Abstract
Introduction
Self-injectable calcitonin gene-related peptide (CGRP) monoclonal antibody (mAb) auto-injectors and non-CGRP oral medications are currently available for migraine prevention in Japan. This study elicited the preferences for self-injectable CGRP mAbs and non-CGRP oral medications and determined differences in the relative importance of auto-injector attributes for patients and physicians in Japan.
Methods
Japanese adults with episodic (EM) or chronic (CM) migraine and physicians who treat migraine completed an online discrete choice experiment (DCE), asking participants to choose a hypothetical treatment they preferred between two self-injectable CGRP mAb auto-injectors and a non-CGRP oral medication. The treatments were described by seven treatment attributes, with attribute levels varying between questions. DCE data were analyzed using a random-constant logit model to estimate relative attribution importance (RAI) scores and predicted choice probabilities (PCP) of CGRP mAb profiles.
Results
A total of 601 patients (79.2% with EM, 60.1% female, mean age: 40.3 years) and 219 physicians (mean length of practice: 18.3 years) completed the DCE. About half (50.5%) of patients favored CGRP mAb auto-injectors, while others were skeptical of (20.2%) or averse (29.3%) to them. Patients most valued needle removal (RAI = 33.8%), shorter injection duration (RAI = 32.1%), and auto-injector base shape and need for skin pinching (RAI = 23.2%). Most physicians (87.8%) favored auto-injectors over non-CGRP oral medications. Physicians most valued less-frequent dosing RAI = 32.7%), shorter injection duration (30.4%), and longer storage outside the fridge (RAI = 20.3%). A profile comparable to galcanezumab showed a higher likelihood of being chosen by patients (PCP = 42.8%) than profiles comparable to erenumab (PCP = 28.4%) and fremanezumab (PCP = 28.8%). The PCPs of the three profiles were similar among physicians.
Conclusion
Many patients and physicians preferred CGRP mAb auto-injectors over non-CGRP oral medications and preferred a treatment profile similar to galcanezumab. Our results may encourage physicians in Japan to consider patient preferences when recommending migraine preventive treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The increased number of treatment options for patients with migraine means that physicians and their patients are faced with a wider assortment of treatment attributes to consider. Preference studies are useful for weighting different treatment attributes and finding key drivers of preferences for treatments of interest. |
Patient and physician preferences for migraine treatments can differ, so physicians should be encouraged to take into account patients’ preferences when recommending treatments. |
This study elicited the preferences of Japanese patients with migraine and physicians who treat migraine to determine how they valued treatment attributes of self-injectable calcitonin gene-related peptide (CGRP) monoclonal antibodies (mAbs) and non-CGRP oral medications. |
What was learned from the study? |
Many patients and physicians in Japan would prefer self-injectable CGRP mAb auto-injectors to non-CGRP oral medications if the treatments were to have a similar efficacy in reducing migraine headache days. |
In considering CGRP mAb auto-injectors for migraine prevention, patients most valued needle removal, shorter injection duration, and auto-injector base shape and need for skin pinching, whereas physicians most valued less-frequent dosing, shorter injection duration, and longer storage outside the fridge. |
Introduction
Migraine is one of the leading causes of disability worldwide, and most commonly affects women of reproductive age [1]. The global prevalence of migraine is estimated to be approximately 14% [2]. In Japan, the estimated prevalence is slightly lower, at approximately 9% [3]. However, the burden of migraine in Japan is substantial, even in patients with fewer than four headache days per month [4].
People who experience more than four migraine attacks per month or eight or more headache days per month are recommended to use preventive treatment [5]. However, many people in Japan who are eligible for preventive treatment for migraine do not receive it [3, 6], due to lack of efficacy [6] and adverse effects, including weight gain, depression, memory impairment, and disturbance in attention [7]. A Japanese survey found that only 57% of respondents sought care for migraine [3]. Unlike most traditional non-calcitonin gene-related peptide (CGRP) oral medications that were not developed specifically to prevent migraine, self-injectable monoclonal antibodies (mAbs) that bind to CGRP (galcanezumab, fremanezumab) or the CGRP receptor (erenumab) have emerged as effective alternatives for migraine prevention for people in whom traditional non-CGRP oral medications have failed [8]. Several injectable CGRP mAbs were approved for migraine prevention in Japan in 2021, including erenumab, galcanezumab, and fremanezumab [9,10,11]. These three CGRP mAbs have not been compared in head-to-head clinical studies [12]; however, there are differences in dosing frequency, injection duration, and characteristics of the injection devices that are used to administer them.
The increased number of treatment options means that physicians and patients are faced with a wider assortment of treatment attributes to consider. Treatment selection requires weighting of these attributes, which include traditional clinical measures and also aspects of drug delivery [13]. While little is known about key drivers of patient preferences for preventive treatments for migraine, a recent preference study conducted in the US, the UK, and Germany found that patients generally valued injection duration, needle removal mechanism, auto-injector base shape and need for skin pinching, and storage requirements, and preferred self-injectable CGRP mAbs over non-CGRP oral medications [14].
Treatment decisions are often driven by physicians’ preferences [15]. Identifying and acknowledging differences in preferences between physicians and patients may increase transparency in treatment recommendations for individual patients [16]. Incorporating patient preferences into treatment decisions is important because patient participation in decision-making can increase treatment compliance, leading to better clinical outcomes [17, 18]. Few studies in Japan have analyzed patients’ involvement in treatment decisions. However, recent studies reported an increased tendency of Japanese patients to participate in treatment decisions for rheumatoid arthritis, inflammatory bowel disease, and prostate cancer [19,20,21].
The preferences of Japanese patients and physicians for devices for self-injecting CGRP mAbs to treat migraine are unknown. We aimed to elicit the preferences of Japanese migraine patients and physicians who treat migraine for different attributes of self-injectable CGRP mAbs for migraine prevention.
Methods
Study Design
The study was conducted in Japan using a discrete choice experiment (DCE). DCEs can be used to quantify the trade-offs people are willing to make between the various attributes of real or hypothetical treatments [22, 23]. In a DCE, participants choose between experimentally designed treatment profiles. The choices implicitly reveal how much value participants place on certain attributes and how much of one attribute they would give up to improve another attribute. Following best-practice recommendations for preference study design [23,24,25,26], the study used a mixed-methods approach to develop and test the DCE instrument. This included a non-systematic targeted literature review and focus group interviews for instrument development and qualitative and quantitative pilots for instrument testing.
The attributes and levels included in the DCE were initially identified through a targeted literature review, and were explored in nine in-person focus groups conducted in the US, the UK, and Germany (three per country) between October and November 2019 [27]. During the focus groups, participants handled and simulated self-injection using five unbranded, deactivated injection devices, and were asked about which device characteristics were important to them and why those characteristics were important. By way of open discussions and interactive ranking of treatment aspects, the focus groups also captured participants’ perspectives on efficacy and safety. The device characteristics found to be relevant to patients in the focus groups informed the development of the attributes for the DCE. Levels of the device attributes were constructed based on information from US FDA package inserts [28,29,30,31] and European Medicines Agency summaries of product characteristics [32,33,34].
The DCE was developed in English and pilot-tested in the US, UK, and Germany, before being translated into Japanese.
The Japanese DCE survey was pilot-tested qualitatively through telephone interviews with people with episodic migraine and physicians, to confirm the translation of survey materials and to ensure that the attributes and levels were relevant and understandable. Participants completed the DCE survey online during the interview, and their feedback necessitated a minor revision to the survey. Following the qualitative pilot, a quantitative pilot was performed in people with migraine and physicians, to provide insight into preferences and to analyze data quality. Data from the quantitative pilot were pooled from the main DCE survey.
Preference Survey
The full web-based survey was fielded between November 2021 and January 2022 for patients and physicians. Participants were shown a 4-min video (Supplementary Material), which introduced the attributes and levels in the DCE and explained how to complete the choice questions. Participants answered a practice choice question and then completed 12 experimental DCE choice questions, which were generated with Ngene v.1.2.1 (ChoiceMetrics, Sydney, Australia). The DCE choice questions asked participants to select between three hypothetical preventive treatments for migraine with different attribute levels: two CGRP mAbs administered using auto-injectors and a daily oral medication. Participants were advised to assume that the treatments were equally effective at reducing migraines. The DCE included the following experimental treatment attributes characterizing self-injectable CGRP mAbs: dosing schedule, storage requirements, device base and need for skin pinching, type of injection steps, injection duration, method of needle removal, and means of dose confirmation (Table 1). The choice questions also included adverse events associated with self-injectable CGRP mAbs and non-CGRP oral medications to make the choice questions more realistic, but were included as a non-experimental attribute with fixed levels. The variations in the DCE choice questions allowed participants to weigh the pros and cons of the treatments, allowing for trade-offs to be made each time a treatment option was chosen. These trade-offs allowed for marginal utilities (Supplementary Material) to be calculated. The DCE choice questions were followed by two non-experimental choice questions that tested the internal validity of participants’ responses. Participant consistency was tested by repeating the practice question (stability test). Additionally, a direct elicitation question asked participants to choose between four options (a prefilled syringe and three different auto-injectors). The four treatment options in the direct elicitation question were based on device attributes describing erenumab, galcanezumab, fremanezumab once a month, and fremanezumab every 3 months. Additional survey questions tested participants on their health literacy and numeracy [35,36,37,38], and collected sociodemographic information and information about migraine experience, including the Migraine Disability Assessment (MIDAS) [39]. Physicians answered questions about their experience of treating migraine, their satisfaction with available preventive treatments for migraine, and areas for improving migraine prevention. For patients and physicians, the time taken to complete the survey was recorded. More details of the DCE survey are given in Table S1. An example English-language DCE choice question is shown in Fig. 1.
Ethics
The study was performed in accordance with International Council for Harmonization Good Clinical Practice, best practices for preference-based outcomes research [23, 40], and the declaration of Helsinki. Initial ethics committee approval of the study by the Japanese Research Institute of Healthcare Data Science Review Services (study number RI2020021) was received on March 8, 2020. Online informed consent was obtained for each participant. Following modifications to the survey after the qualitative pilot interviews, the Japanese Research Institute of Healthcare Data Science Review Services approved the final survey on August 2, 2021.
Study Participants
Participants were residents of Japan who could read and understand Japanese. Patients were recruited from online panels and physicians were recruited from physician online panels.
Patients were adults aged ≥ 20 years with self-reported migraine (as diagnosed by a physician), who had experienced an average of at least four migraine headache days per month over the previous 3 months, and who had headache of at least moderate severity based on the Migraine Symptom Severity Score [41]. They were currently using or had used a prescribed preventive treatment for migraine in the previous 5 years. Patients with ≥ 4 and < 15 headache days per month for > 3 months were considered to have episodic migraine, and those with ≥ 15 headache days per month for > 3 months were considered to have chronic migraine. Physicians were neurologists, neurosurgeons, and internists who had been in practice for ≥ 3 years, had treated ≥ 10 patients for migraine within the previous 3 months, and had prescribed at least one preventive treatment for migraine within the previous 3 months.
Statistics
Statistical analyses were performed using R software v.4.0.2, using data from all participants who completed the survey. Statistical tests were two-sided, with a 0.05 significance level. There were no adjustments for multiple comparisons.
Participant choices were considered to be dominant when they were driven by only one attribute in all 12 experimental choice tasks.
Data from the DCE survey were analyzed using a random-constant logit model estimated within a random utility maximization framework (Supplementary Material) [42,43,44,45].
Relative attribute importance (RAI) was calculated to measure the percentage contribution of an attribute to preferences relative to all other attributes and their levels (Supplementary Material). RAI values were compared between patients and physicians using independent two-tailed z tests.
To understand relative treatment preferences, predicted choice probabilities (PCPs) were computed in a competitive setting that assumed respondents could choose among the treatment profiles of auto-injectable erenumab, galcanezumab, and fremanezumab (every 3 months or every month) [46,47,48]. The PCPs were calculated using a two-step process. First, the marginal utilities (Supplementary Material) were calculated, which were based on the participants’ preferred treatment choices in the DCE. The marginal utilities were then used to predict and calculate the probability of a participant choosing one of the treatment profiles. Each of the treatment profiles were characterized by attribute levels based on the corresponding FDA label. Subgroup-specific RAI scores were obtained based on fear of needles, experience with self-injectables, and number of migraine headache days.
Results
Participants
Of the approximately 400,000 patients and 2,100 physicians invited to participate, 1,382 patients and 233 physicians were eligible (Fig. 2). The DCE survey was completed by 601 patients and 219 physicians.
Patient (left) and physician (right) dispositionaRespondent reported < 4 migraine headache days per month on average for the last 3 monthsbRespondent did not have chronic migraine (CM) or episodic migraine (EM), based on number of headache days; patients with ≥ 4 and < 15 headache days per month for > 3 months were considered to have episodic migraine and those with ≥ 15 headache days per month for > 3 months were considered to have chronic migrainecRespondent did not have headache of at least moderate severity, as evaluated by the Migraine Symptom Severity ScoredPreventive treatments for migraine that are available in Japan (e.g., valproate, topiramate, atenolol, nortriptyline)eDid not report ≥ 3 years of practice in one of the following medical specialties: neurology, neurosurgery, internal medicine
Patient Characteristics
Of the 601 patients, 476 (79.2%) had episodic migraine (EM) and 125 (20.8%) had chronic migraine (CM). The mean [standard deviation (SD)] age of patients in the main DCE was 40.3 (11.7) years, and 361 (60.1%) were female (Table 2). Most patients were employed (81.5%) and had at least some college education (73.9%). Overall, over two-thirds of patients (68.9%) had moderate to very severe disability (grade III or higher on the MIDAS). The mean (SD) time since diagnosis of migraine was 16.5 (11.8) years. Most patients (73.7%) had used ≥ 2 preventive treatments for migraine in the previous 5 years, and commonly used preventive treatments included antidepressants (67.6%), anti-epileptics (35.4%), and antihypertensives (34.8%). Most patients (80.9%) had not used self-injectables, and 38.8% of patients were very or extremely afraid of needles. Sociodemographics and clinical characteristics were generally similar between patients with episodic and chronic migraine, except for MIDAS score [mean (SD) 19.8 (18.0) vs. 43.1 (45.9)], which was worse in patients with chronic versus episodic migraine, and the number of preventive treatments used for migraine in the past 5 years [mean (SD) 2.8 (2.1) vs. 4.8 (6.1)].
Physician Characteristics
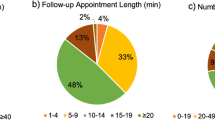
Physicians had been in clinical practice for a mean (SD) of 18.3 (5.3) years and most (74.4%) had treated ≥ 30 patients for migraine in the previous 3 months (Table 3). The treatments they had most frequently prescribed were anti-epileptics (95.9%), antidepressants (71.2%), and antihypertensives (70.3%). Two-fifths (40.6%) of physicians were slightly or very unsatisfied with currently available preventive treatments for migraine. About a third of physicians (31.5%) stated they could not see a place for subcutaneous self-injectable treatments, while another third (36.1%) said they would consider subcutaneous self-injectable treatments but only under certain circumstances. The remaining physicians (32.4%) stated they were excited about the prospect of subcutaneous self-injectable treatments and could see a place for them. When asked to rate possible areas for improving treatment of migraine prevention on a scale from 1 (no improvement needed) to 6 (significant improvement needed), physicians rated pill burden for patients [mean (SD) 4.7 (0.86)] and treatment effectiveness [mean (SD) 4.9 (0.93)] as areas requiring improvement.
Choice Data Validity
About half the patients (54.1%) did not show dominant preferences towards any single attribute, but some made choices predominantly based on needle removal (17.6%), auto-injector base shape and need for skin pinching (9.7%), injection duration (9.5%), storage requirements (5.7%), or dose confirmation (3.5%) (Table S2). Nearly half of physicians (43.4%) did not show dominant attribute preferences, but some made choices predominantly based on needle removal (16.4%), injection duration (12.8%), storage requirements (11.4%), dose confirmation (8.2%), or auto-injector base shape and need for skin pinching (7.8%). While 43.9% of patients never chose oral medication, 23.1% always chose oral medication. Most physicians (78.5%) never chose oral medication, while only 5.0% always chose oral medication. Most patients (73.0%) and physicians (74.9%) showed choice stability (i.e., gave consistent answers to the repeated choice question; p = 0.66, Chi-square test). Overall, 59.7% of patients had adequate health literacy and 91.7% had adequate numeracy. No patients or physicians took < 5 min to complete the survey, and about half (49.3%) of physicians and 21.0% of patients took ≥ 30 min to complete the survey.
Preferences for Treatment Attributes
The estimated model for patients was able to explain the choices they made (adjusted McFadden R2 = 34.9%) and identified three opt-in behaviors among patients (Table S3): “Auto-injector supporters”, who tended to choose auto-injectors (50.5%); “Auto-injector skeptics”, who only chose auto-injectors that included many desirable attribute levels (20.2%); and “Auto-injector opponents”, who tended to choose oral medications (29.3%). Overall, patients preferred the auto-retract feature to manual pull-out (p < 0.001) (Table S3). Patients would rather have an injection time of 10 s (p < 0.05) or 5 s (p < 0.001) than an injection time of 30 s. Patients also preferred a narrow base with no pinching (p < 0.01) and a wide base with no pinching (p < 0.001) compared to a narrow base with pinching. Patients’ preferences for auto-injectors were driven by needle removal (RAI = 33.8%), injection duration (RAI = 32.1%), and auto-injector base shape and need for skin pinching (RAI = 23.2%) (Fig. 3).
Patients’ characteristics affected their preferences. While the overall importance of needle removal did not differ by the level of fear of needles (p ≥ 0.05) (Fig. S1), patients with experience of self-injectables valued needle removal more than those with no experience of self-injectables (RAI = 34.3% vs. 16.4%, p < 0.05) (Fig. S2). Patients with 1–9 migraine headache days per month valued injection duration significantly less (RAI = 6.5%, p < 0.05) than those with 10–19 migraine headache days per month (RAI = 30.4%) or ≥ 20 migraine headache days per month (RAI = 27.1%) (Fig. S3). No significant differences in preferences were observed for dosing schedule, storage requirements, injection steps, or dose confirmation.
The estimated model for physicians was able to explain the choices they made (adjusted McFadden R2 = 32.4%) and identified two opt-in behaviors among physicians (Table S4): “Auto-injector supporters”, who tended to choose auto-injectors (87.8%); and “Auto-injector opponents”, who tended to choose oral medications (12.2%). Physicians preferred a dosing schedule of three injections once every 3 months (p < 0.001) over a dosing schedule of one injection once a month (Table S4). They also preferred an injection duration of 20 s (p < 0.01), 10 s (p < 0.001), or 5 s (p < 0.001) over an injection duration of 30 s. Physicians preferred a treatment that could be stored outside the fridge for up to 7 days (p < 0.001) or up to 14 days (p < 0.001) over one that could only be stored outside the fridge for up to 1 day. They also preferred an auto-retractable needle (p < 0.05) to manual pull-out. No significant differences in preferences were observed for dose confirmation, auto-injector base shape and need for skin pinching, or injection steps. Physicians’ preferences for auto-injectors were explained by dosing schedule (RAI = 32.7%), injection duration (RAI = 30.4%), storage requirements (RAI = 20.3%), and needle removal (RAI = 7.2%) (Fig. 3).
Predicted Choice Probability
In patients, a treatment profile comparable to galcanezumab (one injection every month: PCP = 42.8%; 95% CI = 39.2–46.4) had a significantly higher likelihood of being chosen over profiles comparable to fremanezumab (three injections every 3 months: PCP = 28.8%; 95% CI = 25.5–32.0, p < 0.001) and erenumab (one injection every month: PCP = 28.4%; 95% CI = 25.9–31.0, p < 0.001) (Fig. 4). The likelihood of choosing the treatment profile comparable to fremanezumab was similar to the likelihood of choosing the treatment profile comparable to erenumab (p > 0.05). These results were aligned with the direct elicitation question (Fig. S4) presenting the corresponding attribute levels, in which a profile comparable to galcanezumab was chosen by more patients (44.6%) than a profile comparable to erenumab (17.5%) and fremanezumab (three injections every 3 months: 20.0%).
The treatment profiles comparable to fremanezumab (three injections every 3 months: PCP = 34.7%; 95% CI = 29.6–39.8), galcanezumab (PCP = 34.3%; 95% CI = 29.6–39.0), and erenumab (PCP = 31.0%; 95% CI = 27.1–34.9) were predicted to be chosen by physicians with a similar probability (p > 0.05 each; Fig. 4A). This result was not consistent with the corresponding direct elicitation question (Fig. S4), in which the treatment profile comparable to galcanezumab was chosen by more physicians (53.4%) than ones comparable to erenumab (9.6%) and fremanezumab (three injections every 3 months: 32.4%).
Changing the fremanezumab dosing schedule from three injections every 3 months to one injection once a month resulted in small changes to the PCPs for patients, but did not change the order or statistical significance of their preferences (Fig. 4B). By contrast, changing the dosing schedule of fremanezumab changed the order of physicians’ preferences to favor the treatment profile comparable to galcanezumab over the one comparable to fremanezumab (p < 0.001), but not the one comparable to erenumab (p > 0.05), and to favor the treatment profile comparable to erenumab over the one comparable to fremanezumab (p = 0.002).
Discussion
In the current study, approximately one-third of physicians would consider prescribing subcutaneous self-injectable treatments under certain circumstances; a similar number were excited about the prospect of subcutaneous self-injectable auto-injectors. However, approximately one-third of patients were reluctant or even averse to switching to a CGRP mAb auto-injector. Nonetheless, many of the patients and physicians would prefer self-injectable CGRP mAbs over non-CGRP oral medications if the preventive treatment offered similar efficacy in reducing the frequency of experiencing migraine headache days. Most participants preferred a treatment profile similar to galcanezumab.
While the study confirmed that auto-injectors were preferable to oral medications for both patients and physicians, consistent with findings from another preference study conducted with people with migraine in the US, the UK, and Germany [14], previous studies comparing preferences between subcutaneous injection and oral administration for preventive treatments for migraine gave different results. For example, a DCE completed by people reporting ≥ 6 migraine days per month revealed no significant differences in preferences between the two administration routes [49]. The different results between the studies may be due to dissimilarities in study design and different treatment attributes presented to the patients. Specifically, attributes included in the other DCE include frequency of limitations with physical activities, reduction in headache days per month, weight gain, cognition problems, and monthly out-of-pocket cost; frequency and mode of administration were the only attributes common to both studies [49].
Patients and physicians differed in their preferences in our study. For instance, the main drivers of patient preferences for auto-injectors were needle removal, injection duration, and auto-injector base shape and need for skin pinching, whereas those of physicians were dosing schedule, injection duration, storage requirements, and needle removal. Patients found the most benefit in having an auto-retractable needle rather than a self-removed needle, having a shorter injection duration, and having a narrow or wide base with no pinching rather than a narrow base with pinching. These valuations are aligned with those from the other preference study conducted in the US, the UK, and Germany [14], except that the storage requirements did not significantly affect Japanese patients’ preferences. The finding that needle removal was one of the most important attributes among Japanese patients could be explained by most participants lacking experience with self-injectables and because over a third of them were very or extremely afraid of needles. In patients with diabetes, fear of needles is a common barrier to self-injectables [50], which may be exacerbated by lack of experience with injection therapy [51]. During the qualitative pilot interviews, Japanese patients often identified dosing schedule and injection duration as the most important drivers of their preferences. However, in the DCE, no significant difference was observed between preferences for three injections once every month and one injection once a month. This finding is consistent with the previous preventive migraine treatment preference study [14].
Japanese patients preferred reducing the injection duration to 5 or 10 s, but significant preferences were not detected for 5 s over 10 s. This finding is similar to findings from the other preventive migraine treatment preference study [14], where a significant difference in preferences was not detected for a self-injection lasting 3 or 5 s versus 10 s. While the other preventive migraine treatment preference study found that longer storage outside the fridge was the third most important attribute [14], it did not affect Japanese patients’ treatment valuations. Some studies suggest that storage requirements are associated with treatment compliance [52, 53]. However, patients’ preferences for storage requirements have not been widely studied.
Dosing schedule was the most important attribute driving the choices of physicians, who preferred three injections every 3 months over one injection monthly. However, dosing schedule was not a driver of patients’ preferences. A previous US survey revealed similar preferences for monthly and quarterly injections among physicians who treat migraine [54]. The authors of that study proposed ease of remembering and fewer consecutive injections as reasons for physicians preferring monthly over quarterly injections, and improved treatment compliance, reduced injection burden, and fewer injection days as reasons for preferring quarterly dosing over monthly dosing [54]. While physicians considered an auto-retractable needle to be more desirable than manual needle removal, they placed less importance on this than patients. This could be because it is time-consuming to explain injection methods and use of injection devices, as suggested by a previous comparative usability study about insulin therapy [55].
This study benefitted from a best-practice mixed methods design [56,57,58]. The attributes in the DCE were identified through a targeted literature review and nine in-person focus groups conducted in the US, UK, and Germany, during which patients simulated using unbranded auto-injectors and prefilled syringes [27]. The DCE was also qualitatively and quantitatively pilot-tested before surveying Japanese patients and physicians. In addition, in order to address possible challenges in communicating auto-injector attribute levels to participants, the patient information leaflets for CGRP mAbs and the findings of the focus group study [27] were used to develop a short video to help participants to understand the attributes and to distinguish their levels. This was especially important for attributes describing different parts of the devices, such as the base and dose confirmation window, which would not be familiar to participants who have not used such devices. Also, most patients and physicians took ≥ 10 min to complete the survey, which suggests they took time to understand the choice options and make appropriate choices.
This study had limitations. The attributes of the CGRP mAb auto-injectors were based on FDA package inserts instead of the inserts from the Pharmaceuticals and Medical Devices Agency of Japan, due to the timing of the study and medication approval in Japan. Also, participants did not have the opportunity to physically experience and use CGRP mAb auto-injectors, while CGRP-targeted treatments were not available in Japan at the time of the survey; future research with actual device use may elicit different preferences for the CGRP mAb auto-injectors. Although efforts were made to only include participants who met the eligibility criteria, the generalizability of the results to the wider populations of people with migraine and physicians who treat migraine in Japan remains uncertain. For instance, patients with episodic migraine accounted for 79.2% of our study population, whereas in earlier surveys patients with episodic migraine accounted for 94.5% of participants [6].
Conclusions
Although Japanese patients and physicians valued CGRP mAb auto-injectors more highly than non-CGRP oral medications, and preferred a treatment profile similar to galcanezumab, their preferences for device characteristics and administration profiles differed. Identifying differences in patient and physician preferences can increase transparency for treatment recommendations for individual patients, and potentially increase treatment compliance.
References
Stovner LJ, Nichols E, Steiner TJ, et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(11):954–76.
Stovner LJ, Hagen K, Linde M, et al. The global prevalence of headache: an update, with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain. 2022;23(1):34.
Hirata K, Ueda K, Komori M, et al. Comprehensive population-based survey of migraine in Japan: results of the ObserVational Survey of the Epidemiology, tReatment, and Care Of MigrainE (OVERCOME [Japan]) study. Curr Med Res Opin. 2021;37(11):1945–55.
Matsumori Y, Ueda K, Komori M, et al. Burden of migraine in Japan: results of the ObserVational Survey of the Epidemiology, tReatment, and Care Of MigrainE (OVERCOME [Japan]) Study. Neurol Ther. 2022;11(1):205–22.
Silberstein SD. Preventive migraine treatment. Continuum (Minneap Minn). 2015;21(4):973–89.
Ueda K, Ye W, Lombard L, et al. Real-world treatment patterns and patient-reported outcomes in episodic and chronic migraine in Japan: analysis of data from the Adelphi migraine disease specific programme. J Headache Pain. 2019;20(1):68.
D’Amico D, Tepper SJ. Prophylaxis of migraine: general principles and patient acceptance. Neuropsychiatr Dis Treat. 2008;4(6):1155–67.
Scuteri D, Adornetto A, Rombola L, et al. New trends in migraine pharmacology: targeting calcitonin gene-related peptide (CGRP) with monoclonal antibodies. Front Pharmacol. 2019;10:363.
Emgality (galcanezumab) [package insert]. Japanese PMDA. Eli Lilly and Company. https://www.pmda.go.jp/PmdaSearch/iyakuDetail/ResultDataSetPDF/530471_1190404G1020_1_05.
Aimovig (erenumab) [package insert]. Japanese PMDA. Amgen Inc. https://www.pmda.go.jp/PmdaSearch/iyakuDetail/ResultDataSetPDF/112292_1190406G1029_2_01.
Ajovy (fremanezumab) [package insert]. Japanese PMDA. Teva Pharmaceuticals. https://www.pmda.go.jp/PmdaSearch/iyakuDetail/ResultDataSetPDF/180078_11904A3G2025_1_01.
Barbanti P, Egeo G, Aurilia C, et al. Predictors of response to anti-CGRP monoclonal antibodies: a 24-week, multicenter, prospective study on 864 migraine patients. J Headache Pain. 2022;23(1):138.
Sacco S, Amin FM, Ashina M, et al. European Headache Federation guideline on the use of monoclonal antibodies targeting the calcitonin gene related peptide pathway for migraine prevention—2022 update. J Headache Pain. 2022;23(1):67.
Seo J, Tervonen T, Thomas C, et al. Patient preferences for self-injectable preventive treatments for migraine (poster). 63rd Virtual Annual Scientific Meeting of the American Headache Society (AHS); June 3, 2021.
Mühlbacher AC, Juhnke C. Patient preferences versus physicians’ judgement: does it make a difference in healthcare decision making? Appl Health Econ Health Policy. 2013;11(3):163–80.
Tervonen T, Angelis A, Hockley K, et al. Quantifying preferences in drug benefit-risk decisions. Clin Pharmacol Ther. 2019;106(5):955–9.
Hughes TM, Merath K, Chen Q, et al. Association of shared decision-making on patient-reported health outcomes and healthcare utilization. Am J Surg. 2018;216(1):7–12.
Shay LA, Lafata JE. Where is the evidence? A systematic review of shared decision making and patient outcomes. Med Decis Making. 2015;35(1):114–31.
Aoki A, Suda A, Nagaoka S, et al. Preferences of Japanese rheumatoid arthritis patients in treatment decision-making. Mod Rheumatol. 2013;23(5):891–6.
Mahlich J, Matsuoka K, Sruamsiri R. Shared decision making and treatment satisfaction in Japanese patients with inflammatory bowel disease. Dig Dis. 2017;35(5):454–62.
Schaede U, Mahlich J, Nakayama M, et al. Shared decision-making in patients with prostate cancer in Japan: patient preferences versus physician perceptions. J Glob Oncol. 2018;4:1–9.
Clark MD, Determann D, Petrou S, et al. Discrete choice experiments in health economics: a review of the literature. Pharmacoeconomics. 2014;32(9):883–902.
Bridges JF, Hauber AB, Marshall D, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14(4):403–13.
FDA. Patient preference information—voluntary submission, review in premarket approval applications, humanitarian device exemption applications, and de novo requests, and inclusion in decision summaries and device labeling. Guidance for Industry, Food and Drug Administration Staff, and Other Stakeholders. U.S. Department of Health and Human Services, Food and Drug Administration; Center for Devices and Radiological Health; Center for Biologics Evaluation and Research; 2016. https://www.fda.gov/media/92593/download. Accessed June 8, 2022.
IMI. Patient preferences in benefit-risk assessments during the drug life cycle (PREFER). Innovative Medicines Initiative; 2016. https://www.imi-prefer.eu/digitalAssets/583/c_583778-l_1-k_prefer-redacted.pdf. Accessed June 8, 2022.
Qualification Opinion of IMI PREFER. European Medicines Agency; 2022. https://www.ema.europa.eu/en/documents/regulatory-procedural-guideline/qualification-opinion-imi-prefer_en.pdf. Accessed June 8, 2022.
Seo J, Smith CA, Thomas C, et al. Patient perspectives and experiences of preventive treatments and self-injectable devices for migraine: a focus group study. Patient. 2022;15(1):93–108.
Aimovig (erenumab) [package insert]. U.S. Food and Drug Administration. Amgen Inc.; 2018.
Ajovy (fremanezumab) [package insert]. U.S. Food and Drug Administration. Teva Pharmaceuticals USA, Inc.; 2020.
Emgality (galcanezumab) [package insert]. U.S. Food and Drug Administration. Eli Lilly and Company; 2018.
Teva Pharmaceuticals USA I. Ajovy (fremanezumab) [package insert]. U.S. Food and Drug Administration; 2021.
European Medicines Agency. Emgality—EMEA/H/C/004648-X/0004; 2020.
European Medicines Agency. Aimovig—EMEA/H/C/004447—PSUSA/00010699/201911; 2020.
European. Medicines Agency. Ajovy—EMEA/H/C/004833—II/0008/G; 2021.
Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21(1):37–44.
Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–94.
Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23(5):561–6.
Fransen MP, Van Schaik TM, Twickler TB, et al. Applicability of internationally available health literacy measures in the Netherlands. J Health Commun. 2011;16(Suppl 3):134–49.
Stewart WF, Lipton RB, Dowson AJ, et al. Development and testing of the Migraine Disability Assessment (MIDAS) Questionnaire to assess headache-related disability. Neurology. 2001;56(6 Suppl 1):S20–8.
ISPOR Good Practices for Outcomes Research Index. International Society for Pharmacoeconomics Outcomes Research; 2018. https://www.ispor.org/heor-resources/good-practices-for-outcomes-research. Accessed Oct 16, 2020.
Serrano D, Buse DC, Reed ML, et al. Development of the Migraine Symptom Severity Score (MSSS): a latent variable model for migraine definition: PO-86. Headache. 2010;50(suppl 1):40.
Thurstone LL. A law of comparative judgment. Psychol Rev. 1927;34(4):273–86.
Marschak J. Binary choice constraints on random utility indicators. New Haven: Cowles Foundation for Research in Economics, Yale University; 1959.
McFadden D. Conditional logit analysis of qualitative choice behaviour. New York: Academic Press; 1973.
Manski CF. The structure of random utility models. Theory Decis. 1977;8(3):229–54.
Teva Pharmaceuticals USA I. Ajovy (fremanezumab) [package insert]. U.S. Food and Drug Administration; 2020.
Amgen Inc. Aimovig (erenumab) package insert. U.S. Food and Drug Administration; 2018.
Eli Lilly and Company. Emgality (galcanezumab) [package insert] U.S. Food and Drug Administration; 2018.
Mansfield C, Gebben DJ, Sutphin J, et al. Patient preferences for preventive migraine treatments: a discrete-choice experiment. Headache. 2019;59(5):715–26.
Spain CV, Wright JJ, Hahn RM, et al. Self-reported barriers to adherence and persistence to treatment with injectable medications for type 2 diabetes. Clin Ther. 2016;38(7):1653–64.
Asakura T, Yamazaki T, Cai Z, et al. Comparative study of dulaglutide single-use pen Ateos versus insulin degludec FlexTouch on learning and mock administration time in Japanese patients with type 2 diabetes mellitus—a post-hoc analysis. Curr Med Res Opin. 2020;36(5):765–9.
Vlieland ND, Gardarsdottir H, Bouvy ML, et al. The majority of patients do not store their biologic disease-modifying antirheumatic drugs within the recommended temperature range. Rheumatology (Oxford). 2016;55(4):704–9.
Vlieland ND, van den Bemt BJF, Bekker CL, et al. Older patients’ compliance with drug storage recommendations. Drugs Aging. 2018;35(3):233–41.
Cowan R, Cohen JM, Rosenman E, et al. Physician and patient preferences for dosing options in migraine prevention. J Headache Pain. 2019;20(1):50.
Asakura T, Suzuki S, Aranishi T, et al. Comparative usability study of the dulaglutide single-use pen versus the insulin degludec FlexTouch((R)) among self-injection-naive patients with type 2 diabetes mellitus in Japan. Curr Med Res Opin. 2018;34(6):1117–24.
Ryan M, Watson V, Entwistle V. Rationalising the “irrational”: a think aloud study of discrete choice experiment responses. Health Econ. 2009;18(3):321–36.
Coast J, Al-Janabi H, Sutton EJ, et al. Using qualitative methods for attribute development for discrete choice experiments: issues and recommendations. Health Econ. 2012;21(6):730–41.
Kløjgaard ME, Bech M, Søgaard R. Designing a stated choice experiment: the value of a qualitative process. J Choice Model. 2012;5(2):1–18.
Acknowledgements
We thank the participants of the study for their time and cooperation. We also thank Justin Chen, MHS, who validated Japanese translation of the web-based survey and the video and conducted qualitative pilot interviews in Japanese. Justin Chen was an employee of Evidera at the time of this study but recieved no other funding for his support.
Funding
Funding for this study and the journal’s rapid service fee was provided by Eli Lilly & Co.
Medical writing and/or editorial assistance
Medical writing was provided by Holly Richendrfer, PhD and Stephen Gilliver, PhD (Evidera) and was funded by Eli Lilly & Co.
Author contributions
Jaein Seo contributed to the conception and planning of the work, acquisition and interpretation of the data, and drafting and critical revision of the manuscript. Tommi Tervonen contributed to the conception and planning of the work, interpretation of the data, and critical revision the manuscript. Kaname Ueda contributed to the conception and planning of the work and critical revision of the manuscript. Dian Zhang contributed to the analysis and interpretation of the data and critical revision of the manuscript. Daisuke Danno contributed to the interpretation of the data and critical revision of the manuscript. Antje Tockhorn-Heidenreich contributed to conception and planning of the work, interpretation of the data, and critical revision of the manuscript. All authors participated sufficiently in the work to take public responsibility for the entire content of the manuscript.
Disclosures
Jaein Seo is an employee of Evidera, which was paid by Eli Lilly & Co. for work related to this study. Tommi Tervonen and Dian Zhang were employees of Evidera at the time of this study. Antje Tockhorn-Heidenreich and Kaname Ueda are employees and stockholders of Eli Lilly & Co., which funded the study. Daisuke Danno received lecture fees from: Eli Lilly Japan, Daiichi Sankyo Co., Ltd., Amgen K.K., and Otsuka Pharmaceutical Co., Ltd.
Compliance with ethics guidelines
The study was approved by the central institutional review board of Healthcare Data Science Research Institute, RIHDS (Tokyo, Japan) before any study procedures were initiated (institutional review board reference number RI2020021). All participants provided online consent to participate. Furthermore, this study was conducted in accordance with the declaration of Helsinki.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available as no consent was sought from participants to allow sharing of data with third parties.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Seo, J., Tervonen, T., Ueda, K. et al. Discrete Choice Experiment to Understand Japanese Patients’ and Physicians’ Preferences for Preventive Treatments for Migraine. Neurol Ther 12, 651–668 (2023). https://doi.org/10.1007/s40120-023-00453-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-023-00453-0