Abstract
Neurogenic orthostatic hypotension (nOH) is a sustained fall in blood pressure upon standing that frequently affects patients with neurodegenerative diseases (e.g., Parkinson disease) and manifests with symptoms such as lightheadedness and dizziness upon standing. nOH can severely affect patients by increasing the risk of falls and injuries and by decreasing functionality, independence, and quality of life. However, the condition is often under-recognized because of many factors, including the nonspecific nature of the symptoms, patient comorbidities, and patients’ reluctance to discuss their symptoms with their healthcare providers. Increased awareness of the burden of nOH and recognition of potential barriers to efficient diagnosis may lead to improved clinical outcomes and better quality of life for patients. To better understand the manifestations and real-life impact of living with nOH symptoms, perspectives from a patient with nOH and his caregiver (wife) are provided, along with key findings from a published survey of patients and caregivers on the burden of nOH. In addition, insights and advice on a practical approach for diagnosing, educating, and treating patients with nOH are outlined.
Plain Language Summary
This article discusses what neurogenic orthostatic hypotension (nOH) is, its symptoms, and how patients and healthcare providers (HCPs) can work together to manage nOH symptoms. What is nOH? People with neurologic disorders, like Parkinson disease, may also have a separate condition called nOH. nOH occurs when blood pressure drops too much when standing up after sitting or lying down. What are the symptoms of nOH, and how can they affect people’s lives? Most often, people with nOH report feeling lightheaded, faint, or dizzy when standing up. Other symptoms of nOH include pain in the shoulders and neck, trouble thinking clearly, tiredness, or blurry vision. The symptoms of nOH can cause falls and injuries. Because of nOH symptoms, people may be unable to do daily activities and may feel worried or anxious. What do patients and HCPs need to know when discussing nOH symptoms? A survey showed that patients may not talk about their nOH symptoms with their HCPs unless symptoms are severe, and that patients can find receiving a diagnosis of nOH challenging. Patients can track nOH symptoms in a daily journal to use in discussions with their HCPs. How can HCPs help patients with nOH? HCPs can ask patients with underlying neurologic disorders about symptoms that occur on standing and confirm a diagnosis of nOH by comparing the patient’s blood pressures measured lying down and after standing up. HCPs can provide information about lifestyle changes and medications that are available to manage nOH symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Neurogenic orthostatic hypotension (nOH) commonly occurs in patients with neurodegenerative diseases (e.g., Parkinson disease) as a consequence of autonomic nervous system dysfunction. |
Patients with nOH may experience severe and burdensome symptoms, which can result in functional impairment and decreased quality of life. |
Patients may not recognize nOH and instead attribute their symptoms to the underlying neurologic condition (e.g., Parkinson disease). |
By increasing healthcare providers’ awareness about recognizing, diagnosing, and managing nOH, clinical outcomes and quality of life in the patients they treat may be improved. |
Treatment of nOH symptoms using non-pharmacologic and pharmacologic options may help improve patients’ ability to perform daily activities and increase their sense of well-being. |
Introduction
Aging is associated with an increased likelihood of synucleinopathies (e.g., Parkinson disease [PD]) [1], which can result in autonomic dysfunction [2]. A common consequence of this autonomic dysfunction is neurogenic orthostatic hypotension (nOH), a condition in which orthostatic blood pressure (BP) drops [3]. Healthcare providers (HCPs) may frequently encounter patients with nOH, but the condition may be under-recognized and, consequently, undertreated in clinical practice, despite its severe functional and psychosocial effects on patients [4]. HCPs caring for patients with PD and other neurodegenerative conditions can play a fundamental role in the recognition of nOH because of their frequent and in-depth interactions with these patients and their caregivers. However, patients may be unaware of or reluctant to discuss their nOH symptoms with their HCPs. Greater understanding of these communication barriers and ways to overcome these challenges, especially among HCPs practicing in neurology settings, may lead to more timely diagnosis of nOH and improved patient outcomes.
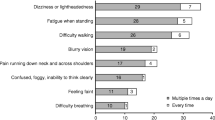
Symptoms of nOH and Their Effect
The cardinal symptoms of nOH are dizziness and lightheadedness; however, the BP reduction and resulting organ hypoperfusion associated with nOH can cause a variety of nonspecific symptoms, including cognitive difficulties, neck and shoulder pain, fatigue, and visual disturbances [2]. The burden of nOH was examined in a survey of 363 patients with an underlying autonomic failure diagnosis and a formal diagnosis of nOH/orthostatic hypotension (OH) or characteristic signs and/or symptoms of nOH/OH (e.g., low BP, dizziness/lightheadedness), and 128 caregivers of such patients. In this survey, between 20 and 40% of patients reported persistently experiencing these types of symptoms (i.e., multiple times a day when moving to a sitting or standing position) [4]. nOH symptoms can increase the risk for falls and related injuries, a particular concern in older persons [2]. In the above-mentioned nOH burden survey, nearly 60% of patients and 80% of caregivers reported ≥ 1 patient fall in the previous year [4]. Although falls due to nOH symptoms can have direct physical, financial, and psychosocial consequences (e.g., disability, mortality, increased healthcare costs, fear of falling, and subsequent limitation of activities) [2, 5,6,7], this survey also provided insight into the overall patient burden of nOH. Most patient and caregiver respondents (> 87%) reported that nOH symptoms impeded the patient’s ability to perform everyday activities (e.g., physical activity/exercise, housework, traveling, leaving the house) [4]. Further, substantial percentages of patients and caregivers indicated that nOH symptoms affected patients by diminishing quality of life, causing a perceived loss of independence, and changing their lives drastically (40–75%). Half of patients reported feeling anxious, worried, depressed, or discouraged because of nOH symptoms [4]. The experience of living with nOH symptoms is illustrated in the following patient perspective.
Patient Perspective on nOH Symptoms
“Initially, I did not realize that I had nOH. I would have a tendency to be slow getting started in a movement, getting sleepy during the day and dozing, overall lethargic feeling, difficult to get motivated.… In the morning in getting dressed and things like that, I would be frozen, and during the day, I would get sleepy. I would try to get up and walk around, but it was hard to get up…. As the day progressed, I became slower and slower and the symptoms were more pronounced.… Sometimes, I would go to bed at 8:00 pm, which is abnormal for me. It was difficult to plan things for the evening after work.… [It was] very hard to get motivated, and [I had] a desire to just go to bed.… Looking back on it, I think it had an impact on my cognitive behavior…. This [led] to depression, loss of sleep, anxiety, and overall malaise.”
Role of HCPS in nOH Care
Although HCPs treating patients at risk of nOH are well suited to recognize symptoms and facilitate discussions regarding nOH with patients and their caregivers (Fig. 1) [2, 3, 8, 9], they also need to understand potential communication challenges. Patients with nOH may hide or minimize their symptoms and not discuss them with their HCP unless the symptoms are severe [4]. Further, patients may attribute the symptoms to the underlying neurodegenerative disease or other comorbidities, not realizing that nOH is a separate condition. Others may be concerned that reporting nOH symptoms or falls could lead to restrictions on their activities and ability to live independently [2]. Patients may not always be forthcoming regarding nOH symptoms, and patient survey data have indicated that patients find the path to diagnosis challenging. Half of patients with nOH reported frustration with the diagnostic process, which may have included multiple HCP consultations before their eventual diagnosis (43% consulted ≥ 3 HCPs) [4]. Increased awareness of these issues will better enable HCPs to diagnose and treat these bothersome symptoms.
When nOH is suspected, orthostatic vital signs should be taken to observe whether the BP drop is indicative of OH (≥ 20 mmHg systolic or ≥ 10 mmHg diastolic) [2, 3]. However, individual in-clinic evaluations of orthostatic vitals might not confirm OH, and an at-home BP and symptom diary may be required [2]. This diary should include the time of each BP measurement and accompanying circumstances, such as recent meals, timing of medications, or exercise. In patients with PD, such a record can also be used to document “on” and “off” periods of dopaminergic medication, allowing the HCP a comprehensive view of the patient’s overall symptom experience. Even after initial recognition of OH/nOH, continued use of a symptom diary can be useful to guide and adjust the treatment plan over time.
Once the presence of OH has been established, HCPs should aim to reduce any non-neurogenic causes of OH (i.e., Fig. 1, Step 4). For example, the potential contributing effects of any concomitant medications should be considered. Patients with PD and other synucleinopathies are often treated with medications such as levodopa (or other dopaminergic agents) and monoamine oxidase inhibitors that are associated with hypotensive effects and may worsen nOH symptoms [2, 10]. Additionally, many other medications commonly used in older populations also have hypotensive effects, including drugs for hypertension, depression, erectile dysfunction, benign prostatic hyperplasia (BPH; alfuzosin or tamsulosin), or hair loss (minoxidil) [2]. In consultation with the care team, use of these medications in patients with nOH should be modified if possible (e.g., dose reduction, adjustment of timing of use [particularly PD medications], discontinuation) without exacerbating the indicated conditions [2]. Referral for specialized autonomic function testing may be appropriate if the diagnosis continues to be unclear.
When managing nOH symptoms, attaining a certain standing blood pressure is not necessary; rather, the goals of treatment should focus on patient outcomes, including decreasing nOH symptom burden, mitigating risk of falls and fall-related injuries, and improving the ability to function independently in daily activities [2]. The precise treatment choices should be tailored to the individual patient’s needs and circumstances considering both non-pharmacologic and pharmacologic options.
Non-pharmacologic measures are an important component of nOH management, but patients may not recognize or readily implement these measures. For example, waist-high compression garments are effective for treating patients with nOH, but patients may be reluctant to wear them because they may find these compression garments uncomfortable (especially in warmer weather) [2]. Patients may also be inadequately hydrated from use of diuretics or self-restricted fluid intake to reduce urinary urgency or frequency related to stress incontinence, BPH, or other bladder disorders [2, 11]. In these cases, HCPs can educate patients to encourage compliance and enlist the help of the caregiver if necessary.
Although non-pharmacologic measures are often used as the initial approach to treat nOH, implementing pharmacotherapy is often necessary for adequate relief of symptoms. Droxidopa and midodrine are approved by the US Food and Drug Administration to treat the symptoms of nOH and OH, respectively (Fig. 1) [8, 9]. Other agents (e.g., fludrocortisone, pyridostigmine) are commonly used off-label for the treatment of nOH [2, 12, 13] but have limited evidence of efficacy based on results from well-designed trials. Several comprehensive reviews on the management of nOH have been published in the past 3 years and are useful resources for detailed guidance and specific considerations of individual non-pharmacologic and pharmacologic interventions [2, 12, 13].
Patient Perspective on nOH Care
“I attributed all of [the symptoms] to PD. It became evident that the nOH was causing me to feel more ‘stuck’ or ‘frozen’ than I would otherwise feel as a Parkinson’s patient. There is so much information that [my HCPs] had, and you just get overwhelmed after a bit and you don’t necessarily connect the dots that [BP] may be an issue…as a non-medical person, I don’t know what factors matter and what to tell [my HCPs]. Or I might get confused as to why something is happening. So I just am very careful not to put any judgment on what I’m feeling when I’m telling them my symptoms. [My HCPs] are very good at asking the same question several different ways to clarify the answers.
I would suggest… to keep a journal of BP, medication changes, environmental changes, and a detailed account of any changes in how [you] are feeling and/or functioning… an [HCP] might be able to look at it and say ‘this guy could have low blood pressure.’
Once we were able to recognize that nOH was an issue [and treatment was initiated], within a few days, I began to perk up, had a bounce in my step, felt overall motivated to exercise and take on projects, slept better, and felt very encouraged. After taking the medication, I’ve been feeling more active and more resilient. You begin to have hope. The improvement in energy levels and the decline of depression and anxiety were great. I felt like my cognitive skills were returning to pre-Parkinson’s level.”
Caregiver Perspective on nOH Care
“I notice a huge difference… his attitude, the way he’s getting up and down; he’s been much better. I think he was beginning to think he couldn’t do stuff. Once [his HCPs] figured it out, I think his attitude changed.”
Conclusions
Patients with nOH may experience burdensome symptoms, functional impairments, and a decreased sense of psychosocial well-being. With increased awareness of the recognition, diagnosis, and management of nOH, HCPs can play a key role in improving clinical outcomes and quality of life in the patients they treat.
References
Savica R, Grossardt BR, Bower JH, Ahlskog JE, Rocca WA. Incidence and pathology of synucleinopathies and tauopathies related to parkinsonism. JAMA Neurol. 2013;70(7):859–66.
Gibbons CH, Schmidt P, Biaggioni I, et al. The recommendations of a consensus panel for the screening, diagnosis, and treatment of neurogenic orthostatic hypotension and associated supine hypertension. J Neurol. 2017;264(8):1567–82.
Freeman R, Wieling W, Axelrod FB, et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res. 2011;21(2):69–72.
Claassen DO, Adler CH, Hewitt LA, Gibbons C. Characterization of the symptoms of neurogenic orthostatic hypotension and their impact from a survey of patients and caregivers. BMC Neurol. 2018;18(1):125.
Merola A, Sawyer RP, Artusi CA, et al. Orthostatic hypotension in Parkinson disease: impact on health care utilization. Parkinsonism Relat Disord. 2017;47:45–9.
Francois C, Biaggioni I, Shibao C, et al. Fall-related healthcare use and costs in neurogenic orthostatic hypotension with Parkinson's disease. J Med Econ. 2017;20(5):525–32.
LeWitt PA, Kymes S, Hauser RA. Parkinson disease and orthostatic hypotension in the elderly: recognition and management of risk factors for falls. Aging Dis. 2020;11(3):679–91.
Northera® (droxidopa). Full prescribing information. Deerfield: Lundbeck NA Ltd; 2017.
ProAmatine® (midodrine hydrochloride). Full prescribing information. Lexington: Shire US Inc.; 2017.
Cutsforth-Gregory JK, Low PA. Neurogenic orthostatic hypotension in Parkinson disease: a primer. Neurol Ther. 2019;8(2):307–24.
Weinberg AD, Minaker KL. Dehydration. Evaluation and management in older adults. Council on Scientific Affairs, American Medical Association. JAMA. 1995;274(19):1552–6.
Freeman R, Abuzinadah AR, Gibbons C, Jones P, Miglis MG, Sinn DI. Orthostatic hypotension: JACC state-of-the-art review. J Am Coll Cardiol. 2018;72(11):1294–309.
Olshansky B, Muldowney J. Cardiovascular safety considerations in the treatment of neurogenic orthostatic hypotension. Am J Cardiol. 2020;125(10):1582–93.
Acknowledgements
The authors thank the patient and his caregiver (wife) for their participation in this project.
Funding
Lundbeck (Deerfield, IL) provided funding for editorial support for manuscript preparation and the Rapid Service and Open Access fees.
Authorship
All named authors meet the International Committee of Medical Journal Editors criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Medical Writing, Editorial, and Other Assistance
Medical writing and editorial assistance in the preparation of this article was provided by Lauren Stutzbach, PhD, and Lisa Havran, PhD, of ICON (North Wales, PA), which was supported by Lundbeck.
Disclosures
Jessie S. Gibson has served as a consultant for Lundbeck and received research support and compensation for speaker bureau participation from Teva Neuroscience. Christine B. Hunter has served on advisory boards for Acorda Therapeutics and Lundbeck. L. Arthur Hewitt is an employee of Lundbeck.
Compliance with Ethics Guidelines
Institutional review board approval was not required for this single-patient case study. Informed consent to share this case was obtained from the patient and his caregiver (wife). All patient information has been anonymized.
Prior Presentation
Aspects of this work were previously presented as a poster at the National Conference for Nurse Practitioners; September 24–27, 2019; Las Vegas, NV.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12631385.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gibson, J.S., Hunter, C.B. & Hewitt, L.A. A Call to Action: The Role of Healthcare Providers in Reducing the Burden Associated with Neurogenic Orthostatic Hypotension. Neurol Ther 9, 205–211 (2020). https://doi.org/10.1007/s40120-020-00203-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-020-00203-6