Abstract
Background
Extracellular vesicles (EVs), which are nanometer-sized vesicles enclosed by lipid membranes, are secreted by most cells and contain lipids, proteins, and various nucleic acid species from the source cell. Due to their natural origin, high biocompatibility, stability, targeting ability, multifunctionality, and low immunogenicity, EVs have been increasingly explored as potential drug delivery system (DDS) agents, offering new strategies for the treatment of cardiovascular disease, neurodegenerative disease, cancer and many other diseases. However, there are several challenges facing EVs as drug delivery systems, such as the low drug loading efficiency and the need for consensus on ideal cell types as sources for EVs at the clinical level.
Area Covered
This article briefly reviews the physiological characteristics of EVs and discusses the applicable conditions for endogenous and exogenous drug loading in EVs, as well as the delivery modes of EVs as carriers. Finally, the challenges of EVs stability and drug encapsulation efficiency of EVs as future DDS are also described.
Expert Opinion
This article mainly focused on the different methods of endogenous and exogenous drug loading, described the delivery modes of EVs as carriers in drug delivery, and the challenges of stability and drug encapsulation efficiency facing in the future in detail and deeply.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extracellular vesicles (EVs) are membrane-bound vesicles secreted by most cells; they are surrounded by a lipid bilayer and serve as crucial regulators of intercellular communication and various physiological and pathological processes, including stem cell maintenance, tissue repair, immune modulation, and tumor growth (Herrmann et al. 2021; Lehmann et al. 2023). In recent years, EVs have shown significant potential for disease treatment. On the one hand, by transporting DNA, RNA, and proteins, EVs can directly exhibit therapeutic effects; on the other hand, EVs can also serve as natural drug delivery system (DDS), offering new strategies for disease treatment (Table 1) (Mentkowski et al. 2018; Hanjani et al. 2022; Kumar et al. 2024).
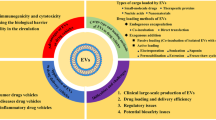
Due to their natural biogenesis, EVs are generated with intrinsic cell targeting properties, the ability to overcome natural barriers, stability in the circulation, and limited immunogenicity, which provide multiple advantages of EVs as a DDS over traditional delivery vehicles (Iravani and Varma 2022; Sil et al. 2020). EVs are naturally secreted by cells and share a membrane composition similar to that of their parent cells. This feature renders EVs less immunogenic and minimizes the likelihood of adverse reactions to the delivered drugs (Kurata et al. 2022). Additionally, EVs can be modified through adjustments of the source cells or their surface decoration, which would allow for the attachment of specific ligands that enhance targeted drug delivery to diseased tissues while reducing nonspecific distribution in normal tissues (Heydari et al. 2023). These characteristics endow EVs with significant potential and applicability in the field of drug delivery systems. However, many challenges persist, such as low drug loading efficiency, relatively poor stability and limitations in the precise control of drug release (Rahimian et al. 2024; Danilushkina et al. 2023). This review provides a comprehensive overview of the current research status of EVs and encompasses their preparation techniques, optimization strategies, and clinical applications (Fig. 1). The objective of this study was to systematically address the existing challenges and to progressively enhance the widespread application of EVs as DDS.
Characterization of EVs
Biological properties of EVs
EVs are lipid bilayer-enclosed vesicles generated and discharged by cells into the extracellular space. They include a diverse array of biologically active substances, including RNA, DNA, lipids, metabolites, and proteins. EVs constitute a diverse array of membrane-bound structures released by nearly all cell types, categorized into three primary classifications based on size (Mohammadi et al. 2023). Exosomes, which typically range from 30 to 200 nm in diameter, originate within intracellular vesicles and are subsequently released into the extracellular space through the fusion of multivesicular bodies with the cell membrane. Notably, exosomes are enriched in proteins, lipids, and RNA, particularly microRNAs, which facilitate intercellular communication. Microvesicles, ranging from 100 to 1000 nm in diameter, are directly shed from the cell membrane through dynamic changes, which results in the release of membrane fragments. Apoptotic bodies between 1000 and 5000 nm in size are generated by cells undergoing apoptosis and may contain nuclear fragments and organelles. For convenience, all three types are collectively referred to as EVs (van der et al. 2012; Mohammadipoor et al. 2023).
Exosomes are generated through the endocytic pathway, which involves invagination of the intracellular membrane and the formation of multivesicular bodies (MVBs). These MVBs can fuse with the plasma membrane, which facilitates the release of exosomes into the extracellular environment. Microvesicles (MVs) originate from outward budding and fission of the plasma membrane. Apoptotic bodies, which involve plasma membrane blebbing, the formation of membrane protrusions, and their subsequent release, emerge in the final stages of cell apoptosis (Table 2) (Thery et al. 2018; Maas et al. 2017). All subtypes share a vesicular lipid bilayer and carry a general composition of various proteins, lipids, and nucleic acids (Fig. 2). The specific contents are largely dependent on biological processes, cell origin, and culture conditions. The isolation of EVs is the primary condition for their use as a DDS, and each isolation method has advantages and limitations (Rao and Godaly 2023; Du et al. 2023) (Table 3). The selection of the appropriate method depends on the sample type, desired purity, and disease characteristics.
Cell source of EVs
When using EVs for drug delivery, careful consideration should be given to the source of cells because EVs from different cell types mediate distinct biological functions.
Immune cells
EVs derived from immune cells harbor a rich repertoire of immune factors and antigens, which enables the modulation of immune responses and the activation or inhibition of the immune system, offering a safer and more reliable DDS platform (Gharavi et al. 2022; Qi et al. 2023). Studies have shown that miRNAs transported by NK cell-derived EVs exhibit powerful tumor-killing and immune-regulating abilities (Neviani et al. 2019). Among these miRNAs, miR-3607-3p, which is abundant in NK-EVs, can directly target IL-26 to inhibit the progression of pancreatic cancer (Sun et al. 2019). Moreover, Dosil et al. reported that miR-10b-5p and miR-92a-3p play crucial roles in immune regulation and that they promote the downregulation of GATA3 and the reprogramming of receptor T cells toward the Th1 phenotype (Dosil et al. 2022).
The high specificity significantly enhances drug accumulation within tumor cells and reduces toxicity to normal cells compared with the direct use of chemotherapy drugs. Park et al. demonstrated the efficiency of immune cell-derived EVs in delivering tyrosinase-related protein-2 (TRP2) peptides to lymph nodes. TRP2-incorporated exosomes are efficiently internalized by macrophages and dendritic cells, which results in a strong release of proinflammatory cytokines and a strong fluorescent signal in the lymph nodes only 1 h after injection; this signal is maintained for at least 4 h (Park et al. 2018). Binding to receptors on the surface of tumor cells, the EVs derived from white blood cell could sencapsulated chemotherapy drugs, such as doxorubicin, results in a highly targeted delivery (Rayamajhi et al. 2019). However, the ability of neutrophil-derived EVs to regulate autologous neutrophils was not satisfactory, and the components of ectosomes were rapidly incorporated into recipient cells where they triggered neutrophil responses and reversed the survival effects of IFNγ and dexamethasone (Hurtado et al. 2022). Immune cell-derived EVs tolerate changes in both intracellular and extracellular environments, such as variations in acidity and enzyme levels. This inflammatory response positions immune cell-derived EVs as potential candidates for drug delivery in the context of inflammatory diseases.
Mesenchymal stem cells (MSCs)
MSCs-derived EVs for use as a DDS exhibit good biocompatibility, low immunogenicity and low immune rejection both in vitro and in vivo. They carry a rich array of bioactive substances that exhibit multiple functions in drug delivery (Ghasempour et al. 2022). Loading anti-inflammatory drugs into MSCs-derived EVs can effectively alleviate inflammatory reactions (Chulpanova et al. 2021). Yousefi et al. indicated that MSCs-EVs can be evaluated as an applicable nano-size carrier for antiviral therapeutic agents (Yousefi et al. 2022). The injection of anti-vascular endothelial growth factor (anti-VEGF) is an established method for treating diabetic retinopathy (DR), but this method is associated with complications such as inflammation and retinal detachment. Reddy et al. compared the efficacy of MSCs and MSCs-EVs loaded with the anti-VEGF drug bevacizumab in a rat model of DR and confirmed that EVs loaded with bevacizumab could reduce the frequency of vitreous injections to treat diabetic retinopathy. After injecting sEVs loaded with bevacizumab into the vitreous, the levels of VEGF, exudate, and leukostasis decreased for more than two months, with a sustained effect (Zhang et al. 2015).
The surface of EVs possesses specific receptors and molecules that can bind to particular cells to enable targeted delivery (Haraszti et al. 2016; Kusuma et al. 2018). This high degree of targeting enhances the accumulation of drugs in target cells and reduces the impact on nontarget cells. In comparison with MSCs, MSCs-derived EVs can avoid cytotoxic reactions and improve drug safety because of a lack of cell activity. Researchers have indicated that EVs extracted from MSCs overexpressing TRAIL, PTEN, and IFN-β1 exhibit strong antitumor and immune-modulating effects in vitro through activation of human immune cells and induction of apoptosis in various types of cancer cells (Bari et al. 2019); moreover, these EVs induce cancer cell apoptosis in a dose-dependent manner but have no cytotoxic effects on primary human bronchial epithelial cells (Reddy et al. 2023). These findings suggest that EVs derived from MSCs hold significant promise as novel carriers for delivering therapeutic agents to the tumor microenvironment.
Cancer cells
EVs originating from cancer cells can be derived from various types of cancer, including breast cancer, lung cancer, and liver cancer. This diversity allows researchers to select specific cancer cell sources for the preparation and optimization of drug delivery as needed (Wang et al. 2022a; Vader et al. 2016). Jiao et al. utilized breast cancer cell-derived EVs to deliver triphenylphosphonium (TPP)-modified therapeutic recombinant P53 proteins. TPP/P53 was loaded into EVs and was targeted to the mitochondria in breast cancer cells where the TPP/P53 molecules induced cancer cell death. EVs delivering TPP/P53 showed good tumor-targeting capability without any obvious toxicity in vivo (Jiao et al. 2022). Other studies have shown that encapsulating anticancer drugs, such as docetaxel, doxorubicin, and erlotinib, within cancer-derived EVs can significantly inhibit tumor growth and progression but can also reduce toxicity to normal cells (Zhao et al. 2021; Stridfeldt et al. 2023).
EVs can also reach distant sites from the primary lesion through the circulatory system, enabling remote delivery, which is particularly suitable for the treatment of metastatic cancer. The restrictive nature of the blood‒brain barrier (BBB) poses significant challenges for delivering drugs to the brain. Research conducted by Morad et al. demonstrated that tumor-derived EVs can breach an intact BBB through a transcytosis mechanism in vivo. The authors further identified the mechanism by which tumor-derived EVs circumvent the low physiologic rate of transcytosis in the BBB by decreasing the expression of Rab7 and increasing the efficiency of EVs transport (Morad et al. 2019). EVs from cancer cells can carry immunosuppressive substances that inhibit immune responses and reduce the body’s immune rejection reaction to drug delivery, thereby improving the effectiveness and stability of drug delivery. Despite the potential use of cancer cell-derived EVs as a drug delivery system, attention should still be given to their potential safety issues. EVs may contain potential pathogenic substances or factors that promote tumor metastasis, which poses certain risks to treatment effectiveness and patient safety.
Cargo loading for EVs
The techniques for loading cargo into EVs can be broadly classified into two main categories: exogenous loading, which involves the incorporation of small molecules, proteins, or RNA into or onto isolated EVs, and endogenous loading, which enables cells to naturally package small molecules, proteins, or RNA into EVs during biogenesis. Hence, it is imperative to consider potential impact of loading approaches based on drug release kinetics, organ-specific targeting, and delivery efficiency (Fig. 3).
Exogenous loading
Incubation
Incubation is a direct loading approach for DDS and involves the drugs to permeate the interior of EVs through diffusion or dissolution. Its direct, rapid, and simple nature makes incubation adaptable to various drugs and carriers (Tian et al. 2014a). Those capable of penetrating the lipid bilayer and small-molecule drugs, demonstrate high loading efficiency (Bulbake et al. 2017). Yang et al. incubated linezolid with macrophage-derived EVs, and the EVs potently killed methicillin-resistant staphylococcus aureus (Yang et al. 2018). Faruque et al. successively modified exosomes derived from human pancreatic ductal cancer cells with the functional ligand RGD (peptide composed of several repetitions of Arg-Gly-Asp), followed by incubation with paclitaxel (PTX) to obtain Exo-PTX, which exhibited increased cytotoxicity and significant targeted antitumor effects (Al et al. 2022). Therefore, the careful selection of cargo for incubation is paramount. However, it is crucial to note that incubation may be less efficient than other methods, which means that only a smaller portion of EVs can successfully carry drugs; this may require longer incubation times or higher drug concentrations.
Optimal conditions, such as temperature, duration, and drug concentration, must be established to maximize loading efficiency during incubation (Tian et al. 2014a; Zhang et al. 2013). Haney et al. reported that the efficiency of incubating catalase with macrophage-derived exosomes at room temperature for 18 h was 4.9%, but when 0.2% saponins were added, the efficiency improved to 18.5% (Haney et al. 2015). A study conducted by Zhuang showed that when EVs and curcumin were incubated at 22 °C for 5 min and then placed in a sucrose solution and centrifuged at 36,000 rpm for 1.5 h, intranasal delivery was effective in mice; this method provided a noninvasive and novel treatment approach for diseases associated with inflammation in the brain (Zhuang et al. 2011). Salomé et al. proposed that direct incubation (incubation of EVs for 2 h at 37 °C in a thermoblock with defined concentrations of a given chemotherapeutic drug) was a more efficient loading protocol than indirect incubation (incubation of the cell culture with the drug for 72 h) (Araujo-Abad et al. 2023). To improve the incubation efficiency, Piffoux et al. used polyethylene glycol (PEG) to induce fusion between EVs and liposomes with various biocompatible compositions and reported that the efficiency was greatest after 2 h in the presence of 30% (v/w) PEG, which increased the number of MSC-derived EVs used to deliver antitumor drugs to tumor cells by 3-4-fold (Piffoux et al. 2018).
Ultrasound
Ultrasonic technology utilizes ultrasonic energy to disrupt the lipid bilayer of EVs, which enables the entry of drugs into the carriers. This technology achieves targeted delivery and release of drugs within EVs through ultrasound aggregation, ultrasound radiation, or ultrasound-mediated cell membrane permeation. (Yudina et al. 2011; Wang et al. 2019; Maeshige et al. 2021). Nguyen et al. reported that EVs can effectively target mitochondria in cancer cells and deliver the photosensitizer chlorin e6 (Ce6) coupled with triphenylphosphonium (TPP) (TPP-Ce6). This leads to an increase in the generation of reactive oxygen species (ROS) in human breast cancer cells after exposure to ultrasound. Importantly, EVs encapsulating TPP-Ce6 effectively destroy mitochondria under ultrasound irradiation, which results in potent anticancer activity (Nguyen et al. 2023). Haney et al. used ultrasound to load catalase into exosomes. The mixture of catalase and exosomes was sonicated (500 V, 2 kHz, 20% power, 6 cycles with a 4 s pulse/2 sec pause), cooled on ice for 2 min, and then sonicated again using Qsonica, which may be a new treatment option for Parkinson’s disease (Haney et al. 2015).
Despite its advantages, such as high drug loading efficiency and continuous drug release, US has adverse effects on the structure of EVs, leading to changes in their spherical shape and in the efficiency of hydrophobic drug loading, which may cause EV aggregation (Zeng et al. 2023). Therefore, the combination of ultrasound with other methods for optimizing drug delivery has been suggested. For instance, a potential optimization approach is pulsed focused ultrasound, where the target tissue is treated with acoustic waves; this may constitute a strategy for enhancing the therapeutic efficacy of MSCs-derived EVs for the treatment of acute kidney injury. In a previous study, EVs significantly improved kidney function and reduced levels of injury markers, inflammation and apoptosis (Ullah et al. 2020).
Electroporation
Electroporation involves the application of an external electric field to modulate the permeability of the cell membrane, which temporarily disrupts its integrity and facilitates the penetration of drugs into the intracellular or extracellular space (Fuhrmann et al. 2015; Johnsen et al. 2016). Investigating the interaction between EVs and specific cell types has enabled the determination of optimal drug delivery strategies (Kooijmans et al. 2013). For instance, researchers have successfully loaded nicotine into EVs through electroporation, which led to neuroprotection and repair. In addition to small molecules and nucleic acid drugs, protein drugs can also be loaded directly into exosomes via electroporation. Rodriguez-Morales et al. successfully obtained insulin-containing exosomes by mixing exosomes with insulin, followed by electroporation and incubation at 37 °C for 1 h. They found that the loading efficiency was highest when the electroporation conditions were 200 V and 50 µF and that the loading efficiency of exosomes from different cell sources varied under the same electroporation conditions (Rodríguez-Morales et al. 2021). Wan et al. reported that the addition of Cas9 ribonucleoprotein complexes to electroporation buffers and electroporating the mixture to form exosome complexes can effectively improve the efficiency of exosome complex targeting of the liver and can be used to treat liver diseases (Wan et al. 2022).
The optimization of electroporation parameters is pivotal for enhancing the permeability and drug delivery efficiency of EVs in a scholarly context. Different cell types and EVs may exhibit varying sensitivities to electroporation parameters, which necessitates adjustments in external electric field strength, frequency, pulse width, and repetition count. Research has indicated that a combination of 18 V/cm voltage, a 10-millisecond pulse duration, and a frequency of 500 Hz yields heightened drug delivery efficiency in electroporation experiments involving cochlear EVs (Ma et al. 2014). Alvarez et al. mixed exosomes at a total protein concentration of 12 µg and 12 µg of siRNA in vivo in 400 µl of electroporation buffer (1.15 mM potassium phosphate, pH 7.2; 25 mM potassium chloride; 21% Optiprep) and electroporated the mixture in a 4 mm cuvette; they demonstrated the therapeutic potential of exosome-mediated siRNA delivery in Alzheimer’s disease (Alvarez-Erviti et al. 2011). Compared with the direct incubation of EVs with miRNA, Pomatto suggested that gentle electroporation can more effectively load and better protect miRNA from RNase degradation (Pomatto et al. 2019). While Kooijmans et al. were inclined that electroporation may induce siRNA precipitation, thereby masking the loading efficiency of biologic drugs in exosomes (Kooijmans et al. 2013). Moreover, electroporation may trigger the aggregation of EVs and alter their morphological characteristics, which highlights the importance of optimizing electroporation protocols to achieve efficient particle engineering in large clinical studies (Sil et al. 2020).
Chemical methods
EVs use chemical methodologies to undergo modifications that allow them to interface with drugs, which facilitates the indirect loading of pharmaceutical agents. These chemical alterations may encompass the introduction of affinity molecules binding to drugs or modifications to surface functional molecules, shielding the cargos from metabolic degradation. Zhuang et al. found that drugs with hydrophobic properties, such as temozolomide, can be dissolved in organic solvents and encapsulated within EVs through interactions with lipids in EVs membranes (Zhuang et al. 2011). In instances where drugs exhibit ionic characteristics, encapsulation into EVs can be achieved by forming ion pairs with membrane ions of opposite charges, which requires suitable ion concentration conditions. With its ionizable nature, doxorubicin can form ion pairs with phosphatidylserine on negatively charged membranes (Tian et al. 2014a). Membrane reconstitution exploits interactions between specific drug components and the EVs membrane to facilitate fusion; this necessitates the introduction of specific compounds through chemical means to establish fusion between EVs and drugs, such as organic solvents or surfactants, to disrupt the membrane. Following membrane disruption, the drug rebinds with the membrane and achieves encapsulation within the EVs (Alvarez-Erviti et al. 2011).
Surface modification is another frequently employed method, wherein surface modifiers possessing suitable functional groups that can interact with the surface of EVs are synthesized based on the drug’s characteristics and targets. These surface modifiers are then mixed with EVs through chemical reactions or covalent bonding to bind them to the membrane. Subsequently, the drug is chemically combined with a surface modifier, which enables the targeted display of the modified drug on the surface of EVs (Lai et al. 2015; Hood and Wickline 2012; Torchilin 2005). For instance, in one study, the surface modifier PEG was covalently attached to EVs to conjugate the anticancer drug cisplatin through a reaction involving the nitroso functional group of the conjugated PEG (Tiwari et al. 2021). The resultant modified EVs exhibited enhanced biostability and efficient drug delivery.
Genetic engineering
Genetic engineering techniques primarily utilize modification of EV surfaces to achieve effective exogenous drug loading. Genetic engineering could facilitate the surface expression or selective labeling of specific proteins or glycans on EVs, leading to targeted drug delivery (Mohammadi et al. 2023; Johnson et al. 2023). Genetic engineering facilitates actively loading soluble proteins into EVs, while loading proteins into purified EVs is challenging. Nedd4 family-interacting protein 1 (Ndfip1) was identified to mediate protein packaging into exosomes. Fusion of Cre recombinase with the WW domain of Nedd4, which interacts with L-domain of Ndfip1, resulted in efficient loading of Cre into exosomes (Sterzenbach et al. 2017). In addition, both soluble proteins and membrane proteins were loaded into exosomes through genetic fusion with ubiquitin at C-termini. Recent research from the Yao group revealed a mechanism by which ribonucleoprotein (RNP) are actively enriched in EVs. They inserted the RNA aptamer com into a single guide RNA and fused the com-binding aptamer-binding protein to both termini of the protein CD63, which is abundant in EVs. The interaction enriched Cas9 and adenine base editor RNP in EVs (Yao et al. 2021). In addition to protein cargoes, nucleic acids were actively loaded into EVs through exosome membrane-tethered RNA-binding domains. Hung et al. study shown that MS2 domain fused to CD63 increases RNA loading by six-fold and the active loading becomes more efficient for smaller RNA molecules (Hung and Leonard 2016).
In a study by Piffoux, researchers developed a genetic method for modifying EVs through fusion with liposomes containing a membrane and soluble cargo, with PEG as the trigger (Piffoux et al. 2018). This process resulted in the formation of a protective hydrophobic polymer shell that shielded the drug delivery carriers from external influences. Insertion of an albumin-binding domain (ABD) into the large extracellular loops (LELs) of CD63, CD9, and CD81 has been shown to drastically extend the plasma circulation time of EVs (Liang et al. 2022). Zheng et al. engineered an ABD into the LEL of TSPAN2, a scaffold protein, which had significantly higher concentration in plasma in comparison to wild-type tetraspanin-engineered EVs (Zheng et al. 2023). It is noteworthy that research on genetic engineering methods to modify EVs as drug delivery vehicles is still in its early stages, and the current modification methods require further optimization. Additional studies are essential to enhance the delivery efficiency, specificity, and stability of these carriers.
Endogenous loading
Endocytosis
During endogenous loading, drugs are captured and packaged by EVs that are synthesized within cells, which allows for their stable encapsulation and protection (Garnacho 2016). According to Verdera, regarding the cellular mechanism of drug uptake into EVs, the uptake of cholesterol and tyrosine kinase is associated with clathrin-independent endocytosis, which is dependent on the activity of cholesterol and tyrosine kinase, while the uptake of Na/H exchangers and phosphatidylinositol 3-kinase occurs primarily through micropinocytosis (Costa et al. 2017). Drugs can enter EVs through receptor recognition and binding to the membrane, followed by internalization through cellular endocytic processes (Oshchepkova et al. 2021). For instance, EVs can be loaded with anticancer chemotherapeutic drugs, such as paclitaxel, and certain aminoglycoside antibiotics such as sparsomycin (Yim et al. 2016). Cargo loading can also be achieved by modulating the oxalic acid endoplasmic reticulum pathway, mainly through the addition of oxalic acid antibiotics, such as streptomycin O, which are transported to endoplasmic reticulum vesicles and subsequently loaded into EVs (Yim et al. 2016). In addition, utilizing endogenous lipid analogs for loading immunomodulators into EVs can enhance their stability and extend their retention time in vivo.
Although endocytic pathways are well characterized, the ability to control them for drug delivery applications is still challenging. Cell-penetrating peptides have been shown to deliver chemical drugs, nucleic acids, and large molecules through cell membranes, which represents a new pathway for exogenous substances to enter cells. Another example is that peptides rich in essential amino acids, such as arginine, have a positive charge, and thus they interact with negatively charged drug molecules and cell membranes through noncovalent interactions, including electrostatic interactions (Hao et al. 2022). As a spatiotemporally controllable stimulus, ultrasound is used to enhance drug delivery efficiency due to its ability to increase cell membrane permeability, especially that of nanocarriers. Understanding the interaction between ultrasound control and cell membrane endocytosis is highly important for precise drug delivery (Wen et al. 2023).
Secretion regulatory
As EVs are carriers for drug delivery systems, the regulated secretion of EVs is orchestrated by a series of intracellular regulatory factors. These factors play a pivotal role in modulating the secretion of EVs by influencing their quantity, composition, and release time, thereby facilitating the endogenous loading of drugs under specific conditions.
Cellular stress is one such factor that has been extensively studied, with numerous investigations indicating that cells respond to stress stimuli, such as inflammatory, oxidative, and heat stress, which increasing the secretion of EVs. These EVs may carry biologically active molecules that regulate inflammation and stress responses, positioning them as potential tools for therapeutic drug delivery across various diseases (Tkach et al. 2018). The activation of specific signaling pathways also contributes to the regulation of EV production by cells. For instance, the activation of extracellular signal-regulated kinases (ERKs), phosphoinositide 3-kinase (PI3K), and mitochondrial signaling pathways can amplify the quantity of EVs released by cells. Furthermore, certain transcription factors and cytokines can impact cell function and reverse drug resistance by regulating EVs secretion (Pegtel and Gould 2019). Cellular responses to extrinsic stimuli play a significant role in regulating EV secretion. When cells are exposed to specific cytokines, growth factors, or hormones, the production and release of EVs are increased (Gyorgy et al. 2011). Notably, one study revealed that the presence of TGF-β in the extracellular environment significantly enhances the production of EVs by tumor cells (Zhang et al. 2017a). In the realm of gene regulation, genetic engineering techniques allow for the insertion of drug genes into the genomic DNA of EV carrier cells. This innovative approach enables cells to express drugs endogenously during EV synthesis and subsequently load them into EVs.
Genetic engineering
The endogenous expression and loading of specific drugs into EVs can be achieved through genetic engineering of carrier cells (Kooijmans et al. 2016b; Hadla et al. 2016; Tian et al. 2018). The transfection method involves the introduction and expression of the target gene in cells, which leads to the selective expression of the target gene by the cells during EV production. One frequently used transfection method is the use of viral vectors, such as adeno-associated viruses or lentiviruses, to deliver the target gene. For example, numerous studies have employed transfection techniques to introduce genes encoding antitumor proteins into cells, which results in the production of drug-loaded EVs by the cells. By transfecting cells with appropriate plasmids or transposons carrying drug gene sequences, EVs containing drugs can be generated. This method is commonly used to load miRNAs for gene knockdown experiments associated with RNA interference (Yang et al. 2015; Wahlgren et al. 2012).
In addition, transgenic approach can be accomplished through gene knock-in, gene mutation, and gene modification. By modifying the cellular genome, targeted genes can be expressed during the production of EVs. Through transgenic technique, cells can express specific proteins or RNAs in EVs, which faciliate targeted drug loading and delivery (Naldini 2015). For example, one study successfully loaded the antitumor drug TRAIL into EVs using genetically modified cells, which enabled the selective killing of tumor cells. CRISPR-Cas9 is a groundbreaking gene editing technology that allows direct targeting and modification of the cellular genome (Osteikoetxea et al. 2022). This powerful system enables researchers to precisely edit specific genes within cells, leading to the expression of targeted proteins, RNA, or other biologically active substances in EVs.
Membrane shedding
EVs carrying intracellular drugs can be naturally released through biological processes such as apoptosis or can be induced by external stimuli. This strategy effectively harnesses the EVs produced by cells for drug loading and delivery. The mechanism underlying the membrane shedding of EVs as carriers for drug delivery is multifaceted and involves various processes. Studies have demonstrated the involvement of matrix metalloproteinases in the membrane shedding of EVs, as these enzymes can hydrolyze components such as collagen and fibronectin in the cell membrane, thereby facilitating the shedding of EVs (Withrow et al. 2016; El-Andaloussi et al. 2012). Subcellular fusion is a crucial mechanism for intracellular membrane shedding and facilitates the secretion of EVs (Vader et al. 2014). In highly secretory-active cells, such as tumor cells, fusion events between the endoplasmic reticulum (ER) and other cellular organelles enhance the production and secretion of EVs. Moreover, in response to various stimuli, including cytokines, growth factors, and inflammatory factors, cells can exhibit a significant increase in EVs release (Kim et al. 2018; Antimisiaris et al. 2018). This stimulus-induced membrane shedding is likely regulated by intracellular signaling pathways such as the phosphoinositide 3-kinase (PI3K)/protein kinase B (Akt) pathway and the extracellular signal-regulated kinase (Erk) pathway, among others.
In general, EVs serve as carriers for DDS and allow for the effective loading of drugs through diverse physical, chemical, or biological methods during exogenous loading (Table 4). EVs leverage endogenous loading mechanisms and rely on the intrinsic biological processes and gene expression regulations or on mechanisms such as membrane fusion with target cells (Table 5). It enables customized and adaptable drug delivery tailored to the demands of specific drugs and target cells, which provides a versatile and diverse strategy for drug delivery and treatment.
Delivery
The use of EVs as drug delivery systems can be categorized into two primary approaches: direct delivery and targeted delivery. By strategically selecting appropriate types of EVs and designing delivery strategies, optimized drug therapy can be achieved to improve treatment efficacy while minimizing adverse reactions (Fig. 4).
Direct injection delivery
Due to the complexity of the metabolic and circulation systems in human body, traditional delivery can be prone to drug degradation and metabolism, decreasing drug half-life time in vivo. In contrast, EVs offer protection to drugs from the external environment, which enhances drug stability and persistence and notably extends a drug’s half-life within the body. When loaded with drugs, EVs can be directly administered to target tissues or sites through injection (Vader et al. 2016; Maiborodin et al. 2021). Nawaz et al. compared the difference in mRNA delivery between epithelial, endothelial, and cardiac progenitor cells, and found EVs from cardiac progenitor cells were the most efficient in promoting angiogenesis, which induced less expression of inflammatory cytokines compared to other vehicles used (Nawaz et al. 2023).
For drug delivery, EVs transport drugs directly to target tissues or cells via injection, and this way, they bypass drug loss and degradation in the bloodstream, which enhances drug stability and bioavailability. In one experiment, EVs containing therapeutic drugs for cancer treatment were intravenously injected into experimental animals to effectively deliver the drugs to cancer cells and inhibit tumor growth. EVs can also enhance drug solubility and improve pharmacokinetic parameters. For instance, direct injection of EVs derived from breast cancer cells effectively delivered antitumor drugs, which led to inhibition of tumor growth (Nawaz et al. 2023; Zhang et al. 2017a). Some drugs face challenges in effective delivery due to their low solubility. EVs, which serve as drug delivery carriers, can enhance drug solubility, thereby improving delivery efficacy. One study revealed that encapsulating calcium oxalate as a drug within EVs significantly enhanced drug solubility and increased the effectiveness of drug delivery to target cells.
Targeted delivery
EVs offer significant potential in the field of drug delivery, especially for achieving targeted delivery and minimizing off-target effects. The selection of suitable EVs sources is critical to achieve cell-targeted delivery. Selecting cells that express corresponding cell surface proteins or glycoproteins facilitates the production of EVs with a propensity for targeting specific cell surface receptors. For example, using HER2 receptor-positive cancer cells as the source can enable the targeting of HER2 receptor-positive tumor cells. In addition, appropriate modifications of EVs are common in cell-targeted delivery. Tian et al. generated a recombinant fusion protein containing the arginine-glycine-aspartic acid fused to the phosphatidylserine-binding domains of lactadherin and attached the targeting ligands onto EVs, which has obvious effect on treatment of ischemic stroke in mouse model (Tian et al. 2021). Pham et al. developed a simple enzymatic method to conjugate peptides and nanobodies onto EVs without any genetic or chemical modification of donor cells. They used protein ligating enzymes to create permanent covalent bonds between EVs and peptides. Targeted delivery of EV-encapsulated PTX at a low dose significantly enhanced the drug efficacy in suppressing tumour growth in lung cancer xenografted mouse model (Pham et al. 2021). This efficient and versatile method for the stable surface modification of EVs facilitated safe and specific delivery of therapeutic payloads to target cells, without the need for genetic and chemical modifications.
Biosynthetic regulation is also important for targeted delivery. Activation of the Wnt/β-catenin signaling pathway, for example, can promote EV production within tumor cells and increase the miRNA content, which enhances targeted delivery to other tumor cells. Further optimization of EV characteristics is important for enhancing cell uptake and drug release. Parameters such as size range, surface charge, lipid composition, and protein composition can be fine-tuned to improve EV stability and the efficiency of cellular uptake in vivo (Kooijmans et al. 2016; Zhang et al. 2016). Other methods, including magnetic control, thermosensitive modifications, surface membrane engineering, and genetic engineering modifications, can be employed to regulate the cellular uptake and drug release of EVs. Successful targeting and delivery efficiency in liver cancer treatment, for instance, have been achieved by modifying the surface of EVs with starch-like glycans.
Challenges
EVs are widely recognized as potential DDS carrier with high expression and enrichment of parent-cell specific signatures, while they also exhibit other typically low abundance and low enrichment of protein components (Fig. 5) (Herrmann et al. 2021). This complexity makes EVs a significant challenge for applications in drug delivery systems.
The complexity of EVs-mediated cell cross-talk responses (Herrmann et al. 2021)
Production of EVs
Due to the complex composition and function of EVs, no standard procedures have been developed for their isolation, purification, cryopreservation and transportation, and consequently, they are prone to contamination and even thrombosis. In addition, natural EVs have several limitations, such as limited function, low yield and variable biological activity, which restrict their practical use as stable therapeutic adjuvants. Most current methods for increasing EVs production are in the laboratory stage and are limited to human and mammalian cells (Mendt et al. 2018). Importantly, most purification methods are not suitable for scaled-up production and cannot be used to process EVs in large quantities of cultured cell samples (Gimona et al. 2017). Therefore, with the increasing demand for the clinical application of EVs, the establishment of an engineered synthesis process for the production, isolation and purification of EVs is urgently needed. Additionally, it is reported a large-scale production protocol of clinical-grade exosomes employing good manufacturing practices (GMP) standards. An ideal GMP-grade EVs production requires sterile generation of exosomes with therapeutic payloads, sufficient amounts for clinical testing, without batch-to-batch variation leading to compromised efficacy (Pedrioli et al. 2021).
Stability of EVs
First, the storage conditions of EVs are one of the challenges for DDS. Research shows that storage at 4 °C can lead to aggregation and structural damage of EVs. Even if the size and quantity of EVs remain unchanged at -80 °C, changes in their biological activity can still be detected. Therefore, freeze-drying has been demonstrated to be an alternative for long-term storage and is the most challenging and costly method in terms of logistics and transportation. Second, the administration of EVs affects their stability. For instance, systemically administered EVs have a short half-life and are rapidly taken up by mononuclear phagocytes, especially in the liver and spleen. Even with the stealth properties conferred by PEG, the terminal half-life of EVs is at most 60 min (Herrmann et al. 2021). Haney et al. found that local administration via intranasal injection of hydrogen peroxide-loaded EVs in a Parkinson’s disease mouse model resulted in greater accumulation of EVs in brain tissue after 4 h than intravenous injection (Haney et al. 2015). Therefore, establishing the most effective EVs delivery route for each application may help improve therapeutic outcomes. Magnetic drug targeting, which involves enhancing drug delivery to selected tissues by applying magnetic field gradients, represents a noninvasive alternative strategy for enhancing therapeutic efficacy. Silva et al. provided proof-of-concept validation for tissue-specific delivery using a combination of EVs and magnetic targeting. They incubated therapeutic agents and iron oxide nanoparticles with macrophages to generate EVs simultaneously loaded with therapeutic and magnetic nanoparticles. Magnetic targeting resulted in enhanced and spatially modulated uptake of EVs and drugs by cancer cells in vitro (Silva et al. 2015).
Finally, the mode of action of functional EVs also influences their stability. Untreated EVs are cleared from the body very quickly after administration, with nonspecific accumulation observed not only in the liver, spleen, gastrointestinal tract, and lungs but also in tumor tissues, and thus the addition of specific targeting ligands is required to enhance efficacy. Therefore, engineering EVs by modifying or attaching molecules to their surfaces is a common strategy for increasing their stability. The engineered modifications aim to optimize the biological distribution, stability, and pharmacokinetic characteristics of EVs, thereby promoting drug delivery (Herrmann et al. 2021; Kumar et al. 2024).
Efficiency of drug encapsulation
The other major challenge in the application of EVs is how to achieve efficient loading of therapeutic drugs. One of the reasons that efficient loading is challenging is that EVs themselves may contain parts of their parent cell contents as they form, which would result in limited space to load exogenous drugs into EVs. Additionally, the properties of the drug and the loading method chosen should be considered (Herrmann et al. 2021; Haney et al. 2015). Typical drugs for chronic diseases often have poor water solubility and low dissolution rates, which result in low bioavailability and a lack of efficacy. It might be beneficial to conduct preformulation studies integrated with the statistical design of the experiment. Hsieh et al. found that the design of experiments is an excellent tool that allows pharmaceutical scientists to systematically manipulate factors according to a prespecified design (Hsieh et al. 2023). Electroporation or ultrasonication has been shown to be successful for both small and large molecules (Alvarez-Erviti et al. 2011), but the potential impact on protein- and nucleic acid-based drugs should be carefully considered. Since the size of nucleic acids encapsulated in EVs by exogenous means is also limited, a cellular nanoperforation method for the mass production of functional EVs has been developed (Yang et al. 2020). This method increased the EV yield and the amount of messenger RNA in the samples. However, the additional steps required for transfection and electrical stimulation make its adoption in industry relatively difficult (Herrmann et al. 2021). Recently, an alternative approach based on liposomal fusion has been proposed (Piffoux et al. 2018). Liposomes containing fused gene lipids are incubated with EVs, and the cargo of synthetic liposomes is merged with the cargo of EVs. This approach may pave the way for the efficient loading of larger molecules without affecting the EVs membrane (de Jong et al. 2019).
In addition, the preformulation of drug cargos may influence their ability to become encapsulated within EVs. A full understanding of the physicochemical characteristics, pharmacokinetics, and efficacy/toxicity of drugs prior to drug loading is also a challenge for improving drug loading efficiency. Hydrophobic ion pairing can successfully increase the release kinetics control of ionizable hydrophilic drugs. Nevertheless, polymeric nanoparticle formulation development requires trial-and-error experimentation to meet the target product profile, which is laborious and costly. Therefore, Dimiouet al. designed a preformulation framework (the interactions between AZD2811, a small hydrophilic molecule, and counterions with different molecular structures) to increase drug loading (Dimiou et al. 2023).
Conclusion
Due to their natural origin, low immunogenicity, controllable delivery performance, stable drug-loading capacity, and potential for treating various diseases, EVs have emerged as a prominent research focus in the field of drug delivery systems. Through further investigations, EVs may evolve into precise drug delivery platforms that can be tailored and optimized for accurate and specific drug delivery purposes. In addition to carrying drugs, EVs can be engineered as multifunctional carriers capable of transporting other functional molecules, thereby expanding the possibilities for drug delivery, gene therapy, immune modulation, and other therapeutic needs. Furthermore, the integration of EVs with microtechnologies and nanotechnologies can enhance control and modification, which would ultimately improve drug delivery efficiency, stability, and controllability. It is anticipated that with ongoing research advancements and innovations, EVs will become a vital tool in the field of drug delivery and that EVs will offer more effective, precise, and personalized solutions for medical treatment.
References
Al FH, Choi ES, Kim JH, Kim E (2022) Enhanced effect of autologous EVs delivering paclitaxel in pancreatic cancer. J Control Release 347:330–346
Alvarez-Erviti L, Seow Y, Yin H, Betts C, Lakhal S, Wood MJ (2011) Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat Biotechnol 29:341–345
Antimisiaris SG, Mourtas S, Marazioti A (2018) Exosomes and exosome-inspired vesicles for targeted drug delivery. Pharmaceutics 10:218
Araujo-Abad S, Manresa-Manresa A, Rodríguez-Cañas E, Fuentes-Baile M, García-Morales P, Mallavia R, Saceda M, de Juan Romero C (2023) New therapy for pancreatic cancer based on extracellular vesicles. Biomed Pharmacother 162:114657
Bari E, Ferrarotti I, Di Silvestre D, Grisoli P, Barzon V, Balderacchi A, Torre ML, Rossi R, Mauri P, Corsico AG, Perteghella S (2019) Adipose mesenchymal extracellular vesicles as alpha-1-Antitrypsin physiological Delivery systems for Lung Regeneration. Cells 8:965
Bulbake U, Doppalapudi S, Kommineni N, Khan W (2017) Liposomal formulations in clinical use: an updated review. Pharmaceutics 9:12
Chulpanova DS, Gilazieva ZE, Akhmetzyanova ER, Kletukhina SK, Rizvanov AA, Solovyeva VV (2021) Cytochalasin B-induced membrane vesicles from human mesenchymal stem cells overexpressing TRAIL, PTEN and IFN-beta1 can kill carcinoma cancer cells. Tissue Cell 73:101664
Costa VH, Gitz-Francois JJ, Schiffelers RM, Vader P (2017) Cellular uptake of extracellular vesicles is mediated by clathrin-independent endocytosis and macropinocytosis. J Control Release 266:100–108
Danilushkina AA, Emene CC, Barlev NA, Gomzikova MO (2023) Strategies for Engineering of Extracellular vesicles. Int J Mol Sci 24:13247
de Jong OG, Kooijmans SAA, Murphy DE, Jiang L, Evers MJW, Sluijter JPG, Vader P, Schiffelers RM (2019) Drug delivery with Extracellular vesicles: from imagination to Innovation. Acc Chem Res 52(7):1761–1770
Dimiou S, McCabe J, Booth R, Booth J, Nidadavole K, Svensson O, Sparén A, Lindfors L, Paraskevopoulou V, Mead H, Coates L, Workman D, Martin D, Treacher K, Puri S, Taylor LS, Yang B (2023) Selecting counterions to improve Ionized Hydrophilic Drug Encapsulation in Polymeric nanoparticles. Mol Pharm 20(2):1138–1155
Dosil SG, Lopez-Cobo S, Rodriguez-Galan A, Fernandez-Delgado I, Ramirez-Huesca M, Milan-Rois P, Castellanos M, Somoza A, Gómez MJ, Reyburn HT, Vales-Gomez M, Sánchez Madrid F, Fernandez-Messina L (2022) Natural killer (NK) cell-derived extracellular-vesicle shuttled microRNAs control T cell responses. Elife 11:e76319
Du S, Guan Y, Xie A, Yan Z, Gao S, Li W, Rao L, Chen X, Chen T (2023) Extracellular vesicles: a rising star for therapeutics and drug delivery. J Nanobiotechnol 21(1):231
El-Andaloussi S, Lee Y, Lakhal-Littleton S, Li J, Seow Y, Gardiner C, Alvarez-Erviti L, Sargent IL, Wood MJ (2012) Exosome-mediated delivery of siRNA in vitro and in vivo. Nat Protoc 7:2112–2126
Fuhrmann G, Serio A, Mazo M, Nair R, Stevens MM (2015) Active loading into extracellular vesicles significantly improves the cellular uptake and photodynamic effect of porphyrins. J Control Release 205:35–44
Garnacho C (2016) Intracellular drug delivery: mechanisms for cell entry. Curr Pharm Des 22:1210–1226
Gharavi AT, Hanjani NA, Movahed E, Doroudian M (2022) The role of macrophage subtypes and exosomes in immunomodulation. Cell Mol Biol Lett 27(1):83
Ghasempour E, Hesami S, Movahed E, Keshel SH, Doroudian M (2022) Mesenchymal stem cell-derived exosomes as a new therapeutic strategy in the brain tumors. Stem Cell Res Ther 13(1):527
Gimona M, Pachler K, Laner-Plamberger S, Schallmoser K, Rohde E (2017) Manufacturing of Human Extracellular vesicle-based therapeutics for clinical use. Int J Mol Sci 18:1190
György B, Szabó TG, Pásztói M, Pál Z, Misják P, Aradi B, László V, Pállinger E, Pap E, Kittel A, Nagy G, Falus A, Buzás EI (2011) Membrane vesicles, current state-of-the-art: emerging role of extracellular vesicles. Cell Mol Life Sci 68:2667–2688
Hadla M, Palazzolo S, Corona G, Caligiuri I, Canzonieri V, Toffoli G, Rizzolio F (2016) Exosomes increase the therapeutic index of doxorubicin in breast and ovarian cancer mouse models. Nanomed (Lond) 11:2431–2441
Haney MJ, Klyachko NL, Zhao Y, Gupta R, Plotnikova EG, He Z, Patel T, Piroyan A, Sokolsky M, Kabanov AV, Batrakova EV (2015) Exosomes as drug delivery vehicles for Parkinson’s disease therapy. J Control Release 207:18–30
Hanjani NA, Esmaelizad N, Zanganeh S, Gharavi AT, Heidarizadeh P, Radfar M, Omidi F, MacLoughlin R, Doroudian M (2022) Emerging role of exosomes as biomarkers in cancer treatment and diagnosis. Crit Rev Oncol Hematol 169:103565
Hao M, Zhang L, Chen P (2022) Membrane internalization mechanisms and design strategies of Arginine-Rich cell-penetrating peptides. Int J Mol Sci 23:9038
Haraszti RA, Didiot MC, Sapp E, Leszyk J, Shaffer SA, Rockwell HE, Gao F, Narain NR, DiFiglia M, Kiebish MA, Aronin N, Khvorova A (2016) High-resolution proteomic and lipidomic analysis of exosomes and microvesicles from different cell sources. J Extracell Vesicles 5:32570
Herrmann IK, Wood MJA, Fuhrmann G (2021) Extracellular vesicles as a next-generation drug delivery platform. Nat Nanotechnol 16(7):748–759
Heydari R, Koohi F, Rasouli M, Rezaei K, Abbasgholinejad E, Bekeschus S, Doroudian M (2023) Exosomes as rheumatoid arthritis diagnostic biomarkers and therapeutic agents. Vaccines (Basel) 11(3):687
Hood JL, Wickline SA (2012) A systematic approach to exosome-based translational nanomedicine. Wiley Interdiscip Rev Nanomed Nanobiotechnol 4:458–467
Hsieh CM, Yang TL, Putri AD, Chen CT (2023) Application of design of experiments in the Development of Self-Microemulsifying Drug Delivery systems. Pharmaceuticals (Basel) 16(2):283
Hung ME, Leonard JN (2016) A platform for actively loading cargo RNA to elucidate limiting steps in EV-mediated delivery. J Extracell Vesicles 5:31027
Hurtado Gutiérrez MJ, Allard FL, Mosha HT, Dubois CM, McDonald PP (2022) Human neutrophils generate extracellular vesicles that modulate their functional responses. Cells 12:136
Iravani S, Varma RS (2022) Advanced Drug Delivery Micro- and Nanosystems for Cardiovascular diseases. Molecules 27:5843
Jiao Y, Tang Y, Li Y, Liu C, He J, Zhang LK, Guan YQ (2022) Tumor cell-derived extracellular vesicles for breast cancer specific delivery of therapeutic P53. J Control Release 349:606–616
Johnsen KB, Gudbergsson JM, Skov MN, Christiansen G, Gurevich L, Moos T, Duroux M (2016) Evaluation of electroporation-induced adverse effects on adipose-derived stem cell exosomes. Cytotechnology 68:2125–2138
Johnson V, Vasu S, Kumar US, Kumar M (2023) Surface-Engineered Extracellular vesicles in Cancer Immunotherapy. Cancers (Basel) 15:2838
Kim MS, Haney MJ, Zhao Y, Yuan D, Deygen I, Klyachko NL, Kabanov AV, Batrakova EV (2018) Engineering macrophage-derived exosomes for targeted paclitaxel delivery to pulmonary metastases: in vitro and in vivo evaluations. Nanomedicine 14:195–204
Kooijmans SAA, Stremersch S, Braeckmans K, de Smedt SC, Hendrix A, Wood MJA, Schiffelers RM, Raemdonck K, Vader P (2013) Electroporation-induced siRNA precipitation obscures the efficiency of siRNA loading into extracellular vesicles. J Control Release 172:229–238
Kooijmans S, Aleza CG, Roffler SR, van Solinge WW, Vader P, Schiffelers RM (2016a) Display of GPI-anchored anti-EGFR nanobodies on extracellular vesicles promotes tumour cell targeting. J Extracell Vesicles 5:31053
Kooijmans S, Schiffelers RM, Zarovni N, Vago R (2016b) Modulation of tissue tropism and biological activity of exosomes and other extracellular vesicles: New Nanotools for cancer treatment. Pharmacol Res 111:487–500
Kumar MA, Baba SK, Sadida HQ, Marzooqi SA, Jerobin J, Altemani FH, Algehainy N, Alanazi MA, Abou-Samra AB, Kumar R, Al-Shabeeb Akil AS, Macha MA, Mir R, Bhat AA (2024) Extracellular vesicles as tools and targets in therapy for diseases. Signal Transduct Target Ther 9(1):27
Kurata A, Kiyohara S, Imai T, Yamasaki-Yashiki S, Zaima N, Moriyama T, Kishimoto N, Uegaki K (2022) Characterization of extracellular vesicles from lactiplantibacillus plantarum. Sci Rep 12:13330
Kusuma GD, Barabadi M, Tan JL, Morton DAV, Frith JE, Lim R (2018) To protect and to preserve: Novel Preservation Strategies for Extracellular vesicles. Front Pharmacol 9:1199
Lai CP, Kim EY, Badr CE, Weissleder R, Mempel TR, Tannous BA, Breakefield XO (2015) Visualization and tracking of tumour extracellular vesicle delivery and RNA translation using multiplexed reporters. Nat Commun 6:7029
Lehmann TP, Golik M, Olejnik J, Łukaszewska M, Markowska D, Drożdżyńska M, Kotecki A, Głowacki M, Jagodziński PP (2023) Potential applications of using tissue-specific EVs in targeted therapy and vaccinology. Biomed Pharmacother 166:115308
Liang X, Niu Z, Galli V, Howe N, Zhao Y, Wiklander OPB, Zheng W, Wiklander RJ, Corso G, Davies C, Hean J, Kyriakopoulou E, Mamand DR, Amin R, Nordin JZ, Gupta D, Andaloussi SE (2022) Extracellular vesicles engineered to bind albumin demonstrate extended circulation time and lymph node accumulation in mouse models. J Extracell Vesicles 11(7):e12248
Ma S, Schroeder B, Sun C, Loufakis DN, Cao Z, Sriranganathan N, Lu C (2014) Electroporation-based delivery of cell-penetrating peptide conjugates of peptide nucleic acids for antisense inhibition of intracellular bacteria. Integr Biol (Camb) 6:973–978
Maas S, Breakefield XO, Weaver AM (2017) Extracellular vesicles: Unique Intercellular Delivery vehicles. Trends Cell Biol 27:172–188
Maeshige N, Langston PK, Yuan ZM, Kondo H, Fujino H (2021) High-intensity ultrasound irradiation promotes the release of extracellular vesicles from C2C12 myotubes. Ultrasonics 110:106243
Maiborodin I, Klinnikova M, Kuzkin S, Maiborodina V, Krasil’nikov S, Pichigina A, Lushnikova E (2021) Morphology of the myocardium after experimental bone tissue trauma and the Use of Extracellular vesicles derived from mesenchymal multipotent stromal cells. J Pers Med 11:1206
Mendt M, Kamerkar S, Sugimoto H, McAndrews KM, Wu CC, Gagea M, Yang S, Blanko EVR, Peng Q, Ma X, Marszalek JR, Maitra A, Yee C, Rezvani K, Shpall E, LeBleu VS, Kalluri R (2018) Generation and testing of clinical-grade exosomes for pancreatic cancer. JCI Insight 3(8):e99263
Mentkowski KI, Snitzer JD, Rusnak S, Lang JK (2018) Therapeutic potential of Engineered Extracellular vesicles. AAPS J 20(3):50
Mohammadi AH, Ghazvinian Z, Bagheri F, Harada M, Baghaei K (2023) Modification of Extracellular Vesicle surfaces: an Approach for targeted drug delivery. BioDrugs 37:353–374
Mohammadipoor A, Hershfield MR, Linsenbardt HR, Smith J, Mack J, Natesan S, Averitt DL, Stark TR, Sosanya NM (2023) Biological function of Extracellular vesicles (EVs): a review of the field. Mol Biol Rep 50:8639–8651
Morad G, Carman CV, Hagedorn EJ, Perlin JR, Zon LI, Mustafaoglu N, Park TE, Ingber DE, Daisy CC, Moses MA (2019) Tumor-derived extracellular vesicles breach the Intact blood-brain barrier via Transcytosis. ACS Nano 13:13853–13865
Naldini L (2015) Gene therapy returns to centre stage. Nature 526:351–360
Nawaz M, Heydarkhan-Hagvall S, Tangruksa B, González-King Garibotti H, Jing Y, Maugeri M, Kohl F, Hultin L, Reyahi A, Camponeschi A, Kull B, Christoffersson J, Grimsholm O, Jennbacken K, Sundqvist M, Wiseman J, Bidar AW, Lindfors L, Synnergren J, Valadi H (2023) Lipid nanoparticles deliver the therapeutic VEGFA mRNA in Vitro and in vivo and transform Extracellular vesicles for their functional extensions. Adv Sci (Weinh) 10:e2206187
Neviani P, Wise PM, Murtadha M, Liu CW, Wu CH, Jong AY, Seeger RC, Fabbri M (2019) Natural killer-derived exosomal miR-186 inhibits Neuroblastoma Growth and Immune escape mechanisms. Cancer Res 79:1151–1164
Nguyen CT, Truong HQ, Hong EJ, Kang SJ, Kang JH, Ravichandran V, Kang HC, Ko YT, Rhee WJ, Shim MS (2023) Mitochondria-targeting sonosensitizer-loaded extracellular vesicles for chemo-sonodynamic therapy. J Control Release 354:651–663
Oh C, Koh D, Jeon HB, Kim KM (2022) The role of Extracellular vesicles in Senescence. Mol Cells 45:603–609
Oshchepkova A, Markov O, Evtushenko E, Chernonosov A, Kiseleva E, Morozova K, Matveeva V, Artemyeva L, Vlassov V, Zenkova M (2021) Tropism of Extracellular vesicles and cell-derived nanovesicles to normal and Cancer cells: New perspectives in Tumor-targeted nucleic acid delivery. Pharmaceutics 13:1911
Osteikoetxea X, Silva A, Lázaro-Ibáñez E, Salmond N, Shatnyeva O, Stein J, Schick J, Wren S, Lindgren J, Firth M, Madsen A, Mayr LM, Overman R, Davies R, Dekker N (2022) Engineered Cas9 extracellular vesicles as a novel gene editing tool. J Extracell Vesicles 11:e12225
Park O, Choi ES, Yu G, Kim JY, Kang YY, Jung H, Mok H (2018) Efficient delivery of tyrosinase related Protein-2 (TRP2) peptides to Lymph Nodes using serum-derived exosomes. Macromol Biosci 18:e1800301
Pedrioli G, Piovesana E, Vacchi E, Balbi C (2021) Extracellular vesicles as Promising Carriers in Drug Delivery: considerations from a cell biologist’s perspective. Biology (Basel) 10(5):376
Pegtel DM, Gould SJ (2019) Exosomes. Annu Rev Biochem 88:487–514
Pham TC, Jayasinghe MK, Pham TT, Yang Y, Wei L, Usman WM, Chen H, Pirisinu M, Gong J, Kim S, Peng B, Wang W, Chan C, Ma V, Nguyen NTH, Kappei D, Nguyen XH, Cho WC, Shi J, Le MTN (2021) Covalent conjugation of extracellular vesicles with peptides and nanobodies for targeted therapeutic delivery. J Extracell Vesicles 10(4):e12057
Piffoux M, Silva A, Wilhelm C, Gazeau F, Tareste D (2018) Modification of Extracellular vesicles by Fusion with liposomes for the design of Personalized Biogenic Drug Delivery systems. ACS Nano 12:6830–6842
Pomatto MAC, Bussolati B, D’Antico S, Ghiotto S, Tetta C, Brizzi MF, Camussi G (2019) Improved loading of plasma-derived extracellular vesicles to encapsulate Antitumor miRNAs. Mol Ther Methods Clin Dev 13:133–144
Qi Y, Zhao X, Dong Y, Wang M, Wang J, Fan Z, Weng Q, Yu H, Li J (2023) Opportunities and challenges of natural killer cell-derived extracellular vesicles. Front Bioeng Biotechnol 11:1122585
Rahimian S, Najafi H, Afzali B, Doroudian M (2024) Extracellular vesicles and exosomes: Novel insights and perspectives on Lung Cancer from early detection to targeted treatment. Biomedicines 12(1):123
Rao KU, Godaly G (2023) Isolation and purification of mycobacterial extracellular vesicles (EVs). Methods Mol Biol 2674:55–60
Rayamajhi S, Nguyen T, Marasini R, Aryal S (2019) Macrophage-derived exosome-mimetic hybrid vesicles for tumor targeted drug delivery. Acta Biomater 94:482–494
Reddy SK, Ballal AR, Shailaja S, Seetharam RN, Raghu CH, Sankhe R, Pai K, Tender T, Mathew M, Aroor A, Shetty AK, Adiga S, Devi V, Muttigi MS, Upadhya D (2023) Small extracellular vesicle-loaded bevacizumab reduces the frequency of intravitreal injection required for diabetic retinopathy. Theranostics 13:2241–2255
Rodríguez-Morales B, Antunes-Ricardo M, González-Valdez J (2021) Exosome-mediated insulin delivery for the potential treatment of diabetes Mellitus. Pharmaceutics 13(11):1870
Sil S, Dagur RS, Liao K, Peeples ES, Hu G, Periyasamy P, Buch S (2020) Strategies for the use of Extracellular vesicles for the delivery of therapeutics. J Neuroimmune Pharmacol 15(3):422–442
Silva AK, Luciani N, Gazeau F, Aubertin K, Bonneau S, Chauvierre C, Letourneur D, Wilhelm C (2015) Combining magnetic nanoparticles with cell derived microvesicles for drug loading and targeting. Nanomedicine 11(3):645–655
Sterzenbach U, Putz U, Low LH, Silke J, Tan SS, Howitt J (2017) Engineered Exosomes as vehicles for biologically active proteins. Mol Ther 25(6):1269–1278
Stridfeldt F, Cavallaro S, Haag P, Lewensohn R, Linnros J, Viktorsson K, Dev A (2023) Analyses of single extracellular vesicles from non-small lung cancer cells to reveal effects of epidermal growth factor receptor inhibitor treatments. Talanta 259:124553
Sun H, Shi K, Qi K, Kong H, Zhang J, Dai S, Ye W, Deng T, He Q, Zhou M (2019) Natural killer cell-derived exosomal mir-3607-3p inhibits pancreatic Cancer progression by targeting IL-26. Front Immunol 10:2819
Thery C, Witwer KW, Aikawa E, Alcaraz MJ, Anderson JD et al (2018) Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles 7:1535750
Tian T, Zhu YL, Zhou YY, Liang GF, Wang YY, Hu FH, Xiao ZD (2014) Exosome uptake through clathrin-mediated endocytosis and macropinocytosis and mediating miR-21 delivery. J Biol Chem 289:22258–22267
Tian Y, Li S, Song J, Ji T, Zhu M, Anderson GJ, Wei J, Nie G (2014a) A doxorubicin delivery platform using engineered natural membrane vesicle exosomes for targeted tumor therapy. Biomaterials 35:2383–2390
Tian T, Zhang HX, He CP, Fan S, Zhu YL, Qi C, Huang NP, Xiao ZD, Lu ZH, Tannous BA, Gao J (2018) Surface functionalized exosomes as targeted drug delivery vehicles for cerebral ischemia therapy. Biomaterials 150:137–149
Tian T, Cao L, He C, Ye Q, Liang R, You W, Zhang H, Wu J, Ye J, Tannous BA, Gao J (2021) Targeted delivery of neural progenitor cell-derived extracellular vesicles for anti-inflammation after cerebral ischemia. Theranostics 11(13):6507–6521
Tiwari S, Kumar V, Randhawa S, Verma SK (2021) Preparation and characterization of extracellular vesicles. Am J Reprod Immunol 85:e13367
Tkach M, Kowal J, Thery C (2018) Why the need and how to approach the functional diversity of extracellular vesicles. Philos Trans R Soc Lond B Biol Sci 373:20160479
Torchilin VP (2005) Recent advances with liposomes as pharmaceutical carriers. Nat Rev Drug Discov 4:145–160
Ullah M, Liu DD, Rai S, Razavi M, Concepcion W, Thakor AS (2020) Pulsed focused ultrasound enhances the therapeutic effect of mesenchymal stromal cell-derived extracellular vesicles in acute kidney injury. Stem Cell Res Ther 11:398
Vader P, Breakefield XO, Wood MJ (2014) Extracellular vesicles: emerging targets for cancer therapy. Trends Mol Med 20:385–393
Vader P, Mol EA, Pasterkamp G, Schiffelers RM (2016) Extracellular vesicles for drug delivery. Adv Drug Deliv Rev 106:148–156
van der Pol E, Boing AN, Harrison P, Sturk A, Nieuwland R (2012) Classification, functions, and clinical relevance of extracellular vesicles. Pharmacol Rev 64:676–705
Wahlgren J, De L, Karlson T, Brisslert M, Vaziri Sani F, Telemo E, Sunnerhagen P, Valadi H (2012) Plasma exosomes can deliver exogenous short interfering RNA to monocytes and lymphocytes. Nucleic Acids Res 40:e130
Wan T, Zhong J, Pan Q, Zhou T, Ping Y, Liu X (2022) Exosome-mediated delivery of Cas9 ribonucleoprotein complexes for tissue-specific gene therapy of liver diseases. Sci Adv 8(37):eabp9435
Wang L, Abhange KK, Wen Y, Chen Y, Xue F, Wang G, Tong J, Zhu C, He X, Wan Y (2019) Preparation of Engineered Extracellular vesicles derived from human umbilical cord mesenchymal stem cells with Ultrasonication for skin rejuvenation. ACS Omega 4:22638–22645
Wang Z, Mo H, He Z, Chen A, Cheng P (2022) Extracellular vesicles as an emerging drug delivery system for cancer treatment: current strategies and recent advances. Biomed Pharmacother 153:113480
Wang C, Li N, Li Y, Hou S, Zhang W, Meng Z, Wang S, Jia Q, Tan J, Wang R, Zhang R (2022a) Engineering a HEK-293T exosome-based delivery platform for efficient tumor-targeting chemotherapy/internal irradiation combination therapy. J Nanobiotechnol 20:247
Wen Z, Liu C, Teng Z, Jin Q, Liao Z, Zhu X, Huo S (2023) Ultrasound meets the cell membrane: for enhanced endocytosis and drug delivery. Nanoscale 15:13532–13545
Withrow J, Murphy C, Liu Y, Hunter M, Fulzele S, Hamrick MW (2016) Extracellular vesicles in the pathogenesis of rheumatoid arthritis and osteoarthritis. Arthritis Res Ther 18:286
Yang T, Martin P, Fogarty B, Brown A, Schurman K, Phipps R, Yin VP, Lockman P, Bai S (2015) Exosome delivered anticancer drugs across the blood-brain barrier for brain cancer therapy in Danio rerio. Pharm Res 32:2003–2014
Yang X, Shi G, Guo J, Wang C, He Y (2018) Exosome-encapsulated antibiotic against intracellular infections of methicillin-resistant Staphylococcus aureus. Int J Nanomed 13:8095–8104
Yang Z, Shi J, Xie J, Wang Y, Sun J, Liu T, Zhao Y, Zhao X, Wang X, Ma Y, Malkoc V, Chiang C, Deng W, Chen Y, Fu Y, Kwak KJ, Fan Y, Kang C, Yin C, Rhee J, Bertani P, Otero J, Lu W, Yun K, Lee AS, Jiang W, Teng L, Kim BYS, Lee LJ (2020) Large-scale generation of functional mRNA-encapsulating exosomes via cellular nanoporation. Nat Biomed Eng 4(1):69–83
Yao X, Lyu P, Yoo K, Yadav MK, Singh R, Atala A, Lu B (2021) Engineered extracellular vesicles as versatile ribonucleoprotein delivery vehicles for efficient and safe CRISPR genome editing. J Extracell Vesicles 10:e12076
Yim N, Ryu SW, Choi K, Lee KR, Lee S, Choi H, Kim J, Shaker MR, Sun W, Park JH, Kim D, Heo WD, Choi C (2016) Exosome engineering for efficient intracellular delivery of soluble proteins using optically reversible protein-protein interaction module. Nat Commun 7:12277
Yousefi Dehbidi M, Goodarzi N, Azhdari MH, Doroudian M (2022) Mesenchymal stem cells and their derived exosomes to combat Covid-19. Rev Med Virol 32(2):e2281
Yudina A, de Smet M, Lepetit-Coiffé M, Langereis S, Van Ruijssevelt L, Smirnov P, Bouchaud V, Voisin P, Grüll H, Moonen CT (2011) Ultrasound-mediated intracellular drug delivery using microbubbles and temperature-sensitive liposomes. J Control Release 155:442–448
Zeng H, Guo S, Ren X, Wu Z, Liu S, Yao X (2023) Current strategies for Exosome Cargo Loading and Targeting Delivery. Cells 12:1416
Zhang Y, Wang Z, Gemeinhart RA (2013) Progress in microRNA delivery. J Control Release 172:962–974
Zhang B, Wu X, Zhang X, Sun Y, Yan Y, Shi H, Zhu Y, Wu L, Pan Z, Zhu W, Qian H, Xu W (2015) Human umbilical cord mesenchymal stem cell exosomes enhance angiogenesis through the Wnt4/beta-catenin pathway. Stem Cells Transl Med 4:513–522
Zhang W, Zhou X, Zhang H, Yao Q, Liu Y, Dong Z (2016) Extracellular vesicles in diagnosis and therapy of kidney diseases. Am J Physiol Ren Physiol 311:F844–F851
Zhang Z, Li X, Sun W, Yue S, Yang J, Li J, Ma B, Wang J, Yang X, Pu M, Ruan B, Zhao G, Huang Q, Wang L, Tao K, Dou K (2017) Loss of exosomal miR-320a from cancer-associated fibroblasts contributes to HCC proliferation and metastasis. Cancer Lett 397:33–42
Zhang H, Deng T, Liu R, Bai M, Zhou L, Wang X, Li S, Wang X, Yang H, Li J, Ning T, Huang D, Li H, Zhang L, Ying G, Ba Y (2017a) Exosome-delivered EGFR regulates liver microenvironment to promote gastric cancer liver metastasis. Nat Commun 8:15016
Zhao Q, Hai B, Kelly J, Wu S, Liu F (2021) Extracellular vesicle mimics made from iPS cell-derived mesenchymal stem cells improve the treatment of metastatic prostate cancer. Stem Cell Res Ther 12:29
Zheng W, Rädler J, Sork H, Niu Z, Roudi S, Bost JP, Görgens A, Zhao Y, Mamand DR, Liang X, Wiklander OPB, Lehto T, Gupta D, Nordin JZ, El Andaloussi S (2023) Identification of scaffold proteins for improved endogenous engineering of extracellular vesicles. Nat Commun 14(1):4734
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 82100992).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Research involving in human and animal rights
This article does not contain any studies with human and animal subjects performed by any of the authors.
Conflict of interest
All authors (Xiaolin Lu, Siyuan Fan, Meng Cao, Dongmei Liu, Kun Xuan and Anqi Liu) declare that they have no confict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lu, X., Fan, S., Cao, M. et al. Extracellular vesicles as drug delivery systems in therapeutics: current strategies and future challenges. J. Pharm. Investig. (2024). https://doi.org/10.1007/s40005-024-00699-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40005-024-00699-2