Abstract
Purpose
The purpose of this study was to establish a baseline for measuring the impact of the programmatic management of drug-resistant TB program by following up on outcomes of all patients diagnosed with multidrug-resistant tuberculosis in Zambia between 2012 and 2014.
Methods
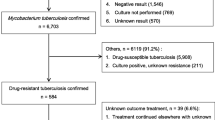
A cohort study of all the MDR-TB patients diagnosed at the national TB reference laboratory from across Zambia. MDR-TB was diagnosed by culture and DST, whereas outcome data were collected in 2015 by patient record checks and home visits.
Results
The total number of patients diagnosed was 258. Of those, 110 (42.6%) patients were traceable for this study. There were 67 survivor participants (60.9%); 43 (39.1%) were deceased. Out of the 110 patients who were traced, only 71 (64.5%) were started on second-line treatment. Twenty-nine (40.8%) patients were declared cured and 16.9% were still on treatment; 8.4% had failed treatment. The survival rate was 20.2 per 100 person-years of follow-up. Taking ARVs was associated with a decreased risk of dying (hazard ratio 0.12, p = 0.002). Sex, age, marital status and treatment category were not important predictors of survival in MDR-TB patients.
Conclusions
More than half of the patients diagnosed with MDR-TB were lost to follow-up before second-line treatment was initiated.




Similar content being viewed by others
References
World Health Organization, Global TB Report 2016. Geneva, Switzerland.
Gandhi NR, Moll A, Sturm AW, Pawinski R, Govender T, Lalloo U, et al. Extensively drug-resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. Lancet. 2006;368:1575–80.
Shah N, Wright A, Bai GH, Barrera L, Boulahbal F, Martín-Casabona N, et al. Worldwide emergence of extensively drug-resistant tuberculosis (XDR TB): global survey of second-line drug resistance among Mycobacterium tuberculosis isolates. Emerg Infect Dis. 2007;13:380–7.
Lukoye D, Ssengooba W, Musisi K, Kasule GW, Cobelens FG, Joloba M, et al. Variation and risk factors of drug resistant tuberculosis in sub-Saharan Africa: a systematic review and meta-analysis. BMC Public Health. 2015;25:291. doi:10.1186/s12889-015-1614-8.
Andrews RJ, Shah NS, Gandhi N, Moll T, Friedland G, et al. Multidrug-resistant and extensively drug-resistant tuberculosis: implications for the HIV epidemic and anti-retroviral therapy rollout in South Africa. JID. 2007;196:S482–90.
Berhan A, Berhan Y, Yizengaw D. A meta-analysis of drug resistant tuberculosis in Sub Saharan Africa: how strongly associated with previous treatment and HIV co-infection? Ethiop J Health Sci. 2013;23:271–82.
Kapata N, Chanda-Kapata P, O’Grady J, Schwank S, Bates M, Mukonka V, et al. Trends of Zambia’s tuberculosis burden over the past two decades. Trop Med Int Health. 2011;16:1404–9.
Moodley R, Godec RT. Short-course treatment for multidrug-resistant tuberculosis: the stream trials. Eur Respir Rev. 2016;25:29–35. doi:10.1183/16000617.0080-2015.
MOH. Guidelines for the programmatic management of drug-resistant tuberculosis in Zambia. Lusaka: Ministry of Health; 2015.
Kapata N, Chanda-Kapata P, Bates M, Mwaba P, Cobelens F, Grobusch MP, et al. Multidrug-resistant TB in Zambia: review of national data from 2000 to 2011. Trop Med Int Health. 2013;18:1386–91.
Kapata N, Mbulo G, Cobelens F, de Haas P, Schaap A, Mwamba P, et al. The Second Zambian National Tuberculosis Drug Resistance survey—a comparison of conventional and molecular methods. Trop Med Int Health. 2015;20:1492–500.
World Health Organization. International Standard Verbal Autopsy questionnaire. 1999. http://www.who.int/healthinfo/statistics/verbal_autopsy_standards2.pdf. Accessed 15 Mar 2014.
Nkosi D, Janssen S, Padanilam X, Louw R, Menezes CN, Grobusch MP. Factors influencing specialist care referral of multidrug- and extensively drug-resistant tuberculosis patients in Gauteng/South Africa: a descriptive questionnaire-based study. BMC Health Serv Res. 2013; 13:268. http://www.biomedcentral.com/1472-6963/13/268. Accessed 10 Jan 2017.
Cox H, Dickson-Hall L, Ndjeka N, Hoog A, Grant A, Cobelens F, et al. Delays and loss to follow-up before treatment of drug-resistant tuberculosis following implementation of Xpert MTB/RIF in South Africa: a retrospective cohort study. PLoS Med. 2017;14:e1002238. doi:10.1371/journal.pmed.1002238.
Xu Z, Xiao T, Li Y, Yang K, Tang Y, Bai L. Reasons for non-enrollment in treatment among multi-drug resistant tuberculosis patients in Hunan Province, China. PLoS One. 2017;12:e0170718. doi:10.1371/journal.pone.0170718.
Ade S, Trébucq A, Harries AD, Ade G, Agodokpessi G, Wachinou P, et al. Follow-up and tracing of tuberculosis patients who fail to attend their scheduled appointments in Cotonou, Benin: a retrospective cohort study. BMC Health Serv Res. 2016;16:5. doi:10.1186/s12913-015-1219-z.
MacPherson P, Houben MGJR, Glynn RJ, Corbett EL, Kranzer K. Pre-treatment loss to follow-up in tuberculosis patients in low- and lower-middle-income countries and high-burden countries: a systematic review and meta-analysis. Bull World Health Organ. 2014;92:126–38. doi:10.2471/BLT.13.124800.
Lange C, Abubakar I, Alffenaar JC, Bothamley G, Caminero JA, et al. Management of patients with multidrug-resistant/extensively drug-resistant tuberculosis in Europe: a TBNET consensus statement. Eur Respir J. 2014;44:23–63. doi:10.1183/09031936.00188313.
Khaliaukin A, Kumar AMV, Skrahina A, Hurevich H, Rusovich V, Gadoev J, et al. Poor treatment outcomes among multidrug-resistant tuberculosis patients in Gomel Region, Republic of Belarus. PHA. 2014;4:S24–8.
Khann S, Eang MT, Rajendra YP, Satyanarayana S, Nagaraja SB, Kumar AMV. Linkage of presumptive multidrug resistant tuberculosis (MDR-TB) patients to diagnostic and treatment services in Cambodia. PLoS One. 2013;8:e59903.
Chadha SS, Sharath BN, Reddy K, Jaju J, Vishnu PH, Rao S, et al. Operational challenges in diagnosing multi-drug resistant TB and initiating treatment in Andhra Pradesh, India. PLos One. 2011;6:e26659.
Singh UB, Pandey P, Mehta G, Bhatnagar AK, Anant Mohan A, Goyal V, et al. Genotypic, phenotypic and clinical validation of GeneXpert in extra-pulmonary and pulmonary tuberculosis in India. PLos One. 2016;11:e0149258. doi:10.1371/journal.pone.0149258 (eCollection2016).
Metcalfe ZJ, Makumbirofa S, Makamure B, Sandy C, Bara W, Mason P, et al. Xpert MTB/RIF detection of rifampin resistance and time to treatment initiation in Harare, Zimbabwe. Int J Tuberc Lung Dis. 2016;20:882–9. doi:10.5588/ijtld.15.0696.
Ade S, Adjibodé O, Wachinou P, Toundoh N, Awanou B, Agodokpessi G, et al. Characteristics and treatment outcomes of retreatment tuberculosis patients in Benin. Tuberc Res Treat. 2016;2016:1468631. doi:10.1155/2016/1468631 (Epub 2016 Mar 24).
Stagg HR, White PJ, Riekstiņa V, Cīrule A, Šķenders G, Leimane V, et al. Decreased time to treatment initiation for multidrug-resistant tuberculosis patients after use of Xpert MTB/RIF test, Latvia. Emerg Infect Dis. 2016;22:482–90. doi:10.3201/eid2203.151227.
Nathavitharana RR, Hillemann D, Schumacher SG, Schlueter B, Ismail N, Omar SV, et al. Multicenter noninferiority evaluation of Hain GenoType MTBDRplus version 2 and Nipro NTMMDRTB line probe assays for detection of rifampin and isoniazid resistance. J Clin Microbiol. 2016;54:1624–30. doi:10.1128/JCM.00251-16.
Nikolayevskyy V, Balabanova Y, Simak T, Malomanova N, Fedorin I, Drobniewski F, et al. Performance of the Genotype® MTBDRPlus assay in the diagnosis of tuberculosis and drug resistance in Samara, Russian Federation. BMC Clin Pathol. 2009;9:2. doi:10.1186/1472-6890-9-2.
Hicks RM, Padayatchi N, Shah NS, Wolf A, Werner L, Sunkari VB, et al. Malnutrition associated with unfavourable outcome and death among South African MDR-TB and HIV co-infected children. Int J Tuberc Lung Dis. 2014;18:1074–83. doi:10.5588/ijtld.14.0231.
Seddon JA, Hesseling AC, Godfrey-Faussett P, Schaaf HS. High treatment success in children treated for multidrug-resistant tuberculosis: an observation cohort study. Thorax. 2014;69:458–64. doi:10.1136/thoraxjnl-2013-203900 (Epub 2013 Sep 24).
Bates M, Shibemba A, Mudenda V, Chimoga C, Tembo J, Kabwe M, et al. Burden of respiratory tract infections at post mortem in Zambian children. BMC Med. 2016;14:99. doi:10.1186/s12916-016-0645-z.
Shean KP, Willcox PA, Siwendu SN, Laserson KF, Gross L, Kammerer S, Wells CD, et al. Treatment outcome and follow-up of multidrug-resistant tuberculosis patients, West Coast/Winelands, South Africa, 1992–2002. Int J Tuberc Lung Dis. 2008;12:1182–9.
Brust JC, Gandhi NR, Carrara H, Osburn G, Padayatchi N, et al. High treatment failure and default rates for patients with multidrug-resistant tuberculosis in KwaZulu-Natal, South Africa, 2000–2003. Int J Tuberc Lung Dis. 2010;14:413–9.
Isaakidis P, Casas EC, Das M, Tseretopoulou X, Ntzani EE, Ford N. Treatment outcomes for HIV and MDR-TB co-infected adults and children: systematic review and meta-analysis. Int J Tuberc Lund Dis. 2015;19:969–78. doi:10.5588/ijtld.15.0123.
Oladimeji O, Isaakidis P, Obasanya OJ, Eltayeb O, Khogali M, Van den Bergh R, et al. Intensive-phase treatment outcomes among hospitalized multidrug-resistant tuberculosis patients: results from a Nationwide Cohort in Nigeria. PLos One. 2014;9:e94393. doi:10.1371/journal.pone.0094393.
Ahuja SD, Ashkin D, Avendano M, Banerjee R, Bauer M, Bayona JN, et al. Multidrug resistant pulmonary tuberculosis treatment regimens and patient outcomes: an individual patient data meta-analysis of 9153 patients. PLos Med. 2012;9:e1001300.
Johnston JC, Shahidi NC, Sadatsafavi M, Fitzgerald JM. Treatment outcomes of multidrug-resistant tuberculosis: a systematic review and meta-analysis. PLos One. 2009;4:e6914.
World Health Organization. The global plan to stop TB: 2011–2015. Geneva: World Health Organization, 2010. http://www.stoptb.org/assets/documents/global/plan/TB_GlobalPlanToStopTB2011–2015.pdf. Accessed 2 Jun 2014.
Loveday M, Wallengren K, Brust J, Roberts J, Voce A, Margot B, et al. Community-based care vs. centralised hospitalisation for MDRTB patients KwaZulu-Natal, South Africa. Int J Tuberc Lung Dis. 2015;19:163–71. doi:10.5588/ijtld.14.0369.
Meressa D, Hurtado MR, Andrews RJ, Diro E, Abato K, Daniel T, et al. Achieving high treatment success for multidrug resistant TB in Africa: initiation and scale-up of MDR TB care in Ethiopia—an observational cohort study. Thorax. 2015;70:1181–8. doi:10.1136/thoraxjnl-2015-207374.
Mitnick DC, Rodriguez AC, Hatton LM, Brigden G, Cobelens F, Grobusch MP, et al. Programmatic management of drug resistant tuberculosis: an updated research Agenda. PLoS One. 2016;11:e0155968. doi:10.1371/journal.pone.0155968.
Holtz TH, Lancaster J, Laserson KF, Wells CD, Thorpe L, Weyer K. Risk factors associated with default from multidrug- resistant tuberculosis treatment, South Africa, 1999–2001. Int J Tuberc Lung Dis. 2006;10:649–55.
Gler MT, Podewils LJ, Munez N, Galipot M, Quelapio MID, Tupasi TE. Impact of patient and program factors on default during treatment of multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2012;16:955–60. doi:10.5588/ijtld.11.050.
Tupasi ET, Garfin GAMC, Kurbatova VE, Mangan JM, Orillaza-Chi R, Naval LC, et al. Factors associated with loss to follow-up during treatment for multidrug-resistant tuberculosis, the Philippines, 2012–2014. Emerg Infect Dis. 2016;22:491. doi:10.3201/eid2203.151788.
Huson MA, Kalkman R, Stolp SM, Janssen S, Alabi AS, Beyeme JO, van der Poll T, Grobusch MP. The impact of HIV on presentation and outcome of bacterial sepsis and other causes of acute febrile illness in Gabon. Infection. 2015;43:443–51. doi:10.1007/s15010-015-0753-2 (Epub 2015 Mar 11).
WHO 2016. The Shorter MDR-TB regimen. http://www.who.int/tb/short_MDR_regimen_factsheet.pdf. Accessed 25 Jul 2017.
Acknowledgements
The authors wish to acknowledge the field staff and collaborators who assisted with data collection; follow-up of participants and overall study implementation.
Author information
Authors and Affiliations
Contributions
Author contributions
Conceptualization: NK, GC, PCK, AZ. Methodology: NK, GC, FC, WN. Data analysis: PCK, MB, MPG, PK, PM. Writing original draft: NK, FC, MPG, MT, SM, PCK. Writing review and editing: NK, MPG, FC, PM, AZ.
Corresponding author
Ethics declarations
Funding
The study was partially funded by the Government of the Republic of Zambia through the Ministry of Health, research unit.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Kapata, N., Grobusch, M.P., Chongwe, G. et al. Outcomes of multidrug-resistant tuberculosis in Zambia: a cohort analysis. Infection 45, 831–839 (2017). https://doi.org/10.1007/s15010-017-1054-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-017-1054-8