Abstract
Introduction
Intermittent cardiac output (CO) studies using thermodilution are considered the gold standard. We have developed a stroke volume (SV) calculator from pulmonary pulse pressure (PP) to allow continuous monitoring of SV and CO from PP.
Methods
Hemodynamic data on 169 patients following orthotopic heart transplantation were used to compare our calculator-derived SV (and SV index, or SVi) against thermodilution-derived SV on admission into intensive care unit immediately following heart transplantation (T0) and 6 h after admission (T6).
Results
The calculated SV correlated with thermodilution-derived SV T0 (r = 0.920, p < 0.001, coefficient of 0.539 and the constant of 2.06). The median calculator SV, adjusted for coefficient and constant, was 48.4 ml (37.7, 60.7), comparable to the median thermodilution-derived SV 47.9 ml (37.5, 61.0), p = 0.737 with acceptable agreement on Bland–Altman plots. The thermodilution-derived SVi was 28.1 ml (19.7, 38.7) and adjusted calculator-derived SVi 28.9 ml (19.7, 39.9), p = 0.781. At T6, median thermodilution-derived SVi was 27.7 ml (19.5, 35.9) compared to the calculator-derived SVi median of 26.1 ml (17.7, 37.7), p = 0.203.
Conclusions
Changes in PP can be used to track changes in SV using this calculator. Changes in PP may be used to assess response to treatment in the early post-operative period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Real-time monitoring of cardiac output may facilitate early recognition of hemodynamic deterioration, but real-time monitoring of cardiac output is not currently available. |
What was learned from the study? |
The calculator developed in this study using pulmonary artery pulse pressure has acceptable agreement with thermodilution derivation of stroke volume. |
Once calibrated, changes in pulmonary artery pulse pressure can be used to derive stroke volume with acceptable agreement with thermodilution-derived stroke volume. |
Future studies should evaluate this calculator in other clinical settings. |
Introduction
Determination of blood flow, i.e., stroke volume (SV) and cardiac output (CO), is an integral part of hemodynamic monitoring in intensive care medicine. Despite the availability of less- or non-invasive technologies, intermittent CO monitoring (thermodilution) using the pulmonary artery catheter (PAC) remains the most widely used modality [1] in critically ill patients with circulatory shock. However, the intermittent nature of CO measurement is a limitation, especially in rapidly changing hemodynamic conditions, such as during dynamic tests of preload responsiveness (e.g., passive leg raising) and therapeutic interventions such as fluid or vasopressor administration.
‘Continuous’ pulmonary artery thermodilution measures CO without the need for intermittent manual indicator injection (e.g., intermittent thermal filament heating). However, in practice, ‘continuous’ CO measurements are intermittent averaged values (averaging improves the signal-to-noise ratio but causes a delay of several minutes). The agreement with intermittent thermodilution is modest [2] and catheters are expensive.
Pulmonary artery pulse pressure (PP) is directly related to SV, a relationship that is modified by pulmonary vascular resistance (R). The purpose of this study was to develop a SV calculator from PP to allow continuous monitoring of SV and CO from PP based on this relationship between PP and SV. We evaluated this calculator in a cohort of patients who underwent heart transplantation. From our previous study [3], we noted no significant changes in R from admission into intensive care unit post-heart transplantation (T0) to 6 h post-admission into the intensive care unit (T6). On this basis, we hypothesized that PP can be used to track SV changes from T0 to T6.
Methods
Theoretical Basis
Analogous to the charging of capacitors, a significant proportion of the right ventricular SV ‘charges’ the reservoir volume and increases pressure in the compliant pulmonary arteries in systole, which discharges during diastole. Total pulmonary arterial capacitance (C) defines this relationship between volume and pressure as the increase in blood volume (ΔV) in the arterial system that produces a unit increase in arterial transmural pressure. In practice, C is difficult to measure because direct measurement of ΔV is not possible due to the continuous outflow from the arterial system. Therefore, the ratio of SV/PP has been used to determine C, accepting that this equation overestimates the true C.
Rearranging this equation:
RC is related to pulmonary arterial wedge pressure (PAWP) as previously described by Tedford et al. [4] and Lankhaar et al. [5, 6]: RC = - 0.0063 × PAWP + 0.46.
Therefore,
Or
to derive SV in ml.
Based on this equation, SV is predominantly related to PP and R. Changes in absolute levels of PAWP have a modest effect on absolute SV. For example, at a constant R of 2.0WU and PP of 20 mmHg, doubling PAWP from 12 to 24 mmHg is associated with a decrease in SV from 64 to 51 ml. However, at PAWP of 12 mmHg and PP of 20 mmHg, SV increases from 64 to 85 ml if PVR is reduced from 2.0 to 1.5 WU.
In the absence of significant changes in R, PP is predominantly related to absolute SV. We hypothesized that changes in PP can be used to track changes in SV and CO in acute settings where R is unchanged.
Study Design
This is a retrospective study that included consecutive patients who underwent orthotopic heart transplantation from two centers from 2019 to 2022. Patients who underwent post-transplant mechanical circulatory support were excluded (n = 43). Hemodynamic data from pulmonary artery catheterization were collected at two separate time points: immediately following admission into intensive care unit post-heart transplantation (T0) and at 6 h thereafter (T6) were used. Fully anonymized data were collected as part of the evaluation of post-transplant management and approved by our institution, University Hospitals Birmingham NHS Foundation Trust (CARMS-18295). Patient consent was not needed, and this study complies with the ethical framework outlined by the NHS Health Research Authority.
This study has two parts: Firstly, we tested the agreement between the calculator-derived SV (i.e., calculator SV) and the SV derived from conventional thermodilution CO (i.e., thermodilution SV) studies at T0.
Secondly, we simulated the condition where repeat thermodilution and wedge studies were not available, so the pulmonary vascular resistance was assumed to be unchanged from baseline. For this simulation, we used baseline (T0) R to ‘calibrate’ the calculator and pulmonary artery diastolic pressure (PADP) at T6 to replace PAWP at T6. The calculator SV using these assumptions were compared against the ‘true’ thermodilution SV.
Statistical Analysis
All data were analyzed for normality with histograms and the Shapiro–Wilk test. Normally distributed data are expressed as mean and standard deviation and non-parametric data are expressed as median and interquartile range (IQR). The Mann–Whitney U test was employed to compare non-parametric data. A p < 0.05 was considered statistically significant.
Correlation and linear regression analyses were performed comparing the calculator-derived SV and the thermodilution-derived SV and SV index (SVi, indexed to body surface area). The calculator SV were adjusted based on the coefficient and constant. The differences, percentage change, and mean between the calculator and thermodilution-derived SV were then calculated and Bland–Altman plots were constructed. The percentage error (i.e., accuracy), derived by the Bland–Altman analysis, is the difference in the measured value from the reference method.
There is inherent error in cardiac output measurements by thermodilution (limits of precision of ± 10–20%). When comparing the current calculator against this reference method (thermodilution), the limits of agreement will inevitably be larger than the limits of precision of the reference method (combining the errors of the test and reference methods). On the basis of an analysis of 25 studies, Critchley et al. [7] suggested that a value of up to 30% is considered clinically acceptable, and this is the limit that we have adopted in this study.
Pearson correlation was performed comparing the raw calculator SV with CO-derived SV and the coefficient and constant yielded was used to adjust the raw calculator SV data. All statistical analyses were performed on IBM SPSS Statistics for Mac, Version 29.0. IBM Corp., Armonk, NY, USA.
Results
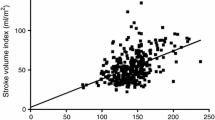
This study included 169 patients who underwent orthotopic heart transplantation from two centers from 2019 to 2022 (Table 1). Hemodynamic data at T0 and T6 are displayed in Table 2. The median thermodilution-derived SV was 47.9 ml (37.5–61.0 ml) and the median calculated SV was 87.4 ml (66.1, 110.1). Calculator SV correlated with thermodilution-derived SV at T0 (r = 0.920, p < 0.001, coefficient of 0.539 and the constant of 2.06) (Fig. 1). After applying the coefficient and constant to the calculator SV, the adjusted median calculator SV was 49.1 (37.4, 63.1) ml. There was no significant difference between the adjusted calculator SV compared with the CO-derived SV (49.1 ml (37.4, 63.1) vs. 48 ml (37, 62.8), p = 0.780).
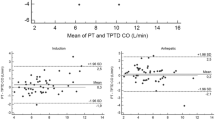
The median difference at T0 between the adjusted calculator SV and thermodilution-derived SV was – 0.052 ml (– 4.12, 4.46), the median percentage change was – 0.078% (– 8.86, 11.6). The difference between the calculator SV and thermodilution-derived SV was not statistically significant (mean – 0.04, SD: 7.97, p = 0.944). The absolute difference between the adjusted calculator SV and the CO-derived SV at T0 was plotted against the mean on Bland–Altman plot [Fig. 2, the red line denoting the mean difference of – 0.043 ml and the black lines representing the 95% confidence interval (95% CI – 15.6 to 15.6)]. The mean percentage change between the adjusted calculator SV and thermodilution-derived SV was 1.83% and 95% CI (– 27.2 to 30.8) (Fig. 3).
a T0 Bland–Altman plot of absolute difference between the adjusted calculator stroke volume (SV) and the thermodilution-derived stroke volumes. The red line denotes the mean ( – 0.04 ml) and the dotted black lines denote the 95% confidence interval (– 15.6 to 15.6). b T0 Bland–Altman plot of absolute difference between the adjusted calculator SV index (SVi) and the thermodilution-derived stroke volume index. The red line denotes the mean (0.0253 ml) and the dotted black lines denote the 95% confidence interval (– 9.33 to 9.38). T0: immediately following orthotopic heart transplantation
a T0 Bland–Altman plot of percentage difference between the adjusted calculator stroke volume (SV) and the thermodilution-derived stroke volumes. The red line denotes the mean (1.83%) and the dotted black lines denote the 95% confidence interval (– 27.2 to 30.8). b T0 Bland–Altman plot of percentage difference between the adjusted calculator SV index (SVi) and the thermodilution-derived stroke volume indices. The red line denotes the mean (1.96%) and the dotted black lines denote the 95% confidence interval (– 27.2 to 31.2). T0: immediately following orthotopic heart transplantation
For indexed stroke volume (stroke volume index, SVi), the median thermodilution-derived SVi was 28.1 ml (19.7, 38.7) and the median calculator SVi was 51.2 ml (34.7, 71.2). Correlation and linear regression analysis showed strong correlation with R2 of 0.911, and a coefficient and constant of 0.552 and 0.6, respectively. The adjusted calculator SVi median was 28.9 ml (19.7, 39.9) compared to the CO-derived SVi of 28.1 ml (19.7, 38.7), and there was no significant difference p = 0.781. Bland–Altman plots for SVi are displayed in Figs. 2b and 3b. Over 95% of the calculator SV were within the 30% limit of agreement with thermodilution-derived SV.
Stroke volume was calculated at T6, adjusted using the same coefficients and constants as above and compared to thermodilution-derived SV, using the simulated conditions where repeat pulmonary vascular resistance measurements were not available. Using the R at baseline (T0) to ‘calibrate’ the calculator and PADP at T6 (instead of PAWP at T6), we found no significant difference between the thermodilution-derived SV vs. the calculator SV at T6: 47.7 ml (37.6, 58.9) vs. 46.4 ml (33.2, 59.6), p = 0.251. The median thermodilution-derived SVi was 27.7 ml (19.5, 35.9) compared to the median adjusted calculator SVi of 26.1 ml (17.7, 37.7) and this was also not statistically significant p = 0.203; suggesting that once ‘calibrated’ at baseline, PP can be used to derive SV at T6. The Bland–Altman plots for T6 are displayed in Figs. 4 and 5. With these assumptions under simulated conditions, there appeared to be greater scatter (about 25% exceeded the 30% limit of agreement), especially at higher SV.
a T6 Bland–Altman plot absolute difference between the adjusted calculator stroke volume (SV) (simulated conditions) and the thermodilution-derived stroke volumes. The red line denotes the mean (0.18 ml) and the dotted black lines denote the 95% confidence interval ( – 41.8 to 42.2). b T6 Bland–Altman plot absolute difference between the adjusted calculator stroke volume index (SVi) (simulated conditions) and the thermodilution-derived stroke volume indices. The red line denotes the mean (0.16 ml) and the dotted black lines denote the 95% confidence interval ( – 22.7 to 23.1). T6: 6 h following orthotopic heart transplantation
a T6 percentage difference between the adjusted calculator stroke volume (SV) (simulated conditions) and the thermodilution-derived stroke volumes. The red line denotes the mean 4.07% and the dotted black lines denote the 95% confidence interval (– 94.7 to 102.9). b T6 percentage difference between the adjusted calculator indices (SVi) (simulated conditions) and the thermodilution-derived stroke volume indices. The red line denotes the mean 4.03% and the dotted black lines denote the 95% confidence interval (– 93.7 to 101.8). T6: 6 h following orthotopic heart transplantation
Discussion
In this study, we have shown that in a cohort of patients who underwent heart transplantation, our calculator once ‘calibrated’ from baseline pulmonary vascular resistance, can track SV from PP within a 6-h interval with an acceptable level of agreement between the calculator-derived and thermodilution-derived SV. Over 95% of the calculator SV were within the 30% limit of agreement with thermodilution-derived SV in an cohort of patients who underwent heart transplantation. There was greater scatter (lower agreement) under the simulated conditions, especially at higher SV.
There are limitations to all CO monitoring devices and technology. The main limitation of calculator-derived (other than the invasiveness of PAC) is the inherent assumptions. Firstly, the pulmonary artery capacitance is calculated as a simple ratio of SV to PP, which overestimates true capacitance. Secondly, the RC time constant reported by Tedford et al. is derived from simple regression of hemodynamic data from a large, mixed cohort of patients. Nonetheless, this simple calculator appears to perform within acceptable limits. We further evaluated this calculator using published data. For example, taking pooled data from 47 publications [8] that described 72 individually evaluated populations comprising of 1187 subjects, the calculator-derived SV of 91 ml is close to the reported mean SV of 96 ml.
Potential applications include the assessment of SV response to intravenous fluid administration or inotropes, both are common interventions in (cardiac) intensive care units. Rapid intravenous fluid administration such as fluid challenges do not appear to have a significant effect on pulmonary vascular resistance. For example, the study by Fujimoto et al. [9] showed no significant changes in pulmonary vascular resistance with rapid saline infusions of 10–15 ml/kg in individuals without heart failure and 0.3–1.0 l of normal saline in patients with heart failure. Similarly, Andersen et al. [10] reported no significant change in pulmonary vascular resistance with fluid administration in patients with heart failure. Indeed, our calculator-derived SV also appears to operate within acceptable limits compared to the hemodynamic data reported by Andersen et al. (Supplementary Material).
One caveat is that the increase in PAWP could confound the relationship between PP and SV. An increase in PAWP would increase PP, even if SV is unchanged. There are two mitigating factors. Firstly, the effect of PAWP on PP and absolute calculator SV is modest. Secondly, PADP can be used to approximate PAWP in most cases in the absence of pulmonary vascular disease. Thus, once ‘calibrated’ with baseline pulmonary vascular resistance and using PADP, the changes in SV in response to fluid administration could be quantified:
to derive SV in ml.
Our data suggest that these assumptions reduced the agreement between calculator SV and thermodilution SV (about 25% exceeded the 30% limit of agreement), but was acceptable in the majority of patients within the first 6 h of heart transplantation. It is likely that a more selected use of this calculator (identifying conditions where these assumptions are valid) would improve the level of agreement.
Aside from the calculator, the physiologic considerations also allow the following ‘rules-of-thumb’ to be applied:
-
1.
With acute intravenous fluid administration, at an unchanged R, the absence of an increase in PP with would suggest the absence of stroke volume increase in response to the fluid challenge.
-
2.
With the administration of inotropes, the potential reduction in R and PAWP would be expected to reduce PP. An increase in PP in response to inotropes must reflect an increase in SV.
Limitations
This study has notable limitations. First, we have only evaluated this calculator in patients who have had heart transplantations. The application of this calculator to other patients would need further study. Secondly, the measurements were not standardized. It is possible that standardization of PP measurement (e.g., during expiratory phase) may improve agreement between the calculator- and thermodilution-derived SVi and CO. Thirdly, we have evaluated a 6-h window early post-transplant, as we have previously shown that pulmonary vascular resistance did not change significantly over this time interval. It is possible that the window may be extended in the absence of any significant changes in ventilatory parameters that could alter pulmonary vascular resistance. Alternatively, this calculator may be used to complement intermittent thermodilution studies (e.g., six-hourly) to derive R to ‘re-calibrate’ the calculator. Finally, although there was general agreement between calculator SV and thermodilution SV under simulated conditions at T6, the level of agreement was poorer and there were individuals with clinically significant deviations; implying that these assumptions are not valid in some patients. Future studies are needed to further examine the use of this calculator.
Conclusions
We describe a calculator to derive SV from PP, as an adjunct to aid continuous hemodynamic monitoring following heart transplantation. Once ‘calibrated’ from baseline pulmonary vascular resistance, this calculator may be used to track SV from PP within a 6-h interval with acceptable level of agreement with thermodilution-derived SV in a selected group of patients.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Judge O, Ji F, Fleming N, Liu H. Current use of the pulmonary artery catheter in cardiac surgery: a survey study. J Cardiothorac Vasc Anesth. 2015;29:69–75. https://doi.org/10.1053/j.jvca.2014.07.016.
Kouz K, Michard F, Bergholz A, Vokuhl C, Briesenick L, Hoppe P, et al. Agreement between continuous and intermittent pulmonary artery thermodilution for cardiac output measurement in perioperative and intensive care medicine: a systematic review and meta-analysis. Crit Care. 2021;25:125. https://doi.org/10.1186/s13054-021-03523-7.
Lim HS, Ranasinghe A, Chue C, Quinn D, Mukadam M, Mascaro J. Cardiac power output index and severe primary graft dysfunction after heart transplantation. J Cardiothorac Vasc Anesth. 2021;35:398–403. https://doi.org/10.1053/j.jvca.2020.07.020.
Tedford RJ, Hassoun PM, Mathai SC, Girgis RE, Russell SD, Thiemann DR, et al. Pulmonary capillary wedge pressure augments right ventricular pulsatile loading. Circulation. 2012;125:289–97. https://doi.org/10.1161/CIRCULATIONAHA.111.051540.
Lankhaar J-W, Westerhof N, Faes TJC, Marques KMJ, Marcus JT, Postmus PE, et al. Quantification of right ventricular afterload in patients with and without pulmonary hypertension. Am J Physiol Heart Circ Physiol. 2006;291:H1731–7. https://doi.org/10.1152/ajpheart.00336.2006.
Lankhaar J-W, Westerhof N, Faes TJC, Gan CT-J, Marques KM, Boonstra A, et al. Pulmonary vascular resistance and compliance stay inversely related during treatment of pulmonary hypertension. Eur Heart J 2008;29:1688–95. https://doi.org/10.1093/eurheartj/ehn103.
Critchley LA, Critchley JA. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput. 1999;15:85–91. https://doi.org/10.1023/a:1009982611386.
Kovacs G, Berghold A, Scheidl S, Olschewski H. Pulmonary arterial pressure during rest and exercise in healthy subjects: a systematic review. Eur Respir J. 2009;34:888–94. https://doi.org/10.1183/09031936.00145608.
Fujimoto N, Borlaug BA, Lewis GD, Hastings JL, Shafer KM, Bhella PS, et al. Hemodynamic responses to rapid saline loading: the impact of age, sex, and heart failure. Circulation. 2013;127:55–62. https://doi.org/10.1161/CIRCULATIONAHA.112.111302.
Andersen MJ, Olson TP, Melenovsky V, Kane GC, Borlaug BA. Differential hemodynamic effects of exercise and volume expansion in people with and without heart failure. Circ Heart Fail. 2015;8:41–8. https://doi.org/10.1161/CIRCHEARTFAILURE.114.001731.
Funding
No funding or sponsorship was received for this study or publication of this article.
Author information
Authors and Affiliations
Contributions
Ivan H. W. Yim: Data collection and analyses. Nigel E. Drury: Manuscript review and revision. Hoong Sern Lim: Study conception, data analyses and manuscript preparation/review.
Corresponding author
Ethics declarations
Conflict of Interest
Ivan H. W. Yim, Nigel E. Drury and Hoong Sern Lim have no conflicts of interest related to this work. Hoong Sern Lim is an Editorial Board member of Cardiology and Therapy. Hoong Sern Lim was not involved in the selection of peer reviewers for the manuscript nor any of the subsequent editorial decisions.
Ethical Approval
Fully anonymized data were collected as part of the evaluation of post-transplant management and approved by our institution, University Hospitals Birmingham NHS Foundation Trust (CARMS-18295). Patient consent was not needed, and this study complies with the ethical framework outlined by the NHS Health Research Authority.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yim, I.H.W., Drury, N.E. & Lim, H.S. Derivation of Stroke Volume from Pulmonary Artery Pressures. Cardiol Ther 13, 401–413 (2024). https://doi.org/10.1007/s40119-024-00360-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-024-00360-x