Abstract
Introduction
The emergence of carbapenemase-producing Klebsiella pneumonia (KPC-Kp) has become a significant problem in terms of public health and clinical outcome in many hospitals in Southern Europe. Treatment options are usually limited and effective treatment of infections caused by these pathogens is a considerable challenge for clinicians. Ceftazidime–avibactam has been recently approved for the treatment of difficult-to-treat infections due to aerobic Gram-negative organisms in patients with limited treatment options.
Case report
We reported the first case of KPC-Kp septic thrombophlebitis and right atrial endocarditis associated with metastatic lung abscesses successfully treated with a prolonged ceftazidime/avibactam plus ertapenem treatment course, suggesting that this combination therapy could be safe and effective for serious Gram-negative infections. Interestingly, we also observed an apparent discrepancy between clinical and microbiological courses: the patient became rapidly afebrile; hemodynamically stable and his procalcitonin levels showed a prompt decreasing trend. Nevertheless, blood cultures remained persistently positive for a prolonged period.
Conclusion
In conclusion, ceftazidime–avibactam plus ertapenem was a safe and effective therapy of serious endovascular infection due to KPC-Kp. Moreover, in this setting, follow-up blood cultures might represent an irreplaceable tool to guide the therapy.
Similar content being viewed by others
Introduction
Gram-negative bacteria are an infrequent cause of infective endocarditis, accounting for the 1–3% of the etiologies according to the International Collaboration on Endocarditis Prospective Cohort Study and the Italian Endocarditis Study [1,2,3]. During the 1970s and 1980s, these infections were mostly community-acquired since that intravenous drug addiction represented the main risk factor for Gram-negative endocarditis (GNE) [3].
Currently GNE has been observed mainly among patients hospitalized or with healthcare contacts who undergo invasive procedures, implant of endovascular devices or are affected by comorbidities that are likely to increase the risk for Gram-negative bacteremia [3].
According to the ICE-PCS the overall in-hospital mortality rate for patients with non-HACEK GNB endocarditis is around 25%. However, recent reports describe trends towards multidrug resistance (MDR) among isolates of GNE with associated higher mortality rates [3, 4].
We here report a unique case of a trauma-patient with right mural endocarditis and central veins thrombophlebitis caused by Klebsiella pneumoniae carbapenemase producing Klebsiella (KPC-Kp) that was successfully treated with adoption of a prolonged ceftazidime-avibactam (CAZ/AVI) plus ertapenem treatment course.
Case report
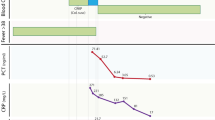
A 49-year-old man was admitted to intensive care unit (ICU) for chest trauma (he had been trampled by a bull). His medical history showed no previous infections and no comorbidities. On admission, he was neither conscious nor hemodynamically stable, and required vasopressors and mechanical ventilation. Lung high resolution computed tomography (HRTC) revealed the presence of multiple lung contusions, rib fractures and bilateral pneumothorax with hemothorax, so three pleural drainage tubes were positioned. On day 7, he developed fever (up to 38.7°C) and respiratory and hemodynamic failure. Lung HRTC revealed new parenchymal infilatrates, meanwhile bronchial aspirate cultures revealed growth of a KPC-Kp strain susceptible only to colistin (MIC < 0.5 µg/ml) according to Vitek 2 (Biomérieux) test. The presence of the Klebsiella pneumoniae carbapenemase gene was confirmed using the GeneXpert System (Cepheid) nucleic acid test. A diagnosis of KPC-Kp ventilator associated pneumonia (VAP) was made and the patient was started on a colistin (9 MU i.v. loading dose, followed by 4.5 MU i.v. q12h and 2MU aerosol q8h), tigecycline (150 mg i.v. loading dose, followed by 100 mg i.v. q12h) and meropenem (2 g extended infusion i.v. q8h) regimen. On day 10, he developed a severe Clostridium difficile infection, unresponsive to topical vancomycin (125 mg po q6h), that resolved with a 10-day fidaxomicin (200 mg po q12h) treatment course. On day 13, KPC-Kp breakthrough bacteremia developed and fosfomycin (8 g i.v. q8h) was added to therapy. As shown in Fig. 2, at the beginning of KPC-Kp bacteremia procalcitonin increased up to 4.6 ng/ml. On day 21 (10th day of treatment course), the patient was afebrile, hemodynamically stable without vasopressors with a significant clinical improvement, and procalcitonin levels decreased below 0.5 ng/ml. However, his blood cultures remained still positive. On day 28, CT scan detected new cavitary lung lesions. A transesophageal echocardiogram (TEE) displayed 0.8 mm vegetation on the superior wall of the right atrium. There was no vegetation at any of the valves and no obvious abscess. CT angiography revealed jugular and superior cava veins thrombosis. Based on these data, a diagnosis of septic thrombophlebitis and right atrial mural endocarditis with secondary septic pulmonary embolism and abscesses was been established (Fig. 1).
Surgical debridement was not recommended and the patient was started on enoxaparin treatment. On day 33, blood cultures still yielded KPC-Kp. Disc diffusion susceptibility test revealed in vitro susceptibility of the KPC isolate to CAZ/AVI and a possible synergy effect of CAZ/AVI with ertapenem [5]. Thus, initial combination of CAZ/AVI (provided for compassionate use) and fosfomycin was modified to a combination of CAZ/AVI (2 g/500 mg i.v. q8h) and ertapenem (1 g i.v. q24h) since day 38 (Fig. 2). No adverse events developed during therapy and clinical conditions continued to improve. Except for a candidemia episode successfully treated with a 14-day caspofungin treatment course, the patient remained afebrile with low procalcitonin levels. Nevertheless, blood cultures continued to be persistently positive until day 80. Subsequently, CT angiography and serial TEEs documented disappearance of both veins and atrial lesions. On day 157, the patient was discharged in good clinical conditions.
The patient resulted no sick at three follow up visits during a 5-month period of clinical observation. Eventually, the patient had a sudden death 6 months after hospital discharge. Close relatives denied any sign or symptom attributable to infection relapse.
Discussion
Nowadays, infections due to hospital-acquired MDR organisms are a major matter of concern for clinicians worldwide [6] being associated with increased short- and long-term mortality rates [7]. In particular, the emergence of KPC-Kp has become a significant problem in terms of public health and clinical outcome since these organism have been not only able to cause numerous infection outbreaks worldwide, but are now considered endemic in many hospitals in southern Europe.
Effective treatment of infections caused by these pathogens is thus a considerable challenge for clinicians [8, 9], and microbial stewardship is a crucial tool in limiting the spreading of the current epidemic [10, 11].
Treatment options are usually limited to colistin, gentamicin and/or tigecycline in association with a carbapenem [12], but the optimal regimen for infections caused by KPC-Kp has yet to defined.
CAZ/AVI consists of a combination of ceftazidime, a widely used expanded-spectrum anti-pseudomonal cephalosporin, and avibactam, a novel non-suicide non-β-lactam β-lactamase inhibitor that restore in vitro activity of ceftazidime against MDR Enterobacteriaceae and P aeruginosa by inhibiting class A (such as ESBLs, Klebsiella pneumonia carbapenemases), class C (AmpC), and some class D (eg, OXA 48) β-lactamases enzymes [13].
CAZ–AVI has been recently approved by European Medicines Agency (EMA) for the treatment of complicated urinary tract infections, nosocomial pneumonia including ventilator-associated pneumonia (VAP), complicated intra-abdominal infections and infections due to aerobic Gram-negative organisms in patients with limited treatment options. In clinical practice, it has been used with encouraging results in small series of patients with CR-Kp bacteremia and pneumonia [13, 14]. Recently, in a large series of 138 cases of KPC-Kp infections in adults who received CAZ/AVI in compassionate-use programs in Italy it appearred to be a promising drug for treatment of as severe infections as bacteremias [15].
To our knowledge, here we describe the first case of septic thrombophlebitis associated to right atrial endocarditis complicated by multiple lung abscesses due to Kp-KPC successfully treated with long-term CAZ/AVI plus ertapenem therapy. Persistent bacteremia and the possible erratic susceptibility to colistin according to Vitek 2 [16, 17] prompted us to change therapy with a CAZ/AVI based regimen. We decided to use CAZ/AVI in combination with a carbapenem hoping to a possible synergistic interaction [5, 18] either able to result in an enhanced antibacterial effect and to prevent the recently reported emergence of resistance during therapy with this agent [19]. In our case, the synergy between both antimicrobials was not clearly demonstrated by adequate “in vitro” studies as time-kill curves or checkerboard assays: therefore, it cannot be definitively ruled out that the beneficial effect of the antimicrobial treatment could be assigned exclusively to CAZ/AVI alone. Moreover, CAZ/AVI plus ertapenem was started on day 38 of evolution and the patient remained with persistent bacteremia until day 80. Thus, it cannot be definitively ruled out that having continued with the initial antimicrobial regimen that the patient received could have been as effective as the combination of antimicrobials used in the final phase of evolution.
Another interesting aspect of our case is the apparent discrepancy between clinical and microbiological course. Indeed, our patient clinically responded to the antibiotic therapy: he became rapidly afebrile, hemodynamically stable and his procalcitonin levels showed a prompt decreasing trend. Nevertheless, blood cultures remained persistently positive for a prolonged period (approximately 8 weeks), despite appropriate antibiotic therapy. This finding not only confirms our recent observation in a small series of GN bacillary thrombophlebitis [20], but is also corroborated by recent observations demonstrating significantly lower PCT levels in endovascular infections as endocarditis or catheter-related infections (0.21 and 0.76 ng/ml, respectively) compared to deep-seated infections (e.g. urinary tract infection, median PCT levels 5.05 or abdominal infection 3.36 ng/ml) [21].
Based on these studies, clinicians should be aware that PCT studies might not be a reliable marker neither for suspicion of infection nor to monitor the clinical outcome of Gram negative bacillary endovascular infections. Under these circumstances, follow up blood cultures remain an irreplaceable tool to guide the therapy.
In conclusion, even if further study is required to confirm this preliminary favourable observation, CAZ/AVI plus ertapenem was safe and effective therapy of a serious infection as septic thrombophlebitis and right atrial endocarditis with secondary septic pulmonary embolism caused by a KPC-Kp. This case report could constitute an argument for initiating the new β-lactamase-inhibitor containing combination at an early time point in the course of a complicated infection due to MDR Klebsiella.
Change history
10 July 2018
The given names and family names of all authors were transposed in the original publication. The original article has been corrected.
References
Murdoch DR, Corey GR, Hoen B, Miró JM, Fowler VG Jr, Bayer AS, Karchmer AW, Olaison L, Pappas PA, Moreillon P, Chambers ST, Chu VH, Falcó V, Holland DJ, Jones P, Klein JL, Raymond NJ, Read KM, Tripodi MF, Utili R, Wang A, Woods CW, Cabell CH, International Collaboration on Endocarditis-Prospective Cohort Study (ICE-PCS) Investigators. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009;169:463–73.
Leone S, Ravasio V, Durante-Mangoni E, Crapis M, Carosi G, Scotton PG, Barzaghi N, Falcone M, Chinello P, Pasticci MB, Grossi P, Utili R, Viale P, Rizzi M, Suter F. Epidemiology, characteristics, and outcome of infective endocarditis in Italy: the Italian study on endocarditis. Infection 2012;40:527–35.
Falcone M, Tiseo G, Durante-Mangoni E, Ravasio V, Barbaro F, Ursi MP, Pasticci MB, Bassetti M, Grossi P, Venditti M, Rizzi M. Risk factors and outcomes of endocarditis due to non-HACEK Gram-negative bacilli: data from the prospective multicenter italian endocarditis study cohort. Antimicrob Agents Chemother. 2018. https://doi.org/10.1128/AAC.02208-17.
Morpeth S, Murdoch D, Cabell CH, Karchmer AW, Pappas P, Levine D, Nacinovich F, Tattevin P, Fernández-Hidalgo N, Dickerman S, Bouza E, del Río A, Lejko-Zupanc T, de Oliveira Ramos A, Iarussi D, Klein J, Chirouze C, Bedimo R, Corey GR, Fowler VG Jr, International Collaboration on Endocarditis Prospective Cohort Study (ICE-PCS) Investigators. Non-HACEK Gram-negative bacillus endocarditis. Ann Intern Med. 2007;147:829–35.
Camargo JF, Simkins J, Beduschi T, Tekin A, Aragon L, Pérez-Cardona A, et al. Successful treatment of carbapenemase-producing pandrug-resistant Klebsiella pneumoniae bacteremia. Antimicrob Agents Chemother. 2015;59:5903–8.
Grundmann H, Glasner C, Albiger B, Aanensen DM, Tomlinson CT, Andrasević AT, Cantón R, Carmeli Y, Friedrich AW, Giske CG, Glupczynski Y, Gniadkowski M, Livermore DM, Nordmann P, Poirel L, Rossolini GM, Seifert H, Vatopoulos A, Walsh T, Woodford N, Monnet DL, European Survey of Carbapenemase-Producing Enterobacteriaceae (EuSCAPE) Working Group. Occurrence of carbapenemase-producing Klebsiella pneumoniae and Escherichia coli in the European survey of carbapenemase-producing Enterobacteriaceae (EuSCAPE): a prospective, multinational study. Lancet Infect Dis. 2017;17:153–63.
Giske CG, Monnet DL, Cars O, Carmeli Y. Clinical and economic impact of common multidrug-resistant Gram-negative bacilli. Antimicrob Agents Chemother. 2008;52:813–21.
Nordmann P, Naas T, Poirel L. Global spread of carbapenemase producing Enterobacteriaceae. Emerg Infect Dis. 2011;17:1791–8.
Nordmann P, Cuzon G, Naas T. The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria. Lancet Infect Dis. 2009;9:228–36.
Giacobbe DR, Del Bono V, Mikulska M, Gustinetti G, Marchese A, Mina F, Signori A, Orsi A, Rudello F, Alicino C, Bonalumi B, Morando A, Icardi G, Beltramini S, Viscoli C, San Martino Antimicrobial Stewardship Group. Impact of a mixed educational and semi-restrictive antimicrobial stewardship project in a large teaching hospital in Northern Italy. Infection. 2017;45:849–56.
Murri R, Fiori B, Spanu T, Mastrorosa I, Giovannenze F, Taccari F, Palazzolo C, Scoppettuolo G, Ventura G, Sanguinetti M, Cauda R, Fantoni M. Trimethoprim-sulfamethoxazole therapy for patients with carbapenemase-producing Klebsiella pneumoniae infections: retrospective single-center case series. Infection. 2017;45:209–13.
Carmeli Y, Akova M, Cornaglia G, Daikos GL, Garau J, Harbarth S, et al. Controlling the spread of carbapenemase-producing Gram-negatives: therapeutic approach and infection control. Clin Microbiol Infect. 2010;16:102–11.
Falcone M, Paterson D. Spotlight on ceftazidime/avibactam: a new option for MDR Gram-negative infections. J Antimicrob Chemother. 2016;71:2713–22.
Shields RK, Nguyen MH, Chen L, Press EG, Potoski BA, Marini RV, Doi Y, Kreiswirth BN, Clancy CJ. Ceftazidime–avibactam is superior to other treatment regimens against carbapenem-resistant Klebsiella pneumonia bacteremia. Antimicrob Agents Chemother. 2017;61:e00883–17.
Tumbarello M, Trecarichi EM, Corona A, De Rosa FG, Bassetti M, Mussini C, Menichetti F, Viscoli C, Campoli C, Venditti M, De Gasperi A, Mularoni A, Tascini C, Parruti G, Pallotto C, Sica S, Concia E, Cultrera R, De Pascale G, Capone A, Antinori S, Corcione S, Righi E, Losito AR, Digaetano M, Amadori F, Giacobbe DR, Ceccarelli G, Mazza E, Raffaelli F, Spanu T, Cauda R, Viale P. Efficacy of ceftazidime–avibactam salvage therapy in patients with infections caused by KPC-producing Klebsiella pneumoniae. Clin Infect Dis. 2018. https://doi.org/10.1093/cid/ciy492.
European Committee on Antimicrobial Susceptibility Testing (EUCAST). EUCAST warnings concerning antimicrobial susceptibility testing products or procedures. Växjö: European Committee on Antimicrobial Susceptibility Testing; 2018. http://www.eucast.org/ast_of_bacteria/warnings. Accessed 15 June 2018.
Matuschek E, Åhman J, Webster C, Kahlmeter G. Antimicrobial susceptibility testing of colistin—evaluation of seven commercial MIC products against standard broth microdilution for Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter spp. Clin Microbiol Infect. 2017. https://doi.org/10.1016/j.cmi.2017.11.020.
Gaibani P, Lewis RE, Volpe SL, Giannella M, Campoli C, Landini MP, Viale P, Re MC, Ambretti S. In vitro interaction of ceftazidime–avibactam in combination with different antimicrobials against KPC-producing Klebsiella pneumoniae clinical isolates. Int J Infect Dis. 2017;65:1–3.
Shields RK, Nguyen MH, Press EG, Chen L, Kreiswirth BN, Clancy CJ. Emergence of ceftazidime–avibactam resistance and restoration of carbapenem susceptibility in Klebsiella pneumoniae carbapenemase-producing K. pneumoniae: a case report and review of literature. Open Forum Infect Dis. 2017;4:ofx101.
Ceccarelli G, Giuliano S, Falcone M, Venditti M. Follow-up blood cultures: a 2.0 diagnostic tool in patients with Gram-negative bacteremia and septic thrombophlebitis. Clin Infect Dis. 2018;66:1154–5.
Yan ST, Sun LC, Jia HB, Gao W, Yang JP, Zhang GQ. Procalcitonin levels in bloodstream infections caused by different sources and species of bacteria. Am J Emerg Med. 2017;35:579–83.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
The original version of this article was revised: The given names and family names of all authors were transposed. The correct names are given above.
Rights and permissions
About this article
Cite this article
Iacovelli, A., Spaziante, M., Al Moghazi, S. et al. A challenging case of carbapenemase-producing Klebsiella pneumoniae septic thrombophlebitis and right mural endocarditis successfully treated with ceftazidime/avibactam. Infection 46, 721–724 (2018). https://doi.org/10.1007/s15010-018-1166-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-018-1166-9