Abstract
Introduction
This study aimed to quantify the contribution of various obstacles to timely reperfusion therapy in acute ST-elevation myocardial infarction (STEMI) and to improve performance in a mixed remote rural/urban region.
Methods
From November 1, 2020 to April 23, 2021, patients with acute STEMI were prospectively monitored with the critical time intervals, treatment modalities, and outcomes registered. Selected clinical decision-makers in 11 hospitals were appointed as improvement agents and systematically provided with weekly updated information about absolute and relative performance. Suggestions for improvements were invited and shared.
Results
Only 29% of the 146 patients received reperfusion therapy within recommended time limits [prehospital thrombolysis, 2/48; in-hospital thrombolysis, 0/20; primary percutaneous coronary intervention (pPCI), 37/68, with median intervals from the first medical contact of 44, 49, and 133 min, respectively]. Efficiency varied considerably between health trusts: median time from the first medical contact to prehospital thrombolysis ranged from 29 to 54 min (hazard ratio 4.89). The predominant, remediable causes for delays were erroneous tactical choices and protracted electrocardiographic diagnostication, decision-making, and administration of fibrinolytic medication. During the trial, the time to pPCI was non-significantly reduced.
Conclusion
We found several targets for system improvements in order to mitigate reperfusion delays along the entire chain of care, regardless of reperfusion modality chosen. More patients should receive prehospital thrombolysis. The most important measures will be training to ensure a more efficient on-site workflow, improved protocols and infrastructure facilitating the communication between first responders and in-hospital clinicians, and education emphasizing prehospital transport times.
Clinical Trials Identifier
NCT04614805.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The proportion of patients receiving rapid reperfusion therapy for acute ST-elevation myocardial infarction in North Norway has over many years been below guideline recommendations and inferior to the rest of our country. |
We aimed to identify, quantify, and overcome barriers to rapid reperfusion therapy. |
Of the 146 patients in the trial, 29% received reperfusion therapy within recommended time limits without any significant improvement during 6 months. |
Too few patients received thrombolytic therapy and hardly anyone did so within the recommended time frame. |
Future improvement efforts should target decision-making, electrocardiographic diagnostication, and on-scene workflow as these factors were the most important, remediable causes for delayed treatment. |
Introduction
Rapid reperfusion therapy in acute ST-elevation myocardial infarction (STEMI) improves health and saves lives. The interval between the first medical contact (FMC) and electrocardiogram (ECG) interpretation should not exceed 10 min. This should be followed by either primary percutaneous coronary intervention (pPCI) within the next 90 min or, if pPCI cannot be reached within this time frame, intravenous (i.v.) fibrinolytic medication should be given within 10 min following the STEMI diagnosis [1]. The University Hospital of North Norway systematically implemented prehospital thrombolysis (PHT) in 1999 in collaboration with the municipality health services. The program included the training of 300 paramedics, local nurses, and general practitioners. The average time saved by providing PHT instead of PCI as the first reperfusion attempt was estimated to be 131 min. The proportion given PHT within 2 h of symptom onset increased from 21% (2000–2003) to 39% (2008–2011), and the incidence of post-STEMI heart failure was more than halved [2]. Despite this pioneering effort, 14 years later less than one-third of patients in Northern Norway received reperfusion therapy within the recommended time limits (2014–2018) [3]. In contrast, the national average has gradually increased from 51% in 2015 to 63% in 2020. The large geographical differences implied a potential for improvement of acute STEMI care and prompted a concerted action, relying on the mobilization of clinical decision-makers and prehospital care providers across all hospitals in our region. Our main objectives were to identify the causes for delays, quantify the contribution of individual barriers to timely treatment, and regularly provide rapid feedback on performance, aiming at short-term gains as well as the creation of a platform for long-term system improvement.
Methods
Setting
The North Norway Regional Health Authority encompasses 11 governmental emergency hospitals which provide acute cardiac care. These are organized within four local health trusts. Population density, hospital locations, and service levels are shown together with airborne resources in Fig. 1. The catchment area has 485,000 inhabitants and covers 113,000 km2 in addition to the Svalbard archipelago. The region’s university hospital runs a 24-h catheterization laboratory, and one other hospital delivers PCI during ordinary hours. The municipalities provide physician-manned out-of-hours primary care at 52 locations. The ambulance services are operated by the health trusts with 119 ground, 9 boat, and 13 air ambulances (7 helicopters and 6 fixed-wing aircraft). All units are professionally staffed and equipped with the Corpuls® apparatus (GS Elektromedizinische Geräte, Kaufering, Germany) for continuous monitoring and immediate electronic 12-lead ECG transmission to dispatch centers and hospitals in the region. Fixed-wing air-ambulance flight time from the 24 airports to the 24/7 PCI center varies from 20 to 75 (median 50) min [4]. In 2020, a regional protocol based on the 2017 European Society of Cardiology guidelines [1] was implemented which covers diagnosis and treatment as well as communication and transfer procedures regarding acute coronary syndromes.
Area covered by the North Norway Regional Health Trust (except the arctic islands) with its 11 somatic acute care hospitals of which one provides percutaneous coronary interventions round the clock and another exclusively during ordinary working hours. Air ambulance bases are shown. The population density is depicted for each municipality. There are 26 operative airports in the area (not shown)
Improvement Strategy and Data Collection
Our basic assumption was that a robust, lasting improvement of acute STEMI treatment could most effectively be achieved by targeting the interaction between clinicians in leadership roles and front-line care providers. We anticipated that frequent and regular feedback on results in near real-time combined with sharing of experiences and ideas would heighten awareness and facilitate knowledge distribution along the entire chain of care, conferring improved workflow and adherence to guidelines. We established a consort of clinical leaders from the 11 emergency hospitals in the region. Our effort to minimize avoidable delays to reperfusion therapy in STEMI was based on evidence-based principles [5] relying on (i) mobilization of hospital leaders and front-line providers by alerting them to substandard care as indicated by national registry data [3], (ii) frequent and systematic feedback of performance to improve knowledge and keep up awareness, (iii) continuous sharing of experience and ideas, (iv) emphasis on geographical differences as indicators of potentially correctable system failures, and (v) repeated distribution of evidence-based guidelines. The protocol was shared with the health trusts’ leaderships, the health workers’ unions, and the chief county, district, and city medical officers. At each hospital site, clinical leaders responsible for acute STEMI care and with the authority to initiate and monitor improvement measures were appointed.
The local collaborators identified patients with STEMI and an indication for immediate reperfusion therapy (intention to treat with thrombolytic medication or pPCI) within 24 h after admission and prospectively monitored the clinical course, decision-making, treatment, critical time intervals, and causes of delays. The data were obtained from pre- and in-hospital records and interviews with personnel involved in the patient’s care, recorded in a standardized form with pre-specified categories, and transferred to the university clinic for immediate analysis.
We wanted to compare our results with those quality performance indicators of the Norwegian Myocardial Infarction Registry [3] which are limited to patients less than 85 years of age presenting within 12 h after symptom onset, and assumed that the intervention could be reliably evaluated following inclusion of at least 100 patients. Inclusion took place from November 1, 2020 to April 23, 2021 (n = 135). Retrospective assessment by searching electronic patient records for admissions with a diagnosis of acute myocardial infarction revealed that three had inadvertently been omitted, giving an inclusion rate of 98%. The database was retrospectively completed to encompass the entire STEMI population (n = 146). Thus, we were able to give a complete picture of the acute reperfusion therapy provided for patients with STEMI within our region corresponding to an all-comers design.
The interim results, essential learning points, and suggestions for improvement were systematically shared at the end of each week through an updated electronic newsletter distributed to each hospital and to the public health authorities in each municipality.
Research Ethics
The regional board of medical ethics considered that approval of the study protocol by the board was not required.
Statistical Analyses
The data were entered into an electronic database (Microsoft Excel®) and analyzed by the Stata software (StataCorp LLC, College St., Texas, USA). To test whether variables were normally distributed, we used the Shapiro–Wilk W test, in order to determine if the prerequisites for parametric testing were fulfilled. We used the Cox regression model for time-to-event analyses. The proportional hazard function assumption was verified using statistical tests and graphical diagnostics based on Schoenfeld residuals.
Results
Patients and Initial Care
The characteristics of the patient population, their care providers, treatment, and outcomes are shown in Table 1. Thirty-seven (25%) of the 146 patients were women. The mean age was 67 (range 27–94) years. The women were on average 5 years older than the men. The initial reperfusion therapy was PHT for 48 patients (33%), in-hospital thrombolysis (IHT) for 20 (14%), pPCI for 68 (47%), and coronary artery bypass surgery for 1 (1%). Nine patients (6%) did not receive any reperfusion attempt in the acute phase. Sixty-three pPCI procedures were performed at the university hospital and five at the other, daytime PCI clinic. Of those who received pPCI, 32 out of 68 were from a non-PCI hospital catchment area. Of these, seven patients were admitted directly to a PCI facility, bypassing their nearest emergency hospital (Table 1). Fifty-nine out of the 68 who received thrombolytic therapy received PCI in the acute or subacute phase (pharmacoinvasive therapy) (Fig. 2).
Timeline for all patients who received reperfusion therapy in the acute phase of an ST-elevation myocardial infarction from November 1, 2020 to April 23, 2021. Bar thickness indicates the number of patients at each point in time. Bar length indicates the duration of the indicated time intervals (median; interquartile range in parentheses). Dashed arrows depict time limits recommended in guidelines [1]. FMC, first medical contact; PHT, prehospital thrombolysis; IHT, inhospital thrombolysis; PCI, percutaneous coronary intervention. The time of the initiation of intravenous fibrinolytic drug administration and the time of arterial puncture are indicated for thrombolysis and PCI, respectively
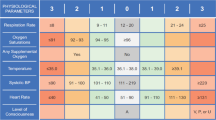
Critical Time Intervals
The overall performance of our health care system with respect to meeting guideline targets is shown in Fig. 2 and Table 2. The median time from symptom onset to notification of the emergency medical services was 72 min [interquartile range (IQR) 20–208]. In response, health care professionals reached 75% of the patients within 22 min (Fig. 6, Supplementary Material). Among patients receiving acute reperfusion therapy, 61 out of 137 (44%) had a 12-lead ECG recorded within 10 min after FMC (Fig. 2, Fig. 7A, Supplementary Material).
Only in two out of 48 cases was PHT administration initiated within the recommended 20 min after FMC, with a median interval of 44 min (IQR 22) (Fig. 7B, Supplementary Material). The prehospital on-scene efficiency varied considerably among the health trusts. The median values (with IQR) were 54 (39), 40 (9), 45 (16), and 29 (17) min for the various trusts (Fig. 3), and the proportions meeting the time target were 0/15, 0/5, 1/18, and 1/10, respectively. The differences with respect to the interval between ECG transmission and the decision to administer PHT was significant (P = 0.02) with a hazard ratio of 5.13 [95% confidence limits (CL) 1.63–16.13] between the most and the least efficient trust (P = 0.005). The time from reaching a PHT decision to its administration also differed (P = 0.003) with a hazard ratio of 12.89 (95% CL 3.19–52.08, P < 0.001) when comparing the extremes (Fig. 3). A multivariable Cox regression analysis incorporating gender, age, and interval from symptom onset to FMC demonstrated that the difference among the four health trust catchment areas with respect to the FMC–PHT interval was highly significant. At any given time, the best health trust had 4.9 times greater hazard for timely treatment than the poorest (hazard ratio 4.89, 95% CL 1.92–12.45, P = 0.001).
Critical time intervals between the first medical contact (FMC) to initiation of prehospital thrombolytic therapy (PHT) in 48 patients with acute ST-elevation myocardial infarction are depicted, stratified on each health trust’s catchment area. For the entire FMC–PHT interval (left panel), the median values were 29 (19), 40 (6), 45 (20), and 54 (39) min, respectively. When the health trust with the longest intervals was used as reference, the hazard ratios (interquartile range and 95% confidence limits are given in parentheses following medians and hazard ratios, respectively; hazard ratios were determined by Cox regression analyses) for the other trusts were 3.35 (1.11–10.13), 1.95 (0.93–4.08), and 5.35 (2.17–13.18), P = 0.004. For the interval from electronic electrocardiogram (ECG) transmission to the decision was made to give PHT (middle panel), the median values were 5 (1), 5 (4), 8 (8), and 12 (7), respectively. Considering the ECG transmitted–PHT decision interval as a dependent variable and the catchment areas as predictor variables, the hazard ratio between the best and poorest results is 5.13 (1.63–16.13), P = 0.005. The median time from the PHT decision to PHT administration was 4 (3), 12 (8), 12 (12), and 21 (3) min for the respective trusts (right panel). The hazard ratio when comparing the best result with the poorest was 12.89 (3.19–52.08), P < 0.001
A long interval between FMC and administration of fibrinolytic medication was associated with reduced left ventricular systolic function as measured by the ejection fraction (EF) [odds ratio (OR) 1.05, 95% CL 1.01–1.09, P = 0.023] (data not shown). Thus, for every extra minute of time to PHT, the risk of left ventricle deterioration below an EF of 40% increased by 5%.
For those 20 patients who received IHT, the median time from FMC was 49 (IQR 35, range 30–438) min and none, not even two patients with in-hospital onset, reached the 20-min time target (Fig. 7C, Supplementary Material).
For the FMC–pPCI interval, the median was 133 (IQR 553, range 45–2639) min (Fig. 7D, Supplementary Material, Tables 2, 3) and slightly better for those less than 85 years of age presenting within 12 h (median 114 (IQR 307) min). Of these, 29 out of 49 received pPCI within 120 min after FMC.
The median time from ECG taken to pPCI was 111 (IQR 486) min; among those patients, 37 out of 68 received pPCI within 2 h after ECG (data not shown). Differences among health trust catchment areas were substantial, as proportions within the 2-h interval were 0/6, 32/37, 5/17, and 0/8, respectively (P = 0.001). For those less than 85 years of age and presentation within 12 h, the median was 88 (IQR 309 min), 34 out of 49 within 2 h (Table 3).
Our data show that reperfusion therapy was initiated within the recommended time for a mere 39 out of 136 (29%) (exempting a single CABG case), and 36 out of 117 (31%) when considering only those less than 85 years of age and presentation within 12 h after onset of symptoms (Table 2).Footnote 1 In terms of time targets met, performance improved only subtly and not statistically significantly over the course of the study (Fig. 4).
For 136 patients with acute ST-elevation myocardial infarction, the time from the first medical contact (FMC) to the first reperfusion therapy administration [thrombolysis; n = 68 (prehospital; 48, in-hospital; 20), primary PCI (pPCI), n = 68] is shown as a function of the duration of the trial. pPCI, P = 0.678; thrombolysis, P = 0.977 [linear regression analysis based on transformed data: 1/√(FMC-thrombolysis interval) and 1/(FMC–pPCI interval)]. PCI, percutaneous coronary intervention; ◯, thrombolysis; ●, pPCI; ···, linear trend thrombolysis; —, linear trend pPCI
Analysis of Delayed Reperfusion
For 78 of the 97 patients receiving reperfusion therapy later than recommended, experienced clinical leaders identified a single, major reason (Table 4). Tardy establishment of a correct ECG diagnosis was the predominating cause and pertained to 17 of those eventually receiving i.v. fibrinolytic medication. A long interval from symptom onset to FMC was also important, rendering patients outside the thrombolysis time-window in 13 out of 38 cases of delayed pPCIs.
In 12 cases, the primary ECG interpretation was wrong (Table 4). For 22 patients, a definite ECG diagnosis constituting indication for reperfusion therapy was not obtained during the FMC. Thirteen of those did not present with ST elevations at that time (Table 5). For various reasons including technical ECG issues and overly optimistic transport time estimates, 11 out of 20 patients had a clear PHT indication but received their—delayed—fibrinolytic medication only after hospital admission (Table 6).
Improvement Measures
During and immediately after the trial period, local clinical leaders launched several improvement initiatives (Table 7).
Mortality
The 30-day case fatality rate was 12% (coinciding with national results from the Norwegian Myocardial Infarction Registry), and total mortality after 1 year was 15% (Table 1, Fig. 5). The corresponding values for those who received reperfusion therapy in the acute phase were 8% and 12%, respectively, regardless of modality (data not shown). Anterior wall infarctions were 2.5 times more lethal (14/62) than inferior wall infarctions (6/67) at day 518 after trial initiation with a hazard ratio of 2.34 (95% CL 0.88–6.23) when adjusted for age and gender (P = 0.08). There was a strong association between the last EF measured during the index hospital stay and case fatality rate (hazard ratio 0.90, 95% CL 0.85–0.96, P = 0.001) which was maintained after adjustment for age and gender (hazard ratio 0.93, 95% CL 0.87–0.99, P = 0.04) (not shown).
Discussion
We here quantitatively describe remediable barriers to timely reperfusion in acute STEMI.
Our region is characterized by long prehospital times, as the median time from FMC to admission at first hospital was 91 (IQR 98) min. In contrast, a mean of only 41 (weighted mean, range 21–88) min was reported in a large meta-analysis including 125,343 patients with STEMI in 100 studies from 20 countries [7]. In line with this observation, we found an interval of 133 min (median) from FMC to pPCI as compared to 96 min (mean) in the meta-analysis [7]. The lengthy prehospital transport for most of our patients with acute STEMI, in particular to the 24/7 invasive cardiology center, mandates instant access to thrombolytic therapy provided by the local emergency services. Our region does indeed stand out because of its extensive use of thrombolysis, with a threefold higher proportion than Norway as a whole [3]. Nevertheless, underutilization of PHT in a deliberate pharmacoinvasive strategy is a main reason for avoidable delays. Too few patients received such treatment, and most of them too late. This is a general experience, as an average FMC–PHT interval of less than 20 min was achieved in only 20% of studies [7]. But timely administration of i.v. fibrinolytic medication should be feasible for most patients in our region since 75% of the patients were reached within 22 min by an ambulance equipped with trained staff, diagnostic tools, tenecteplase, and electronic telecommunication systems securing immediate access to real-time cardiological and emergency medicine expertise. The symptom onset–FMC interval was 80 (IQR 150) min, comparable to a Swedish study reporting a median of 70 min [6]. We have shown that timely thrombolysis is feasible—and the only primary reperfusion modality within reach for most patients with STEMI in our health region. The potential to use the pharmacoinvasive strategy more efficiently is evident also from the considerable differences between local health trusts.
A frequent cause of delays was an overly optimistic assumption that IHT or pPCI could be administered within recommended time frames. Moreover, too much time was spent establishing and acting on the ECG diagnosis. Reaching the ECG diagnosis of STEMI followed by a decision to give PHT took on average 19 min from FMC. Administering tenecteplase took another 14 min. ESC guidelines recommend performance goals of less than 10 min for each of these intervals. Not a single patient received i.v. thrombolytic treatment in-hospital within 20 min after FMC. There are amendable bottlenecks regarding both in-hospital and prehospital practical capabilities, on-scene teamwork, and communication skills.
Although somewhat closer to guideline targets, our results for pPCI are also inferior to those of the national total, e.g., 34 out of 49 patients less than 85 years of age received pPCI within 120 min. The main remediable barriers to timely treatment were prehospital and not related to in-hospital logistics, since 29 out of 31 patients within the university hospital’s catchment area were treated within 2 h after the ECG recording. The differences among the health trusts with respect to meeting time targets for pPCI at least partially reflects the geography. None of the patients from the two catchment areas most remote from interventional cardiology hospitals received pPCI within the recommended time limit (data not shown).
Reflected in the regional operating procedures, stable patients with STEMI within timely reach of PCI would preferably be transported immediately to a hospital with PCI capabilities. Notably, in the catchment areas of our non-PCI hospitals, 25 out of 32 patients were first admitted to the local hospital rather than directly to the PCI center. To what extent this practice is rational because of diagnostic uncertainty, need for stabilization, or unavailability of immediate aircraft transport—or instead reflects a suboptimal decision causing avoidable waste of time—will be addressed in subsequent studies.
Attempts at improvement in complex health systems often fail or take several years to succeed. A mere 14% of published research is translated into bedside practice to the benefit of patients [8]. Implementation of evidence-based care must draw on a scientific approach including behavioral research [9]. We have tried to apply prominent features of eminent health organizations like clinical engagement, senior management support, judicious use of data, a thoroughly planned communication strategy emphasizing continuous feedback on performance, collaboration across institutions, raised awareness along the entire chain of care, and a platform for discussion and problem solving [10]. This approach proved insufficient to obtain substantial improvements over the rather short time frame of 25 weeks. Thus, although we observed a modest reduction of the FMC–pPCI interval, this trend was not statistically significant and may as well reflect parallel improvement efforts like the Safe Acute Medicine project.Footnote 2 Nevertheless, the trial has encouraged ongoing efforts and spurred new improvement initiatives in the entire region.
We will proceed by jointly maintaining and expanding measures to improve individual and collective first responder performance. From what we have learnt, we will encourage more working in parallel rather than in sequence in order to further reduce on-site time. We will strive to accelerate decision-making based on authoritative ECG interpretation, also by replacing conventional pagers and telephones with emergency network radio communication optimized for multi-party deliberations involving first responders, the emergency medical communication center, and the internist/cardiologist on call via our emergency medical dispatch centers. To ensure optimal tactical decisions regarding primary reperfusion method and first hospital destination, we will revise our transfer protocols and improve knowledge of regional geography and prehospital logistics in front-line staff education.
Conclusion
We have identified potential targets for improvement efforts to mitigate undue delays along the entire chain of acute STEMI care. More patients should receive prehospital thrombolysis. The most important measures will be training to ensure a more efficient on-site workflow, improved protocols and infrastructure facilitating the communication between first responders and in-hospital clinicians, and education emphasizing prehospital transport times.
Notes
For the pPCI cohort, these values represent the interval commencing with ECG recording and slightly underestimate actual performance since guidelines use the conclusive ECG interpretation as the starting point.
Safe Acute Medicine: A program for guideline implementation including multidisciplinary training to improve decision-making as well as on-scene practical performance and communication skills regarding chest pain, stroke, and septicemia. See: https://unn.no/fag-og-forskning/samhandling/trygg-akuttmedisin.
References
Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2018;39:119–77.
Mannsverk J, Steigen T, Wang H, et al. Trends in clinical outcomes and survival following prehospital thrombolytic therapy given by ambulance clinicians for ST-elevation myocardial infarction in rural sub-arctic Norway. Acute Cardiovasc Care. 2019;8:8–14.
Govatsmark RES, Halle KK, Berge VB, Sneeggen S, Bønaa KH. Annual report of The Norwegian Acute Myocardial Infarction Registry 2020, www.hjerteinfarktregisteret.no. Accessed 14 Oct 2020.
Skår S, De Windt A, Totland J A et al. The future organization of mechanical thrombectomy services for patients with acute cerebral infarction in the North Norway Regional Health Authority. Internal Report, The North Norway Regional Health Authority 2021.
http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx. Accessed 23 Feb 2022.
Thylén I, Ericsson M, Ângerud KH, Isaksson R, Lawesson SS. First medical contact in patients with STEMI and its impact on time to diagnosis; an explorative cross-sectional study. BMJ Open. 2015;2015(5): e007059. https://doi.org/10.1136/bmjopen-2014-007059.
Alrawashdeh A, Nehme Z, Williams B, Stub D. Emergency medical service delays in ST-elevation myocardial infarction: a meta-analysis. Heart. 2020;106:365–73.
Skoien W, Page K, Parsonage W, Ashover S, Milburn T, Cullen L. Use of the theoretical domains framework to evaluate factors driving successful implementation of the accelerated chest pain risk evaluation (ACRE) project. Implement Sci. 2016;11:136.
Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7:37.
Curry LA, Linnander EL, Brewster AL, Ting H, Krumholz HM, Bradley EH. Organizational culture change in US hospitals: a mixed methods longitudinal intervention study. Implement Sci. 2015;10:29.
Acknowledgements
The statistical expertise of Professor T. Wilsgaard, the judicious comments of Professor M. Gilbert, and the advice of our colleagues across the region are greatly appreciated.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author Contributions
Kristian Bartnes: concept and design, data acquisition and analyses, drafting the manuscript; Hilde Albrigtsen: concept and design, data acquisition and analyses, review of the manuscript; Johanne M. Iversen, Henrik Brovold, Niels H. Møller, Bjørn Wembstad, Frode Arstad, Julia Cortis, Siv J. Olsen, Ståle N. S. Nygaard, Sven G. Kindler, Oddgeir Moe, Christian Hansen: data acquisition and analyses, review of the manuscript; Andreas H. Kristensen: concept and design, data analyses, drafting the manuscript; Jan T. Mannsverk: concept and design, data acquisition and analyses, statistical calculations, drafting the manuscript.
Disclosures
Kristian Bartnes, Hilde Albrigtsen, Johanne M. Iversen, Henrik Brovold, Niels H. Møller, Bjørn Wembstad, Frode Arstad, Andreas H. Kristensen, Julia Cortis, Siv J. Olsen, Ståle N. S. Nygaard, Sven G. Kindler, Oddgeir Moe, Christian Hansen, and Jan T. Mannsverk have nothing to disclose.
Compliance with Ethics Guidelines
The regional board of medical ethics considered that approval of the study protocol by the board was not required.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bartnes, K., Albrigtsen, H., Iversen, J.M. et al. The Barriers to Rapid Reperfusion in Acute ST-Elevation Myocardial Infarction. Cardiol Ther 11, 559–574 (2022). https://doi.org/10.1007/s40119-022-00281-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-022-00281-7