Abstract
Introduction
Hemodynamic measurements can assess for paravalvular aortic regurgitation after transcatheter aortic valve replacement (TAVR). This study compared the utility of different invasive hemodynamic measures in providing prognostic information.
Methods
This retrospective observational study of TAVR patients at a Veterans Hospital assessed aortic regurgitation index, diastolic delta, pulse pressure, and heart rate adjusted diastolic delta obtained at valve implantation. The primary outcome was total mortality.
Results
Overall, 151 patients underwent TAVR. Immediately after implantation, mean aortic regurgitation index was 31 ± 8.6, mean diastolic delta was 38 ± 9.8 mmHg, mean pulse pressure was 67 ± 18 mmHg, and mean heart rate adjusted diastolic delta was 47 ± 14.3 mmHg/beats per minute. Two percent of patients had ≥ moderate paravalvular aortic regurgitation by postoperative transthoracic echocardiography. Total mortality was 15.2% at a mean follow-up of 12.7 ± 9.2 months. Aortic regurgitation index <25 vs. ≥25, diastolic delta <19 vs. ≥19 mmHg, and pulse pressure >60 vs. ≤60 mmHg were not associated with total mortality. However, total mortality was 50% for heart rate adjusted diastolic delta <25 mmHg/beats per minute vs. 12.6% for heart rate adjusted diastolic delta ≥25 mmHg/beats per minute (p = 0.017). In a multivariate Cox regression analysis, heart rate adjusted diastolic delta <25 mmHg/beats per minute vs. heart rate adjusted diastolic delta ≥25 mmHg/beats per minute was associated with total mortality (hazard ratio 9.4, 95% confidence interval 2.0–44, p = 0.004).
Conclusions
Among a cohort of TAVR patients, the only invasive hemodynamic test independently associated with total mortality was heart rate adjusted diastolic delta.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Paravalvular aortic regurgitation is an important complication after transcatheter aortic valve replacement (TAVR). Moderate to severe paravalvular aortic regurgitation has been clearly associated with late mortality; however, this can be a challenging diagnosis [1,2,3]. Various invasive hemodynamics tests have been developed to complement aortography and echocardiography in the assessment of this complication. In two cohorts of patients who received the CoreValve device (n = 146) or the CoreValve/Sapien device (n = 122), the incidence of moderate to severe paravalvular aortic regurgitation was ≥15% [4, 5]. The investigators calculated the difference between the aortic diastolic pressure and left ventricular end-diastolic pressure (LVEDP) in relation to the aortic systolic pressure (aortic regurgitation index). They found a stepwise decrease in the aortic regurgitation index as the severity of paravalvular aortic regurgitation worsened. Aortic regurgitation index <25 was associated with increased 1-year mortality. Other invasive tests, such as the diastolic delta and the heart rate adjusted diastolic delta, have reached similar conclusions about impaired hemodynamics and late mortality [6, 7].
With current generation devices, the incidence of significant paravalvular aortic regurgitation is quite low. In our own practice, we observed that in some patients the aortic regurgitation index can be low despite no evidence of significant paravalvular aortic regurgitation. Moreover, no study has compared these different hemodynamic tests within the same cohort of patients. Accordingly, a reappraisal of the utility of these tests in predicting late mortality and their comparison against each other is warranted.
Methods
This study was approved by the Institutional Review Board at the University of Florida. This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors. All procedures were performed at the Malcom Randall Veterans Hospital for symptomatic severe aortic stenosis or mixed aortic stenosis/aortic regurgitation. Patients with either native or bioprosthetic aortic valve disease were included. Patients were evaluated in a multidisciplinary fashion by a Cardiologist and a Cardiothoracic Surgeon and considered appropriate for TAVR if they were deemed at least intermediate-risk (or high-risk/inoperable earlier in the program) for open-heart surgery. All patients had the following preoperative tests performed: transthoracic echocardiography, cardiac catheterization ± valve study, and TAVR-protocol computed tomography. Select intra-operative testing included transesophageal echocardiography, aortography, and valve study. The valve study was performed with a dual lumen pigtail catheter with simultaneous left ventricular and aortic pressures recorded before and approximately 5–10 min after valve implant. Postoperative transthoracic echocardiography was obtained on all patients.
Aortic regurgitation index was defined as 100 × [(aortic diastolic blood pressure—LVEDP)/systolic blood pressure] [4]. Diastolic delta was defined as the aortic diastolic blood pressure minus LVEDP [6]. Heart rate adjusted diastolic delta was defined as 80 × [(aortic diastolic blood pressure—LVEDP)/heart rate] [7]. Pulse pressure was defined as aortic systolic blood pressure minus aortic diastolic blood pressure [8]. Echocardiographic quantification of aortic regurgitation after TAVR was performed according to the Valve Academic Research Consortium (VARC-2) definitions [9], and Sellers classification was used to grade aortic regurgitation on aortic root angiogram semi-quantitatively by visual assessment [10].
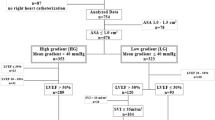
Patients were classified into stages of aortic stenosis as per American College of Cardiology/American Heart Association valvular guidelines [11]. Stage D1 was defined as high-gradient aortic stenosis (mean aortic gradient ≥40 mm Hg). Stage D2 was defined as low-gradient low-ejection fraction aortic stenosis [mean aortic gradient <40 mm Hg and left ventricular ejection fraction (LVEF) <50%]. Stage D3 was defined as low-gradient normal-ejection fraction aortic stenosis (mean aortic gradient <40 mm Hg and LVEF ≥ 50%). The mean aortic gradient was preferentially obtained from the intraoperative valve study. If this was not performed, the preoperative valve study was recorded instead. If neither invasive study was performed, the preoperative transthoracic echocardiography derived value was obtained. The stroke volume index (SVi) was preferentially obtained from the preoperative invasive valve study. Thermodilution derived cardiac output was preferentially obtained; however, fick derived cardiac output was used if that was the only technique performed during right heart catheterization. If a preoperative valve study was not performed, the pre-operative transthoracic echocardiography derived SVi value was obtained instead.
Statistical Analysis
Among the entire cohort, Cox Regression analysis examined univariate hemodynamic predictors for total mortality with cutoffs based on previous studies: aortic regurgitation index <25 [4, 5], diastolic delta <19 mm Hg [6], pulse pressure >60 mm Hg [8], and heart rate adjusted diastolic delta <25 mm Hg/beats per minute [7]. Other potential predictors included age, body mass index, diabetes, prior coronary revascularization, prior stroke/transient ischemic attack, chronic obstructive pulmonary disease/obstructive sleep apnea, pulmonary hypertension, atrial fibrillation, serum creatinine, LVEF, aortic valve mean gradient, SVi, general anesthesia, transapical access, new left bundle block, and paravalvular aortic regurgitation. Receiver operator curve was used to determine the cut point that provided the best discrimination for continuous variables. Univariate predictors that were conservatively significant (p < 0.1) were entered into a multivariate model with significance set at p < 0.05. Results are presented as hazard ratios (HR) and 95% confidence interval (CI) with p value <0.05 considered statistically significant. Descriptive data are presented as mean ± standard deviation, or median and interquartile range if non-normal distribution. Categorical variables are presented as frequencies and percentages. Continuous variables were compared with the Student t test and categorical variables with the Chi square or Fisher exact test if needed. All statistics were carried out with SPSS software (Version 22, IBM Co., Armonk, NY, USA).
Results
Between September 2013 and November 2016, 155 transcatheter heart valve procedures were performed. Three of these were transcatheter mitral valve or mitral ring procedures and were excluded from further analysis. Another patient who had a Sapien XT implanted subsequently developed severe late paravalvular aortic regurgitation, presumably due to late recoil [12]. This was managed with a Sapien S3 valve-in-valve procedure approximately 1 year later. As this second procedure was not for treatment of aortic stenosis, it was excluded from further analysis.
The baseline characteristics of the study cohort (n = 151) are presented in Table 1. Stage D1 aortic stenosis was present in 52.3% of patients; mean gradient = 50.3 ± 10.7 mm Hg, LVEF = 53.7 ± 8.8%, and SVi = 37.1 ± 8.4 cc/m2. Stage D2 aortic stenosis was present in 14.6% of patients; mean gradient = 28.8 ± 6.8 mm Hg, LVEF = 35.9 ± 8.8%, and SVi = 28.7 ± 6.3 cc/m2. Stage D3 aortic stenosis was present in 33.1% of patients; mean gradient = 31.3 ± 5.8 mm Hg, LVEF = 56.0 ± 3.8%, and SVi = 37.8 ± 8.8 cc/m2.
Procedural characteristics are presented in Table 2. Conscious sedation was used in 20%, and the most frequently implanted valve was the Sapien S3. Early outcomes are presented in Table 2. Early deaths were infrequent (30-day mortality = 2%). Only 2% of patients had moderate or greater paravalvular aortic regurgitation as assessed by postoperative transthoracic echocardiography.
Overall mortality was 15.2% at a mean follow-up of 12.7 ± 9.2 months. Aortic regurgitation index <25 versus ≥25, diastolic delta <19 mm Hg versus ≥19 mm Hg, and pulse pressure >60 mm Hg versus ≤60 mm Hg were not associated with total mortality. However, total mortality was 50% for heart rate adjusted diastolic delta <25 mm Hg/beats per minute versus 12.6% for heart rate adjusted diastolic delta ≥25 mm Hg/beats per minute (p = 0.017). In a multivariate Cox regression analysis, heart rate adjusted diastolic delta <25 mm Hg/beats per minute versus heart rate adjusted diastolic delta ≥25 mm Hg/beats per minute was associated with late mortality (HR 9.4, 95% CI 2.0–44, p = 0.004) (Table 3). Salient characteristics of the patients with heart rate adjusted diastolic delta <25 mm Hg/beats per minute are presented in Table 4.
Discussion
Among a cohort of TAVR patients with low incidence of significant paravalvular aortic regurgitation, we observed that a low heart rate adjusted diastolic delta was independently associated with increased total mortality compared with a high heart rate adjusted diastolic delta. Aortic regurgitation index, diastolic delta, and pulse pressure were not associated with increased total mortality. Thirty day (2%) and 1-year mortality (15.2%) was low in this cohort of veterans from a single center experience.
As heart rate increases, diastole shortens resulting in higher aortic diastolic pressure and LVEDP. This may help to explain the superiority of the heart rate adjusted diastolic delta as an invasive hemodynamic test in capturing the complex interplay of heart rate and blood pressure. In the absence of significant aortic regurgitation, a low heart rate adjusted diastolic delta may reflect central aorta stiffness and/or an increase in LVEDP from diastolic dysfunction. Increased pulse pressure is a marker for central aorta stiffness. In an observational study of 22,576 patients with hypertension and coronary artery disease, increased pulse pressure was independently associated with increased all-cause mortality (nadir pulse pressure 60 mm Hg) [8]. The reference standard for non-invasively assessing central aorta stiffness is the aortic pulse wave velocity [13]. Increased pulse wave velocity has been independently associated with increased mortality among hypertensive patients with normal pulse pressure (mean pulse pressure 59 mm Hg) [14]. Pulse wave velocity may be an important risk factor among those without established atherosclerotic disease, while the pulse pressure becomes important later in the disease process [15]. Interestingly, TAVR may be superior to surgical aortic valve replacement in preserving aortic elasticity [16]. This could possibly be related to TAVR not resulting in mediastinal scar formation or inflammatory changes within the aorta [16]. At the present time, central aorta stiffness has not been viewed as an important prognostic factor among patients with valvular heart disease. How this condition is best diagnosed and treated are important future questions. For example, these patients may require different heart rate and/or blood pressure targets; however, these concepts would need to be prospectively evaluated.
Early procedural complications are captured with 30-day mortality, while the patient’s overall medical condition and frailty are better reflected in 1-year mortality [17, 18]. From the Society of Thoracic Surgeons/American College of Cardiology/Transcatheter Valve Therapies registry (STS/ACC/TVT), procedural success was documented at 92%, 30-day mortality, 4.6%–7.0%, and 1-year mortality, 21.6%–23.7% [19,20,21]. Despite excellent acute procedural success and low early mortality, late mortality remains quite high nationally. Therefore, ongoing attempts to understand and improve long-term survival are important.
In addition to heart rate adjusted diastolic delta, other independent predictors of total mortality included severe pulmonary hypertension (mean ≥ 45 mm Hg), low SVi (<24 cc/m2), and moderate or greater paravalvular aortic regurgitation. The current incidence of significant paravalvular aortic regurgitation is quite low (<5%–6% incidence of moderate to severe paravalvular aortic regurgitation with the Sapien S3 and Evolut R devices) [21,22,23]. In addition to device improvements, optimal valve implantation by avoiding implants within significant calcification in the left ventricular outflow tract may also be a contributing factor. As the incidence of significant paravalvular aortic regurgitation continues to decline, other patient characteristics will become more important in predicting late mortality. In fact, moderate to severe paravalvular aortic regurgitation was marginally significant in this dataset, which is likely a reflection of limited events for this outcome.
Previous studies have documented low echocardiography-derived SVi (<35 cc/m2) as a significant independent predictor of late mortality [24, 25]. By using receiver operator curve analysis, we determined that <24 cc/m2 provided the best prediction of late mortality. This variable carried the strongest hazard ratio for late mortality among our four retained variables. Low flow predominately affects stage D2 aortic stenosis patients. In such patients, careful determination of the stroke volume through cardiac catheterization may be preferential to echocardiography derived valves. In patients with markedly reduced stroke volume, consideration could be given to optimization of flow before proceeding with TAVR. Examples could include multi-vessel coronary revascularization, restoration of sinus rhythm, cardiac resynchronization therapy, and control of systemic and/or pulmonary hypertension. We preferentially obtained the SVi from the pre-operative valve study, which may help to explain the different cut point from previous studies. Resting pulmonary hypertension has been reported in up to one third of patients with symptomatic aortic stenosis; however, this is usually mild in severity (23% with mild, 8.9% with moderate, and 4.8% with severe pulmonary hypertension) [26]. Severe pulmonary hypertension has been associated with late mortality after TAVR [27, 28]. However, some data suggest a gender effect that places women at disproportionate risk from pulmonary hypertension [29]. Our analysis, in 98% men, suggests that severe pulmonary hypertension may be equally hazardous in men.
Limitations
Although this is a relatively small dataset, it allows for more detailed variables that are not available in the larger STS/ACC/TVT registry [19]. For example, this allowed us to evaluate the prognostic performance of SVi (predominately derived from catheterization) and heart rate adjusted diastolic delta, which is difficult to obtain on a large scale. SVi was considered from multiple sources, although we preferentially utilized values in the following order (derived from thermodilution cardiac output > derived from fick cardiac output > derived from echocardiogram). This could have decreased the precision of this measurement. Although low heart rate adjusted diastolic delta was retained in the multivariate Cox regression analysis, this predictor was only present in eight patients. Moreover, these hemodynamic indices were obtained in patients who underwent general anesthesia and conscious sedation, which could have resulted in measurement variability. It is possible that the prognostic significance of a low heart rate adjusted diastolic delta was related to unrecognized aortic regurgitation. However, from multiple imaging studies, there was no sign of moderate to severe aortic regurgitation in these patients. Cardiac magnetic resonance imaging might be helpful in selecting patients to evaluate for occult aortic regurgitation [30]. This study applies almost exclusively to men; therefore, any conclusions among women must be cautious.
Conclusion
Among a cohort of veterans with low incidence of paravalvular aortic regurgitation, we documented four variables that predicted late mortality: heart rate adjusted diastolic delta <25 mm Hg/beats per minute, SVi < 24 cc/m2, mean pulmonary pressure ≥45 mm Hg, and moderate to severe paravalvular aortic regurgitation. Further research into the importance of central circulation physiology is warranted.
References
Athappan G, Patvardhan E, Tuzcu EM, et al. Incidence, predictors, and outcomes of aortic regurgitation after transcatheter aortic valve replacement: meta-analysis and systematic review of literature. J Am Coll Cardiol. 2013;61(15):1585–95.
Genereux P, Head SJ, Hahn R, et al. Paravalvular leak after transcatheter aortic valve replacement: the new Achilles’ heel? A comprehensive review of the literature. J Am Coll Cardiol. 2013;61(11):1125–36.
Lerakis S, Hayek SS, Douglas PS. Paravalvular aortic leak after transcatheter aortic valve replacement: current knowledge. Circulation. 2013;127(3):397–407.
Sinning JM, Hammerstingl C, Vasa-Nicotera M, et al. Aortic regurgitation index defines severity of peri-prosthetic regurgitation and predicts outcome in patients after transcatheter aortic valve implantation. J Am Coll Cardiol. 2012;59(13):1134–41.
Vasa-Nicotera M, Sinning JM, Chin D, et al. Impact of paravalvular leakage on outcome in patients after transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2012;5(8):858–65.
Patsalis PC, Konorza TF, Al-Rashid F, et al. Incidence, outcome and correlates of residual paravalvular aortic regurgitation after transcatheter aortic valve implantation and importance of haemodynamic assessment. EuroIntervention. 2013;8(12):1398–406.
Jilaihawi H, Chakravarty T, Shiota T, et al. Heart-rate adjustment of transcatheter haemodynamics improves the prognostic evaluation of paravalvular regurgitation after transcatheter aortic valve implantation. EuroIntervention. 2015;11(4):456–64.
Bangalore S, Messerli FH, Franklin SS, Mancia G, Champion A, Pepine CJ. Pulse pressure and risk of cardiovascular outcomes in patients with hypertension and coronary artery disease: an INternational VErapamil SR-trandolapril STudy (INVEST) analysis. Eur Heart J. 2009;30(11):1395–401.
Kappetein AP, Head SJ, Genereux P, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. J Am Coll Cardiol. 2012;60(15):1438–54.
Sellers RD, Lillehei CW, Edwards JE. Subaortic stenosis caused by anomalies of the atrioventricular valves. J Thorac Cardiovasc Surg. 1964;48:289–302.
Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):2440–92.
Karimi A, Pourafshar N, Park KE, et al. Late paravalvular aortic regurgitation: migration of the valve or late recoil? Cardiol Ther. 2017. (Epub ahead of print).
Laurent S, Cockcroft J, Van Bortel L, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27(21):2588–605.
Laurent S, Boutouyrie P, Asmar R, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001;37(5):1236–41.
Redheuil A, Yu WC, Wu CO, et al. Reduced ascending aortic strain and distensibility: earliest manifestations of vascular aging in humans. Hypertension. 2010;55(2):319–26.
Musa TA, Uddin A, Fairbairn TA, et al. Assessment of aortic stiffness by cardiovascular magnetic resonance following the treatment of severe aortic stenosis by TAVI and surgical AVR. J Cardiovasc Magn Reson. 2016;18(1):37.
Lindman BR, Alexander KP, O’Gara PT, Afilalo J. Futility, benefit, and transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2014;7(7):707–16.
Schoenenberger AW, Stortecky S, Neumann S, et al. Predictors of functional decline in elderly patients undergoing transcatheter aortic valve implantation (TAVI). Eur Heart J. 2013;34(9):684–92.
Holmes DR Jr, Brennan JM, Rumsfeld JS, et al. Clinical outcomes at 1 year following transcatheter aortic valve replacement. JAMA. 2015;313(10):1019–28.
Mack MJ, Brennan JM, Brindis R, et al. Outcomes following transcatheter aortic valve replacement in the United States. JAMA. 2013;310(19):2069–77.
Grover FL, Vemulapalli S, Carroll JD, et al. 2016 Annual Report of the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. J Am Coll Cardiol. 2017;69(10):1215–30.
Kodali S, Thourani VH, White J, et al. Early clinical and echocardiographic outcomes after SAPIEN 3 transcatheter aortic valve replacement in inoperable, high-risk and intermediate-risk patients with aortic stenosis. Eur Heart J. 2016;37(28):2252–62.
Manoharan G, Walton AS, Brecker SJ, et al. Treatment of symptomatic severe aortic stenosis with a novel resheathable supra-annular self-expanding transcatheter aortic valve system. JACC Cardiovasc Interv. 2015;8(10):1359–67.
Le Ven F, Freeman M, Webb J, et al. Impact of low flow on the outcome of high-risk patients undergoing transcatheter aortic valve replacement. J Am Coll Cardiol. 2013;62(9):782–8.
Herrmann HC, Pibarot P, Hueter I, et al. Predictors of mortality and outcomes of therapy in low-flow severe aortic stenosis: a Placement of Aortic Transcatheter Valves (PARTNER) trial analysis. Circulation. 2013;127(23):2316–26.
Magne J, Pibarot P, Sengupta PP, Donal E, Rosenhek R, Lancellotti P. Pulmonary hypertension in valvular disease: a comprehensive review on pathophysiology to therapy from the HAVEC Group. JACC Cardiovasc Imaging. 2015;8(1):83–99.
Barbash IM, Escarcega RO, Minha S, et al. Prevalence and impact of pulmonary hypertension on patients with aortic stenosis who underwent transcatheter aortic valve replacement. Am J Cardiol. 2015;115(10):1435–42.
Lucon A, Oger E, Bedossa M, et al. Prognostic implications of pulmonary hypertension in patients with severe aortic stenosis undergoing transcatheter aortic valve implantation: study from the FRANCE 2 Registry. Circ Cardiovasc Interv. 2014;7(2):240–7.
Lindman BR, Zajarias A, Maniar HS, et al. Risk stratification in patients with pulmonary hypertension undergoing transcatheter aortic valve replacement. Heart. 2015;101(20):1656–64.
Ribeiro HB, Orwat S, Hayek SS, et al. Cardiovascular magnetic resonance to evaluate aortic regurgitation after transcatheter aortic valve replacement. J Am Coll Cardiol. 2016;68(6):577–85.
Acknowledgements
No funding or sponsorship was received for this study or publication of this article. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Anthony A. Bavry discloses the following relationship—Honorarium from American College of Cardiology. Seyed Hossein Aalaei-Andabili, Ashkan Karimi, Ki Park, Calvin Y. Choi, Eddie W. Manning III, Thomas M. Beaver, and Wade W. Stinson have nothing to disclose.
Compliance with ethics guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/2C98F0607EEBC756.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bavry, A.A., Aalaei-Andabili, S.H., Karimi, A. et al. Comparison of Different Invasive Hemodynamic Measurements as a Prediction Tool for Mortality after Transcatheter Aortic Valve Replacement in Men: A Retrospective Observational Study. Cardiol Ther 6, 251–259 (2017). https://doi.org/10.1007/s40119-017-0095-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-017-0095-5