Abstract
Purpose
Especially in oral and maxillofacial surgery, where procedures involving the aero-digestive tract considered clean contaminated, surgical site infections (SSI) represent a severe health care burden. To improve implementation and methodological standard, an upgrade of the existing S1 guideline to a consensus-guided S3 guideline was initiated by the Association of the Scientific Medical Societies in Germany (Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V., AWMF, register number 067/009) and 25 collaborating medical societies.
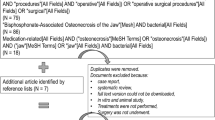
Methods
A systematic literature search based on the Scottish Intercollegiate GL Network (SIGN)-search string for the guideline “Antibiotic prophylaxis in surgery” from 2014 was performed and equivalent exclusion/inclusion criteria were applied. An additional hand search provided latest evidence.
Results
In total, 80 clinical trials, retrospective studies, reviews, and meta-analysis were analyzed. For orthognathic surgery, prolonged antibiotic regimen may reduce risk for SSI but there is lack of evidence for the effects of short- vs. long-term therapy. For maxillofacial traumatology, antibiotic prophylaxis might reduce SSI but prolonged postoperative dosing shows no benefit. For clean-contaminated oncological interventions, anti-infectious therapy for 24 h only can reduce SSI; patients may not benefit from prolonged regimen. In contrast, for dentoalveolar procedures such as implantology or third molar removal, literature reveals ambivalent results.
Conclusion
In summary, consensus process of the planned S3 guideline is much in need to transfer the indecisive results for antibiotic prophylaxis in dentoalveolar surgery in clinical praxis and encourage adherence to guidelines.

Similar content being viewed by others
References
Mercuri LG. Avoiding and managing temporomandibular joint total joint replacement surgical site infections. J Oral Maxillofac Surg. 2012;70:2280–9. https://doi.org/10.1016/j.joms.2012.06.174.
Saleh AM, Torres KM, Murad MH, Erwin PJ, Driscoll CL. Prophylactic perioperative antibiotic use in endoscopic sinus surgery: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2012;146:533–8. https://doi.org/10.1177/0194599811434117.
Wahab PU, Narayanan V, Nathan S, Madhulaxmi. Antibiotic prophylaxis for bilateral sagittal split osteotomies: a randomized, double-blind clinical study. Int J Oral Maxillofac Surg. 2013;42:352–5. https://doi.org/10.1016/j.ijom.2012.10.036.
SIGN SIGN. Antibiotic prophylaxis in surgery. (SIGN publication no104) 2014; 2008.
Allegranzi B, Bischoff P, de Jonge S, Kubilay NZ, Zayed B, Gomes SM, et al. New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;16:e276–87. https://doi.org/10.1016/s1473-3099(16)30398-x.
Lu Q, Xie SQ, Chen SY, Chen LJ, Qin Q. Experience of 1166 thyroidectomy without use of prophylactic antibiotic. Biomed Res Int. 2014;2014:758432. https://doi.org/10.1155/2014/758432.
Langerman A, Ham SA, Pisano J, Pariser J, Hohmann SF, Meltzer DO. Laryngectomy complications are associated with perioperative antibiotic choice. Otolaryngol Head Neck Surg. 2015;153:60–8. https://doi.org/10.1177/0194599815583641.
Berrios-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017. https://doi.org/10.1001/jamasurg.2017.0904.
Higgins JPT GS. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. In: The Cochrane Collaboration; 2011. Accessed 13 Mar 2017.
Tan SK, Lo J, Zwahlen RA. Perioperative antibiotic prophylaxis in orthognathic surgery: a systematic review and meta-analysis of clinical trials. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:19–27. https://doi.org/10.1016/j.tripleo.2010.07.015.
Oomens MA, Verlinden CR, Goey Y, Forouzanfar T. Prescribing antibiotic prophylaxis in orthognathic surgery: a systematic review. Int J Oral Maxillofac Surg. 2014;43:725–31. https://doi.org/10.1016/j.ijom.2014.01.012.
Danda AK, Ravi P. Effectiveness of postoperative antibiotics in orthognathic surgery: a meta-analysis. J Oral Maxillofac Surg. 2011;69:2650–6. https://doi.org/10.1016/j.joms.2011.02.060.
Danda AK, Wahab A, Narayanan V, Siddareddi A. Single-dose versus single-day antibiotic prophylaxis for orthognathic surgery: a prospective, randomized, double-blind clinical study. J Oral Maxillofac Surg. 2010;68:344–6. https://doi.org/10.1016/j.joms.2009.09.081.
Brignardello-Petersen R, Carrasco-Labra A, Araya I, Yanine N, Cordova Jara L, Villanueva J. Antibiotic prophylaxis for preventing infectious complications in orthognathic surgery. Cochrane Database Syst Rev. 2015;1:CD010266. https://doi.org/10.1002/14651858.cd010266.pub2.
Davis CM, Gregoire CE, Steeves TW, Demsey A. Prevalence of surgical site infections following orthognathic surgery: a retrospective cohort analysis. J Oral Maxillofac Surg. 2016;74:1199–206. https://doi.org/10.1016/j.joms.2016.01.040.
Posnick JC, Choi E, Chavda A. Surgical site infections following bimaxillary orthognathic, osseous genioplasty, and intranasal surgery: a retrospective cohort study. J Oral Maxillofac Surg. 2017;75:584–95. https://doi.org/10.1016/j.joms.2016.09.018.
Davis CM, Gregoire CE, Davis I, Steeves TW. Prevalence of surgical site infections following orthognathic surgery: a double-blind, randomized controlled trial on a 3-day versus 1-day postoperative antibiotic regimen. J Oral Maxillofac Surg. 2017;75:796–804. https://doi.org/10.1016/j.joms.2016.09.038.
Naimi-Akbar A, Hultin M, Klinge A, Klinge B, Tranaeus S, Lund B. Antibiotic prophylaxis in orthognathic surgery: a complex systematic review. PLoS ONE. 2018;13:e0191161. https://doi.org/10.1371/journal.pone.0191161.
Morris LM, Kellman RM. Are prophylactic antibiotics useful in the management of facial fractures? Laryngoscope. 2014;124:1282–4. https://doi.org/10.1002/lary.24364.
Schaller B, Soong PL, Zix J, Iizuka T, Lieger O. The role of postoperative prophylactic antibiotics in the treatment of facial fractures: a randomized, double-blind, placebo-controlled pilot clinical study. Part 2: mandibular fractures in 59 patients. Br J Oral Maxillofacial Surg. 2013;51:803–7. https://doi.org/10.1016/j.bjoms.2013.08.008.
Mottini M, Wolf R, Soong PL, Lieger O, Nakahara K, Schaller B. The role of postoperative antibiotics in facial fractures: comparing the efficacy of a 1-day versus a prolonged regimen. J Trauma Acute Care Surg. 2014;76:720–4. https://doi.org/10.1097/TA.0000000000000123.
Lauder A, Jalisi S, Spiegel J, Stram J, Devaiah A. Antibiotic prophylaxis in the management of complex midface and frontal sinus trauma. Laryngoscope. 2010;120:1940–5. https://doi.org/10.1002/lary.21081.
Soong PL, Schaller B, Zix J, Iizuka T, Mottini M, Lieger O. The role of postoperative prophylactic antibiotics in the treatment of facial fractures: a randomised, double-blind, placebo-controlled pilot clinical study. Part 3: Le Fort and zygomatic fractures in 94 patients. Br J Oral Maxillofac Surg. 2014;52:329–33. https://doi.org/10.1016/j.bjoms.2014.01.010.
Gaal A, Bailey B, Patel Y, Smiley N, Dodson T, Kim D, et al. Limiting antibiotics when managing mandible fractures may not increase infection risk. J Oral Maxillofac Surg. 2016;74:2008–18. https://doi.org/10.1016/j.joms.2016.05.019.
Campos GB, Lucena EE, da Silva JS, Gomes PP, Germano AR. Efficacy assessment of two antibiotic prophylaxis regimens in oral and maxillofacial trauma surgery: preliminary results. Int J Clin Exp Med. 2015;8:2846–52.
Habib AM, Wong AD, Schreiner GC, Satti KF, Riblet NB, Johnson HA, et al. Postoperative prophylactic antibiotics for facial fractures: a systematic review and meta-analysis. Laryngoscope. 2018. https://doi.org/10.1002/lary.27210.
Hammond D, Parmar S, Whitty J, McPhillips M, Wain R. Prescription of antibiotics: does it alter the outcome for patients who have fractures of the angle of the mandible? Br J Oral Maxillofac Surg. 2017;55:958–61. https://doi.org/10.1016/j.bjoms.2017.09.015.
Perepa A, Sinha R, Agarwal A, Khan TA. Protocol for antibiotic administration in mandibular trauma: a prospective clinical trial. J Maxillofac Oral Surg. 2018;17:19–23. https://doi.org/10.1007/s12663-016-0964-9.
Schaefer EHT, Caterson EJ. Antibiotic selection for open reduction internal fixation of mandible fractures. J Craniofac Surg. 2013;24:85–8. https://doi.org/10.1097/scs.0b013e318275ef21.
Adalarasan S, Mohan A, Pasupathy S. Prophylactic antibiotics in maxillofacial fractures: a requisite? J Craniofac Surg. 2010;21:1009–11. https://doi.org/10.1097/SCS.0b013e3181e47d43.
Huang W, Lynham A, Wullschleger M. Orbitozygomatic fracture repairs: are antibiotics necessary? Craniomaxillofac Trauma Reconstr. 2015;8:271–6. https://doi.org/10.1055/s-0034-1399795.
Aznar ML, Schonmeyr B, Echaniz G, Nebeker L, Wendby L, Campbell A. Role of postoperative antimicrobials in cleft palate surgery: prospective, double-blind, randomized, placebo-controlled clinical study in India. Plast Reconstr Surg. 2015;136:59e–66e. https://doi.org/10.1097/PRS.0000000000001324.
Rottgers SA, Camison L, Mai R, Shakir S, Grunwaldt L, Nowalk AJ, et al. Antibiotic use in primary palatoplasty: a survey of practice patterns, assessment of efficacy, and proposed guidelines for use. Plast Reconstr Surg. 2016;137:574–82. https://doi.org/10.1097/01.prs.0000475784.29575.d6.
Schonmeyr B, Wendby L, Campbell A. Early surgical complications after primary cleft lip repair: a report of 3108 consecutive cases. Cleft Palate Craniofac J. 2015;52:706–10. https://doi.org/10.1597/14-158.
Zirk M, Kreppel M, Buller J, Pristup J, Peters F, Dreiseidler T, et al. The impact of surgical intervention and antibiotics on MRONJ stage II and III—retrospective study. J Cranio-Maxillofac Surg. 2017;45:1183–9. https://doi.org/10.1016/j.jcms.2017.05.027.
Hoefert S, Eufinger H. Relevance of a prolonged preoperative antibiotic regime in the treatment of bisphosphonate-related osteonecrosis of the jaw. J Oral Maxillofac Surg. 2011;69:362–80. https://doi.org/10.1016/j.joms.2010.06.200.
Koshkareva YA, Johnson JT. What is the perioperative antibiotic prophylaxis in adult oncologic head and neck surgery? Laryngoscope. 2014;124:1055–6. https://doi.org/10.1002/lary.24226.
Kruse AL, Luebbers HT, Gratz KW, Obwegeser JA. Factors influencing survival of free-flap in reconstruction for cancer of the head and neck: a literature review. Microsurgery. 2010;30:242–8. https://doi.org/10.1002/micr.20758.
Russell MD, Goldberg AN. What is the evidence for use of antibiotic prophylaxis in clean-contaminated head and neck surgery? Laryngoscope. 2012;122:945–6. https://doi.org/10.1002/lary.22484.
Man LX, Beswick DM, Johnson JT. Antibiotic prophylaxis in uncontaminated neck dissection. Laryngoscope. 2011;121:1473–7. https://doi.org/10.1002/lary.21815.
Vila PM, Zenga J, Jackson RS. Antibiotic prophylaxis in clean-contaminated head and neck surgery: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2017;157:580–8. https://doi.org/10.1177/0194599817712215.
Cannon RB, Houlton JJ, Mendez E, Futran ND. Methods to reduce postoperative surgical site infections after head and neck oncology surgery. Lancet Oncol. 2017;18:e405–13. https://doi.org/10.1016/s1470-2045(17)30375-3.
Bartella AK, Kamal M, Teichmann J, Kloss-Brandstatter A, Steiner T, Holzle F, et al. Prospective comparison of perioperative antibiotic management protocols in oncological head and neck surgery. J Cranio-maxillofac Surg. 2017;45:1078–82. https://doi.org/10.1016/j.jcms.2017.04.001.
Veve MP, Davis SL, Williams AM, McKinnon JE, Ghanem TA. Considerations for antibiotic prophylaxis in head and neck cancer surgery. Oral Oncol. 2017;74:181–7. https://doi.org/10.1016/j.oraloncology.2017.09.011.
Murphy J, Isaiah A, Dyalram D, Lubek JE. Surgical site infections in patients receiving osteomyocutaneous free flaps to the head and neck Does choice of antibiotic prophylaxis matter? J Oral Maxillofac Surg. 2017;75:2223–9. https://doi.org/10.1016/j.joms.2017.02.006.
Shkedy Y, Alkan U, Roman BR, Hilly O, Feinmesser R, Bachar G, et al. Role of perioperative antibiotic treatment in parotid gland surgery. Head Neck. 2016;38:E1876–80. https://doi.org/10.1002/hed.24339.
Rosengren H, Heal CF, Buttner PG. Effect of a single prophylactic preoperative oral antibiotic dose on surgical site infection following complex dermatological procedures on the nose and ear: a prospective, randomised, controlled, double-blinded trial. BMJ Open. 2018;8:e020213. https://doi.org/10.1136/bmjopen-2017-020213.
Lee JY, Do HS, Lim JH, Jang HS, Rim JS, Kwon JJ, et al. Correlation of antibiotic prophylaxis and difficulty of extraction with postoperative inflammatory complications in the lower third molar surgery. Br J Oral Maxillofac Surg. 2014;52:54–7. https://doi.org/10.1016/j.bjoms.2013.08.010.
Iglesias-Martin F, Garcia-Perla-Garcia A, Yanez-Vico R, Aced-Jimenez E, Arjona-Gerveno E, Gonzalez-Padilla JD, et al. Comparative trial between the use of amoxicillin and amoxicillin clavulanate in the removal of third molars. Med Oral Patologia Oral y Cirugia Bucal. 2014;19:e612–5.
Arteagoitia I, Ramos E, Santamaria G, Barbier L, Alvarez J, Santamaria J. Amoxicillin/clavulanic acid 2000/125 mg to prevent complications due to infection following completely bone-impacted lower third molar removal: a clinical trial. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119:8–16. https://doi.org/10.1016/j.oooo.2014.08.014.
Bezerra TP, Studart-Soares EC, Scaparo HC, Pita-Neto IC, Batista SH, Fonteles CS. Prophylaxis versus placebo treatment for infective and inflammatory complications of surgical third molar removal: a split-mouth, double-blind, controlled, clinical trial with amoxicillin (500 mg). J Oral Maxillofac Surg. 2011;69:e333–9. https://doi.org/10.1016/j.joms.2011.03.055.
Xue P, Wang J, Wu B, Ma Y, Wu F, Hou R. Efficacy of antibiotic prophylaxis on postoperative inflammatory complications in Chinese patients having impacted mandibular third molars removed: a split-mouth, double-blind, self-controlled, clinical trial. Br J Oral Maxillofac Surg. 2015;53:416–20. https://doi.org/10.1016/j.bjoms.2015.02.001.
Pasupathy S, Alexander M. Antibiotic prophylaxis in third molar surgery. J Craniofac Surg. 2011;22:551–3. https://doi.org/10.1097/SCS.0b013e31820745c7.
Martin-Ares M, Barona-Dorado C, Martinez-Rodriguez N, Cortes-Breton-Brinkmann J, Sanz-Alonso J, Martinez-Gonzalez JM. Does the postoperative administration of antibiotics reduce the symptoms of lower third molar removal? A randomized double blind clinical study. J Clin Exp Dent. 2017;9:e1015–22. https://doi.org/10.4317/jced.54024.
Sayd S, Vyloppilli S, Kumar K, Subash P, Kumar N, Raseel S. Comparison of the efficacy of amoxicillin-clavulanic acid with metronidazole to azithromycin with metronidazole after surgical removal of impacted lower third molar to prevent infection. J Korean Assoc Oral Maxillofac Surg. 2018;44:103–6. https://doi.org/10.5125/jkaoms.2018.44.3.103.
Milani BA, Bauer HC, Sampaio-Filho H, Horliana AC, Perez FE, Tortamano IP, et al. Antibiotic therapy in fully impacted lower third molar surgery: randomized three-arm, double-blind, controlled trial. Oral Maxillofac Surg. 2015;19:341–6. https://doi.org/10.1007/s10006-015-0521-6.
Prajapati A, Prajapati A, Sathaye S. Benefits of not prescribing prophylactic antibiotics after third molar surgery. J Maxillofac Oral Surg. 2016;15:217–20. https://doi.org/10.1007/s12663-015-0814-1.
Reiland MD, Ettinger KS, Lohse CM, Viozzi CF. Does administration of oral versus intravenous antibiotics for third molar removal have an effect on the incidence of alveolar osteitis or postoperative surgical site infections? J Oral Maxillofac Surg. 2017;75:1801–8. https://doi.org/10.1016/j.joms.2017.03.038.
Marghalani A. Antibiotic prophylaxis reduces infectious complications but increases adverse effects after third-molar extraction in healthy patients. J Am Dent Assoc. 2014;145:476–8. https://doi.org/10.14219/jada.2013.51.
Isiordia-Espinoza MA, Aragon-Martinez OH, Martinez-Morales JF, Zapata-Morales JR. Risk of wound infection and safety profile of amoxicillin in healthy patients which required third molar surgery: a systematic review and meta-analysis. Br J Oral Maxillofac Surg. 2015;53:796–804. https://doi.org/10.1016/j.bjoms.2015.06.013.
Cho H, Lynham AJ, Hsu E. Postoperative interventions to reduce inflammatory complications after third molar surgery: review of the current evidence. Aust Dent J. 2017;62:412–9. https://doi.org/10.1111/adj.12526.
Lopez-Cedrun JL, Pijoan JI, Fernandez S, Santamaria J, Hernandez G. Efficacy of amoxicillin treatment in preventing postoperative complications in patients undergoing third molar surgery: a prospective, randomized, double-blind controlled study. J Oral Maxillofac Surg. 2011;69:e5–14. https://doi.org/10.1016/j.joms.2011.01.019.
Lang MS, Gonzalez ML, Dodson TB. Do antibiotics decrease the risk of inflammatory complications after third molar removal in community practices? J Oral Maxillofac Surg. 2017;75:249–55. https://doi.org/10.1016/j.joms.2016.09.044.
Arteagoitia MI, Barbier L, Santamaria J, Santamaria G, Ramos E. Efficacy of amoxicillin and amoxicillin/clavulanic acid in the prevention of infection and dry socket after third molar extraction. A systematic review and meta-analysis. Medicina Oral Patología Oral y Cirugia Bucal. 2016. https://doi.org/10.4317/medoral.21139.
Ramos E, Santamaria J, Santamaria G, Barbier L, Arteagoitia I. Do systemic antibiotics prevent dry socket and infection after third molar extraction? A systematic review and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122:403–25. https://doi.org/10.1016/j.oooo.2016.04.016.
Marcussen KB, Laulund AS, Jorgensen HL, Pinholt EM. A systematic review on effect of single-dose preoperative antibiotics at surgical osteotomy extraction of lower third molars. J Oral Maxillofac Surg. 2016;74:693–703. https://doi.org/10.1016/j.joms.2015.11.017.
Sidana S, Mistry Y, Gandevivala A, Motwani N. Evaluation of the need for antibiotic prophylaxis during routine intra-alveolar dental extractions in healthy patients: a randomized double-blind controlled trial. J Evid Based Dent Pract. 2017;17:184–9. https://doi.org/10.1016/j.jebdp.2017.04.007.
Ata-Ali J, Ata-Ali F, Ata-Ali F. Do antibiotics decrease implant failure and postoperative infections? A systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2014;43:68–74. https://doi.org/10.1016/j.ijom.2013.05.019.
Esposito M, Grusovin MG, Worthington HV. Interventions for replacing missing teeth: antibiotics at dental implant placement to prevent complications. Cochrane Database Syst Rev. 2013;7:CD004152. https://doi.org/10.1002/14651858.cd004152.pub4.
Chrcanovic BR, Albrektsson T, Wennerberg A. Prophylactic antibiotic regimen and dental implant failure: a meta-analysis. J Oral Rehabil. 2014;41:941–56. https://doi.org/10.1111/joor.12211.
Lund B, Hultin M, Tranaeus S, Naimi-Akbar A, Klinge B. Complex systematic review—perioperative antibiotics in conjunction with dental implant placement. Clin Oral Implant Res. 2015;26:1–14. https://doi.org/10.1111/clr.12637.
Sharaf B, Jandali-Rifai M, Susarla SM, Dodson TB. Do perioperative antibiotics decrease implant failure? J Oral Maxillofac Surg. 2011;69:2345–50. https://doi.org/10.1016/j.joms.2011.02.095.
Nolan R, Kemmoona M, Polyzois I, Claffey N. The influence of prophylactic antibiotic administration on post-operative morbidity in dental implant surgery. A prospective double blind randomized controlled clinical trial. Clin Oral Implants Res. 2014;25:252–9. https://doi.org/10.1111/clr.12124.
Krasny M, Krasny K, Zadurska M, Fiedor P. Evaluation of treatment outcomes and clinical indications for antibiotic prophylaxis in patients undergoing implantation procedures. Adv Med Sci. 2016;61:113–6. https://doi.org/10.1016/j.advms.2015.10.005.
El-Kholey KE. Efficacy of two antibiotic regimens in the reduction of early dental implant failure: a pilot study. Int J Oral Maxillofac Surg. 2014;43:487–90. https://doi.org/10.1016/j.ijom.2013.09.013.
Park J, Tennant M, Walsh LJ, Kruger E. Is there a consensus on antibiotic usage for dental implant placement in healthy patients? Aust Dent J. 2018;63:25–33. https://doi.org/10.1111/adj.12535.
Arduino PG, Tirone F, Schiorlin E, Esposito M. Single preoperative dose of prophylactic amoxicillin versus a 2-day postoperative course in dental implant surgery: a two-centre randomised controlled trial. Eur J Oral Implantol. 2015;8:143–9.
Carcuac O, Derks J, Charalampakis G, Abrahamsson I, Wennstrom J, Berglundh T. Adjunctive systemic and local antimicrobial therapy in the surgical treatment of peri-implantitis: a randomized controlled clinical trial. J Dent Res. 2016;95:50–7. https://doi.org/10.1177/0022034515601961.
Hallstrom H, Persson GR, Lindgren S, Renvert S. Open flap debridement of peri-implantitis with or without adjunctive systemic antibiotics: a randomized clinical trial. J Clin Periodontol. 2017;44:1285–93. https://doi.org/10.1111/jcpe.12805.
Cachovan G, Boger RH, Giersdorf I, Hallier O, Streichert T, Haddad M, et al. Comparative efficacy and safety of moxifloxacin and clindamycin in the treatment of odontogenic abscesses and inflammatory infiltrates: a phase II, double-blind, randomized trial. Antimicrob Agents Chemother. 2011;55:1142–7. https://doi.org/10.1128/AAC.01267-10.
Gomez-Arambula H, Hidalgo-Hurtado A, Rodriguez-Flores R, Gonzalez-Amaro AM, Garrocho-Rangel A, Pozos-Guillen A. Moxifloxacin versus clindamycin/ceftriaxone in the management of odontogenic maxillofacial infectious processes: a preliminary, intrahospital, controlled clinical trial. J Clin Exp Dent. 2015;7:e634–9. https://doi.org/10.4317/jced.52627.
Bartella AK, Lemmen S, Burnic A, Kloss-Brandstatter A, Kamal M, Breisach T, et al. Influence of a strictly perioperative antibiotic prophylaxis vs a prolonged postoperative prophylaxis on surgical site infections in maxillofacial surgery. Infection. 2018;46:225–30. https://doi.org/10.1007/s15010-017-1110-4.
Lodi G, Figini L, Sardella A, Carrassi A, Del Fabbro M, Furness S. Antibiotics to prevent complications following tooth extractions. Cochrane Database Syst Rev. 2012;11:CD003811. https://doi.org/10.1002/14651858.cd003811.pub2.
Waasdorp JA, Evian CI, Mandracchia M. Immediate placement of implants into infected sites: a systematic review of the literature. J Periodontol. 2010;81:801–8. https://doi.org/10.1902/jop.2010.090706.
Klinge B, Flemming T, Cosyn J, De Bruyn H, Eisner BM, Hultin M, et al. The patient undergoing implant therapy. Summary and consensus statements. The 4th EAO Consensus Conference 2015. Clin Oral Implants Res. 2015;26:64–7. https://doi.org/10.1111/clr.12675.
Knepil GJ, Loukota RA. Outcomes of prophylactic antibiotics following surgery for zygomatic bone fractures. J Cranio-maxillofac Surg. 2010;38:131–3. https://doi.org/10.1016/j.jcms.2009.03.015.
Mercuri LG, Psutka D. Perioperative, postoperative, and prophylactic use of antibiotics in alloplastic total temporomandibular joint replacement surgery: a survey and preliminary guidelines. J Oral Maxillofac Surg. 2011;69:2106–11. https://doi.org/10.1016/j.joms.2011.01.006.
Hindawi YH, Oakley GM, Kinsella CR Jr, Cray JJ, Lindsay K, Scifres AM. Antibiotic duration and postoperative infection rates in mandibular fractures. J Craniofac Surg. 2011;22:1375–7. https://doi.org/10.1097/SCS.0b013e31821c9498.
Langerman A, Thisted R, Hohmann S, Howell M. Antibiotic and duration of perioperative prophylaxis predicts surgical site infection in head and neck surgery. Otolaryngol Head Neck Surg. 2016;154:1054–63. https://doi.org/10.1177/0194599816634303.
Acknowledgements
The authors like to give special thanks to Mr. Wellbe Bartsma for his extensively language edition.
Funding
This work was supported by the Association of the Scientific Medical Societies in Germany (Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V., AWMF).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Blatt, S., Al-Nawas, B. A systematic review of latest evidence for antibiotic prophylaxis and therapy in oral and maxillofacial surgery. Infection 47, 519–555 (2019). https://doi.org/10.1007/s15010-019-01303-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-019-01303-8