Abstract
Introduction
Non-fermenting Gram-negative bacilli (NFGNB) other than Pseudomonas aeruginosa and Acinetobacter baumannii complex are pathogens of interest due to their ability to cause health-care associated infections and display complex drug resistance phenotypes. However, their clinical and microbiological landscape is still poorly characterized.
Methods
Observational retrospective study including all hospitalized patients presenting with a positive positive blood culture (BC) episode caused by less common NFGNB over a four-year period (January 2020–December 2023). Clinical-microbiological features and factors associated with mortality were investigated.
Results
Sixty-six less common NFGNB isolates other than Pseudomonas and Acinetobacter species causing 63 positive BC episodes were recovered from 60 patients. Positive BC episodes were predominantly sustained by Stenotrophomonas maltophilia (49.2%) followed by Achromobacter species (15.9%) that exhibited the most complex resistance phenotype. Positive BC episodes had bloodstream infection criteria in 95.2% of cases (60 out 63), being intravascular device (30.2%) and respiratory tract (19.1%) the main sources of infection. Fourteen-day, 30-day, and in-hospital mortality rates were 6.4%, 9.5%, and 15.9%, respectively. The longer time from admission to the positive BC episode, older age, diabetes, admission due to sepsis, and higher Charlson Comorbidity Index were identified as the main predictors of in-hospital mortality.
Conclusions
Positive BC episodes sustained by NFGNB other than Pseudomonas and Acinetobacter species were predominantly sustained by Stenotrophomonas maltophilia and Achromobacter species, having bloodstream infection criteria in the vast majority of cases. Factors that have emerged to be associated with mortality highlighted how these species may have more room in prolonged hospitalisation and at the end of life for patients with chronic organ diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gram-negative bacteria bloodstream infection (BSI) is a serious clinical condition associated with notable mortality and morbidity rates, especially among immunocompromised and elderly patients [1, 2]. The course of infection is heavily influenced by various microbiological and clinical issues as the type of pathogen and burden of drug resistance [3], patients conditions and rapidity and appropriateness of diagnosis and treatment [4, 5]. Among non-fermenting Gram-negative bacilli (NFGNB) [6], Pseudomonas aeruginosa and Acinetobacter baumannii complex are the most frequently isolated pathogens [1, 2]. Given their high burden of antimicrobial resistance [7] they have been placed on the World Health Organisation’s critical priority list for the development of new antibiotics [8]. These two species have therefore been the target of several surveillance [9], clinical [10,11,12] and microbiological studies [13,14,15]. Interest in them even increased during the SARS-CoV-2 pandemic due to their frequent detection especially in patients with prolonged time of invasive ventilation and hospitalisation [16, 17]. Among NFGNB, however, there are other bacteria such as Stenotrophomonas, Achromobacter, Ochrobactrum, Burkholderia, Aeromonas, Roseomonas, Elizabethkingia, Chryseobacterium, Alcaligenes, Ralstonia, Cupriavidus, Sphingomonas, Rhizobium, Empedobacter, Brevundimonas and other species that are less frequently diagnosed but of interest due to their ability to display complex drug resistance phenotypes [18,19,20,21,22,23]. These organisms are widely distributed in the environment, thriving in soil and water supplies [18]. They initially aroused attention due to their ability to colonise and infect cystic fibrosis [24,25,26] and chronic lung disease patients [27]. They have then emerged as healthcare-associated opportunistic pathogens [28, 29], mainly causing pneumonia and/or BSI [6] and nosocomial outbreaks [30,31,32,33], relying on their ability of colonizing medical devices and therapeutic equipment [31, 33].
Risk factors for infection include older age, malignancy, immunodepression, chronic respiratory disease, presence of intravascular device or drain tube, prolonged antibiotic use and hospital length of stay. Stenotrophomonas maltophilia is the most detected aetiology [6]. The mortality rate of infections caused by these species is reported to vary greatly depending on the type of infection, pathogen, and patient involved [6].
In recent years, the diagnostic accuracy and frequency of diagnosis of NFGNB other than Pseudomonas and Acinetobacter species have certainly increased, but their pathogenic potential remains a topic yet to be explored. The clinical significance of these species detection from blood cultures (BCs) sometimes can be unclear, especially in case of polymicrobial infections or with a low positive/overall BC samples ratio. However, the treatment of associated infections presents a real challenge, as these organisms, which are difficult to eradicate from healthcare facilities, often exhibit a complex resistance phenotype through the production of β-lactamases and mechanisms favouring drug efflux [18, 34]. This might result in a high rate of empirical therapy misuse and widespread antibiotic consumption.
EUCAST has also recently introduced clinical breakpoints for Stenotrophomonas maltophilia, Aeromonas and Achromobacter species [35], but therapeutic recommendations of the associated infections are only partially present in the most widely consulted guidelines [36].
We conducted this four-year monocentric study with the objective of investigating the factors associated with mortality in a cohort of patients who presented with a positive BC episode caused by NFGNB other than Pseudomonas and Acinetobacter species, contributing to the clinical and microbiological characterization of these infections.
Methods
Study design
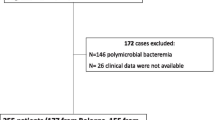
In this observational retrospective four-year study (January 2020–December 2023), we included all NFGNB isolates other than Pseudomonas and Acinetobacter species recovered from positive BCs of patients admitted at the “Città della Scienza e della Salute di Torino”, a 1900-bed tertiary referral hospital in Turin, Italy. Duplicate isolates obtained within a 20-day interval from the same patient were considered as part of a single positive BC episode and therefore excluded from the analysis. The electronic medical records of patients who presented with a positive BC episode caused by NFGNB isolates other than Pseudomonas and Acinetobacter species were retrospectively reviewed. Clinical and microbiological characteristics, and factors associated with in-hospital mortality were investigated.
Microbiological diagnostics
The BACT/ALERT FA and FN Plus BC bottles (bioMérieux, Marcy l’Ètoile, France) were incubated in the BACT/ALERT Virtuo (bioMérieux, Marcy l’Ètoile, France). Positive BCs were subjected to Gram staining and subculture on MacConkey and Blood agar media. Bacterial species identification was performed on overnight subcultures by using matrix-assisted laser desorption ionization–time of flight mass spectrometry (MALDI-TOF MS, Bruker DALTONIK GmbH, Bre-men, Germany). Antimicrobial susceptibility testing was performed through a micro-dilution method (Panel NMDR on automated Microscan WalkAway 96 Plus System, Beckman Coulter, Nyon, Switzerland). Cefiderocol susceptibility testing was carried out by disc diffusion method. Antimicrobial susceptibility testing results were interpreted according to the current EUCAST clinical breakpoints (v. 14.0) [35, 37].
Statistical analysis
Descriptive data are shown as relative (%) and absolute (n) frequencies for categorical data and median and interquartile range (IQR) for continuous variables. χ2 test or Fisher’s exact test were employed to assess the association between binary variables and outcomes. For continuous variables, the Mann-Whitney U test was used to com-pare distributions between groups based on outcome status. XGBoost was used as an explanatory model to rank and identify relative feature importance, using SHAP values as a proxy for feature importance measured at the local data point level. SHAP values are reported as log odds. Analyses have been carried out in Python 3.10.
Results
Sixty-six NFGNB isolates other than Pseudomonas and Acinetobacter species causing 63 positive BC episodes (overall prevalence of 1.6% among Gram-negative bacteria) were recovered from 60 patients. Patients had a median age of 65 years [51.5–74.5], were predominantly male (60.3%) and admitted in medical wards (46%), with a median Charlson comorbidity index estimating a 53% probability of surviving in the next ten years (Table 1).
Among the characteristics of the patients investigated, presence of a long-term intravascular device (52.4%) and cardiovascular disease (71.4%) followed by having been treated with antibiotic therapy in the previous seven days (47.6%), being colonized by multidrug resistant bacteria (28.6%), and neoplasms (35%) were the most prevalent. Patients were predominantly admitted due to sepsis (27%), surgery (25.4%), and trauma (20.6%). The median time to positive BC episode from admission was 17 days [2–34.5] and 68.3% of patients had at least 50% positive BC bottles out of the total number of BC bottles processed. Almost half (41.3%, n = 26) of the BC samples were polymicrobial mainly with other Gram-negative bacteria (57.7%, n = 15). Positive BC episodes were predominantly sustained by Stenotrophomonas maltophilia (49.2%) followed by Achromobacter (15.9%), Ochrobactrum (9.5%), Aeromonas (9.5%), and Burkholderia species (7.9%, with one imported case of melioidosis). Other species accounted for 14.3% and included Rhizobium radiobacter, Chryseobacterium arthrosphaerae, Roseomonas mucosa, Empedobacter falsenii, Elizabethkingia anophelis, and Brevundimonas diminuita. Positive BC episodes had BSI criteria in 95.2% of cases (60 out 63), being intravascular device (30.2%) and respiratory tract (19.1%) the main sources of infection. Patients suffered from BSI had a median Pitt Bacteremia score of one [0–2], presented with neutropenia in 9.5%, and required ICU admission in 14.3% of the cases. The majority of patients (55.6%) were treated with active antibiotic therapy within 48 h from positive BC episode detection. Targeted antibacterial therapy was carried out in equal proportions between monotherapy and combination (47.6%). The most frequently used antibiotic regimes were those that included meropenem (25.4%), piperacillin/tazobactam (23.8%), fluoroquinolones (22.2%), and trimethoprim/sulfamethoxazole (17.5%). Regarding complications, four patients (6.4%) reoccurred with a positive BC episode caused by the same organism at least 14 days after the first one. Regarding outcomes, 14-day, 30-day, and in-hospital mortality rates were 6.4%, 9.5%, and 15.9%, respectively. The median length of stay was 41 days [19.5–72].
Antimicrobial susceptibility profiles of NFGNB isolates other than Pseudomonas and Acinetobacter species included in the study were reported in Table 2. Stenotrophomonas maltophilia isolates displayed over 90% susceptibility only to cefiderocol and trimethoprim/sulfamethoxazole. Achromobacter species showed high rates of resistance towards all the antibiotics tested and high values of inhibition zone diameter with cefiderocol (range 35–39 mm). Aeromonas species displayed susceptibility to third- and fourth-generation cephalosporins, fluoroquinolones and trimethoprim/sulfamethoxazole. Ochrobactrum anthropi displayed high susceptibility to carbapenems as well as to meropenem in Burkholderia species. High values of the diameter of the zone of inhibition with cefiderocol (range 36–40 mm) were also observed in Burkholderia species.
Patients admitted due to trauma had more episodes of positive BC sustained by at least ≥ 50% of the BC bottles positive (27.9% vs. 5%, p = 0.047, Table 3). Less frequent species included in the ‘other’ group were more detected in patients with less than 50% of positive BC bottles (30% vs. 7%, p = 0.023). No more statistically significant differences in terms of patient characteristics, microbiological findings, source of infection, severity of bacteremia, antibiotic management and outcomes were observed.
Comparison of the clinical characteristics of the patients who died during admission vs. those who survived (Table 4) showed non-survivors suffering more from diabetes (p = 0.025), having a higher Charlson Comorbidity index (p = 0.036), having been treated with antibiotic therapy in the previous seven days (p = 0.038), and having a longer time from admission to positive BC episode (p = 0.003) than survivors. No more statistically significant differences in terms of patient characteristics, microbiological findings, reason for admission, source of infection, severity of bacteremia, antibiotic management and complications were observed.
The XGBoost model used to rank features based on their relative importance based on their contribution towards mortality risk patient stratification suggested the most informative features to be the time from admission to the positive BC episode (a high cardinality feature, which inherently increases its importance), older age, diabetes, admission due to sepsis, higher Charlson Comorbidity Index, being treated with combination therapy, and being treated with a meropenem-including regimen. Additionally, the model underscored that male patients and those colonized by multidrug-resistant bacteria were less likely to die compared to female patients and non-carriers under surveillance, respectively (Fig. 1).
XGBoost explanatory model to rank and identify relative feature importance of factors associated with in-hospital mortality. (a) Beeswarm Plot of SHAP Values: Beeswarm plot illustrating the distribution of SHAP (SHapley Additive exPlanations) values for each feature in the dataset. Each dot represents a feature value for a specific patient, with the position along the x-axis indicating the magnitude of the SHAP value. The color of each dot indicates the corresponding feature value, providing insight into the relationship between feature values and their impact on model predictions. Features with wider distributions and greater dispersion of SHAP values suggest higher variability and importance in the model’s decision-making process. Redder dots on the right side of the plot indicate that being positive for that feature or experiencing higher values on it increases the predicted probability of death. Redder dots on the left side indicate the opposite (lower chances of dying). (b) Heatmap of SHAP Values: Heatmap illustrating the SHAP (SHapley Additive exPlanations) values for the top features impacting the model’s mortality prediction scores. Each row corresponds to a feature in the dataset, and each column represents a patient sample. Patient samples are ordered using hierarchical clustering by their explanation similarity, resulting in samples with closer model outputs for the same reason getting grouped together. The color intensity indicates the magnitude and direction of the feature’s impact on the model output: red indicates positive impact (increasing the predicted likelihood of death), while blue indicates negative impact (decreasing the predicted likelihood of death). A feature’s importance can be inferred from the range and variability of its SHAP values across samples. Features with higher absolute SHAP values exert a greater influence on the model predictions. Only the top nine features are herein individually depicted. The output of the model is shown above the heatmap matrix as a line plot centered around the explanation’s base value and the global importance of each model input shown as a bar plot on the right hand side of the plot. (c) Force plots with individual patient examples, breaking down the contribution of each feature to the prediction of a given patient (three random patients with a high/low predicted score shown). Scores are on a log odds scale. Probabilities can be easily inferred as probability = exp(log-odds)/(1 + exp(log-odds))
Discussion
This study offers a contemporary insight into the clinical–microbiological features of positive BC episodes sustained by NFGNB other than Pseudomonas and Acinetobacter species in a cohort of patients admitted in a reference center of Northern Italy encompassing all major medical and surgical specialties and with multiple challenges in the area of antibiotic resistance [38]. Its findings revealed that positive BC episodes sustained by NFGNB other than Pseudomonas and Acinetobacter species were polymicrobial and microbiologically significant in a remarkable proportion of the samples. Stenotrophomonas maltophilia was the most detected species and, together with Achromobacter species, exhibited the most complex resistance phenotype. Clinically, positive BC episodes were more frequent in patients with a long-term intravascular device and had BSI criteria in the vast majority of cases. In contrast, the degree of severity of bacteremia was quite low, as were the associated mortality rates. Time from admission to the positive BC episode, older age, diabetes, admission due to sepsis, higher Charlson Comorbidity Index, being treated with combination therapy and meropenem-inclusive regimen emerged as factors associated with in-hospital mortality.
Knowledge of the clinical significance of NFGNB other than Pseudomonas and Acinetobacter species is currently very limited [6]. Our study only partially assessed the impact of these species given the high proportion of polymicrobial samples. However, our results reported a high correspondence between positive BC episode, ≥ 50% positive/overall BC samples ratio, BSI criteria and targeted treatment prescription, adding some evidence in favor of the likely pathogenic potential of these species.
Our study also confirmed the epidemiological and clinical relevance of Stenotrophomonas maltophilia within the less common NFGNB [6]. A substantial literature already exists on this species and associated infections [18, 39,40,41,42,43,44,45,46,47] so much so that it is the only one to have been included in the Infectious Diseases Society of America treatment guidelines [36]. Our study also highlighted that resistance to sulfamethoxazole/trimethoprim and cefiderocol remains uncommon as already highlighted in recent studies [13, 48].
Despite the limited sample size, our study showed the complex phenotype of Achromobacter species exhibiting low susceptibility to piperacillin/tazobactam, third-generation cephalosporins, carbapenems, and fluoroquinolones. These findings are not consistent with the results of a Spanish study on patients suffering from Achromobacter xylosoxidans bacteremia that showed high susceptibility to meropenem using EUCAST breakpoints for Pseudomonas aeruginosa [49], highlighting Achromobacter potential for innate resistance to all antibiotics [18]. Of note, high values of inhibition zone diameter with cefiderocol were observed among the isolates included in our study, as also previously described [14]. This might highlight cefiderocol as promising treatment of severe Achromobacter species infections, although clinical evidence on in vivo activity is still limited.
The opportunistic pathogenic nature of the less common NFGNB is highlighted in the literature by the fact that they mainly cause nosocomial infections in an increasingly common population with risk factors such as neoplasia or chronic organ disease, prolonged hospitalizations and the need for systemic therapies, including antibiotics, through long-term intravascular devices [18]. This is consistent with the results of our study which identified the presence of a long-term intravascular device as the most frequent clinical feature among patients and the main source of BSI. On the other hand, although our study showed quite low BSI severity indices and consequently low mortality rates, evidence available so far shows different data according to pathogen and cohort of patients considered [6]. Mortality rates among adult patients suffering from Stenotrophomonas maltophilia BSIs ranged from 32 to 54.8% [50,51,52], while for those sustained by Achromobacter species from 20 to 27% [53, 54]. Similar rates have been reported in Elizabethkingia species BSIs [55,56,57], while lower rates have been reported in Chryseobacterium species [58].
Perhaps not surprising, in our study patients who did not survive admission were older, suffered from more baseline comorbidities, were admitted due to sepsis, and experienced both longer time from admission to the positive BC episode and more broad-spectrum antibiotic therapy. Therefore, patient’s general condition prevailed over etiology in patients suffering from less common NFGNB BSIs. The relevance of comorbidities in predicting mortality was well highlighted in an Australian population study over the period 2000–2019 [53]. In a recent meta-analysis on patients with Stenotrophomonas maltophilia bloodstream infection, poor outcomes were associated with infection severity (ICU admission, septic shock, need for mechanical ventilation), comorbidities (indwelling central venous catheter, neutropenia, hematological neoplasms, chronic kidney disease) and antibiotic prescription (inappropriate antimicrobial therapy and prior antibiotic use) [59]. However, our finding differs significantly from a recent multicenter study conducted in Northern Italy on patients suffering from NFGNB BSI (including Pseudomonas aeruginosa and Acinetobacter baumannii complex) that identified older age, septic shock and Acinetobacter baumannii complex etiology as predictors of 30-day mortality [11]. The strength of this study is the collection of data from a surveillance study on a group of bacteria sporadically reported in the literature and investigating their pathogenic potential. Some limitations should be also acknowledged, including its retrospective nature with possible confounders and potential bias not considered and the fact that it was conducted in a single center. The narrow nature of our findings, due to the limited sample size, does not allow generalized conclusions to be drawn.
In conclusion, this study investigated the clinical and microbiological findings of positive BC episodes caused by NFGNB other than Pseudomonas and Acinetobacter species. Positive BC episodes were predominantly sustained by Stenotrophomonas maltophilia and Achromobacter species, having BSI criteria in the vast majority of cases. Achromobacter species isolates showed the most complex resistance phenotype and from the in vitro results, cefiderocol appeared to be a possible option for treating infections caused by these multidrug resistance strains. Long-term intravascular device and respiratory tract were the main sources of infection. No differences in patient comorbidities, infection severity and outcomes were observed on the basis of the percentage of positive BC samples, providing an argument in favor of those who consider these species to have substantial pathogenic potential. The longer time from admission to positive BC episode, older age, diabetes, admission due to sepsis, higher Charlson Comorbidity Index, being treated with combination therapy and meropenem-including regimen emerged as the strongest predictors of in-hospital mortality. This might highlight how these species may have more room in prolonged hospitalisation and at the end of life for patients with chronic organ diseases. Further studies are needed to validate our results, notwithstanding the need for continuous surveillance of these species and their antimicrobial susceptibility profiles.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Kern WV, Rieg S. Burden of bacterial bloodstream infection-a brief update on epidemiology and significance of multi-drug-resistant pathogens. Clin Microbiol Infect. 2020;26:151–7. https://doi.org/10.1016/j.cmi.2019.10.031.
Holmes CL, Anderson MT, Mobley HLT, Bachman MA. Pathogenesis of Gram-negative bacteremia. Clin Microbiol Rev. 2021;34:e00234–20. https://doi.org/10.1128/CMR.00234-20.
Hassoun-Kheir N, Guedes M, Ngo Nsoga MT, Argante L, Arieti F, Gladstone BP, et al. A systematic review on the excess health risk of antibiotic-resistant bloodstream infections for six key pathogens in Europe. Clin Microbiol Infect. 2024;30(Suppl 1):S14–25. https://doi.org/10.1016/j.cmi.2023.09.001.
Kang CI, Kim SH, Park WB, Lee KD, Kim HB, Kim EC, et al. Bloodstream infections caused by antibiotic-resistant gram-negative bacilli: risk factors for mortality and impact of inappropriate initial antimicrobial therapy on outcome. Antimicrob Agents Chemother. 2005;49:760–6. https://doi.org/10.1128/AAC.49.2.760-766.2005.
Zasowski EJ, Bassetti M, Blasi F, Goossens H, Rello J, Sotgiu G, et al. A systematic review of the effect of delayed appropriate antibiotic treatment on the outcomes of patients with severe bacterial infections. Chest. 2020;158:929–38. https://doi.org/10.1016/j.chest.2020.03.087.
Koulenti D, Vandana KE, Rello J. Current viewpoint on the epidemiology of nonfermenting Gram-negative bacterial strains. Curr Opin Infect Dis. 2023;36:545–54. https://doi.org/10.1097/QCO.0000000000000977.
Gniadek TJ, Carroll KC, Simner PJ. Carbapenem-resistant non-glucose-fermenting gram-negative bacilli: the missing piece to the puzzle. J Clin Microbiol. 2016;54:1700–10. https://doi.org/10.1128/JCM.03264-15.
World Health Organization. Prioritization of pathogens to guide discovery, research and development of new antibiotics for drug-resistant bacterial infections, including tuberculosis. Essent Med Health Products 2017. Available on line: https://www.who.int/publications/i/item/WHO-EMP-IAU-2017.12 (accessed on 21 May 2024).
European Centre for Disease Prevention and Control. Antimicrobial resistance surveillance in Europe 2023 – 2021 data. Available on line: https://www.ecdc.europa.eu/sites/default/files/documents/Antimicrobial%20resistance%20surveillance%20in%20Europe%202023%20-%202021%20data.pdf (accessed on 15 May 2024).
Lu L, Xu C, Tang Y, Wang L, Cheng Q, Chen X, et al. The threat of Carbapenem-Resistant Gram-negative Bacteria in patients with hematological malignancies: unignorable respiratory non-fermentative Bacteria-derived blood-stream infections. Infect Drug Resist. 2022;15:2901–14. https://doi.org/10.2147/IDR.S359833.
Pascale R, Corcione S, Bussini L, Pancaldi L, Giacobbe DR, Ambretti S, et al. Non-fermentative gram-negative bloodstream infection in northern Italy: a multicenter cohort study. BMC Infect Dis. 2021;21:806. https://doi.org/10.1186/s12879-021-06496-8.
Montrucchio G, Balzani E, Sales G, Vaninetti A, Grillo F, Trompeo AC, et al. Multidrug-resistant pathogens and ventilator-associated pneumonia in critically ill COVID-19 and non-COVID-19 patients: a prospective observational monocentric comparative study. Respir Res. 2024;25:168. https://doi.org/10.1186/s12931-024-02779-1.
Huang YS, Chuang YC, Chen PY, Chou PC, Wang JT. In vitro activity of cefiderocol and comparator antibiotics against mul-tidrug-resistant non-fermenting gram-negative bacilli. JAC Antimicrob Resist. 2024;6:dlae006. https://doi.org/10.1093/jacamr/dlae006.
Bianco G, Boattini M, Comini S, Gaibani P, Cavallo R, Costa C. Performance evaluation of Bruker UMIC® microdilution panel and disc diffusion to determine cefiderocol susceptibility in Enterobacterales, Acinetobacter baumannii, Pseudomonas aeruginosa, Stenotrophomonas maltophilia, Achromobacter xylosoxidans and Burkolderia species. Eur J Clin Microbiol Infect Dis. 2024;43:559–66. https://doi.org/10.1007/s10096-024-04745-7.
Bianco G, Boattini M, Comini S, Banche G, Cavallo R, Costa C. Disc diffusion and ComASP® Cefiderocol Microdilution Panel to overcome the challenge of Cefiderocol susceptibility testing in Clinical Laboratory Routine. Antibiotics. 2023;12:604. https://doi.org/10.3390/antibiotics12030604.
O’Toole RF. The interface between COVID-19 and bacterial healthcare-associated infections. Clin Microbiol Infect. 2021;27:1772–6. https://doi.org/10.1016/j.cmi.2021.06.001.
Casale R, Bianco G, Bastos P, Comini S, Corcione S, Boattini M et al. Prevalence and impact on mortality of colonization and super-infection by carbapenem-resistant gram-negative organisms in COVID-19 hospitalized patients. viruses. 2023;15:1934. https://doi.org/10.3390/v15091934.
Spencer HK, Spitznogle SL, Borjan J, Aitken SL. An overview of the treatment of less common non-lactose-fermenting gram-negative bacteria. Pharmacotherapy 2020;40:936 – 51. https://doi.org/10.1002/phar.2447.
Chawla K, Vishwanath S, Munim FC. Nonfermenting gram-negative bacilli other than pseudomonas aeruginosa and aci-netobacter spp. Causing respiratory tract infections in a Tertiary Care Center. J Glob Infect Dis. 2013;5:144–8. https://doi.org/10.4103/0974-777X.121996.
Rattanaumpawan P, Ussavasodhi P, Kiratisin P, Aswapokee N. Epidemiology of bacteremia caused by uncommon non-fermentative gram-negative bacteria. BMC Infect Dis. 2013;13:167. https://doi.org/10.1186/1471-2334-13-167.
Asaad AM, Al-Ayed MS, Qureshi MA. Emergence of unusual nonfermenting gram-negative nosocomial pathogens in a Saudi hospital. Jpn J Infect Dis. 2013;66:507–11. https://doi.org/10.7883/yoken.66.507.
Jacquier H, Le Monnier A, Carbonnelle E, Corvec S, Illiaquer M, Bille E, et al. In vitro antimicrobial activity of last-resort antibiotics against unusual nonfermenting gram-negative bacilli clinical isolates. Microb Drug Resist. 2012;18:396–401. https://doi.org/10.1089/mdr.2011.0195.
Parte AC. LPSN—list of prokaryotic names with standing in nomenclature. Nucleic Acids Res. 2014;42(Database issue):D613–6. https://doi.org/10.1093/nar/gkt1111.
Lobo LJ, Tulu Z, Aris RM, Noone PG. Pan-resistant Achromobacter xylosoxidans and Stenotrophomonas maltophilia infection in cystic fibrosis does not reduce Survival after Lung Transplantation. Transplantation. 2015;99:2196–202. https://doi.org/10.1097/TP.0000000000000709.
Díez-Aguilar M, Ekkelenkamp M, Morosini MI, Merino I, de Dios Caballero J, Jones M, et al. Antimicrobial susceptibility of non-fermenting gram-negative pathogens isolated from cystic fibrosis patients. Int J Antimicrob Agents. 2019;53:84–8. https://doi.org/10.1016/j.ijantimicag.2018.09.001.
Mathy V, Grohs P, Compain F. In vitro activity of β-lactams in combination with avibactam against multidrug-resistant Pseudomonas aeruginosa, Stenotrophomonas maltophilia and Achromobacter xylosoxidans isolates from patients with cystic fibrosis. J Med Microbiol. 2018;67:1217–20. https://doi.org/10.1099/jmm.0.000801.
Farfour E, Roux A, Sage E, Revillet H, Vasse M, Vallée A. Rarely encountered Gram-negative rods and lung transplant recipients: a narrative review. Microorganisms. 2023;11:1468. https://doi.org/10.3390/microorganisms11061468.
Bianco G, Boattini M, Audisio E, Cavallo R, Costa C. Septic shock due to meropenem- and colistin-resistant Cupriavidus pauculus. J Hosp Infect. 2018;99:364–5. https://doi.org/10.1016/j.jhin.2018.03.025.
Boattini M, Bianco G, Biancone L, Cavallo R, Costa C. Ralstonia mannitolilytica bacteraemia: a case report and literature review. Infez Med. 2018;26:374–8.
Shaban RZ, Sotomayor-Castillo C, Nahidi S, Li C, Macbeth D, Mitchell BG, Russo PL. Global burden, point sources, and out-break management of healthcare-associated Burkholderia cepacia infections: an integrative review. Infect Control Hosp Epidemiol. 2020;41:777–83. https://doi.org/10.1017/ice.2020.184.
Menekşe Ş, Tanrıverdi ES, Oğuş H, Altınay E, Kaya Ç, Çağlayan E, et al. Stenotrophomonas maltophilia outbreak with a commercial blood gas injector as the culprit and interventions for source and prevention: a possible passage between patient and ECMO water heater device. Am J Infect Control. 2023;51:533–8. https://doi.org/10.1016/j.ajic.2022.07.012.
Yoon SH, Kim H, Lim SM, Kang JM. Nosocomial outbreak of Achromobacter spp. bacteremia due to germicide contamination: a systematic review. Eur Rev Med Pharmacol Sci. 2022;26:6374–81. https://doi.org/10.26355/eurrev_202209_29664.
Inkster T, Peters C, Wafer T, Holloway D, Makin T. Investigation and control of an outbreak due to a contaminated hospital water system, identified following a rare case of Cupriavidus pauculus bacteraemia. J Hosp Infect. 2021;111:53–64. https://doi.org/10.1016/j.jhin.2021.02.001.
Abbott IJ, Peleg AY, Stenotrophomonas. Achromobacter, and nonmelioid Burkholderia species: antimicrobial resistance and therapeutic strategies. Semin Respir Crit Care Med. 2015;36:99–110. https://doi.org/10.1055/s-0034-1396929.
European Committee on Antimicrobial Susceptibility Testing. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_14.0_Breakpoint_Tables.pdf (accessed on 7 May 2024).
Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America 2023 Guidance on the treatment of Antimicrobial resistant gram-negative infections. Clin Infect Dis. 2023;ciad428. https://doi.org/10.1093/cid/ciad428.
European Committee on Antimicrobial Susceptibility Testing. Available on line: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Guidance_documents/When_there_are_no_breakpoints_2024-02-29.pdf (accessed on 7 May 2024).
Bianco G, Boattini M, Comini S, Iannaccone M, Casale R, Allizond V, et al. Activity of ceftolozane-tazobactam, ceftazidime-avibactam, meropenem-vaborbactam, cefiderocol and comparators against Gram-negative organisms causing bloodstream infections in Northern Italy (2019–2021): emergence of complex resistance phenotypes. J Chemother. 2022;34:302–10. https://doi.org/10.1080/1120009X.2022.2031471.
Chang YT, Lin CY, Chen YH, Hsueh PR. Update on infections caused by Stenotrophomonas maltophilia with particular attention to resistance mechanisms and therapeutic options. Front Microbiol. 2015;6:893. https://doi.org/10.3389/fmicb.2015.00893.
Majumdar R, Karthikeyan H, Senthilnathan V, Sugumar S. Review on Stenotrophomonas maltophilia: an emerging Multidrug- resistant opportunistic Pathogen. Recent Pat Biotechnol. 2022;16:329–54. https://doi.org/10.2174/1872208316666220512121205.
Lai JJ, Siu LK, Chang FY, Lin JC, Yu CM, Wu RX. Appropriate antibiotic therapy is a predictor of outcome in patients with Stenotrophomonas maltophilia blood stream infection in the intensive care unit. J Microbiol Immunol Infect. 2023;56:624–33. https://doi.org/10.1016/j.jmii.2023.03.001.
Aysert-Yıldız P, Yıldız Y, Habibi H, Eser S, Özgen-Top Ö, Özger HS, et al. Stenotrophomonas maltophilia bacteremia: from diagnosis to treatment. Infect Dis Clin Microbiol. 2022;4:258–67. https://doi.org/10.36519/idcm.2022.187.
Mojica MF, Humphries R, Lipuma JJ, Mathers AJ, Rao GG, Shelburne SA, et al. Clinical chal-lenges treating Stenotrophomonas maltophilia infections: an update. JAC Antimicrob Resist. 2022;4:dlac040. https://doi.org/10.1093/jacamr/dlac040.
Lupia T, Carnevale-Schianca F, Vita D, Busca A, Caravelli D, Crisà E, et al. Sten-Otrophomonas maltophilia infections in Haematological Malignancies and hematopoietic stem cell transplantation: a Case Series including Cefiderocol-based regimens. Medicina. 2024;60:88. https://doi.org/10.3390/medicina60010088.
Gil-Gil T, Martínez JL, Blanco P. Mechanisms of antimicrobial resistance in Stenotrophomonas maltophilia: a review of current knowledge. Expert Rev Anti Infect Ther. 2020;18:335–47. https://doi.org/10.1080/14787210.2020.1730178.
Banar M, Sattari-Maraji A, Bayatinejad G, Ebrahimi E, Jabalameli L, Beigverdi R, et al. Global prevalence and antibiotic resistance in clinical isolates of Stenotrophomonas maltophilia: a systematic review and meta-analysis. Front Med. 2023;10:1163439. https://doi.org/10.3389/fmed.2023.1163439.
Al-Jasser AM. Stenotrophomonas maltophilia resistant to trimethoprim-sulfamethoxazole: an increasing problem. Ann Clin Microbiol Antimicrob. 2006;5:23. https://doi.org/10.1186/1476-0711-5-23.
Karlowsky JA, Hackel MA, Takemura M, Yamano Y, Echols R, Sahm DF. Vitro susceptibility of Gram-negative pathogens to Cefiderocol in five consecutive annual multinational SIDERO-WT Surveillance studies, 2014 to 2019. Antimicrob Agents Chemother. 2022;66:e0199021. https://doi.org/10.1128/AAC.01990-21.
Pérez Barragán E, Sandino Pérez J, Corbella L, Orellana MA, Fernández-Ruiz M. Achromobacter xylosoxidans bacteremia: clinical and microbiological features in a 10-year case series. Rev Esp Quimioter. 2018;31:268–73.
Dimopoulos G, Garnacho-Montero J, Paramythiotou E, Gutierrez-Pizarraya A, Gogos C, Adriansen-Pérez M, et al. Upraising Stenotrophomonas maltophilia in critically ill patients: a New. Enemy? Diagnostics. 2023;13:1106. https://doi.org/10.3390/diagnostics13061106.
Jacob A, Iyadurai R, Punitha JV, Chacko B, Jasmine S, Bharathy M, et al. Stenotrophomonas isolates in a tertiary care centre in South India. Indian J Med Microbiol. 2022;40:46–50. https://doi.org/10.1016/j.ijmmb.2021.11.004.
Kanchanasuwan S, Rongmuang J, Siripaitoon P, Kositpantawong N, Charoenmak B, Hortiwakul T, et al. Clinical characteristics, outcomes, and risk factors for mortality in patients with Stenotrophomonas maltophilia bacteremia. J Clin Med. 2022;11:3085. https://doi.org/10.3390/jcm11113085.
Isler B, Paterson DL, Harris PNA, Ling W, Edwards F, Rickard CM, et al. Achromobacter species: an Emerging cause of community-onset bloodstream infections. Microorganisms. 2022;10:1449. https://doi.org/10.3390/microorganisms10071449.
Crone CG, Rezahosseini O, Schultz HHL, Qvist T, Johansen HK, Nielsen SD, et al. Achromobacter spp. in a cohort of non-selected pre- and Post-lung Transplant recipients. Pathogens. 2022;11:181. https://doi.org/10.3390/pathogens11020181.
Ma S, Gong Y, Luo X, Peng Y, Zhang C, Zhang X, et al. Emerging prevalence and clinical features of Elizabethkingia meningoseptica infection in Southwest China: a 9-Year retrospective study and systematic review. Infect Drug Resist. 2023;16:531–43. https://doi.org/10.2147/IDR.S397051.
Sarathi S, Behera B, Mahapatra A, Mohapatra S, Jena J, Nayak S. Microbiological characterization and clinical facets of Elizabethkingia Bloodstream Infections in a Tertiary Care Hospital of Eastern India. Infect Drug Resist. 2023;16:3257–67. https://doi.org/10.2147/IDR.S409121.
Umair A, Nasir N. Clinical features and outcomes of critically ill patients with Elizabethkingia meningoseptica: an emerging pathogen. Acute Crit Care. 2021;36:256–61. https://doi.org/10.4266/acc.2020.01158.
Chang J, Kim S, Kwak YG, Um TH, Cho CR, Song JE. Clinical and microbiological characteristics of Chryseobacterium indologenes Bacteremia: a 20-Year experience in a single University Hospital. Infect Chemother. 2023;55:322–7. https://doi.org/10.3947/ic.2022.0133.
Huang C, Lin L, Kuo S. Risk factors for mortality in Stenotrophomonas maltophilia bacteremia - a meta-analysis. Infect Dis. 2024;56:335–47. https://doi.org/10.1080/23744235.2024.2324365.
Funding
Open access funding provided by Università degli Studi di Torino within the CRUI-CARE Agreement. This research was supported by EU funding within the MUR PNRR Extended Partnership initiative on Emerging Infectious Diseases (Project no. PE00000007, INF-ACT).
Author information
Authors and Affiliations
Contributions
G.B. and M.B. designed the study; R.C, S.C. (Sara Comini), S.C. (Silvia Corcione) acquired data; M.B. and P.B. analyzed and interpreted data; R.C. and M.B. wrote the paper; F.G.D.R. and C.C. supervised the study; all authors revised the article critically. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of A.O.U. Città della Salute e della Scienza di Torino-A.O. Ordine Mauriziano-A.S.L. Città di Torino (protocol code 0048443 on 29 April 2022).
Informed consent
Informed consent was waived due to the retrospective nature of the study.
Competing interests
The authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Casale, R., Boattini, M., Comini, S. et al. Clinical and microbiological features of positive blood culture episodes caused by non-fermenting gram-negative bacilli other than Pseudomonas and Acinetobacter species (2020–2023). Infection (2024). https://doi.org/10.1007/s15010-024-02342-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s15010-024-02342-6