 1 min). Finally, the analytes were eluted with 0.30 mL 2% NH4OH in methanol (v/v) into a clean plate. The solvent was evaporated at 45 °C under a stream of nitrogen (approx. 50 L/min) in the SPE Dry-96 sample concentrator for approximately 20 min. The dried residue was reconstituted with 0.20 mL 1% formic acid in 5:95 methanol–water (v/v) by vortex-mixing for 1 min. A 10-µL aliquot (or 6 µL for the high curve range) of the resulting sample was injected for LC–MS/MS analysis.
Chromatographic separation was performed on a Shimadzu (Kyoto, Japan) LC system consisting of an LC-20AD mobile phase delivery system, CTO-20AC column oven, and SIL-20AC Prominence autosampler utilizing a Phenomenex Synergi 4u Polar-RP, 80A column (50 × 2.0 mm, 4 µm particle size) coupled with a Supelco 0.5-µm prefilter using a gradient mobile phase (mobile phase A was 0.1% formic acid in water, and mobile phase B was methanol–ACN (50:50, v/v)). MS/MS detection was performed on a Sciex API 5000 by monitoring m/z 184.1 → 135.0 for ulotaront, 170.1 → 135.0 for SEP-363854, 187.1 → 135.0 for IS1, and 174.1 → 94.0 for IS2. The collision energies were 26, 23, 26, and 38 eV for ulotaront, SEP-363854, IS1, and IS2, respectively. Data acquisition and peak integration were processed by Analyst® Software (version 1.4.1 or higher) from Applied Biosystems-Sciex (Foster City, CA).
For PK sample analysis, all samples (except for predose and the samples expected to be below 0.250 ng/mL exposure) were first analyzed by the high curve range method. Those samples with initial analysis of below 0.250 ng/mL concentration and other expected low concentration samples were analyzed by the more sensitive low curve range method. Therefore, the analytical limit of quantitation was 0.0200 ng/mL for both ulotaront and the metabolite for these two clinical studies. Any data presented as BLQ (below limit of quantitation) in this manuscript means lower than 0.0200 ng/mL. During the sample analysis, an effort was made to analyze the samples from two dosing periods for an individual subject in the same analytical run as long as possible to minimize the potential impact from run-to-run variation.
Pharmacokinetic Assessments
Plasma ulotaront concentration data were used to calculate PK parameters for each study subject and treatment condition by noncompartmental analysis using actual elapsed time from dosing. PK calculations were performed using Phoenix WinNonlin® software (Version 8.3, Certara USA, Inc.). Key PK parameters including Cmax, AUC0–∞, AUC0–last, t1/2, tmax, CL/F, Vz/F, etc. were obtained for the capsule and tablet comparative BE study and the FE study.
Statistical Analysis
The statistical analysis of the work presented here was performed using SAS® Version 9.4 statistical software (SAS Institute Inc., Cary, NC, USA). The relative bioavailability was assessed for ulotaront Cmax and AUC0–∞ between two dosage forms (tablet versus capsule; tablet as test, capsule as reference). A linear mixed-effect model was fitted with the natural logarithm of the PK parameter as the dependent variable, dosage form, sequence, and period as fixed effects, and subject nested within sequence as a random effect. The number of observations used in the model and p values for the fixed effects (dosage form, sequence, period) were presented as obtained from the model. The geometric mean for each dosage form was computed by exponentiating the given least-squares (LS) mean obtained from the model for the given dosage form. The %mean ratio was computed by exponentiating the difference in LS means between dosage forms obtained from the model and then multiplying by 100. The 90% CI of the %mean ratio was obtained by exponentiating the endpoints of the 90% CI of the difference in LS means obtained from the model and multiplying each by 100. The determination of relative bioavailability was accomplished by analysis of the 90% CI for the %mean ratio of the tablet dosage form compared to the capsule dosage form for both ulotaront Cmax and AUC0–∞. Average bioequivalence was established if the 90% CI was completely contained in the 80–125% interval. The relative bioavailability results between tablet and capsule formulations are summarized in Table 2. The FE data were analyzed similar to the BE data. For FE assessment, the comparison of the two dosing conditions, i.e., fed and fasted (fed as test, and fasted as reference) and statistical analysis were preformed and the tmax and tlag were also evaluated. The relative bioavailability results obtained under fed and fasted conditions are summarized in Table 5.
Results and Discussion
Ulotaront Dose Selection and Sample Size Determination
Ulotaront Dose Selection
For the comparative BE study, a single oral dose (capsule and tablet) of 25 mg ulotaront was selected. This dose represents one dose level below the maximum tolerated dose (MTD) defined in healthy adult male subjects in a previous SAD study. In the SAD, changes in exposures with increase in dose (5–125 mg) for ulotaront approximated dose proportionality [12]. In addition, the 25 mg dose has been evaluated as the starting dose in clinical trials for the subjects with schizophrenia.
For the FE study, a single dose of 50 mg ulotaront was administrated in each study period. Ulotaront 50 mg represents the MTD in the healthy adult subjects. On the basis of the results from previous studies, the anticipated potential risks of ulotaront are amenable to detection via safety monitoring consisting of AEs, vital signs, ECGs, clinical laboratory values, and physical examinations. Across all clinical studies during the clinical development program, oral administration of ulotaront was generally well tolerated. In addition, this study was conducted under hospitalization with careful safety monitoring.
Sample Size Determination
For the BE study, the sample size was determined statistically to show bioequivalence between the tablet dosage form versus capsule dosage form using a paired equivalence test (two sided). It was conducted on the log scale with an equivalence criterion of 80–125% for the mean treatment ratio of both AUC0–∞ and Cmax. The input estimates for between- and within-subject variability were obtained from a previously completed study. The assumed common coefficient of variation is 30%, and correlation coefficient is 0.50. The expected mean ratio for both parameters is 1 between tablet and capsule. It was determined that a sample size of 20 subjects would be required. The number of subjects planned would provide 90% power to demonstrate the ratio of the means within 0.80 and 1.25 for each parameter and at least 80% for both primary endpoints. To account for potential early dropout, a total of 24 were enrolled at the beginning of the study.
For the FE study, approximately 24 subjects were dosed in order that 20 subjects complete the study. This sample size has above 90% power to reject the null hypothesis that the ratio of test mean to the reference mean is below 0.80 or above 1.25 for the primary endpoints, assuming that the expected ratio of the means is within 5%, the SD difference (log scale) is 0.212, with one-sided alpha at the 5% level.
LC–MS/MS Method Validation Summary and Pharmacokinetic Sample Analysis Performance
LC–MS/MS Method Validation
As stated in Sect. “Bioanalytical LC–MS/MS Methods for Pharmacokinetic Sample Measurements”, a highly sensitive LC–MS/MS method with an LLOQ of 0.0200 ng/mL was first validated, and the full validation results together with the sample storage stability data for up to 730 days (at − 20 °C and − 70 °C) were presented in our recent publication [12]. On the basis of the dose levels used in these studies and the PK results from the previous SAD study [12], a new and higher curve range (0.250–250 ng/mL) method using 0.100 mL plasma was also validated. For this high curve range method, all the analytical procedures remained unchanged from the low curve range method except for reducing the plasma volume to half and lowering the injection volume to 6 µL. Both curve range methods have demonstrated acceptable linearity (r2 ≥ 0.99) and intra-day and inter-day precision and accuracy (CV ≤ 15% and RE within ± 15% for regular QC samples; CV ≤ 20% and RE within ± 20% for LLOQ QC samples). For the high curve range, so far sample storage stability has been established for at least 582 days at − 20 °C and 806 days at − 70 °C.
Pharmacokinetic Sample Analysis for Tablet and Capsule Comparison Study
For the BE study, a total of 768 plasma samples were analyzed for ulotaront and SEP-363854 concentrations within the established stability period. Eighty-eight samples, i.e., about 11.5% of the total number of samples, were chosen for incurred sample reanalysis (ISR) evaluation to confirm the reproducibility of the assay. The study samples were successfully analyzed in a total of 17 analytical runs. For ulotaront, calibration curves had liner correlation coefficient (r2 ranging from 0.9910 to 0.9996), QC sample precisions (%CV) were 3.8–8.1% for high range assay (n = 14) and 4.2–7.2% for low range (n = 20), and QC accuracies (%RE) were − 0.5% to 1.6% for high range (n = 14) and 0.3–7.5% for low range (n = 20), respectively. For the metabolite SEP-363854, calibration curves had linear correlation coefficient (r2 ranging from 0.9927 to 0.9994), QC sample precisions were 1.9–5.8% for high range assay (n = 14) and 4.3–7.0% for low range (n = 18), and QC accuracies were 3.0–11.0% for high range (n = 14) and 0.2–8.0% for low range (n = 18), respectively. ISR evaluation showed that for ulotaront, 81 out of 88 samples, i.e., 92%, and for the metabolite SEP-363854, 86 out of 87 samples, i.e., 98.6%, met the acceptance criterion (repeat and initial results agreed within 20%). The above results demonstrated the acceptable assay performance for the BE study.
PK Sample Analysis for Food Effect Study
For the FE study, a total of 624 plasma samples were assayed for ulotaront and SEP-363854 concentrations within the available stability. About 10% of the samples from the high curve range assayed samples were chosen for ISR evaluation to confirm the reproducibility of the assay. The study samples were successfully analyzed in a total of 16 analytical runs. For ulotaront, calibration curves had liner correlation coefficient (r2 ranging from 0.9936 to 0.9991), QC sample precisions (%CV) were 3.3–6.9% for high range assay (n = 16) and 2.8–4.9% for low range (n = 14), and QC accuracies (%RE) were − 3.5% to 3.2% for high range (n = 16) and − 7.7% to 4.7% for low range (n = 14), respectively. For the metabolite SEP-363854, calibration curves had linear correlation coefficient (r2 ranging from 0.9933 to 0.9997), QC sample precisions were 3.6–8.0% for high range assay (n = 16) and 3.3% to 8.7% for low range (n = 16), and QC accuracies were − 6.0% to 2.8% for high range (n = 16) and − 11.9% to 0.0% for low range (n = 16), respectively. ISR results showed that for ulotaront 30 out of 32 samples, i.e., 93.8%, and for the metabolite SEP-363854, 31 out of 32 samples, i.e., 96.9%, met the acceptance criterion. These results also indicated the excellent assay performance for the FE study.
Pharmacokinetic Comparison Between Tablet and Capsule Treatments
In the tablet–capsule BE study, all 24 enrolled subjects completed the study and were included in the safety and PK populations. There were no early terminations and no missing PK samples from the study. Mean ulotaront plasma concentration versus time profiles of both the tablet and capsule formulations are presented in Fig. 3a, b. Obtained PK parameters including Cmax, AUC0–∞, AUC0–last, t1/2, tmax, CL/F, and Vz/F are presented in Table 1 and statistical relative bioavailability comparisons are shown in Table 2. The ulotaront Cmax and AUC0–∞ comparisons (percent ratio of tablet versus capsule) between the two formulations are shown in Fig. 4. Mean metabolite SEP-363854 concentration vs. time profiles of both formulations are presented in Fig. 3c, d. PK parameters of the metabolite between two formulations and the metabolite Cmax and AUC0–∞ ratio to parent are summarized in Table 3.
Ulotaront Cmax and AUC0–∞ comparison between the two formulations (tablet vs. capsule). Note: filled circle = Cmax geometric mean ratio (%), filled square = AUC0–∞ geometric mean ratio (%); bars are the upper and lower 90% confidence interval of the geometric mean ratio (%). The capsule was used as the reference for the comparison
Pharmacokinetic Analysis and Comparison for Ulotaront Between Two Formulations
As shown in Fig. 3a, b, the mean ulotaront plasma concentration–time curves obtained from the treatment of tablet and capsule formulations were nearly superimposable. As presented in Table 1, mean Cmax and AUC0–∞ were 95.06 ng/mL and 906 ng·h/mL for tablet treatment, and 88.82 ng/mL and 873 ng·h/mL for capsule treatment, respectively. The elimination half-lives (t1/2) were 11.9 h and 11.8 h for tablet and capsule treatments, respectively. The apparent clearance (CL/F) and the apparent volume of distribution (Vz/F) were 30.0 L/h and 476 L for tablet treatment, and 31.6 L/h and 508 L for capsule treatment. Median tmax was 2.00 h and 3.00 h for tablet and capsule treatments, respectively. These results indicated that both tablet and capsule treatments had very similar exposure and clearance. These results are also in good agreement with those previously reported for the 25 mg dose of ulotaront in human subjects [12, 13]. To evaluate the bioequivalence of the two dosage forms, geometric mean Cmax and AUC0–∞ of each formulation, geometric mean ratio of Cmax and AUC0–∞ between two formulations (tablet/capsule), and 90% CI of geometric mean ratios were calculated and summarized in Table 2. The geometric mean Cmax was 93.28 ng/mL (tablet) and 86.98 ng/mL (capsule), and the Cmax ratio was 107.25% with 90% CI of 101.84–112.94%; the geometric mean AUC0–∞ was 868.8 ng·h/mL (tablet) and 829.3 ng·h/mL (capsule), and AUC0–∞ ratio was 104.76% with 90% CI of 100.68–109.01%. Both Cmax and AUC0–∞ were well within the bioequivalence criteria of 80–125% [14]. Thus, the two dosage forms were deemed bioequivalent. The PK characteristics of ulotaront reported herein are consistent with those expected for a BCS Class I molecule [11, 17].
Metabolite SEP-363854 Pharmacokinetic Comparison Between Two Formulations
The bioanalytical method used was able to simultaneously obtain the plasma concentrations of ulotaront and its N-desmethyl metabolite SEP-363854 (an active metabolite). The metabolite concentration versus time profiles for the two formulation treatments are given in Fig. 3c (linear scale) and Fig. 3d (semi-log scale). The PK parameters of this metabolite are presented in Table 3. For the tablet treatment, mean Cmax, AUC0–∞, tmax, and t1/2 were 1.49 ng/mL, 20.08 ng·h/mL, 3.58 h, and 8.41 h, respectively; for the capsule treatment, mean Cmax, AUC0–∞, tmax, and t1/2 were 1.41 ng/mL, 19.13 ng·h/mL, 3.75 h, and 8.03 h, respectively. The Cmax geometric mean ratio of tablet/capsule was 105.80% and the AUC0–∞ geometric mean ratio was 105.46%. The above data showed that the exposure and other major PK parameters of this metabolite were highly comparable between the tablet and the capsule. In addition, the metabolite (to parent) ratios of Cmax and AUC0–∞ were nearly identical between two formulations [MRCmax = 0.0170 (tablet) and 0.0172 (capsule); MRAUC0–∞ = 0.0251 (tablet) and 0.0250 (capsule)], indicating no impact on the metabolism of ulotaront by switching dosage form from capsule to tablet. The metabolite ratio results obtained from this study further confirmed that the N-demethylation is a minor metabolic pathway for ulotaront, which is consistent with the finding in the first-in-human study [12].
Pharmacokinetic Comparison Between Fed and Fasted Conditions
For the FE study, 20 subjects were enrolled, and 19 completed both treatment periods. The primary PK analysis was based on ulotaront Cmax and AUC0–∞. Mean ulotaront plasma concentration versus time profiles under fed and fasted conditions are depicted in Fig. 5a, b. Derived PK parameters are presented in Table 4. For food effect assessment, only subjects with data for the given parameters for both treatment conditions were included, N = 18. The food effect on the PK results such as Cmax, AUC0–∞, tmax, and tlag are summarized in Table 5. Among 19 completers one subject had emesis within two times the median tmax during the fasted condition treatment period, and this subject was excluded from the FE comparison. The ulotaront Cmax and AUC0–∞ comparisons between the fed and fasted dosing conditions are shown in Fig. 6. Mean metabolite SEP-363854 concentration versus time profiles under both fed and fasted conditions are presented in Fig. 5c, d. PK parameters for the metabolite between the two dosing conditions and the metabolite exposure (Cmax and AUC0–∞) ratios to parent are summarized in Table 6.
Pharmacokinetic Analysis and Comparison of Ulotaront Under Fed and Fasted Conditions
As shown in Fig. 5a, b, the mean ulotaront PK profiles comparing fed and fasted conditions substantially overlap. Major PK parameters found from this FE study, as summarized in Table 4, are also similar to those reported previously for the 50 mg dose of ulotaront in human subjects [12, 13]. As shown in Table 5, the geometric mean of Cmax for ulotaront was calculated as 157.89 ng/mL (fed) and 157.95 ng/mL (fasted). The geometric mean of AUC0–∞ was calculated as 1584.2 ng·h/mL (fed) and 1589.2 ng·h/mL (fasted). When the fasted condition was used as the reference, the geometric mean ratio of ulotaront Cmax (fed/fasted) was 99.96% (90% CI 94.48–105.77%), and geometric mean ratio of ulotaront AUC0–∞ (fed/fasted) was 99.69% (90% CI 95.02–104.58%). As shown in Table 5, the median tmax increased by 1.47 h in the fed state versus fasted, but there was no noticeable change in lag time tlag for appearance of the first quantifiable ulotaront concentration. The 90% CIs for both Cmax and AUC0–∞ of ulotaront when comparing fed to fasted condition were well within the bioequivalence range of 80–125% [15]. Thus, there was no significant impact of high fat meal co-administration on ulotaront plasma exposure (Cmax and AUC0–∞), though there was a slight increase in tmax in the fed state as compared to the fasted state.
Metabolite SEP-363854 Pharmacokinetic Comparison Under Fed and Fasted Conditions
The metabolite SEP-363854 concentration versus time profiles obtained under fed and fasted conditions are plotted in Fig. 5c (linear scale) and Fig. 5d (semi-log scale). The PK parameters of the metabolite are summarized in Table 6. Mean exposure parameters (Cmax and AUC0–∞) were 3.08 ng/mL and 40.3 ng·h/mL in the fed condition and 3.25 ng/mL and 41.0 ng·h/mL in the fasted condition, respectively. The Cmax ratio of fed/fasted was 94.77% and the AUC0–∞ ratio was 98.29%. There was no difference in median tmax between treatment conditions (median tmax was 6.00 h for both dosing conditions). Metabolite to parent ratios (MRCmax and MRAUC0–∞) were 0.0209 and 0.0266 in the fed condition, and 0.0217 and 0.0277 in the fasted condition, respectively, indicating that SEP-363854 is a minor metabolite, and there was no change in exposure between fed and fasted treatment conditions.
Summary of Tablet vs. Capsule Bioequivalence Study and Food Effect Study
On the basis of the results presented above, ulotaront plasma exposure (i.e., geometric means Cmax and AUC0–∞) was similar when comparing tablet vs. capsule formulations, and the 90% CIs of the geometric mean ratios for ulotaront Cmax and AUC0–∞ were contained within the bioequivalence limits of 80–125% recommended by FDA Guidance [14]. Other PK parameters for both the tablet and the capsule were also comparable. Thus, it can be concluded that the two dosage forms are bioequivalent. The PK parameters for the active metabolite SEP-363854 for the two dosage forms were comparable to one another, implying no formulation effect on the metabolism of ulotaront.
For the FE study, PK results showed that the geometric mean ratios (fed/fasted) for ulotaront Cmax and AUC0–∞ were 94.48–105.77% (90% CI) and 95.02–104.58% (90% CI), respectively, and both parameters were well within the predefined equivalence limit of 80–125%, demonstrating there is no food effect on ulotaront PK. A slight delay in tmax in the fed condition was likely due to the effect of the meal on the rate of gastric emptying. The results also showed that food co-administration had no effect on metabolism of ulotaront to its only active metabolite, SEP-363854. The metabolite-to-parent exposure ratio in both BE and FE dosing scenarios was 2–3%, indicating that N-desmethyl is a minor metabolite of ulotaront in humans. The PK results observed for ulotaront in this study are consistent with those of a BCS Class I compound.
Conclusion
In the bioequivalence test of 25 mg tablet vs. 25 mg capsule, the geometric mean ratios and 90% CIs for both Cmax and AUC0–∞ for ulotaront were well within typical bioequivalence criteria of 80–125%, thereby confirming the bioequivalence of the two dosage forms. This is consistent with ulotaront as a BCS Class I compound. Moreover, a food effect study on the 50 mg tablet form of ulotaront showed no difference in ulotaront Cmax and AUC0–∞ under fed or fasting conditions, with a slight increase in tmax when administered with food.
References
Heffernan MLR, Herman LW, Brown S, et al. Ulotaront: A TAAR1 agonist for the treatment of schizophrenia. ACS Med Chem Lett. 2022;13:92–8.
Dedic N, Jones P, Hopkins SC, et al. SEP-363856, a novel psychotropic agent with a unique, non-D2 receptor mechanism of action. J Pharmacol Exp Ther. 2019;371:1–14.
Dedic N, Dworak H, Zeni C, Rutigliano G, Howes OD. Therapeutic potential of taar1 agonists in schizophrenia: evidence from preclinical models and clinical studies. Int J Mol Sci. 2021;22:13185. https://doi.org/10.3390/ijms222413185.
Koblan KS, Kent J, Hopkins SC, et al. A non-D2-receptor-binding drug for the treatment of schizophrenia. N Engl J Med. 2020;382:1497–506.
Koblan KS, Hopkins SC, Kent J, Cheng H, Goldman R, Loebel A. Efficacy and safety of SEP-363856, a novel psychotropic agent with a non-D2 mechanism of action, in the treatment of schizophrenia. CNS Spectr. 2020;25:287–8.
https://clinicaltrials.gov/ct2/show/NCT02969382. A 4-week, randomized, double-blind, parallel-group, placebo-controlled, flexibly-dosed, multicenter Study to evaluate the efficacy and safety of SEP-363856 in acutely psychotic adult subjects with schizophrenia. ClinicalTrials.gov Identifier NCT02969382.
Correll CU, Koblan KS, Hopkins SC, et al. Safety and effectiveness of ulotaront (SEP-363856) in schizophrenia: results of a 6-month, open-label extension study. npj Schizophrenia. 2021;7:63. https://doi.org/10.1038/s41537-021-00190-z.
https://clinicaltrials.gov/ct2/show/NCT04072354. A randomized, double-blind, parallel-group, placebo-controlled, fixed-dose, multicenter study to evaluate the efficacy and safety of SEP-363856 in acutely psychotic subjects with schizophrenia. ClinicalTrials.gov Identifier NCT04072354 (another phase 3 study with higher dose is also ongoing under Identifier INCT04092686).
Bloomberg. Sunovion and PsychoGenics announce that SEP-363856 has received FDA breakthrough therapy designation for the treatment of people. https://www.bloomberg.com/press-releases/2019-05-10/sunovion-and-psychogenics-announce-that-sep-363856-has-received-fda-breakthrough-therapy-designation-for-the-treatment-of-people. May 10, 2019. Accessed 20 Jan 2023
https://en.wikipedia.org/wiki/SEP-363856. Accessed 20 Jan 2023
Xiao G, Chen YL, Dedic N, Xie L, Koblan KS, Galluppi GR. In vitro ADME and preclinical pharmacokinetics of ulotaront, a TAAR1/5-HT1A receptor agonist for the treatment of schizophrenia. Pharm Res. 2022;39(5):837–50.
Chen YL, Shi Y, LaFayette A, Shi L, Koblan KS, Galluppi GR. A sensitive LC–MS/MS method for simultaneous quantification of ulotaront and its N-desmethyl metabolite in human plasma and application to a clinical study. J Pharm Biomed Anal. 2021;207. https://doi.org/10.1016/j.jpba.2021.114404.
Galluppi GR, Polhamus DG, Fisher JM, Hopkins SC, Koblan KS. Population pharmacokinetic analysis of ulotaront in subjects with schizophrenia. CPT Pharmacometrics Syst Pharmacol. 2021. https://doi.org/10.1002/psp4.12692.
US Department of Health and Human Services Food and Drug Administration, Center for Drug Evaluation and Research (CDER). Guidance for Industry Bioavailability and Bioequivalence Studies Submitted in NDAs or INDs—General Considerations, March 2014. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/bioavailability-and-bioequivalence-studies-submitted-ndas-or-inds-general-considerations. Accessed 20 Jan 2023
US Department of Health and Human Services Food and Drug Administration, Center for Drug Evaluation and Research (CDER). Guidance for Industry Food-Effect Bioavailability and Fed Bioequivalence Studies, December 2002. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/food-effect-bioavailability-and-fed-bioequivalence-studies. Accessed 20 Jan 2023
US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER). Guidance for Industry Bioanalytical Method Validation, May 2018. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/bioanalytical-method-validation-guidance-industry. Accessed 20 Jan 2023
US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER). Guidance for Industry M9 Biopharmaceutics Classification System-Based Biowaivers, May 2021. https://www.fda.gov/drugs/guidance-compliance-regulatory-information/guidances-drugs. Accessed 20 Jan 2023
Acknowledgements
We thank the participants of the study. The authors are also grateful to Covance Bioanalytical Laboratories in Madison Wisconsin for performing the PK sample measurement. Sunovion discovered ulotaront in collaboration with PsychoGenics based in part on a mechanism-independent approach using the in vivo phenotypic SmartCube® platform and associated artificial intelligence algorithms.
Funding
This work was fully funded and supported by Sunovion Pharmaceuticals Inc. The Open Access fee is also paid by the Sunovion Pharmaceuticals Inc.
Author Contributions
All the authors, i.e., Yu-Luan Chen, Hironobu Tsukada, Snezana Milanovic, Lei Shi, Yan Li, Yongcai Mao, Kenneth S. Koblan, and Gerald R. Galluppi, have contributed to the writing and review of this manuscript. Yu-Luan Chen and Lei Shi have also been managing all pharmacokinetic sample analysis. Yan Li and Yongcai Mao have contributed to statistical analysis for the presented studies.
Disclosures
The authors have declared no conflicts of interest. Yu-Luan Chen, Hironobu Tsukada, Snezana Milanovic, Lei Shi, Yan Li, Yongcai Mao, Kenneth S. Koblan, and Gerald R. Galluppi are employees of Sunovion Pharmaceuticals Inc.
Compliance with Ethics Guidelines
The BE study SEP361-111, including the final version of the subject informed consent form (ICF), was approved by the Integerview IRB (3815 S Capital of Texas Hwy #320, Austin, TX 78,704) by Dr. Alexander Kenaston. The FE study SEP361-117, including the final version of the subject ICF, were approved by the IRB (Salus IRB 2111 W. Braker Lane, Suite 100, Austin, TX, USA 78,758) chaired by Dr. Alexander Kenaston. Both clinical studies were conducted according to protocol, ICH Good Clinical Practice (GCP), ICH guidelines, and the ethical principles that have their origin in the Declaration of Helsinki. Both studies were conducted at PPD Development LLC at Austin TX, and Dr. LuAnn Bundrant and Dr. Rebecca N. Wood-Horrall served as principal investigator for SEP361-111 and SEP361-117, respectively.
Data Availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author (Yu-Luan Chen) on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chen, YL., Tsukada, H., Milanovic, S. et al. Comparative Bioequivalence of Tablet and Capsule Formulations of Ulotaront and the Effect of Food on the Pharmacokinetics of the Tablet Form in Humans. Neurol Ther 12, 815–832 (2023). https://doi.org/10.1007/s40120-023-00459-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-023-00459-8