Abstract
Introduction
The purpose of this meta-analysis is to compare the efficacy of MitraClip plus medical therapy versus medical therapy alone in patients with functional mitral regurgitation (FMR). FMR caused by left ventricular dysfunction is associated with poor prognosis. Whether MitraClip improves clinical outcomes in this patient population remains controversial.
Methods
We conducted an electronic database search of PubMed, CINAHL, Cochrane Central, Scopus, Google Scholar, and Web of Science databases for randomized control trials (RCTs) and observational studies with propensity score matching (PSM) that compared MitraClip plus medical therapy with medical therapy alone for patients with FMR and reported on subsequent mortality, heart failure re-hospitalization, and other outcomes of interest. Event rates were compared using a random-effects model with odds ratio as the effect size.
Results
Five studies (n = 1513; MitraClip = 796, medical therapy = 717) were included in the final analysis. MitraClip plus medical therapy compared to medical therapy alone was associated with a significant reduction in overall mortality (OR = 0.66, 95% CI = 0.44–0.99, P = 0.04) and heart failure (HF) re-hospitalization rates (OR = 0.57, 95% CI = 0.36–0.91, P = 0.02). There was reduced need for heart transplantation or mechanical support requirement (OR = 0.48, 95% CI = 0.25–0.91, P = 0.02) and unplanned mitral valve surgery (OR = 0.21, 95% CI = 0.07–0.61, P = 0.004) in the MitraClip group. No effect was observed on cardiac mortality (P = 0.42) between the two groups.
Conclusions
MitraClip plus medical therapy improves overall mortality and reduces HF re-hospitalization rates compared to medical therapy alone in patients with FMR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Functional mitral regurgitation caused by left ventricular dysfunction is associated with significant morbidity and mortality. |
Whether MitraClip improves clinical outcomes in this patient population remains controversial. |
We conducted a meta-analysis of all published studies to compare the efficacy of MitraClip plus medical therapy versus medical therapy alone in patients with functional mitral regurgitation. |
Based on our pooled analysis, we found that MitraClip plus medical therapy compared to medical therapy alone was associated with a significant reduction in overall mortality and heart failure re-hospitalization rates. |
There was reduced need for heart transplantation or mechanical support requirement and unplanned mitral valve surgery in the MitraClip group. |
Introduction
Functional mitral regurgitation (FMR) is defined as mitral insufficiency secondary to inadequate leaflet movement due to either left ventricular (LV) wall motion abnormalities or to ventricular and mitral annulus dilatation [1]. In FMR, the mitral valve itself is normal but LV abnormalities cause tenting of the valve, thereby preventing its closure. It is associated with poor clinical outcomes, increased cardiovascular mortality, and frequent re-hospitalizations [2]. Studies have shown that patients with FMR receiving medical therapy alone have grim prognoses and have a mortality rate as high as 50% at 5 years [3]. Although considered curative for primary mitral regurgitation, surgical approaches used for correction of FMR have not been successful as measured by rates of mortality and heart failure re-hospitalizations [4] and is frequently prohibitive given depressed ejection fraction, advanced age, high operative risk, and other comorbidities [5]. Percutaneous mitral valve repair using MitraClip (Abbott Vascular, Santa Clara, CA, USA) offers an innovative solution for this subgroup of patients. The MitraClip creates a double orifice by bringing together the free edges of the anterior and posterior leaflets. It has gained widespread popularity as an effective way to treat patients with severe mitral regurgitation who are at high risk for surgery [6, 7]. In the randomized Endovascular Valve Edge-to-Edge Repair Study (EVEREST) II trial [7], trans-catheter mitral-leaflet approximation with the MitraClip device was found to have similar clinical outcomes, significant reduction in re-hospitalization, and improved symptom control compared to surgical mitral-valve repair for patients with primary mitral regurgitation. In contrast, the data for patients with FMR is conflicting with the Mitra-FR trial [8] reporting no advantage of MitraClip and the recently published COAPT trial [9] showing significant clinical, as well as, mortality benefits.
Therefore, we performed a meta-analysis of all published randomized control trials (RCTs) and observational studies with propensity score matching (PSM) to compare the efficacy of MitraClip plus medical therapy versus medical therapy alone in patients with FMR.
Methods
Study Design
A systematic review of the literature was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [10].
Data Sources and Search Strategy
We systematically searched PubMed, CINAHL, Cochrane Central, Scopus, Google Scholar, and Web of Science databases for all studies that compared MitraClip plus medical therapy with medical therapy alone. All relevant combinations of the following keywords related to MitraClip and FMR were searched: “MitraClip”, “Functional mitral regurgitation”, “Secondary mitral regurgitation,” and “Medical Therapy”. The search was conducted from the inception of these databases to October 30, 2018. No language or age restrictions were applied. Pertinent trials were also searched in http://www.clinicaltrials.gov, and in the proceedings of major international cardiology meetings (American College of Cardiology, American Heart Association, European Society of Cardiology, and Transcatheter Cardiovascular Therapeutics). We also manually searched the references of these articles to find additional articles. Two independent reviewers SG and RT conducted the search.
Study Selection
Studies were included in the meta-analysis if they met the following criteria: (1) a study on human subjects with participants of any age undergoing MitraClip implantation for FMR and, (2) studies comparing the outcomes between MitraClip plus medical therapy versus medical therapy alone. The exclusion criteria included single case reports, reviews, editorials, and studies comparing MitraClip to surgical valve replacement or repair.
The studies included were either RCTs or observational studies, which used PSM to create groups with similar baseline characteristics.
Data Extraction
Two independent reviewers (SG, RPT) screened the titles and abstracts for relevance. Discrepancies between reviewers were discussed until consensus was reached. The manuscripts of selected titles and abstracts were reviewed for inclusion and authors were contacted if additional data was needed. Using the above-mentioned selection criteria, the two reviewers independently determined which articles were to be included and excluded, and the data from the relevant articles were extracted using predefined extraction forms. Any disagreements in data extraction were discussed until consensus was reached. Bibliographies of relevant publications were hand-searched to attempt complete inclusion of all possible studies of interest.
Study End-Points
The primary end-points were overall mortality and HF re-hospitalizations. The secondary end-points were cardiovascular mortality, heart transplantation, or mechanical circulatory support requirement and unplanned mitral valve surgery. All events that occurred during follow-up were analyzed using an intention to-treat principle.
Data Analysis
To analyze the data, the authors used Review Manager Software (RevMan, version 5.3). A random-effects model was used to calculate the pooled mean difference between the MitraClip plus medical therapy and the medical therapy arm. Random-effects model was used for our analysis. Heterogeneity between studies was assessed using Cochran’s Q test and I2 statistics, which denotes the percentage of total variation across studies that is a result of heterogeneity rather than chance. Heterogeneity was considered significant if the P value was < 0.05. Heterogeneity was classified as moderate if the I2 statistic was 30–60%, substantial if 50–90%, and considerable if 75–100%. Pooled mean difference and odds ratio were the effect sizes used for continuous and categorical variables, respectively; 95% confidence intervals were calculated and the level of significance was set to a P value of 0.05. Publication bias was assessed by visual interpretation of funnel plots. Sensitivity analysis was performed wherever appropriate by including either only RCTs or only propensity score matched studies. Risk of bias assessment was evaluated using ROBINS-I tool for propensity score matched studies, and RevMan software for RCTs [11].
Ethics Compliance
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Results
Studies Included
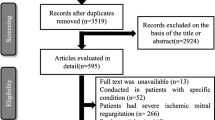
A total of five studies were included in the final analysis [8, 9, 12,13,14] (Table 1 shows salient features of the studies). Figure 1 shows the PRISMA flow diagram describing the search strategy. The initial search yielded 3836 abstracts of which 3743 were excluded based on title and abstract. Ninety-three articles were reviewed with their full text. Five articles met the inclusion criteria, two RCTs and three PSM observational studies (total number of patients = 1513; MitraClip = 796 and medical therapy = 717).
Baseline Characteristics
The mean age of patients was 71.6 ± 10.6 years in the MitraClip group and 72.0 ± 10.8 years in the medical therapy alone group; 71.7% of the MitraClip patients and 67.2% of the medical therapy patients were males. A history of diabetes mellitus was present in 32.8% of the MitraClip patients and 33.1% of the medical therapy patients. Hypertension was prevalent in 78.0% and 67.4% of the MitraClip and medical therapy groups, respectively; 43.8% of the MitraClip patients and 44.2% of the medical therapy patients had a history of atrial fibrillation or atrial flutter; 30.4% and 26.8% of the MitraClip and medical therapy patients, respectively, received cardiac resynchronization therapy. A past history of at least one episode of myocardial infarction was noted in 45.9 and 48.0% of the MitraClip and medical therapy groups, respectively (Table 1).
Primary Outcomes
Overall Mortality
All but one study reported overall mortality with a mean follow-up of 12–24 months and a total of 1393 patients were included for this analysis [8, 9, 12, 13]. The overall mortality rate was 19.8% in the MitraClip arm, as compared to 29.2% in the medical therapy alone group, with an odds ratio of 0.66 (95% CI 0.44–0.99, P = 0.04, I2 = 52%) (Fig. 2a).
HF Re-Hospitalization
The HF re-hospitalization rate was reported in four studies with a total of 1130 patients [8, 9, 13, 14]. One of the studies did not provide the number of re-hospitalization events but did provide a log odds ratio, which was included for the final analysis [13]. In our pooled analysis, the odds ratio for rate of re-hospitalization for HF was found to be 0.57 (95% CI 0.36–0.91, P = 0.02, I2 = 85%) favoring the MitraClip group (Fig. 2b).
Secondary Outcomes
Cardiovascular Mortality
Cardiovascular mortality was reported by three studies with a total of 1010 patients [8, 9, 13]. The rate of cardiac deaths was 20% in the MitraClip group, which was numerically lower than the 29.6% reported in medical therapy alone group. However, the difference was not statistically significant (OR 0.55, 95% CI 0.26–1.13, P = 0.10, I2 = 80%) (Fig. 3a).
a Forest plot showing cardiovascular mortality comparing MitraClip plus medical therapy versus medical therapy alone. b Forest plot showing heart transplantation or mechanical circulatory support requirement comparing MitraClip plus medical therapy versus medical therapy alone. c Forest plot showing unplanned mitral valve surgery comparing MitraClip plus medical therapy versus medical therapy alone
Heart Transplantation or Mechanical Circulatory Support Requirement
Heart transplant or mechanical circulatory support use was reported in two studies with a total of 918 patients. A significantly lower number of patients required heart transplantation or mechanical circulatory support in the MitraClip group compared to medical therapy group [8, 9] (OR: 0.48, 95% CI 0.25–0.91, P = 0.02, I2 = 0%) (Fig. 3b).
Unplanned Mitral Valve Surgery
Unplanned mitral valve surgeries were reported in three studies with a total of 1010 patients. Unplanned mitral valve surgeries were performed in significantly more number of patients receiving medical therapy as compared to those who had MitraClip placed [8, 9, 13] (OR 0.21, 95% CI 0.07–0.61, P = 0.004, I2 = 0%) (Fig. 3c).
Publication Bias Assessment, Sensitivity Analysis, and Risk of Bias Assessment
Based on visual interpretation of the funnel plots there was no significant publication bias for the primary and secondary endpoints [Supplementary figure 1]. Unlike the results of the pooled analysis, sensitivity analysis for overall mortality with RCTs [8, 9] did not show any significant differences between the two groups [Supplementary figure 2A]. However, the analysis with propensity score matched studies [12, 13] did show significant mortality benefit with MitraClip versus medical therapy alone [Supplementary figure 2B]. While there was a significant reduction in re-hospitalization due to heart failure in the initial analysis, there were no significant differences between the groups in the sensitivity analyses with both RCTs [8, 9] [Supplementary figure 2C] and propensity score matched studies [13, 14] [Supplementary figure 2D]. Analysis of cardiac mortality with only RCTs [8, 9] did not show any significant differences between the two groups, which is similar to the initial analysis [Supplementary figures 2E]. Proportion of patients undergoing unplanned mitral valve surgery were significantly lower in the MitraClip group in the sensitivity analysis of propensity score matched studies [13, 14], which is similar to the result of initial analysis [Supplementary figure 2F]. The risks of bias assessments for these outcomes are included in the same forest plots [Supplementary figure 2].
The risks of bias assessments for the sensitivity analyses using propensity score matching are included in the supplementary material.
Discussion
The findings from our meta-analysis can be summarized as follows:
-
1.
MitraClip plus medical therapy compared to medical therapy alone is associated with a significant reduction in overall mortality and reduced rates of re-hospitalization for HF;
-
2.
There is reduced need for heart transplantation or mechanical circulatory support and unplanned mitral valve surgery in the MitraClip group; and,
-
3.
There is no significant difference in cardiac mortality between the two groups.
To our knowledge this is the first meta-analysis comparing MitraClip along with medical therapy versus medical therapy alone selectively in FMR patients only. Previous meta-analyses performed on the same topic have included either observational studies or included patients with degenerative mitral regurgitation (DMR) in their analysis [15, 16]. Given the pathophysiology of DMR patients is fundamentally distinct from that of FMR patients, the inclusion of DMR patients along with FMR patients in these meta-analyses may potentially act as a confounding factor and may, therefore, skew the overall results in either direction.
We believe that the positive results on mortality, reduced HF re-hospitalization rates, and reduced rates of heart transplant or mitral valve surgeries among patients who received MitraClip treatment in our analysis, are secondary to the reduction in the severity of secondary mitral regurgitation seen with the use of MitraClip. The presence of even mild degrees of functional MR in patients with left ventricular dysfunction carries high mortality risk than those without MR [17]. MitraClip use may reverse cardiac remodeling, thus leading to significant improvement in functional class even in highly symptomatic patients with severely dilated hearts [18]. The results of decreased mortality with Mitraclip should be interpreted with caution given the fact that we included propensity score matched studies in our analysis. We included PSM studies in our analysis because of the paucity of randomized data on this subject and given that inclusion of purely observational data would have created an enormous bias given the unequal distribution of confounding variables. With the use of propensity matched model, authors and statisticians can use observational data to control for treatment selection bias. Propensity score is estimated using logistic regression model for each subject and these subjects are matched based on their scores to control confounding. With this kind of purely statistical analysis, there is always a chance that an important variable might have been missed out during propensity regression which may lead to over or underestimation of treatment effect [19].
The contrasting results from the two major randomized trials, Mitra-FR [8] and COAPT [9], included in our analysis could be explained by the following facts:
-
1.
The patient populations in these two trials varied significantly due to differences in how the European Society of Cardiology (ESC) and European Association for Cardio-Thoracic Surgery (EACTS), versus the American College of Cardiology (ACC), and American Heart Association (AHA) define severe FMR (Effective Regurgitation Orifice Area [EROA] > 20 mm2 and Regurgitation Volume [RV] > 30 ml/beat as per ESC/EACTS guidelines [20] and EROA > 30 mm2 and RV > 45 ml/beat as per ACC/AHA guidelines [21]). As such, patients in the COAPT trial who received MitraClip had more severe MR (EROA of 41 mm2) at time of MitraClip implantation as compared to Mitra-FR (EROA of 31 mm2) and, therefore, could have derived more benefit [2];
-
2.
Patients in the COAPT trial were already on optimal medical therapy pre-trial with only minute changes to medical therapy during follow–up, while those in the Mitra-FR were not medically optimized at baseline and had variable adjustments during follow-up period. This may have masked the overall benefit derived from MitraClip [3];
-
3.
The success rate of MitraClip placement and acute reduction of 2 + MR was higher in the COAPT trial (95% versus 91.9% in Mitra-FR trial); and,
-
4.
The reduction of MR to a grade of 2 + or less sustained at 12 months was much higher in the COAPT trial as compared to Mitra-FR group which may have contributed to persistent clinical and mortality benefit.
-
5.
It is also important to understand the secondary or functional MR can be explained either because of distortion if mitral valve function secondary to left ventricular enlargement or those in whom the disease process disproportionately affects the segment of left ventricle responsible for mitral valve cooptation. The first group of patients are considered to have proportionate MR and clinically not severe and thus any intervention the valve might not have any implication on the disease process. It appears that patients included in the COAPT trial had disproportionate MR as is proposed by Grayburn et al. which likely explains the significant difference in the results of the two trials. [22].
The above-mentioned differences between the patients groups of COAPT and MITRA-FR trials could have led to moderate to high heterogeneity seen in our analysis and therefore, the results of our analysis should be interpreted with caution. Although observational studies in the past have shown a positive effect of MitraClip in FMR patients [12,13,14, 23], the first major RCT, Mitra-FR [8] yielded disappointing results. However, the COAPT trial [9] surprisingly showed a robust decrease in overall mortality, re-hospitalizations due to heart failure, and cardiac death. The baseline echocardiographic parameters indicate that the patients included in the COAPT study did not have significant dilation of left ventricle (LVEDV of 101 ml/m2 versus 135 ml/m2 in Mitra-FR), which would indicate that these patients did not have severe remodeling of their LV at the time of enrollment. Moreover, all patients in the COAPT trial were being optimally managed on medical therapy and were followed very closely which is certainly variable in real world populations. This shows that patients without advanced remodeling of LV and who are on optimal medical therapy might be better candidates for MitraClip. Real-world experience with MitraClip may help us better assess the benefits of MitraClip in FMR patients. Lastly, the results of RESHAPE HF 2 trial (NCT02444338) may swing the pendulum in either direction.
There are several limitations to our study:
-
1.
The analysis is based on pooled data from different studies and it shares the possible limitations of the included studies. Furthermore, we were unable to perform any subgroup or survival analysis as we did not have the patient level data;
-
2.
Inclusion of observational studies along with randomized controlled trials in our meta-analysis is a major limitation which could have led to the heterogeneity in the analysis; however, this was a direct result of the scarcity of data on this topic and we did perform appropriate statistical analysis to evaluate sources of bias and heterogeneity;
-
3.
For the observational studies, it was not clear whether the patients in MitraClip group were on optimal medical therapy at baseline or at follow-up and whether the medical therapy between the two groups were similar. We included these studies due to paucity of data;
-
4.
Although, our pooled analysis shows mortality and heart failure re-hospitalization benefits with use of MitraClip, there was moderate heterogeneity between the studies evaluating the mortality outcomes and substantial heterogeneity between studies reporting the heart failure re-hospitalization outcomes. When we performed a sensitivity analysis, the positive effect of MitraClip was not evident for mortality in RCT’s and for HF re-hospitalization in both RCT and PSM studies; and,
-
5.
We were not able to perform a risk of bias analysis as the study designs were different in these studies and there is no single scale that would assess risk of bias in both RCTs and PSM studies.
Conclusions
Based on our meta-analysis, it can be concluded that MitraClip plus medical therapy compared to medical therapy alone improves overall mortality and reduces HF re-hospitalization rates for patients with FMR. As well, there is reduced need for heart transplantation or mechanical circulatory support and unplanned mitral valve surgery in the MitraClip group. However, there is no difference in cardiac mortality between the two groups.
References
De Marchena E, Badiye A, Robalino G, et al. Respective prevalence of the different Carpentier classes of mitral regurgitation: a stepping stone for future therapeutic research and development. J Card Surg. 2011;26:385e92.
Sannino A, Smith RL II, Schiattarella GG, Trimarco B, Esposito G, Grayburn PA. Survival and cardiovascular outcomes of patients with secondary mitral regurgitation: a systematic review and meta-analysis. JAMA Cardiol. 2017;2:1130–9.
Goel S, Bajaj N, Aggarwal B, et al. Prevalence and outcomes of unoperated patients with severe symptomatic mitral regurgitation and heart failure. J Am Coll Cardiol. 2014;63(2):185–6.
DiSalvo TG, Acker MA, Dec GW, Byrne JG. Mitral valve surgery in advanced heart failure. J Am Coll Cardiol. 2010;55:272e82.
Mirabel M, Lung B, Baron G, et al. What are the characteristics of patients with severe, symptomatic, mitral regurgitation who are denied surgery? Eur Heart J. 2007;28:1358–65.
Mack MJ. New techniques for percutaneous repair of the mitral valve. Heart Fail Rev. 2006;11:259e68.
Feldman T, Foster E, Glower DD, et al. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med. 2011;364:1395e406.
Obadia JF, Messika-Zeitoun D, Leurent G, et al. Percutaneous repair or medical treatment for secondary mitral regurgitation. N Engl J Med. 2018. https://doi.org/10.1056/NEJMoa1805374.
Stone GW, Lindenfeld J, Abraham WT, Kar S, Lim DS. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 2018. https://doi.org/10.1056/NEJMoa1806640.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65–9.
https://sites.google.com/site/riskofbiastool/welcome/home/current-version-of-robins-i/robins-i-tool-2016. Last Accessed 4 Aug 2019.
Armeni P, Boscolo PR, Tarricone R, et al. Real-world cost effectiveness of MitraClip combined with medical therapy versus medical therapy alone in patients with moderate or severe mitral regurgitation. Int J Cardiol. 2016;209:153–60.
Asgar AW, Khairy P, Guertin MC, et al. Clinical outcomes and economic impact of transcatheter mitral leaflet repair in heart failure patients. J Med Econ. 2017;20:82–90.
Giannini C, Fiorelli F, De Carlo M, et al. Comparison of percutaneous mitral valve repair versus conservative treatment in severe functional mitral regurgitation. Am J Cardiol. 2016;117:271–7.
Giannini C, D’ascenzo F, Fiorelli F, et al. A meta-analysis of MitraClip combined with medical therapy vs. medical therapy alone for treatment of mitral regurgitation in heart failure patients. ESC Heart Fail. 2018;5(6):1150–8.
Marmagkiolis K, Hakeem A, Ebersole DG, Iliescu C, Ates I, Cilingiroglu M. Clinical outcomes of percutaneous mitral valve repair with MitraClip for the management of functional mitral regurgitation. Catheter Cardiovasc Interv. 2019. https://doi.org/10.1002/ccd.28203.
Enriquez-Sarano M, Akins CW, Vahanian A. Mitral regurgitation. Lancet. 2009;373(1382):1394.
Franzen O, van der Heyden J, Baldus S, et al. MitraClip® therapy in patients with end-stage systolic heart failure. Eur J Heart Fail. 2011;13:569–76.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424.
Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017;38:2739–91.
Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(25):e1159–95.
Grayburn PA, Sannino A, Packer M. Proportionate and disproportionate functional mitral regurgitation: a new conceptual framework that reconciles the results of the MITRA-FR and COAPT trials. JACC Cardiovasc Imaging. 2019;12(2):353–62.
Swaans MJ, Bakker AL, Alipour A, et al. Survival of transcatheter mitral valve repair compared with surgical and conservative treatment in high surgical risk patients. JACC Cardiovasc Interv. 2014;7:875–88.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Sunny Goel, Ravi Teja Pasam, Karan Wats, Srilekha Chava, Joseph Gotesman, Abhishek Sharma, Bilal Ahmad Malik, Sergey Ayzenberg, Robert Frankel, Jacob Shani and Umesh Gidwani have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced digital features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.10265168.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any non-commercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Goel, S., Pasam, R.T., Wats, K. et al. Mitraclip Plus Medical Therapy Versus Medical Therapy Alone for Functional Mitral Regurgitation: A Meta-Analysis. Cardiol Ther 9, 5–17 (2020). https://doi.org/10.1007/s40119-019-00157-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-019-00157-3